Abstract
Background/Aims
With the increasing incidence of cardiovascular disease, angiocardiography using contrast-enhancing media has become an essential diagnostic and therapeutic tool, despite the risk of contrast-medium-induced acute kidney injury (CIAKI). CIAKI may be exacerbated by renin-angiotensin-system (RAS) blockers, which are also used in a variety of cardiovascular disorders. This study evaluated the effects of RAS blockade on CIAKI after coronary angiography.
Methods
Patients who underwent coronary angiography in our hospital between May 2009 and July 2011 were reviewed. Serum creatinine levels before and after coronary angiography were recorded. CIAKI was diagnosed according to an increase in serum creatinine > 0.5 mg/dL or 25% above baseline.
Results
A total of 1,472 subjects were included in this study. Patients taking RAS blockers were older, had a higher baseline creatinine level, lower estimated glomerular filtration rate (eGFR), and had received a greater volume of contrast medium. After propensity score matching, no difference was observed between the RAS (+) and RAS (.) groups. Multiple logistic regression identified RAS blockade, age, severe heart failure, contrast volume used, hemoglobin level, and eGFR as predictors of CIAKI. Multiple logistic regression after propensity matching showed that RAS blockade was associated with CIAKI (odds ratio, 1.552; p = 0.026).
Conclusions
This study showed that the incidence of CIAKI was increased in patients treated with RAS blockers.
Keywords: Renin angiotensin system, Coronary angiography, Acute kidney injury
INTRODUCTION
Recent advancements in angiocardiography have contributed to the rapid diagnosis and treatment of ischemic heart disease. The use of contrast-enhancing media, in particular, has become essential in this and other imaging modalities, resulting in a rapid increase in their use [1]. However, the use of contrast media has been linked to a nonoliguric form of acute kidney injury, known as contrast-medium-induced acute kidney injury (CIAKI), that is characterized by an increase in serum creatinine levels within 48 to 72 hours of exposure to contrast medium [1-6]. CIAKI is the third most common cause of acute renal failure among in-patients [2,7,8]. Elevated serum creatinine levels typically normalize within 7 to 10 days, although in some cases the condition may progress to chronic renal disease [1,5].
The pathophysiological mechanism of CIAKI has not been elucidated. One of the most important risk factors for CIAKI is existing chronic renal disease [2,9,10]; however, age, the volume of contrast medium used, concurrent diabetes mellitus (DM), congestive heart failure, and anemia have also been implicated. CIAKI is primarily classified as an acute ischemic kidney injury caused by vasoconstriction due to contrast agents, but other potentially contributing mechanisms include direct tubular toxicity as well as impaired vasodilation of renal vessels due to increased endothelin and reduced nitric oxide levels [11].
In addition to contrast media, the use of renin-angiotensin-system (RAS) blockers is increasing in a variety of cardiovascular disorders. RAS blockers, such as angiotensin converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs), are used to control hypertension and subsequent complications in at-risk patients. However, conflicting results regarding the impacts of RAS blockade on CIAKI have been reported. Some studies have shown that long-term use of RAS blockade is a risk factor for CIAKI and should be halted before performing contrast studies [2,12], whereas others have reported that RAS blockade protects against CIAKI [13]. To gain insight into these conflicting views, we retrospectively reviewed the medical records of patients who underwent contrast coronary angiography with or without RAS blockade, and we evaluated the impacts of ACEI and ARB use on the incidence of CIAKI.
METHODS
Study design and objectives
The impacts of RAS blockade on CIAKI were evaluated by conducting a retrospective observational study with patients who successfully underwent coronary angiography in our hospital between May 2009 and July 2011. Indications for angiocardiography included suspected or known cardiovascular disease, congestive heart failure, and cardiac valve diseases. Only patients with creatinine levels < 2.0 mg/L were included in this study to minimize the confounding effect of chronic kidney disease on CIAKI incidence. Patients were excluded if they showed creatinine levels > 2.0 mg/L, if they required dialysis, if they did not require contrast medium, if pretreatment or posttreatment creatinine data were lacking, or if they required further contrast studies.
