Abstract
Racial and ethnic minorities suffer disproportionately from diabetes-related morbidity and mortality. With the creation of Accountable Care Organizations (ACOs) under the Affordable Care Act, healthcare organizations may have an increased motivation to implement interventions that collaborate with community resources and organizations. As a result, there will be an increasing need for evidence-based strategies that integrate healthcare and community components to reduce diabetes disparities. This paper summarizes the types of community/health system partnerships that have been implemented over the past several years to improve minority health and reduce disparities among racial/ethnic minorities and describes the components that are most commonly integrated. In addition, we provide our recommendations for creating stronger healthcare and community partnerships through enhanced community support.
Keywords: diabetes, disparities, integration, community, health systems, healthcare, quality improvement, patient education, culturally-tailored, providers, care coordination, interventions
Introduction
Racial/ethnic minorities continue to experience diabetes-related morbidity and mortality that is 50–100% higher than among whites [1]. Of all African-American adults, 12.6% have been diagnosed with diabetes compared to 7.1% of all non-Hispanic Whites. Minorities experience greater rates of hospitalization due to diabetes-related complications, such as end-stage renal disease (ESRD), diabetic retinopathy, and lower-extremity amputations [2–3].
In order to effectively address the variety of factors that contribute to health disparities among racial/ethnic minorities (e.g. cultural practices, social determinants, economic inequalities, access to health care), interventions will need to utilize multi-factorial approaches [4]. Research has shown that culturally-tailored initiatives that involve community/health system collaborations to improve disease management, reduce health disparities and improve health outcomes are well-suited to reduce the burden of disease among underserved populations [2, 5–6]. This is particularly true for diabetes because the decisions impacting diabetes self-management, including the importance of healthy diet and regular physical activity, are influenced greatly by the infrastructure and support available in the community.
In addition, as a result of the Affordable Care Act, healthcare organizations may have incentives to make population-centered health a priority and form collaborations with clinics, providers, and other health services professionals in the public health, community and social services sectors, to expand the impact of health systems, promote quality in health care, and control health costs in order to reduce the burden of chronic disease and improve health outcomes [1, 7]. As the burden of chronic disease increases among racial/ethnic minority populations over time, the need for evidence-based interventions that address diabetes management in both healthcare and community settings will parallel each other in importance. In this paper, we will discuss current research on the strategies implemented in diabetes disparities interventions that integrate healthcare and community components. While not a systematic review, our paper provides a summary of some of the key literature published in the past several years in this field, and describes the major themes that have emerged in the literature on ways that healthcare and community interventions are integrated.
Methods
We searched the PubMed database using combinations of the following keywords: diabetes, disparities, community, minorities, health system, healthcare, clinics, providers, medical center, community health worker, promotoras, promotores, community health advisors, peer, partners, partnership, care management, care coordination, integration and culturally tailored. We primarily included papers published from 2010 to 2013 to highlight the current state of the field. We included only interventions that specifically integrated healthcare and community components to address diabetes disparities among adults.
We did not include community health worker interventions that included provider referrals as their only linkage to the healthcare system, nor did we include patient education by clinicians if they occurred in community settings without direct linkages to health care delivery. And although there exists a growing number of interventions that use technology to connect with patients while at home (e.g. telemedicine, mobile phone technology, patient portals), we did not include these programs in our definition of ‘community linkages’. Finally, we did not include interventions that focused on diabetes prevention (e.g. the Diabetes Prevention Program translated to community settings), despite the public health and economic importance of preventing diabetes, particularly within racial/ethnic minority communities.
We describe common strategies implemented in integrated interventions, including patient education, clinician involvement, and quality improvement/health systems change and provide examples of the ways in which they integrated healthcare with community components. In addition, we provide our recommendations for creating stronger healthcare and community partnerships through enhanced community support. We have created a conceptual model that shows how various health system components are integrated with community organizations and resources (Figure 1).
Figure.
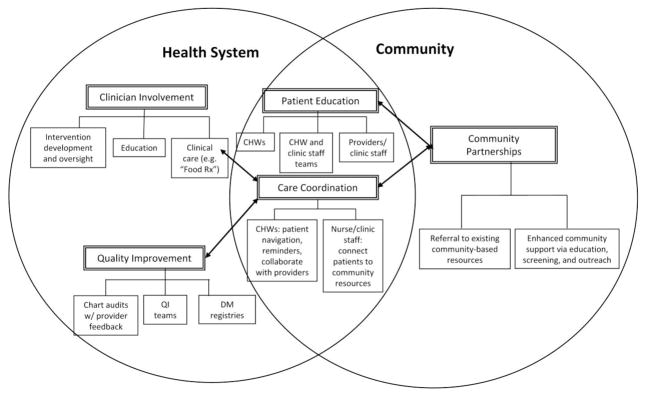
Conceptual model of health system/community linkages.
