Abstract
Objective
Describe the development and evaluation of the “Healthy-Lunchbox-Challenge” (HLC), a nutrition program targeting staff/parents/children in summer day camps (SDCs).
Methods
Single group, pre/post-assessment design was utilized during summer-2011(baseline) and 2012 (intervention). Four community-based SDCs in South Carolina participated. Intervention components were applied over the 11 week SDC program (2012) and consist of: 1) parent/staff education on “Building-a-Better-Lunchbox”, 2) child/staff incentive program. Child/staff foods/beverages were assessed via direct observation (1,977 children; 241 staff). Percentages of foods/beverages brought by children/staff during intervention were compared to baseline measures using mixed-effects regression models.
Results
The percentage of children bringing fruits/vegetables/water increased from 31%–42% (p = 0.00), 5%–16% (p = 0.00), and 47%–60% (p = 0.00) from baseline to post-assessment. Staff fruits/vegetables increased from 30%–47% (p = 0.03), 9%–22% (p = 0.03). A slight decrease was observed for staff water (64%– 58%), however this was not statistically significant. Decreases in low-nutrient-dense foods/beverages were also observed.
Conclusions and Implications
The HLC represents a low-cost, innovative way to influence the nutritional content of child/staff foods/beverages in SDCs.
Keywords: Nutrition Policy, Health Promotion, Summer Day Camp, Child
INTRODUCTION
Summertime, seen as a respite for children from the school year routine, is also the time of the most rapid weight gain in youth 1. A primary factor in unhealthy weight gain observed during summer months is the increased availability/consumption of high-calorie foods 2. Summer day camps (SDCs), seasonal recreational programs providing day long (8am–5pm) child-care during the 8–11weeks of summer, offer a unique opportunity to influence the foods and beverages children consume during this time. Approximately 14.3 million children attend SDCs annually 3, thus SDCs are a potentially high reach setting that can influence children’s eating habits. The National Afterschool Association (NAA) released Healthy Eating Standards (April, 2011) for SDCs to ensure foods and beverages consumed support lifelong health of children. These standards specify children consume a fruit, vegetable, and water daily during SDC while avoiding sugar-based foods and beverages (e.g. candy, non-100% juices) 4. The standards emphasize the role of staff promotion of healthy dietary habits and the importance of providing parents with food guides supporting healthy eating standards. Currently, the extent to which SDCs are meeting these standards is unknown.
Less than ten percent of the 21 million children receiving free or reduced price lunches during the school year participate in the USDA Summer Food Service Program5, 6, leaving parents the responsibility of packing foods and beverages during SDC. Of the studies targeting foods and beverages packed by parents in other settings (e.g., child-care, afterschool programs) 7–9,8, there has been little to no improvement in fruits, vegetables, whole grains, and/or water. This lack of improvement in the foods and beverages packed by parents suggest the need for innovative strategies to influence what parents pack for SDC. Therefore, the purpose of this paper is to describe the development and evaluation of the Healthy Lunchbox Challenge (HLC), an innovative, theory and incentive-based program to influence the amount of fruits, vegetables, and water brought to SDC by children. As a secondary outcome, the HLC also targeted the foods and beverages brought by staff.
METHODS
Participants
Four large-scale community-based SDCs in central South Carolina participated in the study during the summer 2011(baseline) and 2012 (intervention). Site level demographics were assessed for each school district served by the SDCs using the South Carolina Department of Education’s yearly free and reduced lunch eligibility reports. The average percent of children eligible for free or reduced lunch across the four sites was 50%, with a range of 32% to 86%. None of the SDCs were receiving federal reimbursement for meals or snacks. Parents were informed of study procedures through orientation packets, newsletters, and through information posted at each SDC location. Due to the observational nature of this study, participants provided passive consent for the recording of foods and beverages. All procedures were approved by the University of South Carolina’s Institutional Review Board for the Protection of Human Subjects.
