Abstract
Postprandial reactive hypoglycemia, early satiety and diarrhea are well-recognized side effects following full or partial gastrectomy or gastric bypass. It has only recently been realized, however, that patients with normal gastric anatomy may experience similar symptoms and signs due to primary accelerated gastric emptying (Middleton syndrome). In previous case studies, patients responded well to the use of dietary modification (frequent small-volume meals) alone. The authors describe two patients with this syndrome who continued to experience symptoms of reactive postprandial hypoglycemia despite dietary intervention but became asymptomatic following the addition of the alpha-glucosidase inhibitor acarbose.
Keywords: Diarrhea, Dumping syndrome, Gastric emptying, Gastric motility, Hypoglycemia
Abstract
L’hypoglycémie réactive postprandiale, la satiété précoce et la diarrhée sont des effets secondaires bien connus de la gastrectomie partielle et du pontage gastrique. Toutefois, on s’est rendu compte récemment que les patients ayant une anatomie gastrique normale peuvent présenter des signes et symptômes similaires en raison d’une vidange gastrique accélérée (syndrome de Middleton). Dans les études de cas précédentes, les patients répondaient bien à une simple modification du régime (des repas fréquents à petit volume). Les auteurs décrivent le cas de deux patients atteints de ce syndrome qui ont continué de présenter des symptômes d’hypoglycémie réactive postprandiale malgré une intervention diététique, mais qui sont devenus asymptomatiques après l’ajout d’acarbose, un inhibiteur de l’alpha-glucosidase.
Gastric bypass or resection for morbid obesity or malignancy are well-recognized causes of early satiety, diarrhea and postprandial reactive hypoglycemia due to the rapid entry of nutrients into the small intestine. In contrast, the association of identical signs and symptoms, including reactive hypoglycemia with normal gastric anatomy but accelerated gastric emptying, has only recently been recognized. Middleton et al (1) initially reported this association as a case report; subsequently, a more detailed description of the syndrome was provided in a series of six patients (2). In both of these publications, most patient’s symptoms were adequately controlled through dietary modification (introduction of small frequent meals). The present article describes two patients with this syndrome who remained symptomatic following dietary modification but responded well to the introduction of the alpha-glucosidase inhibitor acarbose.
Case 1
A 53-year-old Caucasian woman presented with a two-year history of diarrhea. She had experienced constipation since childhood. Associated symptoms included abdominal distension approximately 30 min after eating, which was often accompanied by diarrhea. She reported severe fatigue, cognitive impairment, weakness, tremor and dizziness approximately 2 h to 3h after eating. During such an episode, she also experienced syncope that was followed by transient memory loss. She reported no allergies, was a nonsmoker and consumed approximately 20 units of alcohol per week. Her only medication was fluoxetine for depression. Physical examination was unremarkable and there was no evidence of an autonomic neuropathy. Routine laboratory tests, including tissue transglutaminase, short synacthen test, thyroid function, urinary 5-hydroxy-indole-acetic acid and van-illylmandelic acid were normal. Similarly, no abnormalities were found on additional investigations including colonoscopy, 23-Seleno-25-homo-tauro-cholate (SeHCAT) retention study and glucose hydrogen breath test. Scintigraphic whole gut transit time using indium diethylenetriaminepentaacetic acid in water (3), revealed rapid gastric emptying with only 9% of liquid remaining in the stomach at 26 min. An extended oral glucose tolerance test with a standard 75 g glucose load (4) demonstrated an appropriate rise in glucose level and return to baseline at 60 min but a subsequent fall to 2.8 mmol/L at 120 min at which time her hypoglycemic symptoms occurred (Figure 1). A diagnosis of idiopathic accelerated gastric emptying and reactive hypoglycemia was made. She was treated with a ‘grazing diet’ (eating regular small meals), which settled her diarrhea symptoms but the hypoglycemic symptoms did not resolve. She was given acarbose 50 mg twice per day before her two main meals, with near complete resolution of symptoms.
Figure 1).