CIAKI was diagnosed if serum creatinine levels increased > 0.5 mg/dL or > 25% of baseline within 48 to 72 hours after angiocardiography. Baseline creatinine levels were determined before angiocardiography or any other contrast study. The same contrast medium was used for all subjects. The Cockcroft-Gault equation was used to calculate the estimated glomerular filtration rate (eGFR), as follows:
| eGFR (mL/min) = [(140 - age) × mass × 0.85 if female] ÷ (72 × serum creatinine) |
Severe congestive heart failure (HF) was defined as having an ejection fraction (EF) ≤ 35%. Subjects were also analyzed with respect to smoking status.
Statistical analyses
Data were analyzed using t tests, chi-square tests, and multiple logistic regression using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). Covariates used in the multiple logistic regression analysis were age, contrast medium volume, eGFR, hemoglobin level, presence of DM, gender, smoking, and severe congestive HF.
To account for covariates that may have influenced whether or not a patient received a given treatment, propensity score matching was performed using the SAS version 9.1 (SAS Institute Inc., Cary, NC, USA), and patients without a corresponding match were excluded. Propensity scores were calculated by modeling the probability of receiving an RAS blockade agent. The probability was predicted by multiple logistic regression, for which the p was 0.087 and C-statistic was 0.646 using the Hosmer-Lemeshow goodness-of-fit test. Regression analysis was then repeated for these matched subjects.
RESULTS
A total of 2,047 patients who underwent coronary angiography were reviewed. Of these, 1,472 patients who met the inclusion criteria were enrolled. The subjects were divided into patients who received RAS blockade (RAS blockade [+]) and patients who did not (RAS blockade [-]) (Table 1). The percentage of patients receiving RAS blockade was 28% in our study group. The mean age (± standard deviation) was 61.39 ± 11.40 years in the RAAS blockade (-) group and 64.56 ± 10.14 years in the RAAS blockade (+) group (p < 0.001). Contrast dye volume was significantly higher in RAAS blockade (+) group than RAAS blockade (-) group (209.54 ± 106.39 mL vs. 184.17 ± 104.79 mL). No significant difference was observed in number of patients with severe heart failure (EF ≤ 35%) between groups. Compared to the RAAS blockade (-) group, the RAAS blockade (+) group had a significantly lower mean hemoglobin level, mean eGFR, the percentage of male, the percentage of current smoker and the percentage of DM (Table 1). In unmatched subjects, RAS blockade was not a significant risk factor for CIAKI in the univariate regression, but became significant in the adjusted multiple regression analysis (adjusted odds ratio [OR], 1.372; p = 0.048) (Table 2). Other significant predictors for CIAKI were age (adjusted OR, 1.027; p = 0.007), severe HF (adjusted OR, 12.454; p < 0.001), contrast or dye volume used (adjusted OR, 0.997; p = 0.001), hemoglobin level (adjusted OR, 0.899; p = 0.031), and eGFR (adjusted OR, 1.016; p = 0.001) in unmatched subjects.
Table 1.
Patients' characteristics according to renin-angiotensin-system blocker use in unmatched subjects
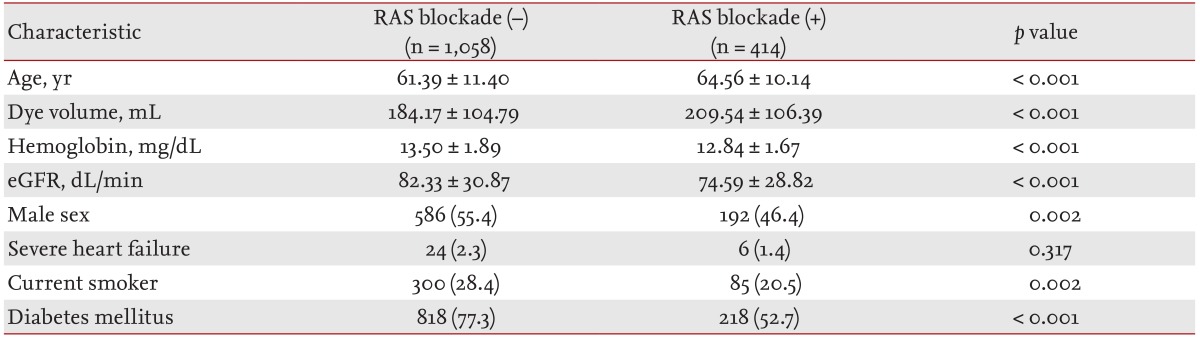
Values are presented as mean ± SD or number (%).
