Dear Editor,
Phacoemulsification in eyes with scarred corneas is challenging and due to the poor surgical view, carries an increased risk of complications.1 In healthy eyes, the cornea is transparent due to the small diameter, and relatively regular size and spacing of stromal collagen fibrils, in addition to similarity of the refractive indices of collagen fibrils (1.411) and the extrafibrillar matrix (1.365).2,3 Corneal scars have higher refractive index and reduce transparency as they disrupt collagen fibril organization and increase light scattering.
It has long been recognized that tissues can be made transparent by impregnation with high refractive index solutions.4 Previously, Maurice described a series of studies investigating the possible use of high refractive index radiological contrast media as corneal clearing agents.5 The rationale was that since corneal scars are of high refractive index,5 if the cornea is impregnated with a contrast solution that matches the refractive index of the scar, light scattering could be reduced and corneal transparency should be improved. Although improvement in transparency would not be permanent, the cornea may clear enough to improve the view during cataract surgery. In Maurice’s experiments, central scars were created in rabbit corneas of such severity that no details of the retina could be seen with an indirect ophthalmoscope. The cornea was then treated with the contrast media metrizamide or iohexol (GE Healthcare, Bucks, UK). The treatment process involved debridement of the corneal epithelium followed by application of the contrast agent for 20 minutes. Treatment resulted in sufficient corneal clearing to allow full details of the fundus to be observed “as in the normal eye”.5 The cornea remained clear for 10 to 20 minutes before reverting to its previous state.
Despite promising animal studies, contrast media have not been tested as corneal clearing agents in humans. We therefore conducted a pilot study to evaluate the use of the contrast medium iohexol as a corneal clearing agent for the first time in humans. Iohexol (refractive index of 1.46) is a contrast agent licensed for oral, intravenous, intrathecal or body cavity use (GE Healthcare, Omnipaque prescribing information), which has previously been used in ophthalmology for dacryocystography and computer tomography guided localization of anesthetics following retrobulbar injection.6 The study was approved by the UK Medical Healthcare Products Regulatory Agency (MHRA) and local Institutional Review Board (IRB). Informed consent was obtained from all patients and the research adhered to the tenets of the Declaration of Helsinki.
Three eyes of 3 patients with cataracts and central corneal scarring (due to rosacea keratitis, trachoma keratopathy and herpes simplex keratitis) were included (Table 1). The surgical procedure was designed to be similar to the method described by Maurice2 as much as possible. The corneal epithelium overlying the area of corneal scarring was debrided using a hockey spatula (E. Janach, Kestrel Ophthalmics, Dorset, UK), with the limbal epithelium left intact. Iohexhol (350mg iodine/ml) was drawn into a 5ml syringe attached to a 30G Rycroft Cannula (BD, Oxford, UK) then applied as drops to the corneal stroma for 15 minutes, aiming to saturate the stroma. The corneal scar was observed for any improvement in transparency and the procedure was recorded using digital video-capture linked to the operating microscope. The eye was then irrigated with balanced salt solution (Alcon, Hemel Hempstead, UK) to minimize the risk of iohexol inadvertently entering the anterior chamber. Phacoemulsification was completed and postoperative treatment consisted of dexamethasone and chloramphenicol eye drops 4 times per day for 4 weeks and topical diclofenac 4 times per day until the epithelial defect had healed. A detailed ophthalmic examination was carried out 2 days, 2 weeks and 4 weeks following surgery.
Table 1.
