Abstract
Anxiety, depression, and somatic complaints are a common set of comorbid problems in children and adolescents. This “internalizing cluster” is highly prevalent, impairing during youth and into adulthood, and has substantial impacts on health-care systems. Fortunately, these problem areas may share several etiological factors and, thus, respond to similar interventions. In this paper, we present (a) the rationale for focusing on this cluster, (b) clinical theory on transdiagnostic processes uniting these problems, (c) description of core treatment techniques for this group, with a description of clinical outcomes for two sample cases, and (d) implications of this approach for new transdiagnostic treatment development and everyday clinical practice.
Keywords: transdiagnostic, youth, anxiety, depression, somatic
Over 50 years ago, the first version of the Diagnostic and Statistical Manual of Mental Disorders (DSM) was published. This nascent DSM was a scant 130 pages and described 106 mental disorders (Grob, 1991). In the four revisions since, the manual has grown ever more complex, with the last published version including nearly 300 disorders and amounting to almost 900 pages (DSM-IV-TR; American Psychiatric Association, 2000). Much of this growth in complexity may be fairly reframed as increasing precision, as broad disorder categories reflecting psychodynamic theories of etiology were replaced by a greater number of empirically based, detailed descriptions of symptom clusters. This said, there is a growing recognition in the field that the trend toward ever more narrow, descriptive subtyping of disorder may have reached the limits of usefulness (DSM-5 Task Force Update; Kupfer & Regier, 2009), and there may be substantial clinical and theoretical value in moving toward a transdiagnostic clustering of related disorders.
A major argument for considering adopting a transdiagnostic approach is the pervasiveness and regularity of comorbidity. Clinicians and researchers alike know that individual patients rarely present with one single, constrained DSM disorder. Comorbidity of psychopathology is the rule, rather than the exception, particularly among “near-neighbor” disorders, such as the 10 ostensibly separate anxiety diagnoses, between anxiety and mood disorders, and between attention, behavioral problems, and substance abuse (e.g., Kessler, 1997; Kessler, Chiu, Demler, Merikangas, & Walters, 2005). Comorbidity presents a theoretical challenge to our diagnostic system but, more practically, comorbidity dramatically complicates treatment planning. Most evidence-based treatments, whether psychosocial or pharmacological, are developed, tested, and “certified” for specific diagnoses. In this context, how should specific treatments be delivered to the person with multiple problems? Should a primary diagnosis be selected to the exclusion of other concerns? Should treatments for comorbid problems be sequenced? Should interventions be blended in order to individually map on to specific patient symptom presentations? How could these strategies be taught and implemented reliably, with high quality, in the context of busy health-care contexts? And finally, does all the added effort and attention to diagnostic specificity, at least within the internalizing cluster of disorders, really matter clinically?
In our work, we struggled with these questions focusing on a common cluster of comorbid problems in children and adolescents—anxiety, depression, and, more recently, medical complaints without a clear organic cause. As we will discuss later, this “internalizing cluster” is highly prevalent, impairing both during youth and into adulthood, and has substantial impacts on health-care systems, a potential gateway for intervention. In this paper, we describe the process of our treatment development work over the course of the last decade and our increasing belief in the value of reaching across all internalizing syndromes for a truly transdiagnostic toolbox. Specifically, we present (a) our growing rationale for focusing on this cluster of related problems, (b) clinical theory on transdiagnostic processes uniting these problems, (c) description of core treatment techniques for this group, and (d) current progress on translating this approach into new trans-diagnostic treatments.
Clinical Focus: The Internalizing Cluster
Prevalence and Impact
Separately and in conjunction, youth anxiety, depression, and somatic symptoms are distressing, disabling, and prevalent (e.g., Bell-Dolan, Last, & Strauss, 1990; Campo, Bridge, et al., 2004; Lewinsohn, Hops, Roberts, Seeley, & Andrews, 1993; Scharff, 1997; Walker, Garber, & Greene, 1993). In the pediatric population, prevalence of anxiety is estimated to be as high as 20% (Bell-Dolan et al., 1990), depression estimates reach up to 25% (Lewinsohn et al., 1993), and rates of impairing somatic complaints vary from 7% to 25% (e.g., recurrent abdominal pain; Scharff, 1997). Left untreated, anxiety and depression in youth may lead to the continuation of internalizing problems in adulthood (Pine, Cohen, Gurley, Brook, & Ma, 1998), generally poor health trajectory (Bittner et al., 2007; Brady & Kendall, 1992), lower educational attainment, poor work history, and adult substance use (Keller et al., 1992; Rohde, Lewinsohn, & Seeley, 1994; Weissman et al., 1999). In a similar fashion, children with somatic complaints—such as recurrent abdominal pain—are more likely to experience poorer health outcomes, problems with school attendance and performance, and other psychosocial difficulties than nondiagnosed youths (Campo, Bridge, et al., 2004; Garber, Zeman, & Walker, 1990; Walker et al., 1993). Additionally, reports of childhood somatic symptoms predict adult psychopathology and onset of persistent pain in adulthood (Gureje, Simon, & Von Korff, 2001). As will be discussed further, problems with anxiety, depression, and somatic complaints tend to co-occur (e.g., Campo, Bridge, et al., 2004; Lipsitz et al., 2004), and this comorbidity may lead to worse outcome than any of these disorders presenting in isolation (e.g., Vaccarino, Sills, Evans, & Kalali, 2008).
Comorbidity Within the Cluster
Rates of comorbidity between anxiety and depression are extremely high (Angold, Costello, & Erkanli, 1999; Birmaher et al., 1996), with 25% to 50% of depressed youths in the community also meeting criteria for an anxiety disorder, and 10% to 15% of anxious youths in the community meeting for concurrent depression (Angold et al., 1999). Importantly, greater levels of comorbidity are found in treatment-seeking samples (Regier et al., 1990), where co-occurring rates of anxiety and depression may range up to 70% (Birmaher et al.). Such findings from the youth anxiety/depression literature are complemented by studies of functional pain and physical complaints. Investigation of somatic complaints often does not result in identification of a medical cause (e.g., Campo & Fritz, 2007); however, unexplained somatic symptoms, such as recurrent abdominal pain, headaches, and noncardiac chest pain, are consistently and strongly associated with anxiety and depressive symptoms and diagnoses (Campo & Fritsch, 1994; Egger, Costello, Erkanli, & Angold, 1999). For example, of youths presenting in primary care with recurrent abdominal pain, approximately 80% meet for an anxiety disorder and over 40% meet for depression (Campo, Bridge, et al., 2004). In youth with noncardiac chest pain, rates of comorbidity with anxiety disorders are between 55% and 75% (Lipsitz et al., 2004; Tunaoglu et al., 1995), with lower but significant rates of co-occurrence with depression (13%; Kashani, Lababidi, & Jones, 1982). Within the somatic literature, it appears that abdominal and noncardiac chest pain have stronger associations with anxiety (Campo & Fritz, 2007; Lipsitz et al.), while fatigue, headaches, and other physical pain (e.g., backache) are more strongly associated with depression (Vaccarino et al., 2008). Current data suggest that the time course of this comorbid cluster begins with the onset of anxiety approximately 3 years prior to co-occurring onset of recurrent abdominal pain and depression (Campo, Bridge, et al., 2004). All of these findings lend support to the idea that anxiety, depression, and somatic symptoms tend to co-occur both cross-sectionally and longitudinally (Lieb, Meinlschmidt, & Araya, 2007).
Evidence for Transdiagnostic Processes From the Psychopathology Literature
The strong evidence for nonrandom associations between pediatric anxiety, depressive, and functional somatic distress raises questions about the nature of the observed comorbidity. Current theories of the development and maintenance of each of these problem areas focus on the interplay between (a) biological sensitivity to life stress, (b) heightened anticipation and experience of pain and emotional distress, (c) mal-adaptive cognitions and poor problem solving, and (d) behavioral inhibition and avoidance. Below, we briefly review the literature implicating each of these processes and their similarities across the internalizing cluster.
Biological Sensitivity to Stress
Both the adult and youth anxiety literatures have theorized a biological vulnerability to acute stress reactions (e.g., Barlow, Allen, & Choate, 2004; Biederman et al., 1993), such that anxious individuals demonstrate overactivity in brain regions that typically work to suppress fight-or-flight and fear responses (e.g., Mathew, Coplan, & Gorman, 2001). Theories of depression suggest a genetic vulnerability to mood dysregulation in response to stressful life events (e.g., Caspi et al., 2003), with polymorphisms in the serotonergic system that parallel serotonin polymorphisms in anxious individuals (e.g., Lanzenberger et al., 2007). Youths with somatic complaints demonstrate physiologic and affective responses to stressors similar to those of anxious and depressed youths (Dorn et al., 2003; Walker, Garber, Smith, Van Slyke, & Claar, 2001), as well as heightened sensitivity to pain, including “visceral hypersensitivity” (Di Lorenzo et al., 2001; Lipsitz et al., 2004). As with anxiety and depression, implicated brain structures for somatic complaints and pain are those relevant to attention and emotional processing of threat and fear (Price, 2000).