Intervention Components
The HLC was grounded in behavioral choice theory (BCT) 10 and goal-setting theory 11. The concept of group goal setting, a key component of the HLC, has been shown to be an important mediator of group task performance11. Additionally, studies employing BCT principles and constructs of goal-setting theory indicate that behavior change may be more likely when messages target increases in positive recommended behaviors (e.g., packing fruits, vegetables, and water) rather than messages restricting behaviors (e.g., do not pack sugar-sweetened beverages, chips, or candy) and clear goals are set to achieve 11– 13. Focusing on recommended behaviors has the potential to elicit substitutions where fruits, vegetables, and water are brought to SDC, and conversely, untargeted reductions in packing non-recommended items, such as chips or soda occur13. Additionally, rewards (identified by each SDC) were used to provide incentive for children and parents to pack fruits, vegetables, and water daily. These approaches served as the theoretical foundation upon which the HLC was created. Considering the lack of onsite refrigeration dairy products were not specifically targeted.
Weekly meetings from March-May 2012 identified strategies to influence parental and staff decisions regarding foods and beverages packed for each day of SDC. From these meetings, two intervention components were developed: 1) parent and staff education and 2) child and staff incentive program. Healthy eating education materials included a description of the HLC mission and procedures, a “Building a Better Lunchbox” guide to choosing foods and beverages that supports healthy eating standards (Figure 1) and tips on making recommended purchases at lower cost (Figure 1). The second component of the HLC was designed to influence parental decisions of foods and beverages purchased for SDC through child incentives, with the assumption that incentives would motivate children’s request for fruits, vegetables, and water to be packed daily. Children were informed about the HLC during daily assembly and/or by their group counselors. Points were tallied by SDC staff, within pre-determined groups (i.e. K-1st, 2nd –3rd) prior to morning snack (children brought food for the entire day) to ensure all possible points were given before snack consumption. To record points, staff asked children to show any fruits, vegetables, and water they had brought for the day. To account for varying group sizes, group points were tallied as total percentage for each category. A maximum of 3 points (i.e., 1 for fruits, 1 for vegetables, and 1 for water) were awarded regardless of the total number of items brought in any given category. Group points were displayed on a 4′×3′ marker board located at the check in/out area. Prizes were awarded to groups with the highest points at the end of each week. The NAA Healthy Eating Standards also emphasize the role staff play in nutrition promotion and modeling 4, therefore staff were also encouraged to participate in the HLC.
Figure 1.
HLC education materials consisting of double sided visual guide to “Building a Better Lunchbox”.
Process Evaluation Measures
Trained research staff conducted one, 30 minute training for SDC directors showing how to record, input, calculate, and display points daily. Technical support consisted of weekly communications and site visits where field notes were recorded to identify and resolve implementation errors, such as incomplete/missing recordings. Electronic recording forms provided to SDC directors enabled them to calculate age group percentages. Recording forms were evaluated weekly by trained research staff for accuracy. To quantify reach, trained research assistants spoke with parents throughout the study duration to evaluate the extent of their knowledge about the HLC. Staff were provided with written evaluation forms (developed by researchers) on the HLC (including discrete and open ended questions) following program completion.