Patient Education and Community Linkages
Patient education plays a central role in health system linkages to the community [8•, 9, 10••, 11, 12••, 13•, 14•, 15•, 16•]. Educational interventions are frequently used to improve self-management and healthy lifestyle behaviors in diabetes patients. However, racial and ethnic minorities experience barriers that limit the effectiveness of these programs, including access to affordable healthy food, safe space for physical activity, and limited health literacy [17–20]. Thus, culturally tailoring diabetes-related education may help to increase success of diabetes interventions with racial and ethnic minorities [6]. Yet barriers still remain in integrating clinic-based education with the community, even if the curriculum is culturally tailored. Reimbursement for diabetes education is typically low and the time and resources spent to identify, establish and support community partnerships is not reimbursed by health insurance plans [21]. Thus, health systems currently must have the vision and capacity to support efforts at integrating patient education into the community, although insurance plans may soon provide incentives for these efforts through changing reimbursement models. For the purpose of this paper, we define culturally tailored education as diabetes-related education, provided either by providers, clinic staff, and/or community health workers (CHWs) in group or individual settings, specifically created or adapted to address the values, preferences, and needs of a racial or ethnic minority population.
Community Health Workers
Community health workers (CHWs) are patients, peers of patients, or other lay community members (e.g. promotoras) without formal medical training who receive training as a part of the intervention in order to provide diabetes-related education and support for patients. Traditionally, the strength of CHWs has been their ability to reach people outside of the health system and work with them in familiar community settings (e.g. churches, recreational facilities, community centers) to improve health behaviors. While CHWs have existed for some time as a means of providing additional education and support to racial/ethnic minority communities, it is relatively recent that efforts have been made to fully integrate them into healthcare delivery systems [22]. There is a growing body of research documenting the efficacy of combining CHWs and nurses to provide comprehensive care management that includes health care (e.g. diabetes treatment titration based on algorithms, vaccination administration), care coordination, patient education and referral/navigation among community resources to support lifestyle changes [8•, 9, 23–26]. Community health workers have also been integrated into health systems by linking community-based patient information (e.g. information from CHW home visits) to patient medical records, having CHWs accompany patients to primary care visits and by having CHWs hired as health system employees to enhance their role as bridges between health care and community-based support [11, 14, 16•, 27–29]. Thus, integrating community health workers into multi-disciplinary health teams providing team-based care is an emerging way in which health systems are providing stronger links for their patients to community resources, in terms of both human capital (i.e. CHWs themselves) and community-based resources (e.g. grocery store tours).
Nurse/CHW teams combine complementary skills and strengths to provide a seamless spectrum of support for patients. Nurses can provide clinical care and high-level patient education and care coordination, while CHWs can address sociocultural barriers to care, provide basic health education and care coordination, and help patients connect to resources within the community. One example is DePue et al.’s culturally adapted diabetes self-management intervention for patients from a community health center in American Samoa, delivered by a nurse-CHW team and based on Gary et al’s program Project Sugar 2 [8•, 9, 24]. CHWs provided individualized education for patients, assisted with appointment scheduling and attendance, and helped to engage families in supporting patient self-management. Treatment algorithms were used to guide patient care, and the nurse/CHW team conducted a visit with patients to review and document their “risk profiles”. Nurses helped to oversee CHWs, delivered group self-management education for high-risk patients, and gave feedback on diabetes patients’ needs to their physicians. Significant improvements were observed in the intervention group as compared to patients receiving usual care; the adjusted difference in HbA1c was 0.53% between groups [8•]. In 2012, Gerber et al published the design of a randomized clinical trial evaluating the effect of a clinical pharmacist/CHW team (vs. clinical pharmacist alone) in managing African-American and Latino diabetes patients, using a similar model of nurse/CHW teams [30]. Clinical pharmacists will provide medication adjustment and disease management services [30]. Results have not been published, but this represents another complementary mechanism of integrating CHWs into medical care teams to address diabetes disparities. In the Advancing Diabetes Self-Management (ADSM) program, a CHW program in an urban community health center with a primarily Latino population, CHWs were integrated into the healthcare team and provided support in clinic and community-based settings through individual counseling, peer support groups, a walking club, and classes on diabetes self-management [15•]. CHWs supported group cognitive-behavioral therapy sessions led by mental health professionals for diabetes patients diagnosed with depression, and delivered education in the community at the farmer’s market, health fairs, and street festivals [15•]. Diabetes control improved at 12 months (0.48% reduction in mean HbA1c levels) with larger improvements noted among those with more frequent CHW interactions (0.28% HbA1c reduction for weekly contact, 1.16% reduction for contact 4 times per week) [15•].
Non-CHW Patient Education
While CHWs can play a vital role in patient education, the majority of diabetes education within health systems is conducted by clinic health educator staff such as certified diabetes educators (CDEs). In attempt to combine the benefits of community health workers (e.g. cultural concordance, enhanced patient trust, etc.) and CDEs (i.e. standardized, certified training in diabetes education), one program purposely recruited ideal candidates from the local community and then trained them to become CDEs [31•]. The team viewed this ‘growing our own’ strategy as one that helped to address diabetes health disparities. The community-recruited CDEs were well integrated into the primary care teams. Patients enrolled in CDE-led classes had 0.5% reductions in mean HbA1c values [31•]. Increasingly, clinic-based patient education is being linked to community resources to enhance the real-world skills needed to support healthy lifestyles (e.g. grocery shopping, food preparation, physical activity classes). This integration of didactic classes, skills training and community resources provides promise for sustaining the health behaviors and health outcomes that typically decline after 6 months [32].