RAS, renin-angiotensin-system; eGFR, effective glomerular filtration rate.
Table 2.
Risk factors for contrast-medium-induced acute kidney injury identified through multiple logistic regression analysis in unmatched subjects
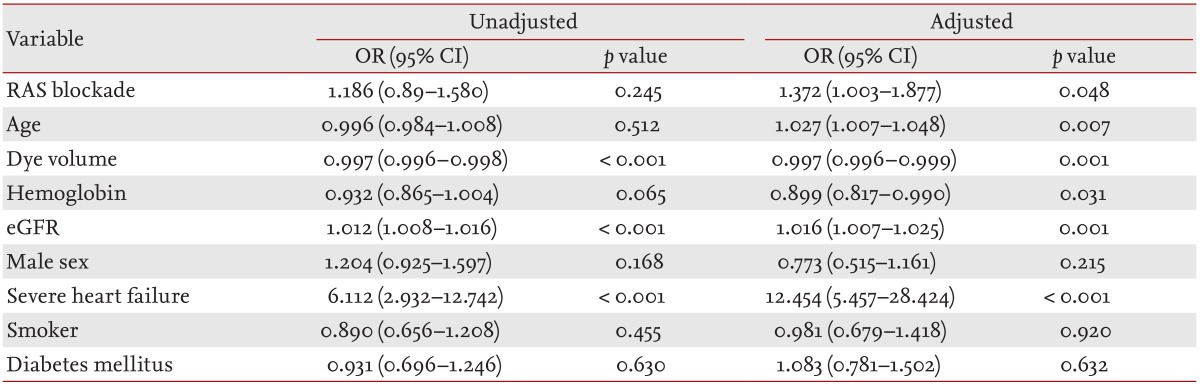
OR, odds ratio; CI, confidence interval; RAS, renin-angiotensin-system; eGFR, effective glomerular filtration rate.
Next, propensity matching was used to identify the effects of RAS blockade excluding other influential factors. The results showed that no significant difference existed between the groups with respect to eGFR, hemoglobin level, or severe HF (Table 3). A further multiple regression analysis after propensity matching showed that the adjusted OR for CIAKI increased significantly to 1.552 among those receiving RAS blockers (Table 4). Age, dye volume used, eGFR, and HF were also significant predictors of CIAKI in matched subjects.
Table 3.
Patients' characteristics according to renin-angiotensin-system blocker use after propensity matching
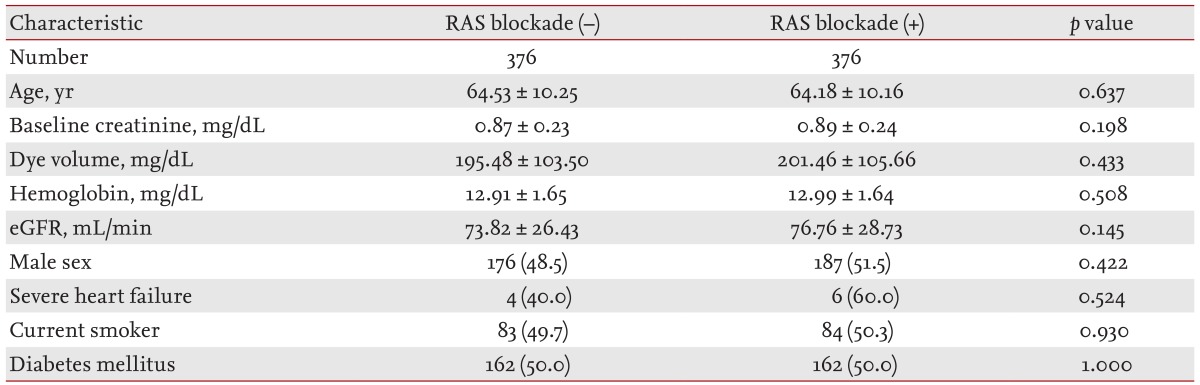
Values are presented as mean ± SD or number (%).