Procedures
The HLC was initiated within the first two weeks of SDC. Each SDC program operated Monday through Friday (7:30am–6pm) for 11 weeks; with group observations took place during weeks 6–9. Each SDC site grouped children daily based on grade level. Based off of weekly camper enrollment, either multiple grade levels were combined (i.e., K-1, 2–3, 4–5) or each grade had its own designated group. Observation groups of children were randomly selected using a stratified sampling procedure, where subsamples of children were randomly selected from each designated grade-level, ensuring observation of the foods and beverages of at least 75% of the children in any given grade level. Two groups of trained data collectors observed four age groups across two SDC sites daily for 16 days. Trained research assistants recorded all food and beverage items brought to SDC by children and staff on an observation form developed from existing direct observation tools for the child-care centers and elementary schools 14, 15 and modified for SDC settings. Categories of foods and beverages (displayed in Table) were classified using existing protocol (i.e.; classification based on nutrient content of foods/beverages) 16 and modified for SDC settings. Children brought all of their foods and beverages for the day with them daily; therefore, trained research assistants recorded all items in each child’s lunchbox at the start of first snack (approximately 9am). Staff food and beverage items were recorded during each snack (morning and afternoon) and lunch time. Estimation of portion sizes in plastic bags and storage containers is unreliable 14; therefore, a child’s food was recorded as item present. For example, if a child brought 2 juice boxes, this was recorded as a child bringing a juice box (i.e., present). Primary outcomes of interest were the proportion of children and staff bringing fruits, vegetables, and water to SDC.
Table.
Percent Change in Food/Beverage Categories for Children (n=1,977) and Staff (n=241) from Baseline to Post-test.
|
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Category | Baseline | Staff Percentage
|
Baseline | Post | % Δ | (95CI) | K-1st | 2nd–3rd | 4th–5th | ||
| Post | % Δ | (95CI) | |||||||||
| Beverages | |||||||||||
| Soda/Pop*c | 3.4 | 1.4 | −2.0 | (−0.03 −0.01) | 10.0 | 3.6 | −6.4 | (− 0.14, 0.01) | −1.6% | −3.4% | −1.1% |
| Water*c | 46.6 | 60.2 | 13.5 | (0.06, 0.21) | 63.5 | 58.1 | −5.4 | (−0.22, 0.11) | 9.2% | 28.1% | 9.8% |
| Juice 100% | 3.5 | 4.5 | 1.0 | (−0.01, 0.03) | 1.6 | 3.3 | 1.6 | (−0.03, 0.01) | 0.6% | −0.3% | 3.2% |
| Juice other*c (non-100% juice, e.g. Capri Sun™, juice boxes) | 46.3 | 33.8 | −12.5 | (−0.19, −0.06) | 14.0 | 7.5 | −6.5 | (−0.16, 0.03) | −12.7% | −10.7% | −14.2% |
| Milk | 0.7 | 0.8 | 0.2 | (−0.01, 0.01) | 0.0 | 0.0 | -- | (-- --) | −0.6% | 1.6% | −0.5% |
| Sports Drink | 13.5 | 11.4 | −2.1 | (−0.06, 0.02) | 15.8 | 13.5 | −2.4 | (−0.13, 0.09) | −0.2% | −2.7% | −5.6% |