Heightened Anticipation and Experience of Pain and Stress
Anxious individuals respond to environmental challenge at lower threshold (e.g., Leonard, 2007; Mathew et al., 2001) and overattend to and interpret threat in ambiguous or nonthreatening situations (Mogg & Bradley, 2005). Indeed, hypervigilance to even minor threatening cues has long been viewed as a core feature of anxiety, and concepts such as anxiety sensitivity, referring to heightened anticipation of harm in relation to threat, have been associated with all manner of pediatric anxiety disorders (Klein, 2009). Higher levels of harm avoidance also appear to characterize youth with functional abdominal pain (Campo, Bridge, et al., 2004), and somaticizing youth display heightened anticipation of pain or stress (Tsao, Lu, Kim, & Zeltzer, 2006) and physiological arousal in response to environmental stressors comparable to that exhibited by anxious youth (Dorn et al., 2003). Data on depressed youth are less clear; however, the threshold for stress-triggered mood episodes may fall over the course of disorder (e.g., Kendler, Thornton, & Gardner, 2001), a process that may reflect either anticipatory processes or biological sensitization over time.
Maladaptive Cognitions and Poor Problem Solving
Anxious youths demonstrate inaccurate and overly threatening cognitive interpretations of events (e.g., anxious apprehension; Barlow, 1988). Similarly, depressed youths exhibit inaccurate, overly negative, and hopeless cognitive styles (e.g., Gladstone & Kaslow, 1995), and youths with somatic complaints appear to overperceive susceptibility to illness (e.g., pediatric abdominal pain; Campo et al., 2001) and express beliefs about pain being inescapable and uncontrollable, which may lead to feelings of helplessness (Banks & Kerns, 1996). In addition, personality traits associated with pessimistic worry, fear of uncertainty, and sensitivity to environmental change or adversity (i.e., negative affect, neuroticism, harm avoidance, trait anxiety) have consistently been associated with a vulnerability to develop anxiety, depression, and functional somatic disorders (Andrews, 1996). There is growing and converging evidence for shared genetic risk between such personality traits and the internalizing cluster of disorders (Hettema, 2008).
Maladaptive Behaviors
Anxious youths demonstrate maladaptive behavioral responses to threat (e.g., behavioral inhibition and avoidance; Biederman et al., 2001), while depressed youths exhibit maladaptive behavioral responses to stress (e.g., avoidance and poor interpersonal problem-solving skills; Gazelle & Rudolph, 2004). Youths with somatic complaints display comparable behaviors. For example, recurrent abdominal pain in youth has been associated with behavioral inhibition and temperamental harm avoidance (Davison, Faull, & Nicol, 1986), and fear and experience of pain may be utilized as an opportunity to withdraw from challenging or physically arousing activities (Walker, Claar, & Garber, 2002). Anxiety, depression, and somatic symptom literatures all identify specific psychological vulnerabilities emerging from early learning as shaping such behavioral patterns (Barlow, 2000; Banks & Kerns, 1996).
Theoretical Summary
The above mentioned factors are not identical across disorder; however, the processes implicated are strikingly similar. The high level of comorbidity between members of the internalizing cluster and these shared underlying features provide good evidence that anxiety, depression, and somatic problems are more related than their separate diagnostic categories suggest.
Evidence for Transdiagnostic Processes From the Treatment Literature
Most evidence-based treatments for youth have been designed to treat specific, single disorders; however, even within this literature, there are glimmers of support for a transdiagnostic treatment approach. The best evidence comes from studies on the positive response of all three problems to cognitive behavioral therapy (CBT) and to selective serotonin-reuptake inhibitors (SSRIs).
Similar Response to CBT
Anxiety, depression, and somatic symptoms all seem to respond to relatively brief CBT interventions. In the treatment of youth anxiety and phobias, CBT has consistently shown positive effects in as little as a single-session (for simple phobias), with some of the highest reported response rates in the psychosocial treatment literature (Compton et al., 2004; James, Soler, & Weatherall, 2005). Likewise, CBT has a two-decade history of positive results in clinical trials for youth depression (Compton et al.), including findings that it outperforms other psychosocial interventions (family therapy, nondirective therapy) for moderately depressed adolescents within 12 sessions (Brent et al., 1997). Although at an earlier stage of development, the literature on CBT for somatic complaints in youths also shows great promise. CBT has also been demonstrated as efficacious in three smaller trials with youths suffering from medically unexplained gastrointestinal complaints and anxiety (Masia Warner, Reigada, Fisher, Saborsky, & Benkov, 2009) and inflammatory bowel disease and dysphoric mood (Szigethy et al., 2004; Szigethy et al., 2007), and one additional study demonstrated a significant decrease in somatic complaints in youths treated with CBT for generalized anxiety disorder (Kendall & Pimentel, 2003). Two additional studies have shown benefit for a very short (6–8 session) CBT protocol for youths with functional recurrent abdominal pain (Sanders et al., 1989; Sanders, Shepherd, Cleghorn, & Woolford, 1994).
Not surprisingly, the key techniques in these CBT interventions are markedly similar across anxious, depressive, and somatic symptom target areas. Table 1 lists the most common CBT techniques for each of these symptom clusters and links each technique to the core processes of internalizing disorder reviewed in our last section. As can be seen in the table, several techniques (e.g., relaxation, problem solving, reducing avoidance) appear across anxiety, depression, and somatic CBT programs. In our own work, these cross-cutting techniques served as the basis for our programs of treatment development.
Table 1.
Elements of CBT for Anxiety, Depression, and Somatic Symptoms
| CBT component by diagnosis | Biological sensitivity | Environmental stressors | Cognitive style | Maladaptive behaviors |
|---|---|---|---|---|
| Anxiety | ||||
| Relaxation | X | X | ||
| Cognitive restructuring | X | |||
| Problem solving | X | X | X | |
| Exposure | X | X | ||
| Depression | ||||
| Relaxation | X | X | ||
| Cognitive restructuring | X | |||
| Problem solving | X | X | X | |
| Behavioral activation | X | X | ||
| Somatic symptoms | ||||
| Relaxation | X | X | ||
| Cognitive restructuring | X | |||
| Problem solving / coping | X | X | X | |
| Behavioral activation | X | X | ||
Similar Response to SSRI
Additional evidence supporting the transdiagnostic nature of anxiety, depression, and somatic complaints comes from their shared response to SSRIs. Pharmacologic interventions with SSRIs for anxious youth have proved as efficacious as CBT at posttreatment assessment (Walkup et al., 2008), and the combination of SSRI treatment with CBT appears to be superior to either single treatment alone for both anxious (Walkup et al.) and depressed youth (Brent et al., 2008; March et al., 2008). Evidence is growing that SSRIs are useful in the management of functional somatic distress in adults (e.g., Jackson et al., 2000; Stahl, 2003), and some preliminary evidence from open trials suggests that they may prove promising in the management of pediatric functional pain and somatic distress (Campo, Perel, et al., 2004).
As discussed previously, serotonin (5-HT) is a neurotransmitter that plays a role in feelings of well-being and is commonly associated with threat perception and anxiety symptoms. The visceral hypersensitivity noted in functional gastrointestinal disorders has also been associated with serotonergic neurotransmission (Bueno, 2005). 5-HT transporter polymorphisms have been associated with variability in responses to threat (Hariri et al., 2002), as well as a number of serotonin receptors and degree of neurotransmitter-receptor binding in anxious individuals (e.g., Lanzenberger et al., 2007). Serotonergic neurotransmission has also been implicated in depression, with pathways projecting to brain areas involved in emotion regulation, stress responses, and rewards (Eley et al., 2004). As with SSRI treatment in anxiety, SSRI treatment for depressed youths increases the synaptic availability of serotonin (Celada, Puig, Amargos-Bosch, Adell, & Artigas, 2004). Given the abundance of serotonin receptors in the gut, SSRI treatment may be useful in the treatment of some somatic complaints, such as functional abdominal pain (Campo, Perel, et al., 2004).
Developing a Transdiagnostic Treatment Approach
In our work, we have begun developing a psychosocial internalizing toolbox to treat this cluster of related problems. In this next section, we briefly review our rationale for focusing on psychosocial treatment and our progress to date in manual development and pilot testing.
Why Not Just Use SSRIs?
Despite SSRI effectiveness, many patients, parents, and providers do not find medication use in children acceptable, even in medical settings (Rushton, Clark, & Freed, 2000; Wisdom, Clarke, & Green, 2006) or wish to attempt intervention by psychosocial means prior to exploring pharmacologic options (e.g., Asarnow et al., 2005). Medication reluctance is especially common among ethnic minority families (Stevens et al., 2009; Young et al., 2006), who already have high perceived barriers to and low rates of seeking mental health services (Chandra et al., 2009). In addition, health service use data indicate that SSRI use is markedly down (e.g., Gibbons et al., 2007; Libby et al., 2007; Libby, Orton, & Valuck, 2009) ever since public FDA hearings on heightened risk of suicidality for youths taking SSRIs and the resultant black box warning label (U.S. Food and Drug Administration, 2004). These data suggest that consumer interest in psychosocial interventions is considerable and focus on such interventions timely.
Given this interest in psychotherapeutic treatment, the field has good evidence to continue modifying cognitive-behavioral interventions for added efficacy/effectiveness. The similarities between techniques across CBT protocols for the internalizing cluster indicate the potential to consolidate core components across disorders into an integrated protocol (e.g., Barlow et al., 2004). Furthermore, practical considerations argue for a transdiagnostic approach, particularly for patients being seen and managed in traditional medical settings or primary care, where clinicians may identify one disorder or another based on the presenting complaint, but where comorbidity is high and access to specialized care is limited.
