CASE PRESENTATION
A 53-year-old man admitted for stem cell transplantation in the context of acute myeloid leukemia was referred for gastric content leakage from a persistent gastrocutaneous fistula. A percutaneous endoscopic gastrostomy (PEG) tube had been placed for four months due to suboptimal nutrition. The PEG tube was subsequently removed due to improvement in caloric intake and nutritional status. Unfortunately, drainage of gastric contents (approximately 250 mL/day) from the gastrocutaneous fistula after removal of the PEG tube persisted. This led to peristomal skin maceration and breakdown resulting in local cutaneous bleeding from the PEG tube site. Despite conservative management with bowel rest, proton pump inhibitor therapy, wound care and parenteral nutrition, drainage and bleeding from the gastrocutaneous fistula site persisted. The remainder of his medical history was noncontributory. Physical examination using subjective global assessment revealed a hemodynamically stable man with adequate nutritional status, without any examination or laboratory contraindications to endoscopy. Informed consent was obtained to proceed with an attempt to close the gastrocutaneous fistula via endoscopic hemoclips before considering surgical closure.
During endoscopy, the opening of the fistula was identified in the antrum (Figure 1). Single-modality therapy was used and three hemoclips were placed in an attempt to close the fistula site (Figure 2). A stoma bag was placed over the pre-existing fistula site; no air leakage was observed at the time of endoscopy. The fistula tract closed within 24 h after the procedure with no further leakage noted.
Figure 1).
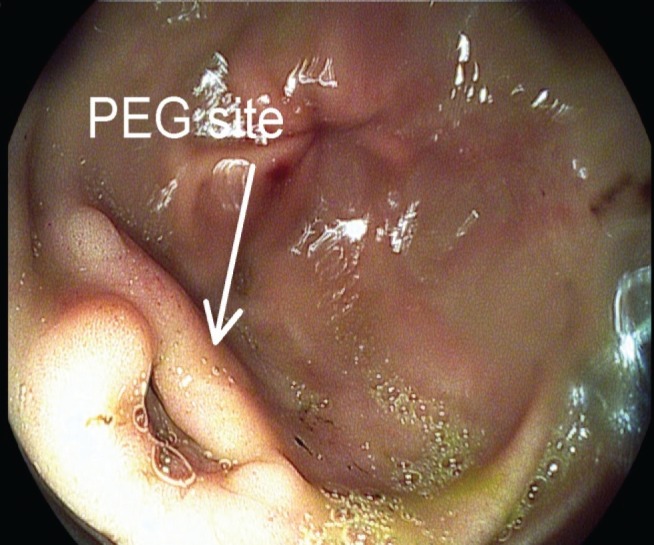
Fistula opening identified in the antrum. PEG Percutaneous endoscopic gastrostomy
Figure 2).
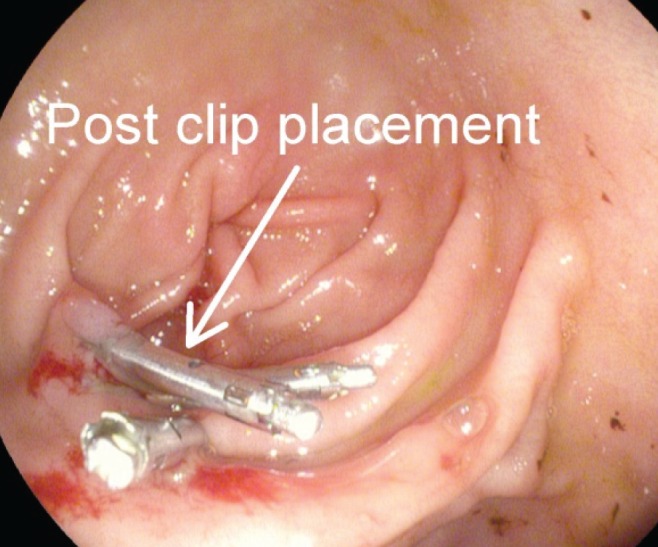
Hemoclip placement at the fistula site
The patient was closely followed over the ensuing week. Daily clinical assessments were conducted and no evidence of gastric content was noted at the previous fistula site. The patient was kept nil per os for three days and proton pump inhibitor therapy was continued. His diet was then advanced. The lack of gastric output from the fistula tract postendoclip placement, even after the initiation of oral feeds, confirmed the successful outcome of the procedure (Figure 3).
