Abstract
Background/Aims
The aim of this study is to measure the difference of ionized calcium between heparinized whole blood and serum.
Methods
We recruited 107 maintenance hemodialysis (HD) patients from our hospital HD unit. The clinical and laboratory data included ionized calcium in serum and in whole blood (reference, 4.07 to 5.17 mg/dL).
Results
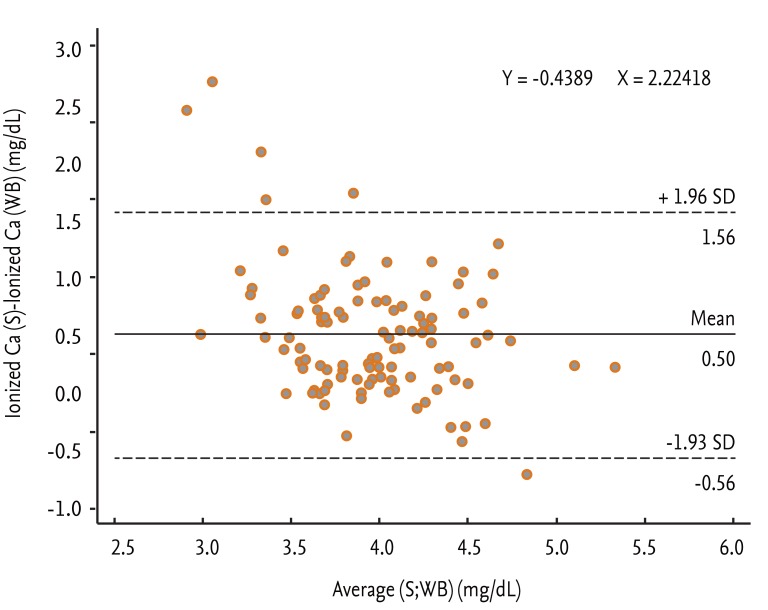
The level of ionized calcium in serum was higher than that in whole blood (p < 0.001). Bland-Altman analysis showed that difference for ionized calcium was 0.5027. For the difference, the nonstandardized β was -0.4389 (p < 0.001) and the intercept was 2.2418 (p < 0.001). There was a significant difference in the distribution of categories of ionized calcium level between two methods (κ, 0.279; p < 0.001).
Conclusions
This study demonstrates that whole blood ionized calcium is underestimated compared with serum ionized calcium. Positive difference increases as whole blood ionized calcium decreases. Therefore, significant hypocalcemia in whole blood ionized calcium should be verified by serum ionized calcium.
Keywords: Renal dialysis, Heparin, Hypocalcemia
INTRODUCTION
Chronic kidney disease-mineral bone disease is a well-known complication in dialysis patients [1-3]. Proper calcium and phosphorus levels are associated with declines in vascular calcification, morbidity, and mortality in dialysis patients [1-4]. Total calcium is divided into ionized calcium (free calcium) and bound calcium (complex-bound calcium). The National Kidney Foundation Kidney Disease Outcomes Quality Initiative clinical practice guidelines recommend that serum total calcium corrected for albumin is within the normal range for the laboratory (reference in our center, 8.6 to 10.6 mg/dL) [1]. However, there is a lack of a standardized formula for corrected calcium. Although according to Kidney Disease: Improving Global Outcomes guidelines ionized calcium is not cost effective, specificity for ionized calcium is higher than that for total calcium or corrected total calcium [5,6]. Ionized calcium is actually measured in many centers to identify calcium abnormalities. Ionized calcium can be measured using whole blood or serum. It can be influenced by pH, phosphate, lactate, and anticoagulants. The anticoagulant heparin is associated particularly with lower ionized calcium levels in whole blood than in serum [7,8]. The aim of this study was to evaluate the difference in ionized calcium level between heparinized whole blood and serum and to determine whether heparinized whole blood calcium is useful for diagnosis of calcium abnormalities.
METHODS
We included 107 patients under maintenance hemodialysis (HD) in our hospital HD unit. This study was conducted in full compliance with the amended Declaration of Helsinki following approval from the Institutional Review Board of Yeungnam University Hospital (YUH-12-0401-O52). All of the 107 subjects enrolled in this study gave written informed consent for this study.