Development of Two Psychosocial Programs
To date, we have developed two integrated protocols treating (a) co-occurring anxiety and depression and (b) co-occurring anxiety and recurrent abdominal pain, and piloted their use in primary care settings. The process of manual development occurred simultaneously in distinct settings and began with the most natural combination of highly comorbid conditions—anxiety and depression, and anxiety and recurrent abdominal pain. The context in which each treatment was developed lent itself heavily to the progression of each manual: While our treatment development for co-occurring anxiety and depression occurred as a result of work in both primary care and community clinics, where youths often presented with significant symptoms of both anxiety and depression as their primary complaints, the manual for co-occurring anxiety and recurrent abdominal pain occurred in a medical setting, where youths presenting with stomachaches in pediatric and gastroenterology departments also often reported symptoms of anxiety. Below we describe these two treatments in detail, provide case examples, and discuss implications for further consolidation of these techniques for potential use as a single transdiagnostic toolbox for the internalizing cluster.
In the selection of core intervention techniques for the development of our integrated manuals, we turned to the literature for evidence on the relative efficacy of specific CBT techniques. We focused on the child and adolescent treatment literature when available and the adult literature in the absence of evidence from youth studies. Because CBT programs differ significantly in their complexity and number of techniques employed, and because we were interested in brief interventions that could be disseminated in community settings and taught to mental health workers with various levels of psychotherapy expertise, we adopted parsimonious approaches for each manual.
Moreover, these integrated treatments were intended to be both structured and flexible in their administration. Treated youths typically receive all modules presented in the same order; however, therapist and youth work together to tailor the treatment techniques to individual youth symptom presentations and areas of functioning that disorder has affected. The approach is one that offers flexibility of patient and clinician choice within a structured format. For example, treatment focus with a primarily anxious youth will lend towards more exposure-focused sessions, while treatment with a comorbid anxious/depressed youth may require behavioral activation in early sessions (e.g., getting out of bed and going back to school) prior to working on exposure hierarchies (e.g., talking to teacher at school about making up missed homework). Similarly, youths may report that specific techniques are less useful than others (e.g., youth likes progressive muscle relaxation better than guided imagery), and therapist and youth may decide together to focus on different personalized methods of relaxation for the youth to use in stressful situations. Likewise, parental involvement varies from youth to youth. Typically parents are present more often in treatment with children than with adolescents; however, this also depends in part on youth presentation, developmental level, and cognitive or attentional difficulties (e.g., ADHD), since frequently emotional and behavioral development may occur independently of chronological age. While the current integrated manual for anxiety and depression does not include a required parent-only session, the anxiety and recurrent abdominal pain treatment devotes an entire session in Week 2 to parental contingency training specifically in order to target parental responses to youths’ somatic complaints and teach parents how to reward healthy coping behaviors and strategies employed by youths when they experience pain. In general, decisions regarding treatment flexibility are informed by youth and parent descriptions of symptoms and functioning, but therapist clinical judgment is ultimately necessary in order to guide the focus of therapy.
Brief Behavioral Therapy (BBT) for Pediatric Anxiety and Depression
As previously detailed, the development of a unified manual for the treatment of youth anxiety and depression is warranted on grounds of both theoretical (i.e., comorbidity and similar etiology findings) and public health significance. Therefore, we sought to develop a brief (8 to 12 session) psychosocial intervention that might provide maximum dose of the effective core techniques across anxiety and depression CBT manuals.
The anxiety literature provides evidence that exposure to stimuli perceived as threatening may be the central pathway through which intervention effects are achieved. Exposure is as efficacious as more comprehensive CBT in the treatment of youth phobias (Ollendick & King, 1998) and the majority of anxiety symptom remission occurs in the second half of treatment (e.g., during exposure modules; Kendall et al., 1997). Meta-analysis of the adult anxiety treatment literature also lends support to this: Exposure produces outcomes equivalent to CBT (e.g., Gould, Buckminster, Pollack, Otto, & Yap, 1997) and the total number of exposure sessions (across studies) predicts treatment outcome (Feske & Chambless, 1995; Gould, Otto, & Pollack, 1995).
Similarly, data from the depression literature point to the effectiveness of behavioral activation (BA) as a stand-alone treatment, separate from classic CBT, including a significant emphasis on cognitive restructuring (e.g., Hopko, Lejuez, & Hopko, 2004). In comparison to a full CBT protocol, BA has been found to be as or more effective in relieving depression, altering depressogenic thinking (Jacobson et al., 1996), and matching medication effects at posttreatment and surpassing medication at follow-up (Dimidjian et al., 2006). Clinical impressions of the BA protocol suggest that the intervention was particularly effective for adults who experienced difficulty in mastering cognitive restructuring skills in CBT (Dimidjian et al., 2003). If confirmed, this result would certainly inform efforts to create a protocol suitable for the developmental level of children and adolescents, especially with real-world samples likely to also suffer from comorbid attention and learning difficulties. As an additional note, we would like to highlight the difficulty in cognitive work with youths, as developmental level may prevent mastery of skills such as abstract reasoning and identifying and challenging maladaptive thoughts (Kingery et al., 2006; Weisz & Weersing, 1999).
Therefore, in developing our manual we focused heavily on behavioral techniques by adapting and combining compatible aspects of exposure and behavioral activation as “graded engagement.” (For a detailed description of similarities in components and composition of graded engagement technique, as well as session-by-session description of BBT, please see Weersing, Gonzalez, Campo, & Lucas, 2008). In our selection of core treatment techniques for our brief integrated manual, we also included psychoeducation, relaxation, and problem-solving skills. These techniques did not emerge from our literature review as strongly as exposure and behavioral activation, but relaxation is considered beneficial for anxiety and its common comorbid problems (i.e., pain and somatic symptoms; Husain, Browne, & Chalder, 2007) and problem solving is utilized across internalizing and comorbid conditions, as well as in several adult depression protocols within quality-improvement (QI) primary care interventions (e.g., Unüetzer et al., 2002). BBT sessions moved from psychoeducation and easily taught skills (i.e., relaxation and guided imagery) to graded engagement, which constitutes at least half of therapy (and longer for youths who returned for up to four booster sessions after 8 weeks of therapy). For a session-by-session outline of BBT sessions, see the left-hand column of Table 2.
Table 2.
Integrated Brief CBT Programs for Internalizing Disorders
| BBT FOR AN XIETY / DEPRESSION | BBT FOR ANXIETY / PAIN | ||
|---|---|---|---|
| Session 1 | Psychoeducation Treatment rationale |
Session 1 | Psychoeducation Treatment rationale |
| Session 2 | Relaxation Coping with negative affect |
Session 2 | Problem solving (parent session) |
| Session 3 | Problem solving | Session 3 | Relaxation Coping with negative affect and pain |
| Session 4 | Reducing avoidance Setting goals |
Session 4 | Reducing avoidance Setting goals |
| Session 5 | Increasing activation | Session 5 | Increasing activation Problem solving review |
| Session 6 | Increasing activation | Session 6 | Relapse prevention and termination |
| Session 7 | Increasing activation | ||
| Session 8 | Booster session (optional) | ||
| Session 9 | Booster session (optional) | ||
| Session 10 | Booster session (optional) | ||
| Session 11 | Booster session (optional) | ||
| Session 12 | Relapse prevention and termination | ||
BBT for Anxiety and Pediatric Abdominal Pain
Due to comorbidity, underlying etiology, and similarities in treatment techniques for anxiety and pediatric abdominal pain, we have also developed a brief (six session) psychosocial intervention to be used in primary care and other medical settings. Again, public health significance of an integrated manual for anxiety and somatic symptoms is substantial, given that most youths present for care in the medical setting, and that many youths presenting for somatic complaints also experience significant levels of anxiety (Campo, Bridge, et al., 2004).
In parallel with the anxiety literature’s strong emphasis on exposure, the somatic and pain literatures also focus primarily on behavioral techniques (e.g., Sanders et al., 1994). The underlying assumption implicates pain behaviors in producing contingent consequences, such as attention, sympathy, and subsequent avoidance of undesirable activities that become reinforcing for youths to continue displaying the pain behaviors (Sanders et al., 1989). Said differently, youths may view pain and anxiety as signals or alarms that “something’s not quite right”; their resultant behaviors of complaints and attempts to avoid, as well as the consequences (e.g., parental reassurance, avoidance) reinforce the behavior and cause the feared stimuli (e.g., pain in the case of somatic complaints, social interaction with peers in the case of social phobia) to appear even more threatening over time. Thus, exposure in CBT for somatic symptoms is viewed from a rehabilitative perspective such that avoidance is discouraged and youths learn to tolerate pain in a graded fashion—for longer periods of time over a variety of settings that involve higher levels of distress. This behavioral emphasis extends across treatment modules, including parent contingency training, problem solving, relaxation, and behavioral activation. We describe each of these below (see Table 2 for session-by-session treatment techniques).