Physicians and Community Linkages
Physicians were sometimes involved in the development and/or implementation of patient education programs, in which patients were linked to community resources [10••, 12••, 33•]. For example, one intervention used providers as well as clinic staff to teach the content of a culturally-tailored class for diabetes patients that focused on diabetes self-management and skills for engaging in shared decision-making [12••]. While the classes took place in a healthcare setting, providers and clinics staff linked class participants to community-based efforts, such as a monthly food pantry/health fair, that included additional education and resources to help with lifestyle changes [12••]. In 2011, Geller et al reported an intervention where the physician was integrally linked to both health care and community components. The physician led weekly group medical visits and also served as the ‘fitness instructor’ at a local gym for a weekly exercise class featuring culturally-appropriate activities chosen by the Latino diabetes patients enrolled in the study [33•]. Having the clinician lead classes in both settings (health system and community) was felt to be important to overall patient engagement in the program. Improvements were noted in patient reports of general health, mental health and quality of life as well as decreased symptoms of depression [33•].
Physicians were sometimes only indirectly tied to healthcare/community linkages. That is, they were involved in the larger intervention to address diabetes disparities but not the components with immediate community ties. For example, physicians were sometimes targeted to receive information about the intervention (e.g. community-based education to which physicians could refer patients), diabetes-related educational topics, and/or study patients’ clinical information (e.g. HbA1c results) [8•, 9, 12••, 13•, 15•, 16•]. Provider education included diabetes-related continuing medical education [14•], training in the behavior change theory [12••, 15•], and workshops on improving confidence in skills related to cultural competency, communication, and shared decision-making that mirrored the content of culturally-tailored education for providers’ patients [12••]. In the Latinos en Control project, providers were members of the study team for the intervention, which included culturally-tailored patient education in community-based settings, and were sent their patients’ study-related lab results, including emailed graphs of unsafe glucose values downloaded directly from patients’ glucometers [13•, 34]. Significant change was observed in HbA1c at 4 months (0.88% reduction for intervention participants vs. 0.35% reduction for the control group), and in diabetes knowledge, glucose monitoring, and diet at 12 months [13•].
Quality Improvement/Health Systems Changes and Community Linkages
Quality improvement (QI) strategies are utilized widely across diabetes disparities interventions, and can improve care for diabetes patients in safety-net clinics with minority populations [35–36]. There is a growing trend for QI strategies to incorporate community components as part of broader implementation of the Chronic Care Model. In 2012, Hargraves et al reported on efforts of a statewide diabetes QI collaborative to incorporate a CHW component with the hope of having a synergistic effect between health system and community components, and reduce diabetes disparities [37]. The health centers that were randomized to receive the CHWs had significant increases in self-management goal setting among their patients in comparison to health centers that continued to receive only the QI intervention [37]. Current trends are for diabetes QI strategies to focus on care coordination to help patients develop skills to navigate the healthcare system, and manage their disease throughout their everyday lives in the community [8•, 9, 10••, 11, 12••, 14•, 15•, 16•, 23, 25–26, 29–30, 38]. Care coordination encompasses a range of individualized support for diabetes patients from clinic staff and/or CHWs, including education and consultation on self-management goals, assistance in healthcare system navigation, facilitating communication with providers, and connecting patients to community resources. In 2013, Willard-Grace et al reported on their use of medical assistants as care coordinators or ‘health coaches’ to the primarily Latino and African-American patients receiving care in San Francisco’s safety net clinics. These health coaches provided health education and skills training, gave support (e.g. active listening, emotional support), facilitated medication adherence, and helped patients navigate the health system and community resources. They contacted patients via telephone, made home visits, and accompanied patients to medical visits. This trial is still underway to seek to evaluate HbA1c, blood pressure and LDL cholesterol as their primary outcome measures [38].
The REACH 2010 Charleston and Georgetown Diabetes Coalition project encompassed a number of QI strategies within the Coalition’s partner ambulatory care systems, one of which involved the use of a patient-held record that included HbA1c, blood pressure, and lipid values [10••, 39, 40••]. Called the Gold Card, this tool was meant to serve as a link for patients between the health system and community. Patients could refer to the Gold Card at home as a reminder of areas on which to focus their self-management and also bring the Gold Card to clinic to serve as a prompt for physicians to discuss disease monitoring and facilitate patients being more actively involved in managing their diabetes care [39]. Peek et al’s “South Side Diabetes Project” also disseminated similar diabetes cards for patients to use at home and in medical visits [12••, 41].
While most of the QI/community health linkages have originated within health systems, there are several recent cases where community efforts led to QI changes within clinics. The Latino Health for All Coalition has utilized a community-based participatory research (CBPR) approach to address Latino diabetes disparities, and their efforts have led to the addition of interpreter services and language/literacy-appropriate educational materials at a local safety net clinic, changes that likely would not have happened without the Coalition [42•].
It is important to note that QI/health systems interventions often involve multiple QI projects. Some of these might integrate with the community, while other QI efforts stand separate from the community, but are nonetheless important. Examples of “stand-alone” QI projects in the interventions we identified included the creation of multidisciplinary quality improvement teams to bring together providers and clinic staff as a means for sharing best practices for working with diabetes patients [10••, 12••], the use of medical chart audits to assess the impact of quality improvement strategies [10••, 12••], and the creation of diabetes registries [10••, 16•].
