Abstract
Implication for health policy/practice/research/medical education:
Much has been published on the epidemiology and clinicopathological characteristics of IgM nephropathy, but there is little information on the etiology,pathogenesis and specific therapy of the disease. Controversy still shrouds the definition and nosologic status of the disease. Well-coordinated and concerted international efforts and collaboration between researchers in the developing and developed countries are needed to make further progress on the above aspects of the disease.
Keywords: IgM nephropathy, Minimal change disease, IgA nephropathy
A recent issue of this journal carried a review article on IgM nephropathy (IgMN) by Professor Vanikar with a question right in the title as “can we still ignore it?” (1). This was a timely call for action on this subject, but I contend her point that the disease is being ignored. Indeed, the disease is not being neglected in terms of under-diagnosis but rather some aspects of the disease are not being investigated at par with some other features such as the epidemiological and clinicopathological parameters. The point to ponder is why the disease is still controversial even after almost five and half decades after its initial description in mid and late 1970s (2-6). There are several reasons for this state of affairs. Some important points are discussed in this editorial.
First of all, there are serious and largely unresolved definitional problems (5-14). What constitutes IgMN on light microscopy (LM) and more importantly on immunofluorescence (IF)? To give an example, I have put a picture of LM of one representative glomerulus from a biopsy and IgM immunostaining in Figure 1. What do the readers think of the diagnosis in this case? I can bet that it will invoke a mixture of responses. Some will call it IgMN, while others as minimal change disease (MCD) with trace or 1+ IgM deposits. As a matter of fact, there are as many definitions of the disease as there are studies (1-14). To put in other words, there is no universally accepted definition of the disease at present. Some authors have included cases with trace positivity of IgM on IF as IgMN, while others have set the threshold of IgM positivity much higher (1,5-13). This will obviously have affected the results and conclusions about the clinicopathological presentation, therapy and prognosis of the disease. So, the question is how to tackle this problem of definition? It can only be tackled efficiently by a dedicated and concerted international effort by all the concerned health care professionals.
Figure 1.
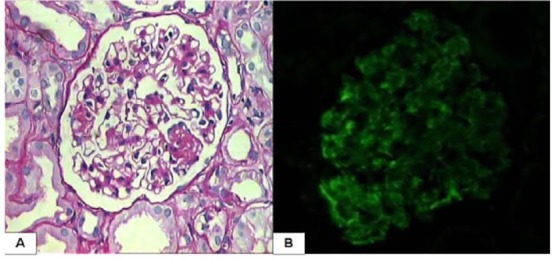
Two representative pictures, one of light microscopy and other of immunofluorescence from a renal biopsy from an 8 year old child with steroid dependant nephrotic syndrome. The interpretation of these findings is open to all the readers. A. This is high-power view of one representative glomerulus from the above case. (PAS, ×400). B. Immunofluorescence staining for IgM by the direct technique on the same biopsy. (IgM, ×400).
Second, the pathogenesis of the condition is still largely unknown and more importantly, little investigated. Only occasional studies are available in the literature, which have specifically addressed this issue and these have yielded somewhat conflicting results (10-16). Majority of the studies, especially those reported from third world countries, on IgMN have focused on determining the epidemiology, demography and clinicopathological correlates of the disease (17-27). The lack of pathogenetic studies is, in large part, attributable to the lack of interest of Western researchers in the disease (1,24,25,28). Here, collaboration between researchers in the developing countries, where there is sufficient raw material in the form of disease burden, with those in the developed nations, where research facilities and funding abound, can help in elucidating the mechanistic pathways involved in the disease. This will not only shed light on the pathophysiology of the disease but also pave way for the tailored treatment of the condition in future (28).
Although a few studies have addressed the assessment of prognostic factors, both clinical and histopathological in nature, much remains to be done on this front as well (19,20-23). Here, the example of Oxford classification of IgA nephropathy (IgAN) can serve as a useful blueprint for action (29). Since the lesions of IgMN closely resemble those of IgAN, the Oxford classification can be tested for its utility in this disease. Perhaps a slight modification of the above scheme may serve the purpose more usefully. Last but not the least, the issue of therapy and prognosis also warrant large-scale, robust and prospective studies, as only about one third of all patients are steroid responsive in this disease. For the remaining majority of patients, optimal treatment is still elusive (1,25).
However, the scenario is not entirely gloomy. Not all aspects of the disease are poorly studied or characterized. A few citations will suffice to illustrate this point. The author’s group has published extensively on the epidemiology, clinicopathological correlations and short to medium term outcome of the disease in some of the largest studies on IgMN in the world literature (22,23). We have also published fairly comprehensive reviews on this topic (25). Our group is actively following a very large number of patients, especially children with the disease and plan to publish its long term experience of the disease. Our neighbors from India have rivaled us closely on this front also. Professor Vanikar’s group has also come up with their part of experience with the disease both in children and adults (20,21). It is interesting to note, that the studied disease characteristics are more or less similar in this region (28). The Finnish group has also worked extensively on this disease with one of the largest and longest follow-up study originating from their experience (8,14,19).