A feature that distinguishes this protocol from BBT for anxiety and depression is a parent-only session in Week 2. Parental involvement in the treatment of pediatric chronic pain is associated with maintenance of treatment gains over time (Chambers, 2003). Because parents are the gatekeepers to treatment and frequently present in medical settings for services to target unexplained youth somatic complaints, parental involvement in psychosocial intervention may help parents to reframe their understanding of their child’s somatic symptoms. Parents are taught contingency management training to reward healthy coping behaviors and strategies employed by the youth, which may minimize emotional arousal and distress in anticipation of or response to pain triggers, as well as illness and avoidance behaviors (Sanders et al., 1989). Our manual focuses on parent acting as the child’s “coach,” rather than “protector,” so that the youth may begin to exhibit developmentally appropriate independence and manage their pain effectively. Therapists help parents devise a plan for rewarding brave and healthy behaviors. Likewise, teaching parents problem solving allows them to conceptualize pain as a problem to be solved, rather than a danger they must protect their child from. Problem solving is also taught to youths early on in therapy and is continually returned to throughout treatment as a context for reducing avoidance and increasing adaptive coping for youths, and for parental reinforcement of youth behavior.
As with graded engagement in BBT for anxiety and depression, exposure in this protocol is supplemented with BA as both distraction and an opportunity for reintroduction of previously avoided activities in order to learn to cope with pain across contexts. Self-management of pain is considered integral in the treatment of youth somatic symptoms (Masek et al., 1984). In our protocol, youths learn to manage their mood and pain by engaging in pleasant activities, understanding avoidance and problem solving for alternate options when they are afraid, upset, or feeling pain, and using positive self-statements to feel competent in their own pain management. We have also included a relaxation session, as it is considered useful as a strategy to manage anxiety and somatic symptoms (Edwards, Finney, & Bonner, 1991; Husain et al., 2007). As with other treatments, the focus throughout is on the youth using problem-solving and active coping behaviors (e.g., Sanders et al., 1989) to manage their anxiety and somatic symptoms.
While half to two-thirds of BBT for anxiety-depression is spent on activities related to graded engagement, BBT for abdominal pain-anxiety focuses much more on planning for out-of-session challenges and how to manage them, rather than constructing a planned exposure hierarchy per se. Exposures in the BBT for abdominal pain-anxiety protocol are focused on how to manage somatic distress without changing the situation or daily plans. Furthermore, treatment in BBT for abdominal pain and anxiety moves from weekly sessions early in therapy, with a focus on parental contingency management training and problem solving, to biweekly sessions with the potential for telephone check-ins between sessions, as youths begin to reduce their avoidance and practice adaptive coping behaviors discussed in session. The brevity of this intervention provides youths and their parents with specific skills to target anxiety and pain, yet anticipates the necessity of cost-effective and concise intervention in the primary care setting.
Clinical Case Examples1
Two cases are presented here to illustrate application of the above-described interventions in the pediatric primary care setting.2 These particular cases were chosen to highlight the integrated nature of the manuals for youths with co-occurring anxiety-depression and anxiety-recurrent abdominal pain. Note that both cases are conceptualized as primarily internalizing youths. The first case, Natalie, demonstrates use of BBT for anxiety-depression in an adolescent with social anxiety, significant irritability, and other symptoms of depression, and complaints of stomachaches. Natalie was seen in a nonprofit primary care practice that provides healthcare to low-income, under- and uninsured individuals. The second case, Alexis, demonstrates use of BBT for anxiety-somatic complaints in a child with anxiety and ongoing abdominal pain. Alexis was seen in a primary care clinic at a children’s hospital and referred to us by a gastrointestinal specialist. Following these case descriptions, we discuss the potential for future integration of these two manuals into a single protocol.
Natalie
Natalie was a 17-year-old Caucasian female suffering from significant social anxiety, some generalized worries about her own and family’s safety, and minor depression.3 Natalie’s primary care provider referred her to us for treatment. She had initially presented to the provider, and began seeing him monthly, for abdominal pain (he had started her on a GI medication, which had not helped in symptom reduction at her first visit with us). As Natalie presented for treatment by her provider each month, she would share her worries and current mood with him, and after only a few visits the provider identified Natalie as a youth with significant anxiety and depression. At intake with us, Natalie reported self-consciousness and difficulty navigating social relationships in her high school, avoidance of school activities (e.g., ditching class, quitting the softball team), worries about academic achievement, and feeling sad and irritable most of the day, nearly every day. Natalie also endorsed daily stomachaches, although she and her mother both reported that she often participated in activities (school, softball) despite feeling pain and discomfort. In addition, her mother reported that Natalie was irritable with the family and her best friend. Natalie told her therapist in the first session that she avoided most activities across school, social, and family domains, and became both afraid and irritated when she was unable to avoid (e.g., becoming angry each morning when her mother would not permit her to skip school).
Because she identified her somatic symptoms as related to anticipatory anxiety, Natalie found discussion of fight-or-flight in Session 1 and learning relaxation techniques in Session 2 as helpful in providing her with a sense of control over her physiology. Problem-solving (Session 3) played a significant role in Natalie’s treatment, as she and her therapist returned to this technique almost every session (e.g., how to talk to a teacher about making up schoolwork, navigating a new romantic relationship, managing conflict at home with parents and siblings, and how to respond if a friend said or did something mean).
Using these skills as a starting point, Natalie developed an exposure hierarchy for social anxiety and safety concerns and began actively utilizing BA to manage her mood and reward herself for being brave (Session 4). In session, Natalie practiced making mistakes while reading, writing, and talking to others, first with her therapist, then with other study and pediatric reception staff, and finally in the practice waiting room. Outside of session, Natalie practiced making mistakes while speaking with family members and friends, and her ultimate exposure involved dropping a binder full of papers in a crowded hallway at school. These exposures were anxiety provoking, but at the end of treatment Natalie was able to articulate that everyone made mistakes, and that if she slowed down to think and practice her techniques (e.g., relaxation, problem-solving, BA), she would come to a reasonable conclusion rather than becoming irritated and withdrawing. Furthermore, by the end of treatment Natalie was able to successfully assert herself in her romantic relationship and she also rejoined the softball team she had previously quit. Moreover, she reported a significant decrease in her stomachaches, even though these were not directly targeted in treatment.
Therapy with Natalie was not without its challenges. At intake, Natalie reported very low self-esteem, intermittent thoughts of hopelessness, and passive thoughts of cutting herself in order to relieve distress. Clearly symptoms associated with significant risk, Natalie’s therapist checked in with her about these during every session and phone contact. Twice during treatment, Natalie and therapist had to utilize problem-solving in order to create, and then modify, a safety plan when she endorsed thoughts about cutting herself. Additionally, about halfway through treatment, Natalie confided in her therapist that she had just recently become sexually active with an older adolescent male and was having difficulty asserting herself in this new relationship. These treatment challenges were addressed through problem-solving, while doing exposures flexibly and often assigning the majority of her exposure work for at-home practice.
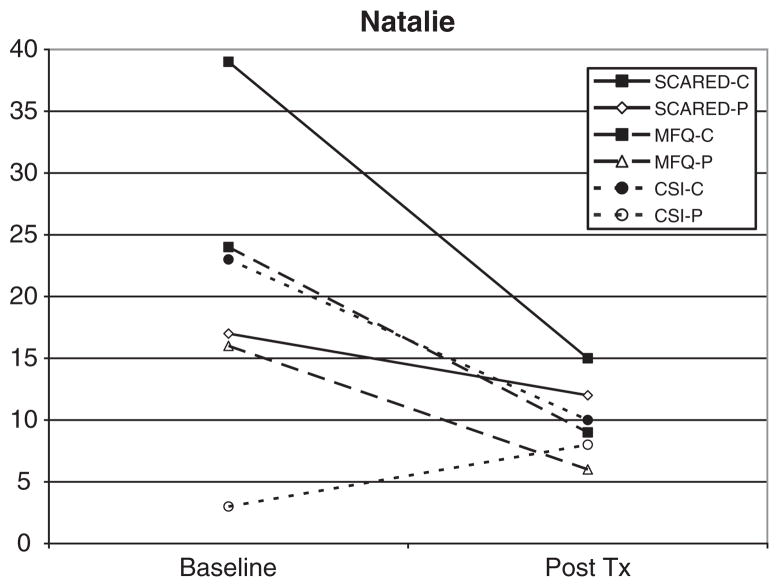
Natalie’s anxiety scores4 at baseline were extremely high, with her self-reported level of anxiety 1.5 standard deviations above the clinical cutoff for the measure. Her levels of depression5 and somatic6 symptoms were just above clinical cutoffs. The independent evaluator rated her as markedly ill at baseline, with significant impairment in multiple settings due to difficulties with anxiety and depression. By the end of treatment, Natalie demonstrated significant symptom reduction across all three internalizing domains (see Figure 1 for self- and parent-reports of symptom change from baseline to posttreatment). According to conventional criteria for evaluating clinical significance (Jacobson & Truax, 1991), her reduction in anxiety symptoms represented a reliable change.7 Natalie’s depression and somatic symptoms also substantially improved by the end of treatment, and came very close to meeting criteria for reliable change. By posttreatment, Natalie no longer met criteria for either of her anxiety or depression diagnoses, and was rated as “much improved” in her overall levels of functioning.
Figure 1.