Multiple Integrated Systems& Community Linkages
Patient education, Physicians, & Quality Improvement/Health Systems Change
While some interventions focused on integrating a single aspect (e.g. patient education) with community linkages, other interventions sought to integrate multiple components (i.e. patients, physicians, staff and/or the health system) with community resources. For example, in 2009 the Merck Foundation launched the Alliance to Reduce Disparities in Diabetes, wherein 5 sites throughout the U.S. sought to implement diabetes self-management education, provider education, quality improvement strategies, and community engagement strategies in order to reduce diabetes disparities [43••]. REACH 2010, funded by the Centers for Disease Control and Prevention, has included several projects that primarily focus on diabetes. REACH 2010 projects have typically used community-based health approaches, but several have integrated with health systems and the Charleston/Georgetown Coalition had a multi-faceted integrated intervention [10••, 14•, 28, 39, 40••].
The REACH 2010 Charleston and Georgetown Diabetes Coalition has had the goal of improving access, care, reimbursement, education, and outcomes for the over 12,000 African American diabetes patients served through their affiliated ambulatory care health systems [10••, 39, 40••].They utilized QI strategies, patient education, provider engagement, and strong community partnerships (e.g. local libraries, faith-based organizations, local businesses and civic organizations). For example, CHWs, or “Community Health Advisors”, and health professionals provided self-management education and connected diabetes patients to assistance for medications and diabetic supplies. The coalition also created a Health Information Network that updated diabetes-related materials for distribution in the community (e.g. local libraries) [10••, 39].Baseline disparities in healthcare process measures (e.g. HbA1c, lipid and kidney testing, eye exams) and health outcome measures (e.g. blood pressure control) between African Americans and Whites/’Other’ races had resolved at 24 months [39]. The Charleston/Georgetown team also reported a 36% reduction in population-level lower extremity amputations over a 9 year period [10••].
The “South Side Diabetes Project” (officially known as “Improving Diabetes Care and Outcomes on the South Side of Chicago”) is another example of a multi-component integrated intervention that includes patient education, provider training, and a QI collaborative, and links these healthcare components to enhanced community-based support. The South Side Diabetes Project is part of the Alliance to Reduce Disparities in Diabetes and is also supported by the National Institutes of Health. The South Side Diabetes Project launched a “Food Rx” program where physicians write “prescriptions” for healthy food that patients can redeem as discounts or vouchers for fresh fruits and/or vegetables at a local farmer’s market or any of 9 Walgreens stores with a “food desert” designation [44]. To date, over 1000 “Food Rx “have been distributed in clinics and community settings. Patient-friendly educational tours of the farmer’s market and grocery aspects of the Walgreens stores are coordinated by the intervention staff and led by certified diabetes educators (CDEs), pharmacists, and trained community members. Clinic patients from the diabetes education classes receive ‘special invitations’ to the community events. Several patients have been trained to lead educational tours at the farmer’s market as well as at Save-A-Lot, a low cost grocer where the South Side team has trained health educators and community members to educate community residents with limited financial means on how to buy and prepare healthy foods. The intervention also includes a QI collaborative, in which the 6 participating health centers are working to implement care coordinators to serve as additional bridges between the health systems and community resources [12]. Participating clinics reported significant improvements in community linkages, diabetes self-management, delivery system design, and Chronic Care Model integration [12].
Social Determinants of Health
There are interventions that are attempting to go beyond bridging health systems to community resources and take a more macro-level approach to health disparities [45•, 46••, 47••]. Such approaches recognize that there are many social determinants that affect health and contribute to health disparities (e.g. low socioeconomic status, limited literacy) and have worked collaboratively with other community-level institutions to improve educational systems, promote economic development, and enhance community development. These interventions typically have taken a holistic approach to wellness and often address prevention and chronic disease management more broadly rather than exclusively on diabetes. A “Whole Community” model was developed to address health disparities in the Cambodian community in Lowell, Massachusetts [46••]. Their model includes networks that address domestic violence, youth development, and language access as well as HIV education/prevention and diabetes/cardiovascular education and support [46••]. Their diabetes work, funded through the CDC’s Cambodian Community Health 2010 project, has included outreach, peer support, stress management, case management and media programs. The program evolved over time to integrate with local health systems and currently utilizes community health workers as part of clinical care teams to bridge diabetes health care with their prior community-based diabetes outreach and support [46••]. The Diabetes Health and Wellness Institute (DHWI) in Baylor, Texas has 4 pillars that represent the scope of their partnerships: Educational Initiatives, Economic Development, Public Health Care Initiatives and Faith Community Initiatives [47••]. The DWHI has partnered with the City of Dallas, local churches (through a ministerial advisory board), Baylor Health Care System and community organizations to address local diabetes disparities. For example, the DWHI educates schools, churches, community leaders, and local businesses about community-specific health risks with the goal of enhancing community awareness and engagement around health [47••].
