Abstract
Warfarin-induced skin necrosis is an infrequent complication occurring in individuals under warfarin treatment who have a thrombophilic history or after administration of large loading doses of warfarin particularly without simultaneous initial use of heparin. A 62-year-old lady developed skin necrosis 4 days after initiating warfarin therapy of 5 mg daily without initial co-administration of heparin. The patient had a normal clotting profile. Skin necrosis progressed to eschar formation after cessation of warfarin and heparinization stopped expanding. Warfarin was reintroduced at 2 mg daily, initially together with low molecular weight heparin. Autolytic debridement of the necrotic tissue was followed by healing of the cutaneous deficit by secondary intention. Prompt diagnosis and discontinuation of warfarin are crucial for the prognosis.
Keywords: Anticoagulants, Necrotic lesions, Warfarin
INTRODUCTION
Skin necrosis from warfarin is an uncommon but serious condition, occurring in 1:10,000 patients who receive the drug, with a female:male ratio of 1:4. Obesity, perimenopausal age, viral infections, hepatic disease, and drug interactions are other predisposing factors1. Deficiency of protein C, protein S or Factor V Leiden, antithrombin III, hyperhomocysteinaemia, and antiphospholipid antibodies are common underlying risk factors1-5. Warfarinization with large loading doses or without initial concomitant heparinization, are common clues in the clinical history, as in the patient presented herein.
CASE REPORT
A 62-year-old woman was referred for skin necrosis on the lateral aspect of the right thigh (Fig. 1A), 12 days after admission for refractory atrial fibrillation secondary to mitral valve stenosis and insufficiency. Her ventricular rate had been controlled by isoprolol and the patient had been started immediately on 5 mg warfarin per day without simultaneous administration of heparin. On day 4, she developed painful ecchymosis of the lateral surface of the right thigh, initially misinterpreted as a hematoma, and the warfarin was reduced to 2 mg daily. On day 6, skin necrosis with eschar formation developed, and warfarin therapy was resumed to 1 mg per day. On day 12, the patient presented with a full thickness cutaneous necrosis. A laboratory workup indicated a normal clotting profile (Table 1). A histopathologic examination of incisional cutaneous biopsy was suggestive of warfarin-induced skin necrosis (Fig. 1B).
Fig. 1.

(A) Clinical appearance of the patient and (B) histopathologic examination of the cutaneous necrosis (H&E, ×200): skin necrosis with evidence of fibrin deposits in the post capillary venules, absence of arteriolar thrombosis, and lack of vascular or perivascular inflammation.
Table 1.
Coagulation screening of the patient
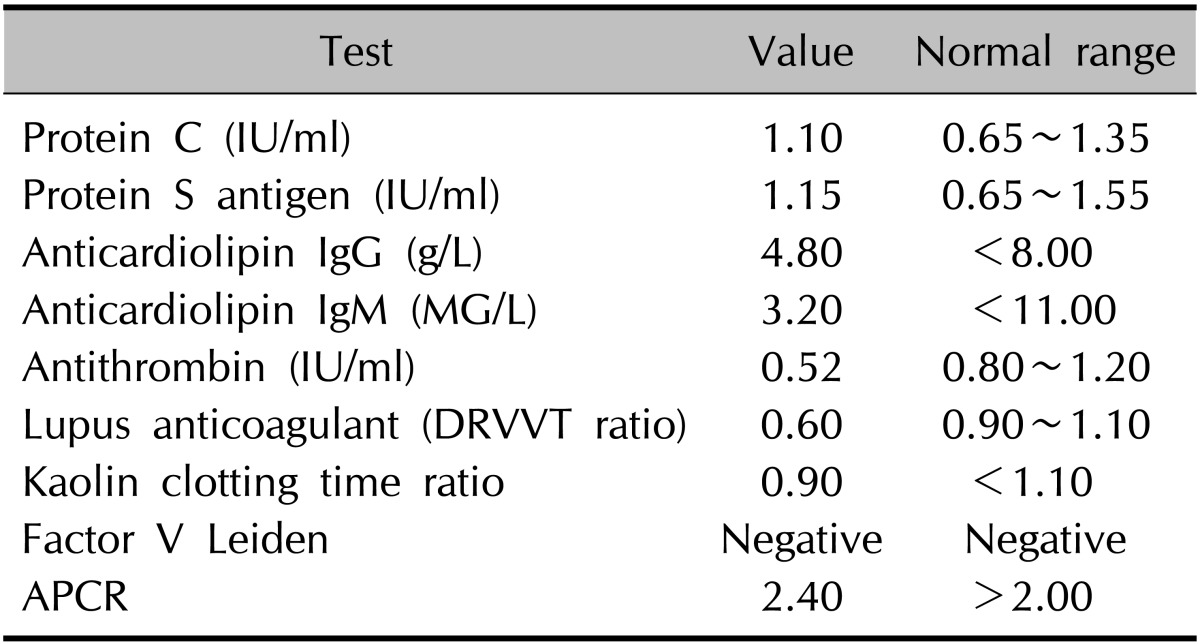
Prolonged dilute Russell's viper venom time (DRVVT) was used to detect lupus anticoagulant. Ig: immunoglobulin, APCR: activated protein C resistance.