The patients were all dialyzed two or three times per week (3.5 to 4.5 hours per session) using hollow-fiber dialyzers. The standard blood flow was 250 to 300 mL/min and the dialysate flow was 500 mL/min. Clinical and laboratory data collected at the time of sampling included age, gender, disease underlying end-stage renal disease, HD duration, total calcium (reference range, 8.6 to 10.6 mg/dL), corrected total calcium (mg/dL), phosphorus (mg/dL), calcium-containing phosphate binder use, high-sensitivity C-reactive protein (hs-CRP; mg/dL), serum albumin (g/dL), lactate (mmol/L), pH, bicarbonate (mmol/L), and ionized calcium in serum and in whole blood (reference range, 4.07 to 5.17 mg/dL). These laboratory parameters were measured in the same blood draw.
Blood samples were obtained from nonfasting patients before the first HD session of the week. Non-heparinized, dry Vacutainer tubes were used to determine serum ionized calcium levels. Whole blood ionized calcium levels were determined using sodium heparin-coated 3-mL syringes. Ionized calcium was detected by two methods using an ABL800 analyzer (Radiometer, Copenhagen, Denmark). Samples for serum were stored at 4℃ immediately after sampling and separated from cells within 1 hour. Ionized calcium in whole blood was measured within 15 minutes after sampling. Serum albumin and CRP levels were measured using an Olympus AU4500 (Olympus, Tokyo, Japan) automatic chemical analyzer (bromocresol green for albumin). Corrected serum calcium level was calculated using Payne formula: corrected calcium (mg/dL) = total calcium (mg/dL) + 0.8 × [4 - albumin (g/dL)] [1].
The data are expressed as numbers (%) for categorical variables and medians and interquartile range (25% percentile; 75% percentile) for continuous variables. Differences in total calcium and corrected total calcium were compared using Wilcoxon signed-rank test. Pearson correlation analysis was used to assess the strength of the relation between pairs of variables. Categorical variables were compared using Pearson chi-square test or Fisher exact test with κ tests. These analyses were performed using SPSS version 19 (IBM Co., Armonk, NY, USA). Bland-Altman plots were used to visually assess differences between the two methods [9,10]. Differences are plotted against the averages of the two methods. Horizontal lines indicate the mean difference and ± 1.96 × the standard deviation. This is useful to identify the size or trend of the differences. Differences were calculated as follows: ionized calcium in serum-ionized calcium in whole blood. This analysis was performed using MedCalc version 11.6.1.0 (MedCalc Software, Mariakerke, Belgium). The level of statistical significance was set at p < 0.05.
RESULTS
One hundred and seven HD patients participated in this study (Table 1). The median HD duration was 23 months (8; 55). These 54.2% of the study participants were male. The pH was 7.36 (7.33; 7.38), the noncorrected total calcium level was 8.3 mg/dL (8.0; 8.8), and the corrected total calcium level was 8.28 (7.86; 9.02). The ionized calcium level was 3.76 mg/dL (3.41; 4.01) in whole blood and 4.15 mg/dL (3.89; 4.47) in serum. The ionized calcium level was higher in serum than in whole blood (p < 0.001). Serum ionized calcium was correlated with whole blood ionized calcium, total calcium, and corrected total calcium (r = 0.464 for whole blood ionized calcium, r = 0.803 for total calcium, and r = 0.789 for corrected total calcium; p < 0.001 for all three variables) (Table 2). There was no significant correlation with phosphorus, calcium-containing phosphate binder use, hs-CRP, lactate, pH, or bicarbonate (Table 2).
Table 1.