RAS, renin-angiotensin-system; eGFR, effective glomerular filtration rate.
Table 4.
Effects of renin-angiotensin-system blockade on contrast-medium-induced acute kidney injury in matched subjects
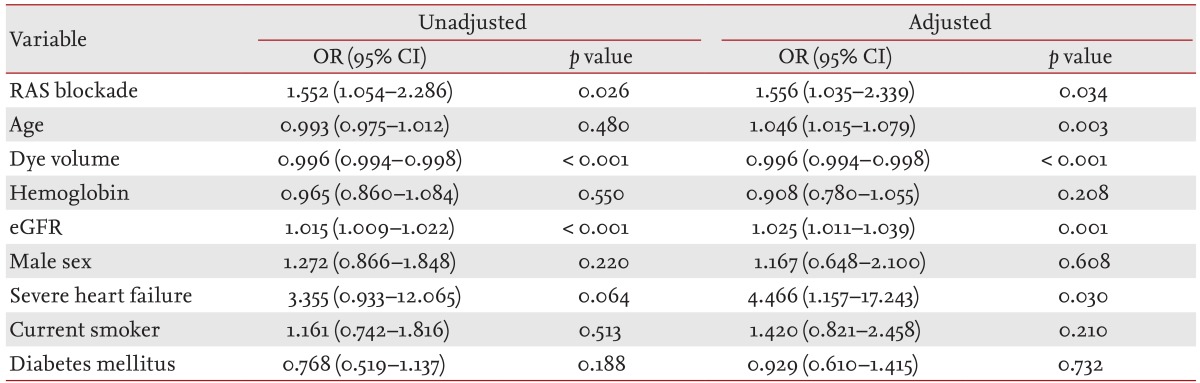
OR, odds ratio; CI, confidence interval; RAS, renin-angiotensin-system; eGFR, effective glomerular filtration rate.
DISCUSSION
Conflicting views exist regarding the effects of RAS blockers, such as ACEIs and ARBs, on CIAKI. In this study, we used propensity matching and multiple regression analysis to show that previous use of a RAS blocker significantly increased the risk of CIAKI.
Large-scale studies have shown that RAS blockade has beneficial effects on left ventricular systolic dysfunction, congestive HF, and prevention of the progression of diabetic nephropathy [14-18]. However, an acute rise in serum creatinine levels after the use of RAS blockers is frequently observed in clinical practice. Several factors have been suggested to explain this phenomenon. ACEIs reduce the pressure head from the afferent arterioles and lead to a reduction in intraglomerular pressure. Thus, the compensatory elevation of single-nephron GFR observed in renal insufficiency and diabetes is reduced during concurrent hypoperfusion and ACE inhibition [19]. Another explanation is related to renal autoregulation of pressure through the nephrons [19-21]. Bilateral renal artery stenosis may also cause elevated serum creatinine levels following initiation of ACEI therapy.
The effect of RAS blockade on CIAKI incidence remains unclear. ACE-inhibitor therapy decreased the incidence of CIAKI in 71 diabetic patients after cardiac catheterization and in more than 7,000 patients with chronic kidney disease undergoing percutaneous coronary intervention [22,23]. Kiski et al. [2] examined the effects of ACEIs and ARBs on contrast-induced nephropathy (CIN); the study included 412 patients, among whom 269 patients were receiving RAS blockers. Although the study revealed no significant difference in age, serum creatinine, or left ventricular function between groups, the incidence of CIN was significantly higher in the RAS blockade group (11.9%) than in the untreated group (4.2%; p = 0.001). Toprak et al. [15] also showed that the ACEI captopril was a risk factor for developing CIAKI, whereas Gupta et al. [23] stated that captopril offered protection against CIN. However, both of these studies had limited statistical power due to small sample sizes, and did not account for confounding effects due to inclusion of diabetic patients [15,23]. Other studies into the effects of RAS blockade have included patients with chronic kidney disease [23] or failed to account for other important risk factors for CIAKI, such as baseline kidney function, contrast agent volume, and congestive HF. These limitations and differences in study design may explain conflicting reports as to the effect of RAS blockade on CIAKI.