Summary and Conclusions
The healthcare policy movement towards population management and accountable care organizations calls for evidence-based healthcare interventions that build upon existing community-based resources. This approach may be particularly effective for improving diabetes-related care and outcomes in racial and ethnic minority populations that are disproportionately affected by the disease and experience additional barriers to accessing equitable care. We sought to identify the commonly integrated healthcare and community components in the diabetes disparities interventions included in this paper. While there is a wide range of evidence supporting different strategies for reducing diabetes disparities [6], most of the interventions we found reported that integrated healthcare and community components were initiated in the healthcare setting and used a combination of strategies across three common domains: (1) patient education, (2) clinician involvement, and (3) quality improvement/health system change. Within these domains, culturally-tailored patient education and care coordination were included across the majority of interventions we found, suggesting that these components may be particularly well positioned for integration. We found that only a subset of interventions is currently attempting to integrate more than one domain with community resources, and physicians often had no direct link with community programs. This speaks to the challenges in implementing fully integrated programs to address diabetes disparities, as well as the need for more real-world examples to inform the field.
In order to fully integrate healthcare and community components, we believe that it is important to go beyond merely referring patients to existing community resources, to actively collaborating with community partners to provide education and outreach outside of the healthcare setting. This is partly because leveraging existing social capital among patients (e.g. through social linkages formed in patient education classes) to provide a “warm hand-off” to community-based resources may be particularly effective in promoting the early adoption of lifestyle changes (e.g. physical activity). That is, patients may be more willing to try out a community resource if they can do so with the support of existing peer groups (e.g. peer educators, co-participants in patient classes) and trusted intervention team members (e.g. nurses, clinic staff, CDEs). In addition, stronger linkages between the healthcare and community components may result if common staff is present in both settings. Finally, we believe that it is fundamentally important to enhance the infrastructure of grassroots/resource-limited community organizations as a means of improving the health of the community and its members. While it is important to collaborate with community organizations, it can be challenging for health systems, researchers, and community organizations with common missions to find each other and forge successful partnerships. CommunityResearchPartners.net is an online tool designed to promote community engaged research by serving as a ‘matchmaker’ between community organizations and researchers in Nashville, Tennessee (48). This tool, developed by researchers at Vanderbilt University in collaboration with Community Campus Partnership for Health (CCPH), is currently being revised and expanded for national use in the fall of 2013.
While it is important to establish partnerships in order to link diabetes patients from the healthcare setting to enhanced support in the community, there are also many people with diabetes that frequently attend community events (e.g. health fairs) but do not have a regular source of medical care. Most of the intervention included in this paper were initiated in the healthcare setting, and linked out to the community. Thus, most of the intervention participants were current health system patients that already had a source of primary medical care. The South Side Diabetes project is one example of an intervention that leveraged community partnerships to link community members to healthcare providers. Intervention staff collaborated with the University of Chicago’s Urban Health Initiative to conduct outreach at community events in order to identify people with diabetes living on Chicago’s South Side without regular access to care, and subsequently connect those community members to a medical home [12••]. This has implications for the implementation of accountable care organizations that may be responsible for geographic populations of persons regardless of whether they are existing patients in the health system. Providing enhanced support in community-based settings can improve the reach of projects initiated in healthcare settings, and can also serve as a link from the community to the healthcare system.
Acknowledgments
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) (Grant No. R18DK083946), the Chicago Center for Diabetes Translation Research (Grant No. P30 DK092949-01) and the Alliance to Reduce Disparities in Diabetes of the Merck Company Foundation. Monica Peek was supported by the Mentored Patient-Oriented Career Development Award of the NIDDK (Grant No. K23 DK075006) and the Robert Wood Johnson Foundation. Marshall Chin is supported by an NIDDK Midcareer Investigator Award in Patient-Oriented Research (Grant No. K24 DK071933).
Footnotes
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Monica E. Peek, Molly Ferguson, Nyahne Bergeron, Debra Maltby, and Marshall H. Chin declare that they have no conflict of interest.
Contributor Information
Monica E. Peek, Email: mpeek@medicine.bsd.uchicago.edu, University of Chicago, Section of General Internal Medicine, 5841 South Maryland Avenue, MC 2007, Chicago, IL 60637, 773-702-2083 (phone), 773-834-2238 (fax).
Molly Ferguson, Email: molljean@me.com, University of Chicago, Section of General Internal Medicine, 5841 South Maryland Avenue, MC 2007, Chicago, IL 60637, 773-456-9420 (phone), 773-834-2238 (fax).
Nyahne Bergeron, Email: nbergeron@medicine.bsd.uchicago.edu, University of Chicago, Section of General Internal Medicine, 5841 South Maryland Avenue, MC 2007, Chicago, IL 60637, 773-702-8847 (phone), 773-834-2238 (fax).
Debra Maltby, Email: dmaltby@medicine.bsd.uchicago.edu, University of Chicago, Section of General Internal Medicine, 5841 South Maryland Avenue, MC 2007, Chicago, IL 60637, 773-834-2605 (phone), 773-834-2238 (fax).
Marshall H. Chin, Email: mchin@medicine.bsd.uchicago.edu, University of Chicago, Section of General Internal Medicine, 5841 South Maryland Avenue, MC 2007, Chicago, IL 60637, 773-702-4769 (phone), 773-834-2238 (fax).