Patients' characteristics (n = 107)
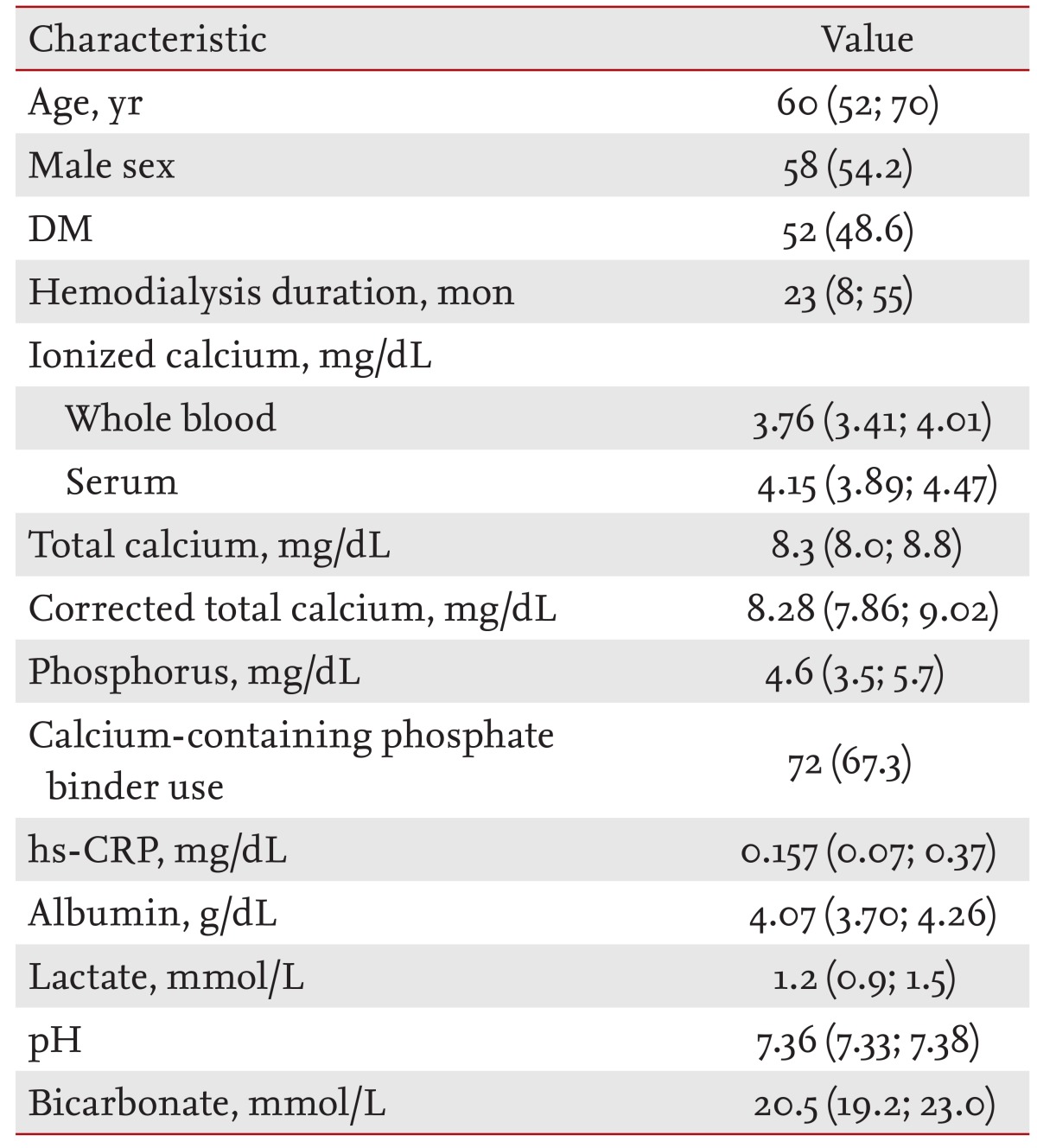
Values are presented as medians and interquartile range (25% percentile; 75% percentile) for continuous variables or number (%) for categorical variables.
DM, diabetes mellitus; hs-CRP, high sensitivity C-reactive protein.
Table 2.
Associations between serum ionized calcium and other variables
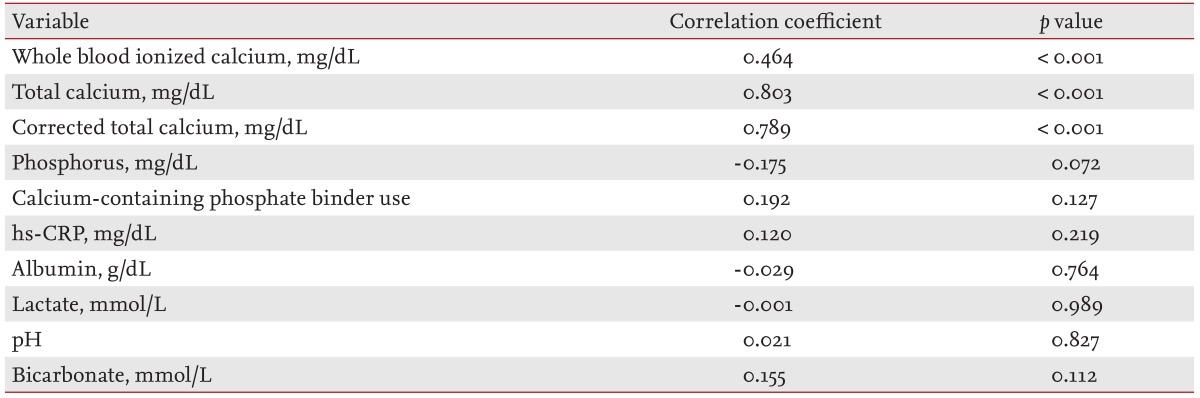
hs-CRP, high sensitivity C-reactive protein.