To overcome these issues, we examined a broader range of potential confounders and used propensity score matching to correct for biases due to treatment recruitment. We observed significant differences in terms of age, dye volume, hemoglobin level, eGFR, gender, smoking status, and the incidence of diabetes between subjects receiving RAS blockade and those without. In order to clarify the effect of RAS blockade on CIAKI, we matched other risk factors using the propensity score method and found that RAS blockade increased the incidence of CIAKI in our multiple logistic regression analysis, with an adjusted OR of 1.556 (p = 0.034) (Table 4). A similar trend was observed among unmatched subjects (adjusted OR, 1.372; p = 0.048) (Table 2), and these results are consistent with those of a recent study [24].
Several theories regarding the pathophysiology of CIAKI have been suggested. One theory states that contrast medium increases vasoconstriction at the corticomedullary junction in the kidney and reduces vasodilation due to a reduction in nitric oxide production, resulting in hypoxia and acute tubular necrosis [25]. Therefore, CIAKI can be principally classified as an ischemic acute kidney injury caused by the vasoconstrictive properties of contrast media. In addition, contrast media not only have a direct toxic effect on endothelial cells and renal tubules but also potentiate toxicity by reducing erythrocyte flexibility and activating leukocyte adhesion molecule, which facilitates the binding of leukocytes to endothelial cells. Contrast media also stimulate adenosine receptor A1 and induce vasoconstriction of the afferent arterioles, resulting in renal ischemia [25].
Several risk factors can be inferred from these theories of CIAKI pathogenesis. One of the most significant risk factors for CIAKI is existing chronic renal disease. We found that elevated eGFR increased CIAKI risk with a relatively small but statistically significant OR (adjusted OR, 1.025) (Table 4), which is in contrast to previous reports of no effect [24,26]. However, it is possible that we detected a significant effect because we were better able to limit the confounding effect of chronic kidney disease by excluding patients with serum creatinine levels > 2.0 mg/dL. We furthermore used a continuous variable (eGFR) to account for kidney function, rather than a categorical variable like presence/absence of chronic kidney disease, which may have increased sensitivity. The volume of contrast medium used is also an important risk factor for CIAKI because the dye itself may cause vasoconstriction of renal tubular arterioles and direct tubular toxicity [27]. In our results, the use of less contrast medium in coronary angiography tended to increase CIAKI risk, but its OR was close to 1 (Table 4). In the baseline characteristics, contrast medium volume was lower in the CIAKI (+) group than in the CIAKI (-) group (data not shown). In clinical practice, cardiologists regulate the amount of contrast medium used during coronary angiography based on several factors. If patients show multiple risk factors for CIAKI, the cardiologist may reduce contrast dye volume to prevent CIAKI. Thus, clinical judgments can also be a confounding factor in retrospective studies examining the effect of contrast medium volume on CIAKI. In addition, age, anemia, and congestive HF were significant risk factors for CIAKI in both matched and unmatched subjects (Tables 2 and 4), which is consistent with other studies [24,26,28].
Our study had several limitations. First, this study was conducted at a single center, although it involved a large population of more 1,400 patients. Second, this was an observational, rather than a randomized controlled, study. RAS blockade was not randomized and other risk factors differed between the RAS (-) versus RAS (+) groups. Because smoking is an important risk factor for coronary atherosclerosis, it would have been useful to analyze smoking status in more detail, although such information was not attainable given the retrospective nature of this study. To overcome these limitations, we used the propensity-score-matching method.