Clinical characteristics of the patients, including cause of reduced corneal transparency and best corrected preoperative (preop) and 4-weeks postoperative (postop) visual acuity (VA)
| Patient Number | Age (years) | Sex | Pathology | Description of corneal scar (duration) | Preop VA | Postop VA |
|---|---|---|---|---|---|---|
| 1 | 82 | Female | Herpes simplex keratitis | Diffuse anterior stromal opacity involving the central cornea (>20 years) | 6/12 | 6/6 |
| 2 | 52 | Male | Ocular rosacea | Vascularised, predominantly anterior stromal (6 months) | 6/36 | 6/9 |
| 3 | 81 | Female | Trachoma | Diffuse anterior stromal (>20 years) | 6/18 | 6/12 |
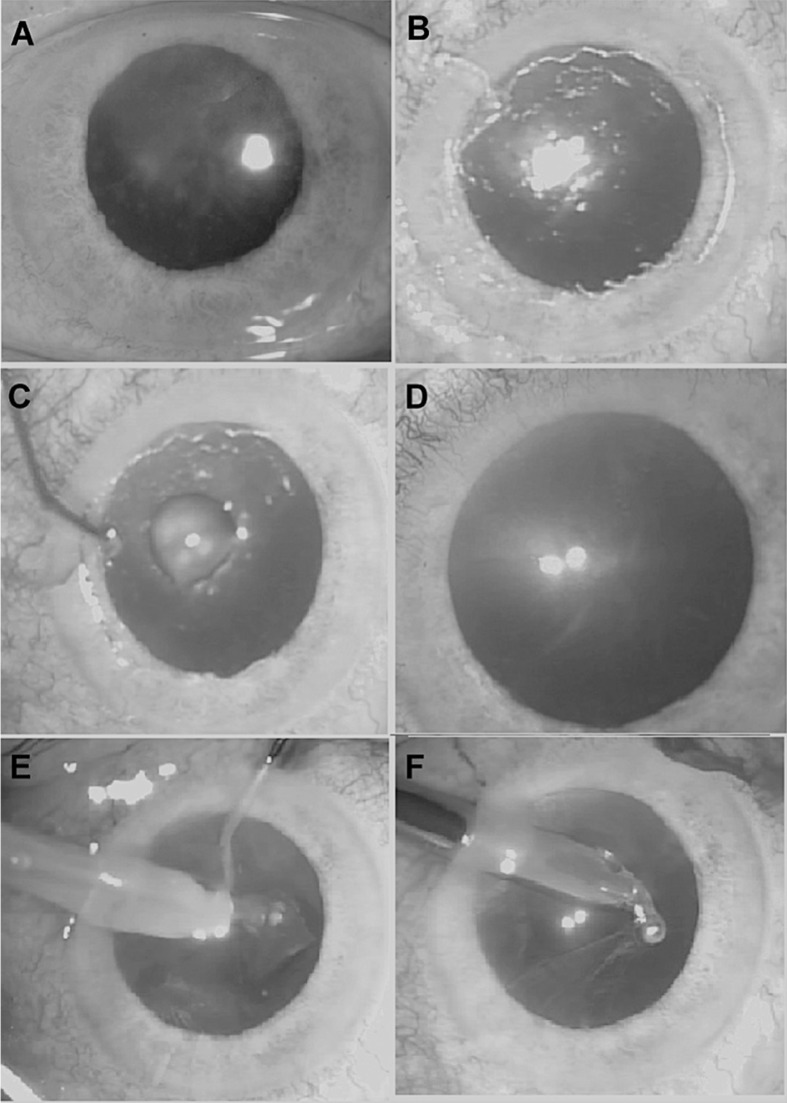
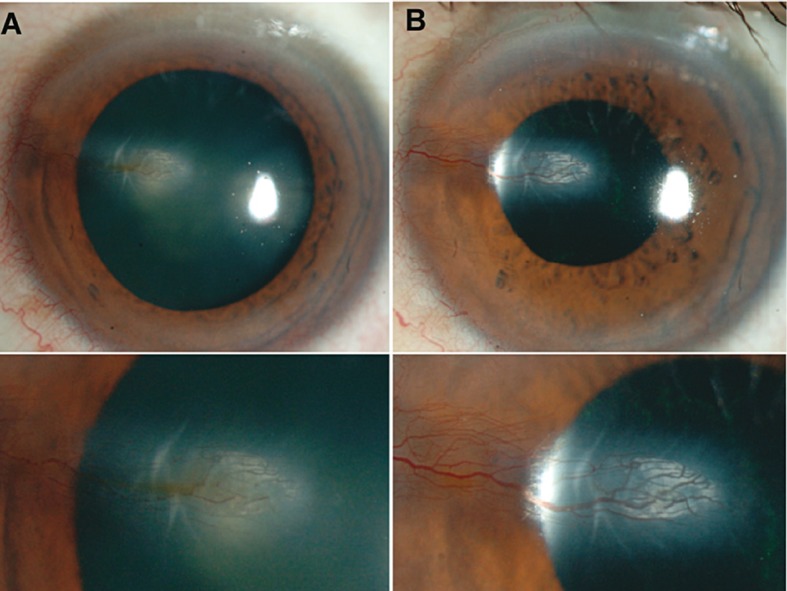
Despite the promising animal studies, iohexol was found to have little effect on corneal transparency. Patients 1 and 3 had no significant change in corneal transparency (Figure 1) and although patient 2 demonstrated a small improvement in transparency, this change did not significantly aid cataract surgery (Figure 2). In all patients, the epithelial defects healed by 2 weeks and there were no adverse effects observed.
Figure 1.
Photographs of patient #1 taken preoperatively (A), following epithelial debridement (before iohexol application) (B), during iohexol application (C), 15 minutes following iohexol but before irrigation of the cornea with balanced salt solution (D), during subsequent cataract extraction (E-F).
Figure 2.
Operative photographs taken of patient #2 preoperatively (A), and at the end of surgery (B).
The reason for the lack of corneal clearing in this study, as compared to animal studies, is unclear. We used the most concentrated formulation of iohexol available (350mg iodine/ml) and the exposure time was similar to the animal studies; however, it is possible that contrast agents with different refractive indices or longer durations of exposure may have been more effective. Furthermore, contrast media may have been more effective clearing agents in animal studies as in the animal studies the corneal scars were not longstanding. Effectiveness may also depend on scar characteristics such as depth and etiology.