Outcome trajectory for Natalie on youth- and parent-report of anxiety (SCARED), depression (MFQ), and somatic (CSI) symptoms
Alexis
Alexis was an 8-year-old African American female suffering from recurrent abdominal pain and a variety of other somatic complaints, as well as significant worry and difficulty separating from her mother. Although Alexis was referred for treatment by her gastrointestinal specialist due to concerns about ongoing, unexplained somatic complaints and some worries, at our intake we conceptualized Alexis as a primarily internalizing (and not primarily a chronic pain) patient because she and her mother both endorsed that Alexis’ somatic complaints were reliably triggered by episodes of anxiety. Alexis reported daily abdominal pain, occasional muscle aches and pains, and headaches twice a month, as well as feeling worried, tense, and stressed when separated from her mother (e.g., at school or a friend’s house), being concerned about her competence in school and social settings. Alexis’ comments about herself indicated that she had a very poor self-concept, and she reported ruminating about being inadequate and incompetent across school and social domains. Alexis and her mother both reported that Alexis almost always experienced pain or somatic discomfort related to separation and school, although she also reported somatic complaints unrelated to her anxiety. Her mother reported that Alexis was excessively self-conscious, overconcerned about academic competence, and worried about past events/behaviors, with subsequent related reassurance-seeking. Alexis’ mother viewed her as fragile, sick, and damaged, but also reported concerns that Alexis’ sensitivity made it difficult for her to manage everyday stressors, such as tests at school and reprimands at home.
Alexis and her mother both found the psychoeducation about anxiety and functional abdominal pain provided in session one very helpful. During the session, Alexis was able to identify the fight-or-flight response as occurring within her body when she experienced anticipatory anxiety about separation, and responded to the analogy of anxiety and somatic symptoms as an “overly sensitive alarm system.” In Session 2, Alexis’ mother was taught to reinforce healthy behaviors and “coach” her daughter to manage her anxiety and pain. The therapist taught her to validate Alexis’ pain but to encourage Alexis to actively engage in an activity as a strategy to take control of the situation. Relaxation was also taught as a strategy for Alexis to manage her pain and worry.
Problem solving was introduced in Session 3. The therapist helped Alexis reframe her pain and anxiety as a problem to be solved rather than as a reason to simply avoid school and peers. With the assistance of her therapist at the end of Session 3, Alexis was able to teach her mother how to use the problem-solving framework in relation to her own avoidance. Additional strategies to manage pain and worry that Alexis and her mother found particularly helpful included the use of distraction and coping statements. Alexis and her mother generated a list of activities that Alexis enjoyed independently and with others, and they even came up with the idea of creating a “distraction box” in which Alexis could put drawing paper, markers, CDs, books, and games to be used when she felt pain, anxiety, or felt “bad” for no reason. Alexis and her therapist developed coping statements to reinforce feelings of control; these were written down on index cards and included in her distraction box.
By the end of treatment, Alexis and her mother utilized the techniques taught in early treatment sessions (parent contingency management, relaxation, and problem solving) as strategies to aid Alexis in engaging in activities that she previously had great difficulty with. Alexis was able to consistently respond to both anxiety and pain by using her distraction box, relaxation skills, and coping statements. She also effectively used “I” statements to express her needs to her mother (e.g., “I would like to spend some more time with you”). Her mother consistently validated Alexis by acknowledging that her pain was real but that it was a problem to be solved, rather than a debilitating condition. As she and her mother practiced the skills, Alexis’ abdominal pain decreased and she was able to face challenging situations at school and separate from her mother more comfortably, which improved her functioning at school and with peers.
Therapy with Alexis also involved some challenges. Alexis’ mother initially viewed her daughter as sick and fragile and initially was resistant to challenging Alexis outside of session. Related to this, because Alexis was only 8 years old and some of her symptoms involved separation concerns, the therapist had to work with Alexis’ mother in order to negotiate appropriate parental responses and out-of-session assignments that Alexis’ mother felt comfortable following through with, and that would increase Alexis’ independence and address her somatic complaints in anticipation of and during separation. The therapist utilized the problem-solving framework with both Alexis and her mother in order to discuss what would happen if Alexis was not able to independently manage her somatic distress, as well as her anxiety, as she entered adolescence and adulthood.
At baseline Alexis was at or above clinical cutoff on anxiety8 and somatic9 symptom measures according to her and her mother’s reports, as well as elevated depressive10 symptom scores. The independent evaluator rated her as moderately ill at baseline, with significant impairment in multiple settings due to her feelings of anxiety and pain. By the end of the six treatment sessions, Alexis demonstrated significant symptom reduction across all three internalizing domains that either met or came close to reliable clinical change (see Figure 2 for for self- and parent-reports of symptom change from baseline to posttreatment).
Figure 2.
Outcome trajectory for Alexis on youth- and parent-report of anxiety (SCARED), depression (MFQ), and somatic (CSI) symptoms
Future Directions
In this report, we describe our group’s efforts to develop an internalizing toolbox for youths struggling with anxiety, depression, and/or somatic symptoms. At this point, our work has coalesced into two parallel protocols—one targeting the “emotional cluster” of anxiety and depression, and one targeting the “physical cluster” of anxious arousal and somatic symptoms. This two-protocol distinction, however, hides considerable overlap in the practical implementation of our treatments. As discussed in our case example, our “emotional” youths frequently have significant somatic symptoms, and our somaticizers display significant anxious and depressive features, even if they do not meet full criteria for diagnosis.
As we move toward the next generation of our toolbox, we face several decisions. First, we are weighing the value of complete integration of treatment techniques—developing a single common protocol addressing the emotional and physiological aspects of internalizing sensitivity. Pros of this approach include strong applicability to comorbid youths, both to their current symptom presentation and across time to their future selves. Given the lifetime comorbidity of anxiety, depression, and somatic symptoms, delivering an integrated approach designed to treat all three conditions can be thought of as not only current treatment but also as prevention of disorders within the internalizing cluster that have yet to develop. The second major argument for full integration is greater ease of training, implementation of treatment, and dissemination into practice of a single manual compared to the complexity of multiple protocols. The principal drawback to this full integration approach is the loss of some of the specific framing and content that is particularly applicable to different internalizing presentations. For example, youths with anxiety and/or depression (even with comorbid somatic complaints) are frequently comfortable using emotional and mental health language to describe stress and distress. In contrast, youths with somatic symptoms and high anxiety begin treatment with a very different language to describe their distress. Psychoeducation for these youths includes a more extensive and slower discussion of physical sensations as manifestations of emotional processes (e.g., a comprehensive review of all of the physical changes in the fight or flight response). Work with the parents of somatic youths also begins with a physical frame of reference, involves more extensive psychoeducation, and includes a more explicit discussion of contingency management around “sick behaviors” and handling school refusal.
An alternate approach for the next generation of our work would be to adopt a modularized toolbox design. This modular toolbox would perhaps have different “front ends” to match the symptom presentation and psychoeducational needs of youths with different patterns of internalizing comorbidity. After this more customized introduction, the tools provided to treat the internalizing disorders could be relatively interchangeable (e.g., problem solving could be taught in the same way to anxious, depressed, or somatic youths). The modular approach also allows for the editing of treatment techniques to match the specific, current symptoms displayed by youths—for example, depressed youths without extensive current somatic symptoms might skip relaxation training altogether. The advantages and disadvantages of the modular approach mirror those of the complete integration pathway. The modular approach may be time-efficient for youths and appear customized and very relevant to current concerns. However, this customization does not carry the potential benefit of teaching skills that may be useful in the future for these internalizing youths over development. Furthermore, the modular technique approach requires a high level of clinical judgment in the selection and omission of treatment elements—a challenge for training, supervision, and implementation by community providers.
As we wrestle with the challenges involved in further integration of these two treatment manuals into a single intervention, whether unified or modular, we use our clinical experiences with youths, and the emerging treatment literature, to guide us. Against this backdrop, our approach is likely to continue to emphasize simple, behavioral interventions. These techniques are highly experiential and engaging for youths and designed to work well across the school age through adolescent developmental period. This concrete behavioral focus is also intended to facilitate implementation of treatment by community practitioners without prior training in evidence-based treatments. Indeed, within our deployment-focused development framework, issues of training, supervision, cost-effectiveness, and provider preference are likely to shape the form of our work most strongly in the years to come.
Acknowledgments
Data collection and manuscript preparation were facilitated by support from the National Institute of Mental Health, the Robert Wood Johnson Foundation, and the William T. Grant Foundation. We gratefully acknowledge the following colleagues who aided in the conduct of these studies: Araceli Gonzalez, Carrie Fascetti, Jennifer Strohm, Sheree Shafer, Fallon Gallatin, Steve Savorelli, and Erin Warnick.
Footnotes
Details about these cases have been modified to protect the identity of the clients.
It should be noted that BBT for anxiety-depression has been administered by our group in both primary care and community clinic settings by nurses, social workers, and master’s-level psychologists, while BBT for anxiety-somatic complaints has been administered in medical settings by social workers. These differences have been more a function of practicality and convenience (e.g., developing relationships with specific settings, availability of on-site staff to be part of projects versus hiring staff expressly for the purpose of administering these protocols). Thus far, all BBT therapists across both protocols were supported by grants. We hope that the future forms of these protocols can be administered across health and mental health settings and by a variety of providers.
Natalie endorsed sufficient criteria to meet for a probable (missing one, non-core symptom) diagnosis of depression.