| Energy Drink | 0.3 | 1.2 | 0.9 | (−0.01, 0.02) | 0.0 | 0.0 | -- | (-- --) | 0.0% | 1.1% | 2.3% |
| Fruits and Vegetables | |||||||||||
| Vegetable*c,s | 4.6 | 15.6 | 10.9 | (0.07, 0.15) | 8.6 | 21.5 | 12.9 | (0.03, 0.23) | 6.1% | 11.5% | 17.1% |
| Fruit Fresh*c,s | 30.3 | 42.1 | 11.8 | (0.08, 0.16) | 29.8 | 47.4 | 17.5 | (0.02, 0.33) | 11.0% | 26.6% | 8.8% |
| Fruit Dried | 2.9 | 3.3 | 0.4 | (−0.02, 0.03) | 5.2 | 0.0 | −5.2 | (−0.02, 0.01) | −0.5% | 0.4% | 2.1% |
| Fruit Cup | 9.1 | 10.0 | 0.9 | (0.01, 0.01) | 4.2 | 6.4 | 2.2 | (−0.05, 0.09) | 1.9% | 2.6% | −3.8% |
| Apple Sauce | 8.0 | 9.2 | 1.1 | (−0.02, 0.04) | 4.8 | 2.5 | −2.3 | (−0.09, 0.05) | −1.2% | 2.6% | 1.2% |
| Sweeteners | |||||||||||
| Fruit Candy | 15.9 | 16.7 | 0.7 | (−0.03, 0.05) | 4.3 | 2.2 | −2.1 | (−0.07, 0.03) | 0.3% | 1.6% | −1.2% |
| Cereal*c | 1.9 | 4.1 | 2.2 | (0.00, 0.04) | 3.4 | 0.6 | −2.8 | (−0.07, 0.01) | −0.5% | 4.3% | 4.3% |
| Granola/cereal bar | 13.2 | 15.4 | 2.2 | (−0.02, 0.06) | 3.6 | 25.5 | 21.8 | (−0.10, 0.17) | −4.0% | 5.3% | 5.9% |
| Candy bar*c | 5.6 | 3.9 | −1.7 | (−0.03, 0.00) | 2.0 | 1.3 | −0.7 | (−0.04, 0.03) | −0.8% | −1.9% | −4.8% |
| Cookie | 24.8 | 22.2 | −2.6 | (−0.07, 0.02) | 10.5 | 7.9 | −2.6 | (−0.13, 0.07) | −6.6% | 1.6% | 0.0% |
| Pastries | 15.0 | 9.9 | −5.1 | (−0.09, 0.01) | 10.3 | 9.2 | −1.1 | (−0.12, 0.10) | −1.3% | −7.8% | −7.5% |
| Other Dessert | 9.4 | 8.7 | −0.7 | (−0.04, 0.02) | 5.9 | 1.4 | −4.5 | (−0.10, 0.02) | −1.0% | 3.3% | −6.4% |
| Salty Foods | |||||||||||
| Cracker*s | 25.2 | 30.3 | 5.2 | (−0.01, 0.11) | 12.4 | 27.4 | 15.0 | (0.03, 0.27) | 7.6% | 12.6% | −6.2% |
| Popcorn | 3.1 | 2.4 | −0.7 | (−0.03, 0.01) | 4.3 | 1.7 | −2.6 | (−0.08, 0.02) | −0.1% | −0.5% | −2.6% |
| Chips*c,s | 55.4 | 40.7 | −14.7 | (−0.21, −0.09) | 48.0 | 17.5 | −30.5 | (−0.46, −0.15) | −13.8% | −11.2% | −8.2% |
| Added “visible” fats | |||||||||||
| Dips*s | 4.0 | 6.6 | 2.5 | (0.00, 0.05) | 2.4 | 13.5 | 11.0 | (0.03, 0.12) | 2.8% | 3.3% | 2.3% |
| Dairy | |||||||||||
| Cheese*c | 5.7 | 9.3 | 3.5 | (0.00, 0.07) | 2.1 | 4.1 | 2.0 | (−0.03, 0.07) | 3.4% | 3.5% | 3.3% |
| Yogurt*c | 5.8 | 9.8 | 4.0 | (0.00, 0.08) | 2.6 | 8.7 | 6.1 | (−0.01, 0.13) | 5.5% | 0.5% | 4.5% |
| Pre-packaged Foods | |||||||||||
| Fast food*c | 7.6 | 3.4 | −4.3 | (−0.08, 0.00) | 9.0 | 7.9 | −1.1 | (−0.11, 0.08) | −2.9% | −3.3% | −6.6% |
| Lunchable™ | 17.0 | 16.9 | −0.1 | (−0.04, 0.04) | 4.1 | 4.9 | 0.8 | (−0.05, 0.07) | 0.8% | −3.4% | 4.3% |
| Sandwiches | |||||||||||
| Brown bread with meat*s | 5.3 | 7.1 | 1.7 | (−0.01, 0.05) | 0.1 | 10.4 | 10.5 | (0.05, 0.16) | 0.8% | 2.8% | 1.4% |
| White bread with meat | 18.9 | 15.4 | −3.6 | (−0.08, 0.01) | 17.1 | 6.3 | −10.8 | (−0.22, 0.00) | −9.5% | 4.0% | −2.4% |
| Brown bread non-meat | 7.4 | 8.0 | 0.5 | (−0.03, 0.04) | 5.7 | 3.5 | −2.2 | (−0.07, 0.03) | −5.8% | 4.8% | 5.2% |
| White bread non-meat | 19.0 | 14.9 | −4.1 | (−0.08, 0.00) | 3 .0 | 5.9 | 2.9 | (−0.04, 0.09) | 1.2% | −5.6% | −5.5% |
| Meat sandwich (bread type not provided) | -- | -- | -- | (-- --) | 9.3 | 8.1 | −1.2 | (−0.10, 0.07) | -- | -- | -- |