Although the results of this first human pilot study do not support the use of iohexol as a corneal clearing agent, there was no evidence of toxicity from the treatment, and given the dramatic clearing reported in animal studies, further experimentation with contrast media of different refractive indices and using different treatment durations may be worthwhile.
Footnotes
Conflicts of Interest
None.
REFERENCES
- 1.Oshima Y, Shima C, Maeda N, Tano Y. Chandelier retroillumination-assisted torsional oscillation for cataract surgery in patients with severe corneal opacity. J Cataract Refract Surg. 2007;33:2018–2022. doi: 10.1016/j.jcrs.2007.07.055. [DOI] [PubMed] [Google Scholar]
- 2.Maurice DM. The structure and transparency of the cornea. J Physiol. 1957;136:263–286. doi: 10.1113/jphysiol.1957.sp005758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCally RL, Freund DE, Zorn A, Bonney-Ray J, Grebe R, de la Cruz Z, et al. Light-scattering and ultrastructure of healed penetrating corneal wounds. Invest Ophthalmol Vis Sci . 2007;48:157–165. doi: 10.1167/iovs.06-0935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Potts AM. Anatomic methods for study of the bulbus oculi. Am J Ophthalmol. 1968;65:155–163. doi: 10.1016/0002-9394(68)93579-4. [DOI] [PubMed] [Google Scholar]
- 5.Maurice DM. Clearing media for the eye. Br J Ophthalmol. 1987;71:470–472. doi: 10.1136/bjo.71.6.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ropo A, Nikki P, Ruusuvaara P, Kivisaari L. Comparison of retrobulbar and periocular injections of lignocaine by computerized tomography. Br J Ophthalmol. 1991;75:417–420. doi: 10.1136/bjo.75.7.417. [DOI] [PMC free article] [PubMed] [Google Scholar]