References
Papers of particular interest, published recently, have been highlighted as:
• Of Importance
•• Of Major Importance
- 1.Chow EA, Foster H, Gonzalez V, McIver L. The disparate impact of diabetes on racial/ethnic minority populations. Clin Diabetes. 2012;30(3):130–3. [Google Scholar]
- 2.Agency for Health Research and Quality (AHRQ) Diabetes disparities among racial and ethnic minorities. Rockville, MD: Agency for Healthcare Research and Quality; 2001. AHRQ Publication No.02-P007. [Google Scholar]
- 3.National Diabetes Information Clearinghouse (NDIC) National diabetes statistics, 2011. Bethesda, Maryland: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2011. NIH Publication No. 11–3892. [Google Scholar]
- 4.Chin MH, Clarke AR, Nocon RS, Casey AA, Goddu AP, Keesecker NM, et al. A roadmap and best practices for organizations to reduce racial and ethnic disparities in health care. J Gen Intern Med. 2012;27:992–1000. doi: 10.1007/s11606-012-2082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Betancourt JR, Duong JV, Bondaryk MR. Strategies to reduce diabetes disparities: An update. Curr Diabetes Rep. 2012;12(6):762–8. doi: 10.1007/s11892-012-0324-1. [DOI] [PubMed] [Google Scholar]
- 6.Peek ME, Cargill A, Huang ES. Diabetes health disparities: A systematic review of health care interventions. Med Care Res Rev. 2007;64(5 SUPPL):101S–56S. doi: 10.1177/1077558707305409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shortell SM. Bridging the divide between health and health care. JAMA. 2013;309(11):1121–2. doi: 10.1001/jama.2013.887. [DOI] [PubMed] [Google Scholar]
- 8•.DePue JD, Dunsiger S, Seiden AD, et al. Nurse-community health worker team improves diabetes care in American Samoa. Diabetes Care. 2013;36:1947–53. doi: 10.2337/dc12-1969. This intervention utilized a nurse-CHW team to provide self-management education and care coordination for patients in the underserved area of American Samoa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gary TL, Batts-Turner M, Yeh HC, et al. The effects of a nurse case manager and a community health worker team on diabetic control, emergency department visits, and hospitalizations among urban African Americans with type 2 diabetes mellitus. Arch Intern Med. 2009;19:1788–94. doi: 10.1001/archinternmed.2009.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10••.Jenkins C, Pope C, Magwood G, et al. Expanding the Chronic Care Framework to improve diabetes management: the REACH case study. Prog Community Health Partnersh. 2010;4:65–79. doi: 10.1353/cpr.0.0108. This article outlines the expansion of the Chronic Care Model (CCM) to the Community CCM, which integrates community and health systems components and was informed by the REACH Charleston and Georgetown Diabetes Coalition. [DOI] [PubMed] [Google Scholar]
- 11.Palmas W, Teresi JA, Findley S, et al. Protocol for the Northern Manhattan Diabetes Community Outreach Project. A randomized trial of a community health worker intervention to improve diabetes care in Hispanic adults. BMJ Open. 2012;2:1–6. doi: 10.1136/bmjopen-2012-001051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12••.Peek ME, Wilkes AE, Roberson TS, et al. Early lessons from an initiative on Chicago’s South Side to reduce disparities in diabetes care and outcomes. Health Aff. 2012;31:177–86. doi: 10.1377/hlthaff.2011.1058. This multi-faceted intervention integrated patient education, clinician involvement, quality improvement, and community linkages, and provided enhanced support in the community through education, screening, and outreach. This intervention also provided a link from the community to the healthcare system by connecting community members without a medical home to a regular source of care. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13•.Rosal MC, Ockene IS, Restrepo A, et al. Randomized trial of a literacy-sensitive, culturally-tailored diabetes self-management intervention for low-income Latinos. Diabetes Care. 2011;34:838–44. doi: 10.2337/dc10-1981. This intervention integrated culturally-tailored patient education in community-based settings with community-health center clinician involvement. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14•.Spencer MS, Rosland AM, Kieffer E, et al. Effectiveness of a community-health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am J Public Health. 2011;101:2253–60. doi: 10.2105/AJPH.2010.300106. This intervention utilized CHWs to provide education and care coordination in community-based settings, conducted a joint patient visit with CHWs and primary care providers, and provided enhanced community support through healthy eating and exercise activities as well as a local farmer’s market. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15•.Thompson JR, Horton C, Flores C. Advancing diabetes self-management in the Mexican American population: a community health worker model in a primary care setting. Diabetes Educ. 2007;33 (Suppl 6):159S–65S. doi: 10.1177/0145721707304077. This study outlines the value of community health workers to improve diabetes education and management, reduce health disparities, foster improved patient-provider communication, and act as navigators to needed care services and resources for Mexican-American patients in a primary care setting. [DOI] [PubMed] [Google Scholar]