Bland-Altman analysis showed that the difference for ionized calcium was 0.5027 (95% confidence interval [CI], 0.3990 to 0.6064). In most patients, ionized calcium in serum-ionized calcium in whole blood was within ± 1.96 standard deviation of 0.5027 (Fig. 1). For the difference, the nonstandardized β was -0.4389 (95% CI, -0.6648 to -0.2131; p < 0.001) and the intercept was 2.2418 (95% CI, 1.3417 to 3.1419; p < 0.001). There was a significant difference between the two methods in the distribution of categories according to ionized calcium level (κ = 0.279, p < 0.001) (Table 3). When ionized calcium in whole blood was measured, 43 patients with normocalcemia (67.2%) were miscategorized to hypocalcemia. Two patients with hypercalcemia (66.6%) were miscategorized to normocalcemia or hypocalcemia. In addition, among 64 patients with normocalcemia, patients miscategorized to hypocalcemia had higher ionized calcium levels in whole blood than corrected total calcium levels.
Figure 1.
Bland-Altman plot showing limits of agreement between ionized calcium levels in serum and whole blood. Difference 0.5027 (95% confidence interval, 0.3990 to 0.6064). Ca, calcium; S, serum; WB, whole blood; SD, standard deviation.
Table 3.
Calcium state according to calcium method
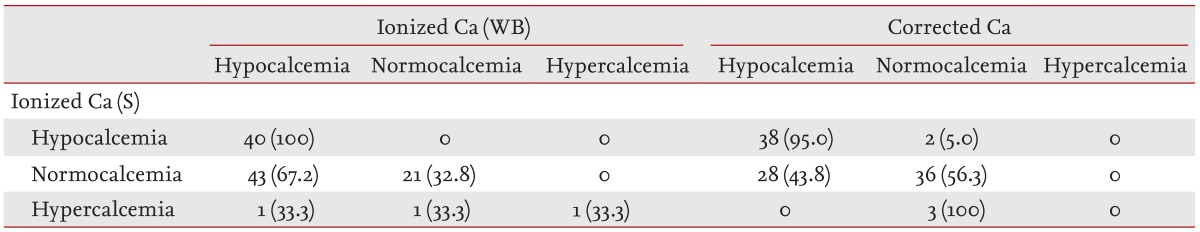
Values are presented as number (%).
Ca, calcium; WB, whole blood; S, serum.
DISCUSSION
The results of the present study show that the whole blood ionized calcium level, determined using heparin-coated syringes, shows a 0.5-mg/dL difference compared to ionized calcium in serum. The difference increased as the whole blood ionized calcium level decreased.
Ionized calcium can be measured in whole blood or serum. The Clinical Laboratory Standards Institute (CLSI) suggests that both methods are acceptable [7]. Measurement of serum ionized calcium has disadvantages of delayed analysis and cellular metabolism during centrifugation. Measurement of ionized calcium using whole blood has the advantages of rapid results, minimization of cellular metabolism, and simultaneous measurement of potassium. And while it requires heparinization of whole blood, it does not require centrifugation of blood to isolate serum. Heparin binds significant amounts of ionized calcium and reduces the ionized calcium level [8]. The CLSI recommends that the sodium heparin concentration should be below 10 IU/mL and that the calcium-titrated heparin concentration should not exceed 70 IU/mL [7].
Bland-Altman analysis showed that mean value of serum ionized calcium-whole blood ionized calcium was 0.5 mg/dL, and that the regression equation for the difference between the two methods was as follows: difference = 2.2418 - 0.4389 × [average of serum and whole blood ionized calcium (mg/dL)]. This equation shows that the difference between the two methods increases as the ionized calcium level decreases. The proportion of ionized calcium bound to heparin increases as the ionized calcium level decreases. If the average of the whole blood and serum ionized calcium levels is 5.108 mg/dL, the difference will be approximately 0. Therefore, if hypercalcemia is defined as > 5.17 mg/dL, most whole blood ionized calcium levels in patients without hypercalcemia will underestimate the serum ionized calcium level.
When serum ionized calcium was defined as a reference, there was no significant difference in distribution of patients with hypocalcemia. More than half of all patients with normocalcemia (67.2%) were miscategorized to hypocalcemia based on whole blood ionized calcium. For categorization according to ionized calcium level, agreement between the two measurements was only 27.9%. This result suggests that ionized calcium should be measured using serum in patients who are suspected to have hypocalcemia. In addition, diagnosis of hypocalcemia based on whole blood ionized calcium should be verified by simultaneous measurement of serum ionized calcium.