This study identified RAS blocking agents as a possible risk factor for CIAKI in angiocardiography patients. Although this study does not present sufficient evidence to justify halting the use of RAS blockers before coronary angiography, as has taken place in several institutes, our results demonstrate that clinicians should be aware of the risks of RAS blockade for CIAKI and exercise caution when necessary.
KEY MESSAGE
1. Angiocardiography have been increased to diagnosis and treat an ischemic heart disease and the use of contrast media has been linked to an acute kidney injury.
2. Renin-angiotensin-system (RAS) blockers are used to control hypertension and subsequent complications in at-risk patients.
3. The impacts RAS blockade on contrast-medium-induced acute kidney injury (CIAKI) have been controversial. In this study, the incidence of CIAKI was increased in patients treated with RAS blockers.
4. Clinicians should be aware of the risks of RAS blockade for CIAKI.
Acknowledgments
The authors owe thanks to Prof. Won-Kee Lee, Health Promotion Research Center, Kyungpook National University School of Medicine for providing helpful comments on the statistical approach of this study.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Laville M, Juillard L. Contrast-induced acute kidney injury: how should at-risk patients be identified and managed? J Nephrol. 2010;23:387–398. [PubMed] [Google Scholar]
- 2.Kiski D, Stepper W, Brand E, Breithardt G, Reinecke H. Impact of renin-angiotensin-aldosterone blockade by angiotensin-converting enzyme inhibitors or AT-1 blockers on frequency of contrast medium-induced nephropathy: a post-hoc analysis from the Dialysis-versus-Diuresis (DVD) trial. Nephrol Dial Transplant. 2010;25:759–764. doi: 10.1093/ndt/gfp582. [DOI] [PubMed] [Google Scholar]
- 3.Morcos SK, Thomsen HS European Society of Urogenital Radiology. European Society of Urogenital Radiology guidelines on administering contrast media. Abdom Imaging. 2003;28:187–190. doi: 10.1007/s00261-001-0186-5. [DOI] [PubMed] [Google Scholar]
- 4.Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31. doi: 10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nikolsky E, Aymong ED, Dangas G, Mehran R. Radiocontrast nephropathy: identifying the high-risk patient and the implications of exacerbating renal function. Rev Cardiovasc Med. 2003;4(Suppl 1):S7–S14. [PubMed] [Google Scholar]
- 6.Thomsen HS. European Society of Urogenital Radiology Guidelines on Contrast Media, Ver. 7.0. Heidelberg: European Society of Urogenital Radiology; 2008. [DOI] [PubMed] [Google Scholar]
- 7.Nyman U, Almen T, Aspelin P, Hellstrom M, Kristiansson M, Sterner G. Contrast-medium-Induced nephropathy correlated to the ratio between dose in gram iodine and estimated GFR in ml/min. Acta Radiol. 2005;46:830–842. doi: 10.1080/02841850500335051. [DOI] [PubMed] [Google Scholar]
- 8.Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis. 2002;39:930–936. doi: 10.1053/ajkd.2002.32766. [DOI] [PubMed] [Google Scholar]
- 9.Bartholomew BA, Harjai KJ, Dukkipati S, et al. Impact of nephropathy after percutaneous coronary intervention and a method for risk stratification. Am J Cardiol. 2004;93:1515–1519. doi: 10.1016/j.amjcard.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 10.Mehran R, Aymong ED, Nikolsky E, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;44:1393–1399. doi: 10.1016/j.jacc.2004.06.068. [DOI] [PubMed] [Google Scholar]
- 11.Persson PB, Tepel M. Contrast medium-induced nephropathy: the pathophysiology. Kidney Int Suppl. 2006;(100):S8–S10. doi: 10.1038/sj.ki.5000367. [DOI] [PubMed] [Google Scholar]