- 16•.Walton HW, Snead CA, Collinsworth AW, Schmidt KL. Reducing diabetes disparities through the implementation of a community-health worker-led diabetes self-management education program. Fam Community Health. 2012;25:161–71. doi: 10.1097/FCH.0b013e31824651d3. This intervention integrated CHWs into a primary care system, and created a web-based diabetes registry and management system for use by CHWs and clinicians. [DOI] [PubMed] [Google Scholar]
- 17.Rothman R, Malone R, Bryant B, Horlen C, DeWalt D, Pignone M. The relationship between literacy and glycemic control in a diabetes disease-management program. Diabetes Educ. 2004;30:263–73. doi: 10.1177/014572170403000219. [DOI] [PubMed] [Google Scholar]
- 18.Rhee MK, Cook CB, El-Kebbi I, Lyles RH, Dunbar VG, Panayioto RM, et al. Barriers to diabetes education in urban patients: perceptions, patterns, and associated factors. Diabetes Educ. 2005;31:410–7. doi: 10.1177/0145721705277022. [DOI] [PubMed] [Google Scholar]
- 19.von Goeler DS, Rosal MC, Ockene JK, Scavron J, De Torrijos F. Self-management of type 2 diabetes: a survey of low-income urban Puerto Ricans. Diabetes Educ. 2003;29:663–72. doi: 10.1177/014572170302900412. [DOI] [PubMed] [Google Scholar]
- 20.Horowitz CR, Colson KA, Hebert PL, Lancaster K. Barriers to buying healthy foods for people with diabetes: evidence of environmental disparities. Am J Pub Health. 2004;94:1549–54. doi: 10.2105/ajph.94.9.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carpenter DM, Fisher EB, Greene SB. Shortcomings in public and private insurance coverage of diabetes self-management education and support. Popul Health Manag. 2012;15:144–8. doi: 10.1089/pop.2011.0042. [DOI] [PubMed] [Google Scholar]
- 22.Shah M, Kaselitz E, Heisler M. The role of community health workers in diabetes: update on current literature. Curr Diabetes Rep. 2013;13:163–71. doi: 10.1007/s11892-012-0359-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brown SA, Garcia AA, Winter M, Silva L, Brown A, Hanis CL. Integrating education, group support, and case management for diabetic Hispanics. Ethn Dis. 2011;21(1):20–6. [PMC free article] [PubMed] [Google Scholar]
- 24.Gary TL, Bone LR, Hill MN, Levine DM, McGuire M, Saudek C, et al. Randomized controlled trial of the effects of nurse case manager and community health worker interventions on risk factors for diabetes related complications in urban African Americans. Prev Med. 2004;37(1):23–32. doi: 10.1016/s0091-7435(03)00040-9. [DOI] [PubMed] [Google Scholar]
- 25.Allen JK, Himmelfarb CD, Szanton SL, et al. COACH Trial: A randomized controlled trial of nurse practitioner/community health worker cardiovascular disease risk reduction in urban community health centers. Circ Cardiovasc Qual Outcomes. 2011;4(6):595–602. doi: 10.1161/CIRCOUTCOMES.111.961573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Philis-Tsimikas A, Gilmer TP, Schultz J, et al. Community-created programs: can they be the basis of innovative transformations in our health care practice? Implications from 15 years of testing, translating, and implementing community-based, culturally tailored diabetes management programs. Clin Diabetes. 2012;30(4):156–63. [Google Scholar]
- 27.Fisher EB, Earp JA, Maman S, et al. Cross-cultural and international adaptation of peer support for diabetes management. Fam Pract. 2010;27:i6–16. doi: 10.1093/fampra/cmp013. [DOI] [PubMed] [Google Scholar]
- 28.Spencer MS, Hawkins J, Espitia NR, Sinco B, Jennings T, Lewis C, et al. Influence of a community health worker intervention on mental health outcomes among low-income Latino and African-American adults with type 2 diabetes. Race Soc Probl. 2013;5:137–46. doi: 10.1007/s12552-013-9098-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McCloskey J, Tollestrup K, Sanders M. A community integration approach to social determinants of health in New Mexico. Fam Community Health. 2011;34:S79–91. doi: 10.1097/FCH.0b013e318202a852. [DOI] [PubMed] [Google Scholar]
- 30.Gerber BS, Rapacki L, Castillo A, Tilton J, Touchette DR, Mihailescu D, et al. Design of a trial to evaluate the impact of clinical pharmacists and community health promoters working with African-American and Latinos with diabetes. BMC Pub Health. 2012;(12):891. doi: 10.1186/1471-2458-12-891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31•.Kahn LS, Tumiel-Berhalter L, D’Aniello R, et al. The impacts of “Growing Our Own”: a pilot project to address health disparities by training health professionals to become certified diabetes educators in safety net practices. Diabetes Educ. 2012;38:86–93. doi: 10.1177/0145721711427455. The article outlines the evaluation of a certified diabetes educators (CDE) training initiative, the impact of CDEs on patient diabetes outcomes, and the integration of the CDEs into a primary care practice team in an effort to improve diabetes management and education among minority patients in Buffalo, New York. [DOI] [PubMed] [Google Scholar]
- 32.Haas L, Marynuik M, Beck J, et al. On behalf of the 2012 Standards Revision Task Force. National standards for diabetes self-management education and support. Diabetes Care. 2012;35:2393–401. doi: 10.2337/dc12-1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33•.Geller JS, Orkaby A, Gleghorn GD. Impact of a group medical visit program on Latino health-related quality of life. Explor. 2011;7:94–9. doi: 10.1016/j.explore.2010.12.005. This intervention utilized a medical home and group medical visit model to improve quality of life measures, mental health, and diabetes management among Latinos with diabetes. [DOI] [PubMed] [Google Scholar]