Self- and parent-reported anxiety were measured by the Screen for Child Anxiety Related Emotional Disorders (SCARED;Birmaher, Brent, Chiappetta, Bridge, Monga, & Baugher, 1999), a reliable and valid 41-item youth and parent-report questionnaire. Scores range from 0 to 82, with scores above 25 considered clinically significant.
Self- and parent-reported depression were measured by the Mood and Feelings Questionnaire (MFQ; Wood, Kroll, Moore, & Harrington, 1995), a reliable and valid 33-item youth and 34-item parent-report questionnaire. Scores range from 0 to 66 for the youth version, and 0 to 68 for the parent version, with scores above 25 considered clinically significant.
Self- and parent-reported somatic symptoms were measured by the Children’s Somatization Inventory (CSI; Walker & Garber, 2003), a reliable and valid 19-item youth and parent-report questionnaire. Scores range from 0 to 76.
Reliable change index (RCI) was calculated according to methods outlined by Jacobson and Truax (1991) using the following formula: where , x1 =pretreatment score, x2 =posttreatment score, s1 =standard deviation of the normal population, rxx =test-retest reliability of the measure. An RCI>1.96 represents reliable change (at α =.05). A change is said to be clinically significant if (a) there is a reliable change and (b) the pre- to posttreatment score on the measure crosses the clinical cutoff. Normative data used to measure RCI and clinical change in these cases were as follows: CSI: s1 =14.45, rxx =.81 (Walker & Garber, 2003); MFQ: s1 =12.40, rxx =.78 (Wood, Kroll, Moore, & Harrington, 1995); SCARED: s1 =12.14 (Wren, Bridge, & Birmaher, 2004), rxx =.86 (Birmaher et al., 1997).
Self- and parent-reported anxiety were measured by the Screen for Child Anxiety Related Emotional Disorders (SCARED;Birmaher, Brent, Chiappetta, Bridge, Monga, & Baugher, 1999), a reliable and valid 41-item youth and parent-report questionnaire. Scores range from 0 to 82, with scores above 25 considered clinically significant.
Self- and parent-reported somatic symptoms were measured by the Children’s Somatization Inventory (CSI; Walker & Garber, 2003), a reliable and valid 19-item youth and parent-report questionnaire. Scores range from 0 to 76.
Self- and parent-reported depression were measured by the Mood and Feelings Questionnaire (MFQ; Wood, Kroll, Moore, & Harrington, 1995), a reliable and valid 33-item youth and 34-item parent-report questionnaire. Scores range from 0 to 66 for the youth version, and 0 to 68 for the parent version, with scores above 25 considered clinically significant.
Contributor Information
V. Robin Weersing, San Diego State University/University of California, San Diego.
Michelle S. Rozenman, San Diego State University/University of California, San Diego
Maureen Maher-Bridge, Nationwide Children’s Hospital and The Ohio State University.
John V. Campo, Nationwide Children’s Hospital and The Ohio State University
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text revision. [Google Scholar]
- Andrews G. Comorbidity and the general neurotic syndrome. British Journal of Psychiatry. 1996;168:76–84. [PubMed] [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology, Psychiatry, and Allied Disciplines. 1999;40:57–87. [PubMed] [Google Scholar]
- Asarnow JR, Jaycox LH, Duan N, LaBorde AP, Rea MM, Murray P, Wells KB. Effectiveness of a quality improvement intervention for adolescent depression in primary care clinics: A randomized controlled trial. Journal of the American Medical Association. 2005;293:311–319. doi: 10.1001/jama.293.3.311. [DOI] [PubMed] [Google Scholar]
- Banks SM, Kerns RD. Explaining high rates of depression in chronic pain: A diathesis-stress framework. Psychological Bulletin. 1996;119:95–110. [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. New York: Guilford; 1988. [Google Scholar]
- Barlow DH. Unraveling the mysteries of anxiety and its disorders from the perspective of emotion theory. American Psychologist. 2000;55:1247–1263. doi: 10.1037//0003-066x.55.11.1247. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- Bell-Dolan D, Last CG, Strauss CC. Symptoms of anxiety disorders in normal children. Journal of the American Academy of Child & Adolescent Psychiatry. 1990;29:759–765. doi: 10.1097/00004583-199009000-00014. [DOI] [PubMed] [Google Scholar]
- Biederman J, Hirshfield-Becker DR, Rosenbaum JF, Herot C, Friedman D, Snidman N, Faraone SV. Further evidence of association between behavioral inhibition and social anxiety in children. American Journal of Psychiatry. 2001;158:1673–1679. doi: 10.1176/appi.ajp.158.10.1673. [DOI] [PubMed] [Google Scholar]
- Biederman J, Rosenbaum JF, Bolduc-Murphy EA, Faraone SV, Chaloff J, Hirshfeld DR, Kagan J. Behavioral inhibition as a temperamental risk factor for anxiety disorders. Child and Adolescent Psychiatric Clinics of North America. 1993;2:814–821. [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders scale (SCARED): A replication study. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric properties. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J, Dahl RE, Nelson B. Childhood and adolescent depression: A review of the past 10 years, Part I. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:1427–1439. doi: 10.1097/00004583-199611000-00011. [DOI] [PubMed] [Google Scholar]
- Bittner A, Egger HL, Erkanli A, Costello EJ, Foley DL, Angold A. What do childhood anxiety disorders predict? Journal of Child Psychology and Psychiatry. 2007;48:1174–1183. doi: 10.1111/j.1469-7610.2007.01812.x. [DOI] [PubMed] [Google Scholar]
- Brady EU, Kendall PC. Comorbidity of anxiety and depression in children and adolescents. Psychological Bulletin. 1992;111:244–255. doi: 10.1037/0033-2909.111.2.244. [DOI] [PubMed] [Google Scholar]
- Brent DA, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, Zelazny J. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: The TORDIA randomized controlled trial. Journal of the American Medical Association. 2008;299:901–913. doi: 10.1001/jama.299.8.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Holder D, Kolko D, Birmaher B, Baugher M, Roth C, Johnson B. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive treatments. Archives of General Psychiatry. 1997;54:877–885. doi: 10.1001/archpsyc.1997.01830210125017. [DOI] [PubMed] [Google Scholar]
- Bueno L. Gastrointestinal pharmacology: Irritable bowel syndrome. Current Opinions in Pharmacology. 2005;5:583–588. doi: 10.1016/j.coph.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Campo JV, Bridge J, Ehmann M, Altman S, Lucas A, Birmaher B, Brent DA. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics. 2004;113:817–824. doi: 10.1542/peds.113.4.817. [DOI] [PubMed] [Google Scholar]
- Campo JV, Di Lorenzo C, Chiappetta L, Bridge J, Colborn D, Gartner J, Brent DA. Adult outcomes of pediatric recurrent abdominal pain: Do they “just grow out of it”? Pediatrics. 2001;108:E1. doi: 10.1542/peds.108.1.e1. [DOI] [PubMed] [Google Scholar]
- Campo JV, Fritsch SL. Somatization in children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:1223–1235. doi: 10.1097/00004583-199411000-00003. [DOI] [PubMed] [Google Scholar]
- Campo JV, Fritz GK. Somatoform disorders. In: Martin A, Volkmar F, editors. Lewis’ Child and Adolescent Psychiatry. 4. Baltimore: Lippincott, Williams, & Wilkins; 2007. [Google Scholar]
- Campo JV, Perel J, Lucas A, Bridge J, Ehmann M, Kalas C, Brent DA. Citalopram treatment of pediatric recurrent abdominal pain and comorbid internalizing disorders: An exploratory study. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:1234–1242. doi: 10.1097/01.chi.0000136563.31709.b0. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, Poulton R. Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Celada P, Puig MV, Amargos-Bosch M, Adell A, Artigas F. The therapeutic role of 5-HT1A and 5-HT2A receptors in depression. Journal of Psychiatry and Neuroscience. 2004;29:252–265. [PMC free article] [PubMed] [Google Scholar]
- Chambers CT. The role of family factors in pediatric pain. In: McGrath PJ, Findley GA, editors. Pediatric pain: Biological and social context. Seattle: IASP Press; 2003. [Google Scholar]
- Chandra A, Scott MM, Jaycox LH, Meredith LS, Tanielian T, Burnam A. Racial/ethnic differences in teen and parent perspectives toward depression treatment. Journal of Adolescent Health. 2009;44:546–553. doi: 10.1016/j.jadohealth.2008.10.137. [DOI] [PubMed] [Google Scholar]
- Compton SN, March JS, Brent D, Albano AM, Weersing VR, Curry J. Cognitive-behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: An evidence-based medicine review. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:930–959. doi: 10.1097/01.chi.0000127589.57468.bf. [DOI] [PubMed] [Google Scholar]
- Davison I, Faull C, Nicol A. Research note: Temperament and behaviour in six-year-olds with recurrent abdominal pain: A follow up. Journal of Child Psychology and Psychiatry. 1986;27:539–544. doi: 10.1111/j.1469-7610.1986.tb00640.x. [DOI] [PubMed] [Google Scholar]