- 12.Louis BM, Hoch BS, Hernandez C, et al. Protection from the nephrotoxicity of contrast dye. Ren Fail. 1996;18:639–646. doi: 10.3109/08860229609047689. [DOI] [PubMed] [Google Scholar]
- 13.Reinecke H, Fobker M, Wellmann J, et al. A randomized controlled trial comparing hydration therapy to additional hemodialysis or N-acetylcysteine for the prevention of contrast medium-induced nephropathy: the Dialysis-versus-Diuresis (DVD) Trial. Clin Res Cardiol. 2007;96:130–139. doi: 10.1007/s00392-007-0473-4. [DOI] [PubMed] [Google Scholar]
- 14.Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy: the Collaborative Study Group. N Engl J Med. 1993;329:1456–1462. doi: 10.1056/NEJM199311113292004. [DOI] [PubMed] [Google Scholar]
- 15.Toprak O, Cirit M, Bayata S, Yesil M, Aslan SL. The effect of pre-procedural captopril on contrast-induced nephropathy in patients who underwent coronary angiography. Anadolu Kardiyol Derg. 2003;3:98–103. [PubMed] [Google Scholar]
- 16.Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345:851–860. doi: 10.1056/NEJMoa011303. [DOI] [PubMed] [Google Scholar]
- 17.Swedberg K, Kjekshus J. Effects of enalapril on mortality in severe congestive heart failure: results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS) Am J Cardiol. 1988;62:60A–66A. doi: 10.1016/s0002-9149(88)80087-0. [DOI] [PubMed] [Google Scholar]
- 18.Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. The SOLVD Investigators. N Engl J Med. 1991;325:293–302. doi: 10.1056/NEJM199108013250501. [DOI] [PubMed] [Google Scholar]
- 19.Toto RD. Renal insufficiency due to angiotensin-converting enzyme inhibitors. Miner Electrolyte Metab. 1994;20:193–200. [PubMed] [Google Scholar]
- 20.Christensen PK, Hansen HP, Parving HH. Impaired autoregulation of GFR in hypertensive non-insulin dependent diabetic patients. Kidney Int. 1997;52:1369–1374. doi: 10.1038/ki.1997.463. [DOI] [PubMed] [Google Scholar]
- 21.Modification of Diet in Renal Disease Study Group. Short-term effects of protein intake, blood pressure, and antihypertensive therapy on glomerular filtration rate in the Modification of Diet in Renal Disease Study. J Am Soc Nephrol. 1996;7:2097–2109. doi: 10.1681/ASN.V7102097. [DOI] [PubMed] [Google Scholar]
- 22.Dangas G, Iakovou I, Nikolsky E, et al. Contrast-induced nephropathy after percutaneous coronary interventions in relation to chronic kidney disease and hemodynamic variables. Am J Cardiol. 2005;95:13–19. doi: 10.1016/j.amjcard.2004.08.056. [DOI] [PubMed] [Google Scholar]
- 23.Gupta RK, Kapoor A, Tewari S, Sinha N, Sharma RK. Captopril for prevention of contrast-induced nephropathy in diabetic patients: a randomised study. Indian Heart J. 1999;51:521–526. [PubMed] [Google Scholar]
- 24.Rim MY, Ro H, Kang WC, et al. The effect of renin-angiotensin-aldosterone system blockade on contrast-induced acute kidney injury: a propensity-matched study. Am J Kidney Dis. 2012;60:576–582. doi: 10.1053/j.ajkd.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 25.Tumlin J, Stacul F, Adam A, et al. Pathophysiology of contrast-induced nephropathy. Am J Cardiol. 2006;98(6A):14K–20K. doi: 10.1016/j.amjcard.2006.01.020. [DOI] [PubMed] [Google Scholar]
- 26.Gopalan PD. Contrast-induced acute kidney injury. South Afr J Anaesth Analg. 2011;17:193–195. [Google Scholar]
- 27.Perazella MA. Renal vulnerability to drug toxicity. Clin J Am Soc Nephrol. 2009;4:1275–1283. doi: 10.2215/CJN.02050309. [DOI] [PubMed] [Google Scholar]
- 28.Weisbord SD, Palevsky PM. Strategies for the prevention of contrast-induced acute kidney injury. Curr Opin Nephrol Hypertens. 2010;19:539–549. doi: 10.1097/MNH.0b013e32833d42e3. [DOI] [PubMed] [Google Scholar]