| Non-meat sandwich*s (bread type not provided) | -- | -- | -- | (-- --) | 11.6 | 2.6 | −9.0 | (−0.17, −0.01) | -- | -- | -- |
| Nuts | -- | -- | -- | (-- --) | 0.6 | -- | -- | (-- --) | -- | -- | -- |
| Coffee | -- | -- | -- | (-- --) | 0.6 | 0.0 | −0.6 | (−0.02, 0.01) | -- | -- | -- |
| Other (pasta, eggs) *c,s | 16.3 | 13.1 | −3.3 | (−0.04, −0.02) | 14.1 | 27.5 | 13.4 | (0.02, 0.25) | −9.0% | 4.7 | 0.8 |
indicates significant changes (p < .05) in the percentage of children bringing food/beverages from baseline to post-assessment determined mixed effects regression
indicates significant changes (p < .05) in the percentage of staff bringing food/beverages from baseline to post-assessment determined mixed effects regression
Inter-Observer Reliability
Observers received a two hour classroom training to become familiarized with data collection protocol/operational definitions and 8 field-based trainings to practice food and beverage assessments. Inter-observer reliability of categories was estimated using weighted kappa (κw) and percent agreement. Percent agreement ranged from 77% to 100% (median 91%) and κw ranged from 0.22 to 1.00 (median 0.66) across all food and beverage categories. For the primary outcomes of fruit, vegetables, and water, percent agreement ranged from 94% to 97% and κw ranged from 0.71 to 0.87, indicating a high level of inter-observer reliability. Low κw or percent agreement were due to the limited occurrence (< 5% of observations) of specific food and beverages observed (e.g., meat sandwiches on brown bread, milk).
Statistical Analysis
Snack category percentages [(food type/total staff or total children)*100] were calculated separately for children and staff for baseline and post assessment and were compared through a mixed-effects regression model. Data was analyzed using STATA/SE 11.0 (College Station, TX).
RESULTS
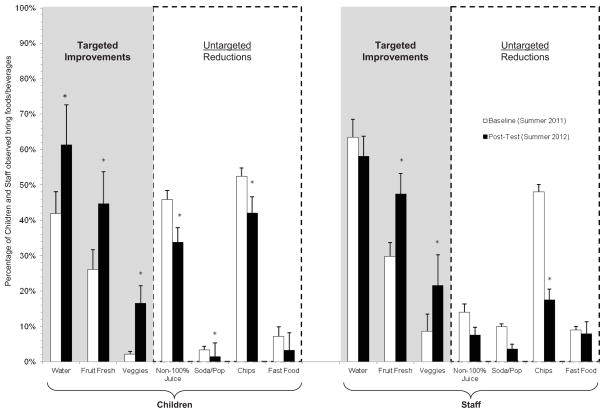
A total of 1,977 children and 241 staff were observed over 43 days across 4 sites. An average of 20.4 (range 6 to 43) children and 3.0 (range 1 to 7) staff were observed for a single group. Outcomes from the mixed-effects regression model for all foods and beverages observed for children (K-5th) and staff are presented in Table below. For children, there were improvements in each of the main outcomes of interest, with a 12% increase in amount of fresh fruit (p = 0.00) being brought to SDC from baseline to post-test, an 11% increase in vegetables (p = 0.00) and a 14% increase in water (p = 0.00). Although not directly targeted by the HLC, significant decreases were seen in several low-nutrient-dense foods and beverages with a 15% decrease in chips (p = 0.00) brought to SDC by children, as well as a 13% decrease in non-100% fruit juices (p = 0.00). A secondary analysis yielded some variance in percent change of food and beverage categories across age groupings, however, the direction and magnitude of change for all primary outcomes of interest remained constant (Table).