- Di Lorenzo C, Youssef N, Sigurdsson L, Scharff L, Griffiths J, Wald A. Visceral hyperalgesia in children with functional abdominal pain. Journal of Pediatrics. 2001;139:838–843. doi: 10.1067/mpd.2001.118883. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Hollon S, Dobson K, Schmaling K, Kohlenberg B, McGlinchey J, et al. Behavioral activation, cognitive therapy, and antidepressant medication in the treatment of major depression: Design and acute phase outcomes. In: Hollon SD Chair, editor. Behavioral activation, cognitive therapy, and antidepressant medication in the treatment of major depression; Symposium conducted at the annual meeting of the Association for Advancement of Behavior Therapy; Boston, Massachusetts. 2003. Nov, [Google Scholar]
- Dimidjian S, Hollon S, Dobson K, Schmaling K, Kohlenberg B, McGlinchey J, Jacobson NS. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology. 2006;74:658–670. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- Dorn L, Campo JV, Thato S, Dahl R, Lewin D, Chandra R, Di Lorenzo C. Psychological comorbidity and stress reactivity in children and adolescents with recurrent abdominal pain and anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42:66–75. doi: 10.1097/00004583-200301000-00012. [DOI] [PubMed] [Google Scholar]
- Edwards MC, Finney JW, Bonner MJ. Matching treatment with recurrent abdominal pain symptoms: An evaluation of dietary fiber and relaxation treatments. Behavior Therapy. 1991;22:257–267. [Google Scholar]
- Egger HL, Costello EJ, Erkanli A, Angold A. Somatic complaints and psychopathology in children and adolescents: Stomach aches, musculoskeletal pains, and headaches. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:852–860. doi: 10.1097/00004583-199907000-00015. [DOI] [PubMed] [Google Scholar]
- Eley TC, Sugden K, Corsico A, Gregory AM, Sham P, McGuffin P, Craig IW. Gene-environment interaction analysis of serotonin system markers with adolescent depression. Molecular Psychiatry. 2004;9:908–915. doi: 10.1038/sj.mp.4001546. [DOI] [PubMed] [Google Scholar]
- Feske U, Chambless DL. Cognitive behavioral versus exposure only treatment for social phobia: A meta-analysis. Behavior Therapy. 1995;26:695–720. [Google Scholar]
- Garber J, Zeman J, Walker L. Recurrent abdominal pain in children: Psychiatric diagnoses and parental psychopathology. Journal of the American Academy of Child & Adolescent Psychiatry. 1990;29:648–656. doi: 10.1097/00004583-199007000-00021. [DOI] [PubMed] [Google Scholar]
- Gazelle H, Rudolph KD. Moving toward and away from the world: Social approach and avoidance trajectories in anxious solitary youth. Child Development. 2004;75:829–849. doi: 10.1111/j.1467-8624.2004.00709.x. [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Brown CH, Hur K, Marcus SM, Bhaumik DK, Erkens JA, et al. Early evidence of the effects of regulators’ suicidality warnings on SSRI prescriptions and suicide in children and adolescents. American Journal of Psychiatry. 2007;164:1356–1363. doi: 10.1176/appi.ajp.2007.07030454. [DOI] [PubMed] [Google Scholar]
- Gladstone TR, Kaslow NJ. Depression and attributions in children and adolescents: A meta analytic review. Journal of Abnormal Child Psychology. 1995;23:597–606. doi: 10.1007/BF01447664. [DOI] [PubMed] [Google Scholar]
- Gould RA, Buckminster S, Pollack MH, Otto MW, Yap L. Cognitive-behavioral and pharmacological treatment for social phobia: A meta-analysis. Clinical Psychology: Science and Practice. 1997;4:291–306. [Google Scholar]
- Gould RA, Otto MW, Pollack MH. A meta-analysis of treatment outcome for panic disorder. Clinical Psychology Review. 1995;15:819–844. [Google Scholar]
- Grob GN. Origins of DSM-I: A study in appearance and reality. American Journal of Psychiatry. 1991;194:421–431. doi: 10.1176/ajp.148.4.421. [DOI] [PubMed] [Google Scholar]
- Gureje O, Simon GE, Von Korff M. A cross-national study of the course of persistent pain in primary care. Pain. 2001;92:195–200. doi: 10.1016/s0304-3959(00)00483-8. [DOI] [PubMed] [Google Scholar]
- Hariri AR, Mattay VS, Tessitore A, Kolachana B, Fera F, Goldman D, Weinberger D. Serotonin transporter genetic variation and the response of the human amygdala. Science. 2002;297:400–403. doi: 10.1126/science.1071829. [DOI] [PubMed] [Google Scholar]
- Hettema JM. What is the genetic relationship between anxiety and depression? American Journal of Medical Genetics Part C, Seminars in medical genetics. 2008;148C:140–146. doi: 10.1002/ajmg.c.30171. [DOI] [PubMed] [Google Scholar]
- Hopko DR, Lejuez CW, Hopko SD. Behavioral activation as an intervention for coexistent depressive and anxiety symptoms. Clinical Case Studies. 2004;3:37–48. [Google Scholar]
- Husain K, Browne T, Chalder T. A review of psychological models and interventions for medically unexplained somatic symptoms in children. Child and Adolescent Mental Health. 2007;12:2–7. doi: 10.1111/j.1475-3588.2006.00419.x. [DOI] [PubMed] [Google Scholar]
- Jackson JL, O’Malley PG, Tomkins G, Balden E, Santoro J, Kroenke K. Treatment of functional gastrointestinal disorders with antidepressant medications: Of meta-analysis. American Journal of Medicine. 2000;108:65–72. doi: 10.1016/s0002-9343(99)00299-5. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Dobson KS, Truax PA, Addis ME, Koerner K, Gollan JK, Prince A. A component analysis of cognitive-behavioral treatment for depression. Journal of Consulting and Clinical Psychology. 1996;64:295–304. doi: 10.1037//0022-006x.64.2.295. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- James A, Soler A, Weatherall R. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database of Systematic Reviews. 2005;(4):Art. No.: CD004690. doi: 10.1002/14651858. [DOI] [PubMed] [Google Scholar]
- Kashani JH, Lababidi Z, Jones RS. Depression in children and adolescents with cardiovascular symptomatology: The significance of chest pain. Journal of the American Academy of Child & Adolescent Psychiatry. 1982;21:187–189. doi: 10.1016/s0002-7138(09)60918-3. [DOI] [PubMed] [Google Scholar]
- Keller M, Lavori P, Wunder J, Beardslee W, Schwartz C, Roth J. Chronic course of anxiety disorders in children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:595–599. doi: 10.1097/00004583-199207000-00003. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, Southam-Gerow M, Henin A, Warman M. Therapy for youths with anxiety disorders: A second randomized clinical trial. Journal of Consulting and Clinical Psychology. 1997;65:366–380. doi: 10.1037//0022-006x.65.3.366. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Pimentel SS. On the physiological symptom constellation in youth with Generalized Anxiety Disorder (GAD) Journal of Anxiety Disorders. 2003;17:211–221. doi: 10.1016/s0887-6185(02)00196-2. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Thornton LM, Gardner CO. Genetic risk, number of previous depressive episodes, and stressful life events in predicting onset of major depression. American Journal of Psychiatry. 2001;158:582–586. doi: 10.1176/appi.ajp.158.4.582. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The prevalence of psychiatric comorbidity. In: Wetzler S, Sanderson WC, editors. Treatment strategies for patients with psychiatric comorbidity. New York: John Wiley & Sons; 1997. [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingery JN, Roblek TL, Suveg C, Grover RL, Sherrill JT, Bergman RL. They’re not just “little adults”: Developmental considerations for implementing cognitive-behavioral therapy with anxious youth. Journal of Cognitive Psychotherapy. 2006;20:263–273. [Google Scholar]
- Klein RG. Anxiety disorders. Journal of Child Psychology and Psychiatry. 2009;50:153–162. doi: 10.1111/j.1469-7610.2008.02061.x. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Regier DA. APA Division of Research Report. 2009. Mar, Current activities: Report of the DSM-V Task Force. DSM-V Task Force and Work Group update. [Google Scholar]
- Lanzenberger RR, Mitterhauser M, Spindelegger C, Wadsak W, Klein N, Mein L, Tauscher J. Reduced serotonin-1A receptor binding in social anxiety disorder. Biological Psychiatry. 2007;61:1081–1089. doi: 10.1016/j.biopsych.2006.05.022. [DOI] [PubMed] [Google Scholar]
- Leonard BE. HPA and immune axes in stress: Involvement of the serotonergic system. Neuroimmunomodulation. 2007;13:268–276. doi: 10.1159/000104854. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. Journal of Abnormal Psychology. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- Libby AM, Brent DA, Morrato EH, Orton HD, Allen RD, Valuck RJ. Decline in treatment of pediatric depression after FDA advisory on risk of suicidality with SSRIs. American Journal of Psychiatry. 2007;164:884–891. doi: 10.1176/ajp.2007.164.6.884. [DOI] [PubMed] [Google Scholar]
- Libby AM, Orton HD, Valuck RJ. Persisting decline in depression treatment after FDA warnings. Archives of General Psychiatry. 2009;66:633–639. doi: 10.1001/archgenpsychiatry.2009.46. [DOI] [PubMed] [Google Scholar]
- Lieb R, Meinlschmidt G, Araya R. Epidemiology of the association between somatoform disorders and anxiety and depressive disorders: An update. Psychosomatic Medicine. 2007;69:860–863. doi: 10.1097/PSY.0b013e31815b0103. [DOI] [PubMed] [Google Scholar]