Three patients had hypercalcemia. Many patients are needed to evaluate the differences in ionized calcium levels between whole blood and serum in patients with hypercalcemia. However, because the differences decrease with increasing whole blood ionized calcium level, the number of cases of hypercalcemia determined by whole blood measurement may not be changed. Among patients with normocalcemia, the rate of miscategorization to hypocalcemia was 43.8% for corrected calcium. Corrected calcium may not substitute for serum ionized calcium.
The pH is associated with ionized calcium level [7,11-13]. Changes in pH in whole blood and serum are related to loss of CO2 and lactic acid formation, respectively [7,8,11-13]. To minimize the effect of loss of CO2, whole blood ionized calcium was measured within 15 minutes after sampling. To minimize contact with erythrocytes, serum ionized calcium samples should be centrifuged within 1 hour after sampling and should be stored at 4℃. In the present study, the pH values were all within 0.15 units (7.36 ± 0.04), and change in pH was not correlated with ionized calcium. The narrow pH interval in our cohort may explain the apparent lack of an association between ionized calcium and pH.
In conclusion, this study demonstrates that the whole blood ionized calcium level is underestimated compared to the serum ionized calcium level. The difference between measurements increases with decreasing whole blood ionized calcium level. Therefore, ionized calcium should be measured in serum. Significant hypocalcemia in whole blood should be verified by measuring serum ionized calcium.
KEY MESSAGE
1. Significant hypocalcemia in whole blood should be verified by measuring serum ionized calcium.
Footnotes
This research was supported by a grant from Daewoong Pharm. Co., Ltd., Republic of Korea.
References
- 1.National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003;42(4 Suppl 3):S1–S201. [PubMed] [Google Scholar]
- 2.Block GA, Klassen PS, Lazarus JM, Ofsthun N, Lowrie EG, Chertow GM. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol. 2004;15:2208–2218. doi: 10.1097/01.ASN.0000133041.27682.A2. [DOI] [PubMed] [Google Scholar]
- 3.Young EW, Albert JM, Satayathum S, et al. Predictors and consequences of altered mineral metabolism: the Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2005;67:1179–1187. doi: 10.1111/j.1523-1755.2005.00185.x. [DOI] [PubMed] [Google Scholar]
- 4.An WS, Kim SE, Kim KH, Bae HR, Rha SH. Associations between oxidized LDL to LDL ratio, HDL and vascular calcification in the feet of hemodialysis patients. J Korean Med Sci. 2009;24(Suppl):S115–S120. doi: 10.3346/jkms.2009.24.S1.S115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) Kidney Int Suppl. 2009;(113):S1–S130. doi: 10.1038/ki.2009.188. [DOI] [PubMed] [Google Scholar]
- 6.Gauci C, Moranne O, Fouqueray B, et al. Pitfalls of measuring total blood calcium in patients with CKD. J Am Soc Nephrol. 2008;19:1592–1598. doi: 10.1681/ASN.2007040449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sachs C, Rabouine P, Chaneac M, Kindermans C, Dechaux M. In vitro evaluation of a heparinized blood sampler for ionized calcium measurement. Ann Clin Biochem. 1991;28(Pt 3):240–244. doi: 10.1177/000456329102800307. [DOI] [PubMed] [Google Scholar]
- 8.D'Orazio P, Toffaletti JG, Wandrup J National Committee for Clinical Laboratory Standards. Ionized Calcium Determinations: Precollection Variables, Specimen Choice, Collection, and Handling: Approved Guideline. 2nd ed. Wayne: National Committee for Clinical Laboratory Standards; 2001. [Google Scholar]
- 9.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 10.Bland JM, Altman DG. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet. 1995;346:1085–1087. doi: 10.1016/s0140-6736(95)91748-9. [DOI] [PubMed] [Google Scholar]
- 11.McLean FC, Hastings BA. The state of calcium in the fluids of the body: I. the conditions affecting the ionization of calcium. J Biol Chem. 1935;108:285–321. [Google Scholar]
- 12.Hinkle JE, Cooperman LH. Serum ionized calcium changes following citrated blood transfusion in anaesthetized man. Br J Anaesth. 1971;43:1108–1112. doi: 10.1093/bja/43.12.1108. [DOI] [PubMed] [Google Scholar]
- 13.Thode J, Fogh-Andersen N, Wimberley PD, Moller Sorensen A, Siggaard-Andersen O. Relation between pH and ionized calcium in vitro and in vivo in man. Scand J Clin Lab Invest Suppl. 1983;165:79–82. [PubMed] [Google Scholar]