Most of the literature on IgMN and the discussion above is concerned with the disease in native kidneys. Occasional case reports are also available on the involvement of the transplanted kidney by the disease, either in de novo or recurrent form (30-32). Although, we have not yet systematically analyzed our kidney transplant cases of IgMN nephropathy, we have a small number of irrefutable cases in our files. Indeed, renal allografts serve as very useful models for the study of natural history and evolution of many glomerulopathies and IgMN is one of the examples that can be studied in detail in this setting.
In conclusion, although much has been published on the epidemiology and clinicopathological characteristics of IgMN, there is little information on the etiology, pathogenesis and specific therapy of the disease. Controversy still shrouds the definition and nosologic status of the disease. Concerted and well coordinated international efforts and collaboration between researchers in the developing and developed countries are needed to resolve these issues.
Author’s contribution
MM is the single author of the manuscript.
Conflict of interests
The author declared no competing interests.
Funding/Support
None.
Please cite this paper as: Mubarak M. IgM nephropathy; time to act. J Nephropathol. 2014; 3(1): 22-25. DOI: 10.12860/jnp.2014.05
References
- 1.Vanikar A. IgM nephropathy: Can we still ignore it. J Nephropathol. 2013;2(2):98–103. doi: 10.12860/JNP.2013.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van de Putte LB, DeLaRiviere GB, Van Breda Vriesman PJ. Recurrent or persistent hematuria, sign of mesangial immune-complex deposition. N Engl J Med. 1974;290:1165–70. doi: 10.1056/NEJM197405232902104. [DOI] [PubMed] [Google Scholar]
- 3.Cohen AH, Border WA, Glassock RJ. Nephrotic syndrome with glomerular mesangial IgM deposits. Lab Invest. 1978;38(5):610–9. [PubMed] [Google Scholar]
- 4.Bhasin HK, Abeulo JG, Nayak R, Esparza AR. Mesangial proliferative glomerulonephritis. Lab Invest. 1978;39(1):21–9. [PubMed] [Google Scholar]
- 5.Lawler W, Williams G, Tarpey P, Mallick NP. IgM associated primary diffuse mesangial proliferative glomerulonephritis. J Clin Pathol. 1980;33(11):1029–1038. doi: 10.1136/jcp.33.11.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mampaso F, Gonzalo A. et al. Mesangial deposits of IgM in patients with the nephrotic syndrome. Clin Nephrol. 1981;16(5):230–4. [PubMed] [Google Scholar]
- 7.Cavalo T, Johnson MP. Immunopathologic study of minimal change glomerular disease with mesangial IgM deposits. Nephron. 1981;27(6):281–4. doi: 10.1159/000182071. [DOI] [PubMed] [Google Scholar]
- 8.Helin H, Mustonen J, Pasternack A, Antonen J. IgM associated glomerulonephritis. Nephron. 1982;31(1):11–16. doi: 10.1159/000182598. [DOI] [PubMed] [Google Scholar]
- 9.Hsu HC, Chen WY, Lin GJ, Chen L, Kao S-L, Huang CC. et al. Clinical and immunopathologic study of mesangial IgM nephropathy: report of 41 cases. Histopathology. 1984;8(3):435–46. doi: 10.1111/j.1365-2559.1984.tb02355.x. [DOI] [PubMed] [Google Scholar]
- 10.Pardo V, Riesgo I, Zilleruelo G, Strauss J. The clinical significance of mesangial IgM deposits and mesangial hypercellularity in minimal change nephrotic syndrome. Am J Kidney Dis. 1984;3(4):264–9. doi: 10.1016/s0272-6386(84)80043-8. [DOI] [PubMed] [Google Scholar]
- 11.Ji-Yun Y, Melvin T, Sibley R, Michael AF. No evidence for a specific role of IgM in mesangial proliferation of idiopathic nephrotic syndrome. Kidney Int. 1984;25(1):100–6. doi: 10.1038/ki.1984.14. [DOI] [PubMed] [Google Scholar]
- 12.Kopolovic J, Shvil Y, Pomeranz A, Ron N, Rubinger D, Oren R. IgM nephropathy: morphological study related to clinical findings. Am J Nephrol. 1987;7(4):275–80. doi: 10.1159/000167485. [DOI] [PubMed] [Google Scholar]
- 13.Border WA. Distinguishing minimal change disease from mesangial disorders. Kidney Int. 1988;34(3):419–24. doi: 10.1038/ki.1988.197. [DOI] [PubMed] [Google Scholar]