- Lipsitz JS, Masia-Warner C, Apfel H, Marans Z, Hellstern B, Forand N, Fyer AJ. Anxiety and depressive symptoms and anxiety sensitivity in youngsters with noncardiac chest pain and benign heart murmurs. Journal of Pediatric Psychiatry. 2004;29:607–612. doi: 10.1093/jpepsy/jsh062. [DOI] [PubMed] [Google Scholar]
- March JS, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, et al. The Treatment for Adolescents with Depression Study (TADS): Long-term effectiveness and safety outcomes. Archives of General Psychiatry. 2008;64:1132–1143. doi: 10.1001/archpsyc.64.10.1132. [DOI] [PubMed] [Google Scholar]
- Masek BJ, Russo DC, Varni JW. Behavioral approaches to the management of chronic pain in children. Pediatric Clinics of North America. 1984;31:1113–1131. doi: 10.1016/s0031-3955(16)34687-9. [DOI] [PubMed] [Google Scholar]
- Masia Warner C, Reigada LC, Fisher PH, Saborsky AL, Benkov KJ. CBT for anxiety and associated somatic complaints in pediatric medical settings: an open pilot study. Journal of Clinical Psychology in Medical Settings. 2009;16:169–177. doi: 10.1007/s10880-008-9143-6. [DOI] [PubMed] [Google Scholar]
- Mathew SJ, Coplan JD, Gorman JM. Neurobiological mechanisms of social anxiety disorder. American Journal of Psychiatry. 2001;158:1558–1567. doi: 10.1176/appi.ajp.158.10.1558. [DOI] [PubMed] [Google Scholar]
- Mogg K, Bradley BP. Attentional bias in generalized anxiety disorder versus depressive disorder. Cognitive Therapy and Research. 2005;29:29–45. [Google Scholar]
- Ollendick TH, King NJ. Empirically supported treatments for children with phobic and anxiety disorders. Journal of Clinical Child Psychology. 1998;27:156–167. doi: 10.1207/s15374424jccp2702_3. [DOI] [PubMed] [Google Scholar]
- Pine D, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depression disorders. Archives of General Psychiatry. 1998;55:56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- Price D. Psychological and neural mechanisms of the affective dimension of pain. Science. 2000;288:1769–1772. doi: 10.1126/science.288.5472.1769. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. Journal of the American Medical Association. 1990;264:2511–2518. [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Are adolescents changed by an episode of major depression? Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:1289–1298. doi: 10.1097/00004583-199411000-00010. [DOI] [PubMed] [Google Scholar]
- Rushton JL, Clark SJ, Freed GL. Primary care role in the management of childhood depression: A comparison of pediatricians and family physicians. Pediatrics. 2000;105:957–962. [PubMed] [Google Scholar]
- Sanders MR, Rebgetz M, Morrison M, Bor W, Gordon A, Dadds M, Shepherd R. Cognitive-behavioral treatment of recurrent nonspecific abdominal pain in children: An analysis of generalization, maintenance, and side effects. Journal of Consulting and Clinical Psychology. 1989;57:294–300. doi: 10.1037//0022-006x.57.2.294. [DOI] [PubMed] [Google Scholar]
- Sanders M, Shepherd R, Cleghorn G, Woolford H. The treatment of recurrent abdominal pain in children: A controlled comparison of cognitive-behavioral family intervention and standard pediatric care. Journal of Consulting and Clinical Psychology. 1994;62:306–314. doi: 10.1037//0022-006x.62.2.306. [DOI] [PubMed] [Google Scholar]
- Scharff L. Recurrent abdominal pain in children: A review of psychological factors and treatment. Clinical Psychology Review. 1997;17:145–166. doi: 10.1016/s0272-7358(96)00001-3. [DOI] [PubMed] [Google Scholar]
- Stahl S. Antidepressants and somatic symptoms: Therapeutic actions are expanding beyond affective spectrum disorders to functional somatic syndromes. Journal of Clinical Psychiatry. 2003;64:745–746. [PubMed] [Google Scholar]
- Stevens J, Wang W, Fan L, Edwards MC, Campo JV, Gardner W. Parental attitudes toward children’s use of antidepressants and psychotherapy. Journal of Child and Adolescent Psychopharmacology. 2009;19:289–296. doi: 10.1089/cap.2008.0129. [DOI] [PubMed] [Google Scholar]
- Szigethy E, Kenney E, Carpenter J, Hardy DM, Faircough D, Bousvaros A, et al. Cognitive-behavioral therapy for adolescents with inflammatory bowel disease and subsyndromal depression. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46:1290–1298. doi: 10.1097/chi.0b013e3180f6341f. [DOI] [PubMed] [Google Scholar]
- Szigethy E, Whitton SW, Levy-Warren A, DeMaso DR, Weisz J, Beardslee WR. Cognitive-behavioral therapy for depression in adolescents with inflammatory bowel disease: A pilot study. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:1469–1477. doi: 10.1097/01.chi.0000142284.10574.1f. [DOI] [PubMed] [Google Scholar]
- Tsao JC, Lu Q, Kim SC, Zeltzer LK. Relationships among anxious symptomatology, anxiety sensitivity and laboratory pain responsivity in children. Cognitive Behaviour Therapy. 2006;35:207–215. doi: 10.1080/16506070600898272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tunaoglu FS, Olgunturk R, Akcabay S, Oguz D, Gucuyener K, Demirsoy S. Chest pain in children referred to a cardiology clinic. Pediatric Cardiology. 1995;16:69–72. doi: 10.1007/BF00796820. [DOI] [PubMed] [Google Scholar]
- Unüetzer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, Harpole L, et al. Collaborative care management of late-life depression in the primary care setting: A randomized controlled trial. Journal of the American Medical Association. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- U.S. Food and Drug Administration. Public Health Advisory: Suicidality in children and adolescents being treated with antidepressant medications. 2004 Oct 15; Retrieved September 29, 2005, from. http://www.fda.gov/cder/drug/antidepressants/default.htm.
- Vaccarino AL, Sills TL, Evans KR, Kalali AH. Prevalence and association of somatic symptoms in patients with major depressive disorder. Journal of Affective Disorders. 2008;110:270–276. doi: 10.1016/j.jad.2008.01.009. [DOI] [PubMed] [Google Scholar]
- Walker LS, Claar RL, Garber J. Social consequences of children’s pain: When do they encourage symptom maintenance? Journal of Pediatric Psychology. 2002;27:689–698. doi: 10.1093/jpepsy/27.8.689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker LS, Garber J. Manual for the Children’s Somatization Inventory. Nashville, TN: Vanderbilt University Medical Center; 2003. [Google Scholar]
- Walker LS, Garber J, Greene J. Psychosocial correlates of recurrent childhood pain: A comparison of pediatric patients with recurrent abdominal pain. Journal of Abnormal Child Psychology. 1993;102:248–258. doi: 10.1037//0021-843x.102.2.248. [DOI] [PubMed] [Google Scholar]
- Walker LS, Garber J, Smith CA, Van Slyke DA, Claar RL. The relation of daily stressors to somatic and emotional symptoms in children with and without recurrent abdominal pain. Journal of Consulting and Clinical Psychology. 2001;69:85–91. [PMC free article] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, Kendall P. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. The New England Journal of Medicine. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weersing VR, Gonzalez A, Campo JV, Lucas AN. Brief behavioral therapy for pediatric anxiety and depression: Piloting an integrated treatment approach. Cognitive and Behavioral Practice. 2008;15:126–139. [Google Scholar]
- Weissman MM, Wolk S, Wickramaratne P, Goldstein RB, Adams P, Greenwald S, Steinberg D. Children with prepubertal-onset major depressive disorder and anxiety grown up. Archives of General Psychiatry. 1999;56:794–801. doi: 10.1001/archpsyc.56.9.794. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Weersing VR. Psychotherapy with children and adolescents: Efficacy, effectiveness, and developmental concerns. In: Cicchetti D, Toth SL, editors. Rochester symposium on developmental psychopathology: Vol. 9. Developmental approaches to prevention and intervention. Rochester, NY: University of Rochester Press; 1999. pp. 341–386. [Google Scholar]
- Wisdom JP, Clarke GN, Green CA. What teens want: Barriers to seeking care for depression. Mental Health Services Research. 2006;33:133–145. doi: 10.1007/s10488-006-0036-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood A, Kroll L, Moore A, Harrington R. Properties of the Mood and Feelings Questionnaire in adolescent psychiatric outpatients: A research note. Journal of Child Psychology and Psychiatry. 1995;36:327–334. doi: 10.1111/j.1469-7610.1995.tb01828.x. [DOI] [PubMed] [Google Scholar]
- Wren FJ, Bridge JA, Birmaher B. Screening for childhood anxiety symptoms in primary care: Integrating child and parent reports. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:1364–1371. doi: 10.1097/01.chi.0000138350.60487.d3. [DOI] [PubMed] [Google Scholar]
- Young BJ, Beidel DC, Turner SM, Ammerman RT, McGraw K, Coaston SC. Pretreatment attrition and childhood social phobia: Parental concerns about medication. Journal of Anxiety Disorders. 2006;20:1133–1147. doi: 10.1016/j.janxdis.2006.03.007. [DOI] [PubMed] [Google Scholar]