Accordingly, warfarin was discontinued and intravenous unfractionated heparin therapy was initiated. As the patient refused surgery, conservative autolytic debridement with hydrogel and hydrocolloid dressings was achieved, and the cutaneous deficit was healed by secondary intention. Unfractionated heparin was replaced with low-molecular weight (LMW) heparin for 17 days. Subsequently, warfarin was re-introduced at a daily dose of 2 mg with continuation of heparin, until international normalized ratio (INR) was within the therapeutic range. The cutaneous lesion healed with a scar and the patient developed no further skin necrosis during 15 months of follow-up.
DISCUSSION
Skin reactions associated with warfarin commonly occur 3 to 5 days after initiating of treatment. Breasts, buttocks, abdomen, thighs, and calves are more susceptible probably because of the reduced blood supply to adipose tissue. Rapid progression of plaques to skin necrosis increases morbidity1,3.
Skin necrosis usually occurs shortly after initiating warfarin therapy with a large loading dose or without concomitant heparin. Warfarin inactivates vitamin K-dependent clotting factors II, VII, IX, and X. At the same time, vitamin K-dependent proteins C and S are inactivated. This may cause a paradoxical hypercoagulable milieu in which microthrombi develop in cutaneous and subcutaneous venules, as the concentration of anticoagulant protein C falls more rapidly than other vitamin K-dependent precoagulant factors, which have longer half-lives1-3. However, the clotting profile of our patient was normal.
The differential diagnosis included hematoma, disseminated intravascular coagulation, purpura fulminans, necrotizing fasciitis, cellulitis, venous gangrene and calciphylaxis1,6,7. The diagnosis was mainly clinical, as protein C and S concentration tests are neither sensitive nor specific. Cessation of warfarin treatment is the mainstay of treatment. If anticoagulation is essential, intravenous heparin should be administered, followed by LMW heparin until the necrosis shows signs of improvement. Cautious reintroduction of warfarin can be attempted in combination with heparin. The latter should be stopped when INR reaches therapeutic levels. Occasionally vitamin K is used to reverse untoward warfarin effects. Protein C concentrates can be used for life-threatening coagulation. Prostacyclin is also effective6. Large areas of skin necrosis may require debridement and skin grafting.
Warfarin-induced skin necrosis should be suspected in all patients who undergo aggressive warfarinization, even with an initially normal clotting profile. Prompt diagnosis and discontinuation of warfarin are crucial for the prognosis.
ACKNOWLEDGMENT
We are grateful to Mrs. Lambropoulou Maria, Assistant Professor of Histology-Embryology, Democritus University in Thrace, for the histopathological evaluation of the specimen.
References
- 1.Eby CS. Warfarin-induced skin necrosis. Hematol Oncol Clin North Am. 1993;7:1291–1300. [PubMed] [Google Scholar]
- 2.Broekmans AW, Bertina RM, Loeliger EA, Hofmann V, Klingemann HG. Protein C and the development of skin necrosis during anticoagulant therapy. Thromb Haemost. 1983;49:251. [PubMed] [Google Scholar]
- 3.Wattiaux MJ, Hervé R, Robert A, Cabane J, Housset B, Imbert JC. Coumarin-induced skin necrosis associated with acquired protein S deficiency and antiphospholipid antibody syndrome. Arthritis Rheum. 1994;37:1096–1100. doi: 10.1002/art.1780370716. [DOI] [PubMed] [Google Scholar]
- 4.Moreb J, Kitchens CS. Acquired functional protein S deficiency, cerebral venous thrombosis, and coumarin skin necrosis in association with antiphospholipid syndrome: report of two cases. Am J Med. 1989;87:207–210. doi: 10.1016/s0002-9343(89)80698-9. [DOI] [PubMed] [Google Scholar]
- 5.Dahlbäck B. Protein S and C4b-binding protein: components involved in the regulation of the protein C anticoagulant system. Thromb Haemost. 1991;66:49–61. [PubMed] [Google Scholar]
- 6.Nazarian RM, Van Cott EM, Zembowicz A, Duncan LM. Warfarin-induced skin necrosis. J Am Acad Dermatol. 2009;61:325–332. doi: 10.1016/j.jaad.2008.12.039. [DOI] [PubMed] [Google Scholar]
- 7.Warkentin TE. Venous limb gangrene during warfarin treatment of cancer-associated deep venous thrombosis. Ann Intern Med. 2001;135:589–593. doi: 10.7326/0003-4819-135-8_part_1-200110160-00009. [DOI] [PubMed] [Google Scholar]