Figure 3).

Nil output in the stoma bag three days after initiation of feeds confirming the success of the procedure
DISCUSSION
PEG tube insertion is a common intervention for providing intermediate and long-term nutritional and hydration support when oral feeds are suboptimal (1,2). After removal of PEG tubes, the communication between the stomach and the skin traditionally closes within hours to days.
Persistent gastrocutaneous fistula after removal of PEG tubes is an unusual complication observed in approximately 24% to 34% of patients (2). The most important predictive factor for persistent gastrocutaneous fistula appears to be the length of time the tube is in place before its removal (3). Although the precise mechanism in the formation of persistent gastrocutaneous fistulas is not well established, it is postulated that it may be the result of epithelialization of the fistula tract (3). Several factors, such as delayed gastric emptying, poor wound healing, flow of gastric contents through the fistula and medication, may also affect healing of the fistula tract. Conservative management of these fistulas includes medications aimed at increasing gastric emptying with promotility agents and increasing gastric pH with proton pump inhibitors, although these are rarely effective in facilitating closure. The standard treatment approach for fistulas is surgical closure; however, most of the patients in this population are poor surgical candidates secondary to their underlying comorbid conditions (3). Other nonsurgical procedures that have been used with variable success include electric and chemical cauterization, argon plasma coagulation, endoscopic suturing, collagen plugs and fibrin glue (4,5).
Use of hemoclips as a therapeutic intervention for control of gastrointestinal bleeding was first described more than 30 years ago. Hemoclips have subsequently evolved and improved, allowing for a wide variety of indications (3–5). To our knowledge, successful closure of persistent gastrocutaneous fistula using hemoclips has only been described twice in the literature, but all in combination with the use of thermocoagulation in an attempt to de-epithelialize the fistula tract.
The present report is the first to document endoscopic closure of a gastrocutaneous fistula solely with hemoclips. The present case suggests that endoscopic clip closure of a nonhealing gastrocutaneous fistula is feasible without the application of thermocoagulation. Gastroenterologists should be aware of this straightforward solution because it may help avoid surgical intervention in an otherwise high-risk patient population.
The Canadian Journal of Gastroenterology is considering a limited number of submissions for IMAGE OF THE MONTH. These are based on endoscopic, histological, radiological and/or patient images, which must be anonymous with no identifying features visible. The patient must consent to publication and the consent must be submitted with the manuscript. All manuscripts should be practical and relevant to clinical practice, and not simply a case report of an esoteric condition. The text should be brief, structured as CASE PRESENTATION and DISCUSSION, and not more than 700 words in length. A maximum of three images can be submitted and the number of references should not exceed five. The submission may be edited by our editorial team.
REFERENCES
- 1.Janik TA, Hendrickson RJ, Janik JS, Landholm AE. Analysis of factors affecting the spontaneous closure of a gastrocutaneous fistula. J Pediatr Surg. 2004;39:1197–9. doi: 10.1016/j.jpedsurg.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 2.Kobak GE, McClenathan DT, Schurman SJ. Complications of removing percutaneous endoscopic gastrostomy tubes in children. J Pediatr Gastroenterol Nutr. 2000;30:404–7. doi: 10.1097/00005176-200004000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Siddiqui AA, Kowalski T, Cohen S. Closure of a nonhealing gastrocutaneous fistula using an endoscopic clip. South Med J. 2007;100:75–6. doi: 10.1097/SMJ.0b013e31802f86a2. [DOI] [PubMed] [Google Scholar]
- 4.Kalim S, Hameed H. Closure of a nonhealing gastrocutaneous fistula using argon plasma coagulation and endoscopic hemoclips. Can J Gastroenterol. 2009;23:217–9. doi: 10.1155/2009/973206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teitelbaum JE, Gorcey SA, Fox VL. Combined endoscopic cautery and clip closure of chronic gastrocutaneous fistulas. Gastrointest Endosc. 2005;62:432–5. doi: 10.1016/j.gie.2005.04.047. [DOI] [PubMed] [Google Scholar]