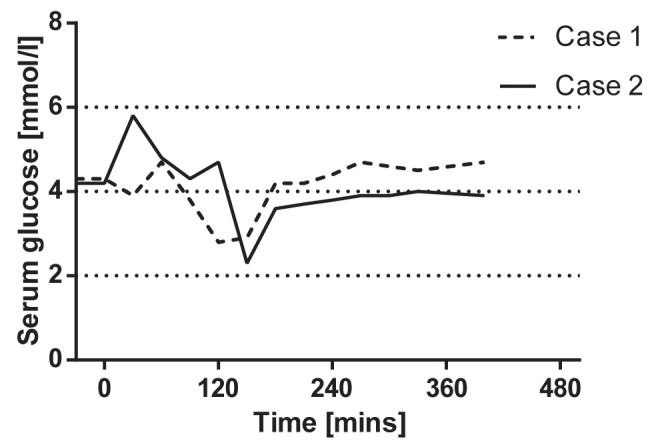
Results of an extended glucose tolerance test, using a standard 75 g glucose load. In both patients, an appropriate rise in serum glucose and return to baseline in 30 min was apparent. However, both exhibited a subsequent fall corresponding to the onset of symptoms
Case 2
A 26-year-old woman presented with abdominal discomfort and diarrhea in the postprandial period followed by severe debilitating tired-ness when she would often fall asleep. This was frequently associated with nausea and malaise. She took no alcohol, was a nonsmoker and was receiving thyroxine replacement therapy. Physical examination was unremarkable and there were no signs of autonomic neuropathy. Routine laboratory blood tests, thyroid function, duodenal and colonic biopsies, a short synacthen test and a SeHCAT retention study were normal. Fasting gut hormone levels, glucose hydrogen breath test, video capsule endoscopy, abdominal computed tomography scan and fecal elastase were also normal. A scintigraphic solid-phase gastric emptying (5) study revealed accelerated gastric emptying with a half emptying time of 26 min. An extended glucose tolerance test with a standard 75 g glucose load demonstrated an appropriate rise in serum glucose and return to baseline in 30 min but a subsequent fall to 2.3 mmol/L at 150 min, at which time her hypoglycemic symptoms occurred (Figure 1). A diagnosis of primary accelerated gastric emptying was made and she was advised to adhere to a ‘grazing diet’. This dietary approach settled her symptoms of diarrhea but did not resolve the hypoglycemic symptoms. She was, therefore, given acarbose 50 mg before her main meals two or three times per day, which resulted in a near complete resolution of symptoms, with only mild fatigue occurring after a large meal.
DISCUSSION
Motility disorders of the gastrointestinal tract are not easily identified by their associated symptoms (6), which can consequently lead to delays in diagnosis. A study involving 649 consecutive patients who underwent scintgraphic gastric emptying studies (7) reported that in patients with suspected accelerated gastric emptying on clinical grounds, this was confirmed in 69%, but 7% demonstrated delayed gastric emptying. Of patients suspected to have gastroparesis, only 29% were found to demonstrate delayed gastric emptying on scintigraphic testing and 23% had accelerated gastric emptying. This study implies that the clinical diagnosis of gastric dysmotility is difficult because symptoms do not reliably reflect the underlying nature of the motility disorder, and symptoms believed to indicate gastroparesis may be caused by accelerated gastric emptying.
Early satiety, postprandial diarrhea and subsequent hypoglycemic symptoms, such as nausea, fatigue, sweating and cognitive impairment, should lead the clinician to consider the diagnosis of ‘Middleton syndrome’, in which the primary abnormality is accelerated gastric emptying. Symptoms usually respond well to dietary intervention but, as described in the present report, may occasionally require additional treatment with an alpha-glucosidase inhibitor, such as acarbose, to resolve refractory hypoglycemic symptoms.
REFERENCES
- 1.Middleton SJ, Balan K. Post-prandial reactive hypoglycaemia and diarrhea caused by idiopathic accelerated gastric emptying: A case report. J Med Case Rep. 2011;5:177. doi: 10.1186/1752-1947-5-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Middleton SJ, Balan K. Idiopathic accelerated gastric emptying presenting in adults with post-prandial diarrhea and reactive hypoglycemia: A case series. J Med Case Rep. 2012;6:132. doi: 10.1186/1752-1947-6-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sørensen M, Johansen OE. Idiopathic reactive hypoglycaemia – prevalence and effect of fibre on glucose excursions. Scand J Clin Lab Invest. 2010;70:385–91. doi: 10.3109/00365513.2010.491869. [DOI] [PubMed] [Google Scholar]
- 4.Bonapace ES, Maurer AH, Davidoff S, Krevsky B, Fisher RS, Parkman HP. Whole gut transit scintigraphy in the clinical evaluation of patients with upper and lower gastrointestinal symptoms. Am J Gastroenterol. 2000;95:2838–47. doi: 10.1111/j.1572-0241.2000.03195.x. [DOI] [PubMed] [Google Scholar]
- 5.Malmud LS, Fisher RS, Knight LC, Rock E. Scintigraphic evaluation of gastric emptying. Seminar Nuclear Med. 1982;12:116–25. doi: 10.1016/s0001-2998(82)80003-2. [DOI] [PubMed] [Google Scholar]
- 6.Balan K, Alwis L, Sonoda LI, Pawaroo D, Parry-Jones DR, Middleton S. Utility of whole gut transit scintigraphy in patients with chronic gastrointestinal symptoms. Nucl Med Commun. 2010;31:328–33. doi: 10.1097/MNM.0b013e328335e5a9. [DOI] [PubMed] [Google Scholar]
- 7.Balan K, Sonoda LI, Seshadri N, Solanki C, Middleton S. Clinical significance of scintigraphic rapid gastric emptying. Nucl Med Commun. 2011;32:1185–9. doi: 10.1097/MNM.0b013e32834bf262. [DOI] [PubMed] [Google Scholar]