- 14.Saha H, Mustonen J, Pasternack A, Helin H. Clinical follow up of 54 patients with IgM nephropathy. Am J Nephrol. 1989;9(2):124–8. doi: 10.1159/000167950. [DOI] [PubMed] [Google Scholar]
- 15.Al Eisa A, Carner JE, Lirenman DS, Magil AB. Childhood IgM nephropathy: comparison with minimal change disease. Nephron. 1996;72(1):37–43. doi: 10.1159/000188804. [DOI] [PubMed] [Google Scholar]
- 16.Kishimoto H, Arakawa M. Clinico-pathological characterization of mesangial proliferative glomerulonephritis with predominant deposition of IgM. Clin Exp Nephrol. 1999;3(2):110–5. [Google Scholar]
- 17.Donia AF, Sobh MA, Moustafa FE, Bakr MA, Foda MA. Clinical significance and long term evolution of minimal change histopathologic variants and of IgM nephropathy among Egyptians. J Nephrol. 2000;13(4):275–81. [PubMed] [Google Scholar]
- 18.Chan YH, Wong KM, Choi KS, Chak WL, Cheung CY. Clinical manifestation and progression of IgM mesangial nephropathy: a single center perspective. Hong Kong J Nephrol. 2000;2(1):23–6. [Google Scholar]
- 19.Myllymaki J, Saha H, Mustonen J, Helin H, Pasternack A. IgM nephropathy: clinical picture and long term prognosis. Am J Kidney Dis. 2003;41(2):343–50. doi: 10.1053/ajkd.2003.50042. [DOI] [PubMed] [Google Scholar]
- 20.Singhai AM, Vanikar AV, Goplani KR, Kanodia KV, Patel RD, Suthar KS. et al. Immunoglobulin M nephropathy in adults and adolescents in India: a single center study of natural history. Indian J Pathol Microbiol. 2011;54(1):3–6. doi: 10.4103/0377-4929.77315. [DOI] [PubMed] [Google Scholar]
- 21.Vanikar AV, Kanodia KV, Patel RS, Suthar KS, Patel HV, Gumber MR. et al. IgM nephropathy in India: a single centre experience. Indian J Pediatr. 2012;79(8):1025–7. doi: 10.1007/s12098-012-0693-0. [DOI] [PubMed] [Google Scholar]
- 22.Mubarak M, Kazi JI, Shakeel S, Lanewala A, Hashmi S, Akhtar F. Clinicopathologic characterstics and steroid response of IgM nephropathy in children presenting with idiopathic nephrotic syndrome. APMIS. 2011;119(3):180–6. doi: 10.1111/j.1600-0463.2010.02708.x. [DOI] [PubMed] [Google Scholar]
- 23.Mubarak M, Naqvi R, Kazi JI, Shakeel S. IgM nephropathy in adults: A clinicopathological study. IJKD. 2013;7(3):214–9. [PubMed] [Google Scholar]
- 24.Nasri H. IgM nephropathy: not uncommon but still a controversial entity. IJKD. 2013;7(3):174–6. [PubMed] [Google Scholar]
- 25.Mubarak M, Kazi JI. IgM nephropathy revisited. Nephro-Urol Mon. 2012;4(4):603–8. doi: 10.5812/numonthly.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mokhtar GA. IgM nephropathy: clinical features and pathological findings in 36 patients. Saudi J Kidney Dis Transplant. 2011;22(5):969–75. [PubMed] [Google Scholar]
- 27.Bhowmik D, Chitale A, Bulchand S. IgM nephropathy in adults: incidence and correlation with electron microscopic features. Indian J Pathol Microbiol. 2007;50(3):511–4. [PubMed] [Google Scholar]
- 28.Mubarak M. Immunoglobulin M nephropathy in adults and adolescents in India: a single center study of natural history. Indian J Pathol Microbiol. 2012;55(1):126–7. doi: 10.4103/0377-4929.94889. [DOI] [PubMed] [Google Scholar]
- 29.Mubarak M. Oxford classification of IgA nephropathy: broadening the scope of the classification. J Nephropathol. 2012;1(1):13–6. doi: 10.5812/jnp.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Salmon AH, Kamel D, Mathieson PW. Recurrence of IgM nephropathy in a renal allograft. Nephrol Dial Transplant. 2004;19(10):2650–2. doi: 10.1093/ndt/gfh434. [DOI] [PubMed] [Google Scholar]
- 31.Westphal S, Hansson S, Mjörnstedt L, Mölne J, Swerkersson S, Friman S. Early recurrence of nephrotic syndrome (immunoglobulin m nephropathy) after renal transplantation successfully treated with combinations of plasma exchanges, immunoglobulin, and rituximab. Transplant Proc. 2006;38(8):2659–60. doi: 10.1016/j.transproceed.2006.07.034. [DOI] [PubMed] [Google Scholar]
- 32.Betjes MG, Roodnat JI. Resolution of IgM nephropathy after rituximab treatment. Am J Kidney Dis. 2009;53(6):1059–62. doi: 10.1053/j.ajkd.2008.10.038. [DOI] [PubMed] [Google Scholar]