For staff, increases were seen for fruits and vegetables brought to SDC. An 18% increase in fruits (p = 0.03) was observed from baseline to post-test and a 13% increase in vegetables (p = 0.03). There was a 5% decrease in the percentage of water brought by staff; however this was not statistically significant. Observations showed a significant decrease of 31% in chips (p = 0.00) brought to SDC by staff and a 6.4% decrease in soda (p = 0.08). Targeted improvements and untargeted reductions from baseline to post-test are shown in Figure 2.
Figure 2.
Targeted improvements and untargeted reductions from baseline to post-test.
*Indicates significant changes (p < .05) in the percentage of children and/or staff bringing food/beverages from baseline to post-assessment
Process Evaluation
Of the 243 parent contacts, 69% of parents were aware of the HLC. Weekly percentages indicating awareness of the HLC ranged from 48% (week 1) to 97% (week 5). Staff surveys indicated they were informed/trained on the HLC and that the majority of staff reported wanting to be good role models and were actively involved in the HLC. Seventy percent of staff felt children were interested in the HLC; however, common explanations given for the lack of interest by children were that the prizes (e.g., lunchbox shaped pins with “HLC” initials) were not motivating, or that some age groups (e.g., K, 1st) were too young to understand and be interested in the challenge. Staff felt the HLC challenge encouraged them to bring healthier foods and beverages and that they felt more energetic after doing so. The most common responses when asked for suggestions for future HLC improvements were to: 1) add additional prizes, 2) add more food types (e.g., whole grains) that count toward points and 3) increase parental involvement. In addition to recording/reporting inconsistencies observed by researchers, some SDC staff also reported the lack of uniformity in awarding prizes.
DISCUSSION
The increases seen in fruits and vegetables along with decreases in non-recommended foods for both children and staff are consistent with concepts of the BCT 17–20. Findings suggest there were substitutions of non-recommended foods and beverages for those that were recommended (e.g., fruit or vegetables for chips). While the percentage of staff that brought water on a daily basis decreased, so did other beverages. In fact, decreases were seen in all beverages other than 100% fruit juice from baseline to post-test for staff. Decreases in each beverage category indicate that staff were not consuming beverages in front of children as often as seen at baseline; therefore, refraining from drinking non-recommended beverages shows positive changes in role modeling behaviors.
This study is the first to implement and evaluate a SDC program aimed at meeting benchmarks set forth by the NAA Healthy Eating Standards. Other studies targeting food choice behaviors of parents in regards to their children have shown minor success8. While previous studies targeted parents through direct communication or handouts, they lacked the incentive based program, like the one described herein, aimed at motivating children to request healthier foods and beverages. Incentives were intended to provide continuous exposure to messages regarding the importance of packing recommended foods and beverages and to create an atmosphere where children were motivated to bring these items to receive recognition. Child motivation, coupled with parental education, was potentially the driving force of parental decisions to pack healthier foods and beverages.
Strengths of this study include the community-based participatory approach, integration of the program into the normal SDC routine, use of existing parent communication methods, collection of a large number of foods and beverages, use of direct observation and the extensive time frame of daily observations (i.e., ensuring that each snack/meal was observed), sample size, and theoretical foundation to the HLC. Additionally, the use of multiple process evaluation measures allowed for recording of program implementation and participant reach. Study limitations include the lack of a control group and the minimal direct contact with parents who inevitably purchase foods and beverages for their child. However, results from this current study indicate that existing resources (i.e., newsletters, HLC board display) used to inform parents were largely successful. Plus, this amount of contact is realistic based on the amount of interaction SDCs have with parents. The current study did not measure consumption; therefore there is no knowledge of the actual fruit, vegetable, and water intake. Future studies should explore tracking consumption of these foods and beverages. Finally, only four SDC sites were used in this study, potentially limiting generalizability.