- 34.Rosal MC, White MJ, Restrepo M, et al. Design and methods for a randomized clinical trial of a diabetes self-management intervention for low-income Latinos: Latinos en Control. BMC Med Res Methodol. 2009;9:1–11. doi: 10.1186/1471-2288-9-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chin MH. Quality improvement implementation and disparities: the case of the health disparities collaboratives. Med Care. 2010;48(8):668–75. doi: 10.1097/MLR.0b013e3181e3585c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wilkes AE, Bordenave K, Vinci L, Peek ME. Addressing Diabetes Racial and Ethnic Disparities: Lessons Learned From Quality Improvement Collaboratives. Diabetes Mgmt. 2011;1(6):653–60. doi: 10.2217/dmt.11.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hargraves JL, Ferguson WJ, Lemay CA, et al. Community health workers assisting patients with diabetes in self-management. J Ambul Care Manag. 2012;35(1):15–26. doi: 10.1097/JAC.0b013e31822cbe35. [DOI] [PubMed] [Google Scholar]
- 38.Willard-Grace R, DeVore D, Chen EH, et al. The effectiveness of medical assistant health coaching for low-income patients with uncontrolled diabetes, hypertension, and hyperlipidemia: protocol for a randomized controlled trial and baseline characteristics of the study population. BMC Fam Pract. 2013;14:27. doi: 10.1186/1471-2296-14-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jenkins C, McNary S, Carlson BA, et al. Reducing disparities for African Americans with diabetes: progress made by the REACH 2010 Charleston and Georgetown Diabetes Coalition. Pub Health Rep. 2004;119:322–30. doi: 10.1016/j.phr.2004.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40••.Jenkins C, Myers P, Kelechi TJ, et al. Efforts to decrease diabetes-related amputation in African Americans by the Racial and Ethnic Approaches to Community Health Charleston and Georgetown Diabetes Coalition. Fam Community Health. 2011;34 (Suppl 1):S63–78. doi: 10.1097/FCH.0b013e318202bc0b. This article outlines successful strategies to reduce disparities in diabetes-related amputations for African Americans, including improvements in diabetes messaging in the community and diabetes care, and improved diabetes-related policies. [DOI] [PubMed] [Google Scholar]
- 41.Peek ME, Harmon S, Scott S, Eder M, Roberson TS, Tang H, Chin MH. Culturally tailoring patient education and communication skills training to empower African-Americans with diabetes. Transl Behav Med. 2012;2(3):296–308. doi: 10.1007/s13142-012-0125-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42•.Fawcett SF, Collie-Akers V, Schultz JA, et al. Community-based participatory research within the Latino Health for All Coalition. J Prev Interv Community. 2013;41(3):142–54. doi: 10.1080/10852352.2013.788341. This intervention was supported by a community-academic partnership and utilized the Health for All Model in alignment with key principles of community-based participatory research (CBPR) to promote healthy nutrition, physical activity, and access to health services among Latinos. [DOI] [PubMed] [Google Scholar]
- 43••.Clark NM, Brenner J, Johnson P, et al. Reducing disparities in Diabetes: the Alliance Model for health care improvements. Diabetes Spectr. 2011;24:226–30. The Alliance Model emphasizes the importance of patient self-management education, health systems change, education for providers, and stakeholder engagement as key components of reducing disparities in diabetes. [Google Scholar]
- 44.Goddu AP, Roberson TS, Raffel KE, et al. Food Rx: a community-university partnership to prescribe healthy eating on the South Side of Chicago. Journal of Prevention and Intervention in the Community. doi: 10.1080/10852352.2014.973251. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45•.McCann E. Building a community-academic partnership to improve health outcomes in an underserved community. Pub Health Nurs. 2009;27(1):32–40. doi: 10.1111/j.1525-1446.2009.00824.x. The article outlines the creation of a sustainable community-academic partnership aiming to provide comprehensive health care services and improve health outcomes for underserved residents of the East Garfield Park community in Chicago, IL. [DOI] [PubMed] [Google Scholar]
- 46••.Grigg-Saito D, Toof R, Silka L, et al. Long-term development of a “whole community” best practice model to address health disparities in the Cambodian refugee and immigrant community of Lowell, Massachusetts. Am J Pub Health. 2010;100:2026–9. doi: 10.2105/AJPH.2009.177030. Through a partnership with a federally qualified health center, this intervention involved a multifactorial, culturally-centered approach that utilized community-based collaborations, care coordination, and a range of health care services to address the health needs of a Cambodian refugee and immigrant population. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47••.Rice D, Bain TM, Collinsworth A. Effective strategies to improve the management of diabetes: Case illustration from the Diabetes Health and Wellness Institute. Prim Care Clin Off Pract. 2012;39:363–79. doi: 10.1016/j.pop.2012.03.008. This intervention aimed to reduce health disparities within an underserved minority population through the formation of community-based partnerships, development of interprofessional teamwork and care coordination, and improvement of the patient health care experience in order to improve diabetes management within the primary care setting of a large-scale urban health care system in Dallas, TX. [DOI] [PubMed] [Google Scholar]
- 48.Community Research Partners. [Accessed September 9, 2013]; Available at www.communityresearchpartners.net.