IMPLICATIONS FOR RESEARCH AND PRACTICE
This study demonstrated that implementation of the HLC components is feasible for the SDC setting and can result in sizable increases in fruit, vegetable, and water brought to SDC. Consistent with BCT, this approach has potential to decrease non-recommended foods (e.g., sugar sweetened beverages, salty snacks) through untargeted substitutions. Findings from the present study have important implications for SDCs and other child-care settings where there is minimal control over the foods brought on site.
First, the HLC is a low-cost program requiring minimal resources. Total cost for HLC materials was approximately $450 per site. Sites were free to choose their own incentives and decided to design/purchase ($200 per site) HLC pins for awards; however, suggestions of potential free of cost incentives were given, such as, extra swim time, “spirit sticks”, and recognition during assembly. Other costs ($250 per site) included materials to display HLC points (e.g., marker board, easels). Given that each site had free access to a printer, printing cost for HLC recorder forms/parent newsletters were not included in the total cost, yet these additional costs may need to be considered for future studies.
Secondly, the HLC was effective at increasing the amount of fruits, vegetables, and water brought to SDC by children despite some inconsistencies with implementation, suggesting potential for larger increases in healthier foods and beverages when the program is implemented as intended. SDC leaders have the potential to improve implementation of the HLC by overseeing staff to ensure that the HLC is incorporated into daily routines. With over 14 million children attending SDCs, introduction of the HLC can serve as a way to influence the eating habits of children during the summer.
In conclusion, the HLC improved the percentage of children bringing fruits, vegetables, and water to SDC, while decreasing the amount of some low-nutrient-dense foods. Thus, the HLC represents a low-cost method to influence the dietary behaviors of children in SDCs. Future evaluations of the HLC should explore additional modes of parental communication such texting and social networking, as well as, staff perceived barriers to program implementation. Further dissemination of the HLC is needed to determine its effectiveness in other child care settings.
Acknowledgments
We would like to extend our appreciation to the Summer Day Camp staff, children, and parents that made this study possible.
Funding: The project described was supported by Award Number R21HL106020 from the National Heart, Lung, And Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, And Blood Institute or the National Institutes of Health
Footnotes
Potential conflicts of interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.von Hippel PT, Powell B, Downey DB, Rowland NJ. The effect of school on overweight in childhood: gain in body mass index during the school year and during summer vacation. Am J Public Health. 2007 Apr;97:696–702. doi: 10.2105/AJPH.2005.080754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gillis L, McDowell M, Bar-Or O. Relationship between summer vacation weight gain and lack of success in a pediatric weight control program. Eat Behav. 2005 Feb;6:137–143. doi: 10.1016/j.eatbeh.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 3.America After 3PM Special Report on Summer. [Accessed April 16, 2013.];Afterschool Alliance. http://www.afterschoolalliance.org/documents/Special_Report_on_Summer_052510.pdf. Published 2010.
- 4.National Afterschool Association Standards for Healthy Eating and Physical Activity. National Afterschool Association; [Accessed April 16, 2013.]. http://www.niost.org/pdf/host/Healthy_Eating_and_Physical_Activity_Standards.pdf. Published 2011. [Google Scholar]
- 5.Ellnson L, Bethel J, Deak MA, Li S, Milfort R, Caperna K, et al. Evaluation of the Summer Food Service Program Enhancement Demonstrations: 2011 Demonstration Evaluation Report Prepared by Westat under Contract No. GS-23F-8144H. Alexandria, VA: United States Deparment of Agriculture, Food and Nutrition Service; Published November 2012. [Google Scholar]
- 6.USDA. [Accessed 9/5/2012];National School Lunch Program. 2012 http://www.fns.usda.gov/cnd/Lunch/AboutLunch/NSLPFactSheet.pdf. Published 2012.
- 7.Sweitzer SJBM, Roberts-Gray C. Do snack lunches provided by parents meet the nutritional needs of young children who attend childcare? J Am Diet Assoc. 2009;109:141–144. doi: 10.1016/j.jada.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 8.Sweitzer SJ, Briley ME, Roberts-Gray C, Hoelscher DM, Harrist RB, Staskel DME, et al. Lunch is in the bag: increasing fruits, vegetables, and whole grains in sack lunches of preschool-aged children. J Am Diet Assoc. 2010 Jul;110:1058–1064. doi: 10.1016/j.jada.2010.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peterson S. [Accessed 9/11, 2012];The Lunch Box Program-Packing healthy take-along lunches for preschool children, USDA Land-Grant Success Stories in Competency Training: Cooperative State Research, Education and Extension service. http://www.csrees.usda.gov/nea/family/sri/child_sri_competencies.html. Published 2009.
- 10.Bickel WKVR. Reframing health behavior change with behavioral economics. New Jersey: Lawrence Erlbaum Associates, Inc; 2000. [Google Scholar]
- 11.Locke EA, Latham GP. New directions in goal-setting theory. Curr Dir Psychol SCI. 2006;15:265–268. [Google Scholar]
- 12.Spring BSK, McFadden HG, Vaughn J, Kozak AT, Smith M, Moller AC, Epstein L, et al. Make Better Choices (MBC): Study design of a randomized controlled trial testing optimal technology-supported change in multiple diet and physical activity risk behaviors. BMC Publich Health. 2010;10:586. doi: 10.1186/1471-2458-10-586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spring BSK, McFadden HG, Vaughn J, Kozak AT, Smith M, Moller AC, et al. Multiple Behavior Changes in Diet and Physical Activity. Arch Intern Med. 2012:172. doi: 10.1001/archinternmed.2012.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ball SCBS, Ward DS. Development and reliability of an observation method to assess food intake of young children in child-care. J Am Diet Assoc. 2007;107:656–661. doi: 10.1016/j.jada.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Economos CDSJ, Sacheck JM, Chui K, Kwan Ho, Irizarry L, Guillemont J, Collins JJ, et al. School-based behavioral assessment tools are reliable and valid for measurement of fruit and vegetable intake, physical activity, and television viewing in young children. J Am Diet Assoc. 2008;108:695–701. doi: 10.1016/j.jada.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 16.Mozaffarian RS, Wiecha JL, Roth BA, Nelson TF, Lee RM, Gortmaker SL. Impact of Organizational Intervention Designed to Improve Snack and Beverage Quality in YMCA After-School Programs. Am J Public Health. 2009;100:925–932. doi: 10.2105/AJPH.2008.158907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwartz M. The Influence of a Verbal Prompt on School Lunch Fruit Consumption: A Pilot Study. IJBNPA. 2007;4:5. doi: 10.1186/1479-5868-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Just DR, Mancino L, Wansink B. Could Behavioral Economics Help Improve Diet Quality for Nutrition Assistance Participants. USDA-ERS Economic Research Services; [Accessed October 24, 2013.]. http://www.ers.usda.gov/media/196724/err43_reportsummary_1_.pdf. Pubished 2007. [Google Scholar]
- 19.French SA, Stables G. Environmental interventions to promote vegetable and fruit consumption among youth in school settings. Prev Med. 2003;37:593–610. doi: 10.1016/j.ypmed.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 20.Noble C, Corney M, Eves A, Kipps M, Lumbers M. Food choice and secondary school meals: The nutritional implications of choices based on preference rather than perceived healthiness. Int J Hosp Manage. 2003;22:197–215. [Google Scholar]