Abstract
Background
Pain and other sensations from an amputated or absent limb, called phantom pain and phantom sensations, are well-known phenomena.
Objective
The aim of this retrospective study was to evaluate the effects of anesthetic techniques on phantom pain, phantom sensations, and stump pain after lower limb amputation.
Methods
Ninety-two patients with American Society of Anesthesiologists physical status I to III were analyzed for 1 to 24 months after lower limb amputation in this retrospective study. Patients received general, spinal, or epidural anesthesia or peripheral nerve block for their amputations. Standardized questions were used to assess phantom limb pain, phantom sensation, and stump pain postoperatively. Pain intensity was assessed on a numeric rating scale (NRS) of 0 to 10. Patients' medical histories were determined from hospital records.
Results
Patients who received epidural anesthesia and peripheral nerve block perceived significantly less pain in the week after surgery compared with patients who received general anesthesia and spinal anesthesia (NRS [SD] values, 2.68 [1.0] and 2.70 [1.0], respectively). After approximately 14 to 17 months, there was no difference in phantom limb pain, phantom sensation, or stump pain among the anesthetic techniques for amputation.
Conclusions
In patients undergoing lower limb amputation, performing epidural anesthesia or peripheral nerve block, instead of general anesthesia or spinal anesthesia, might attenuate phantom and stump pain in the first week after operation. Anesthetic technique might not have an effect on phantom limb pain, phantom sensation, or stump pain at 14 to 17 months after lower limb amputation.
Key words: amputation stumps, anesthesia and analgesia, limb, phantom
Introduction
Different pathologic processes such as phantom sensations, phantom limb pain, and stump pain usually develop after lower limb amputation surgery. It has been reported in various trials that the estimated prevalence of phantom pain varies from 49% to 83%.1,2 This observed wide range might be due to terminology differences when defining phantom pain, phantom sensations, and stump pain.2
Phantom pain and sensations are defined as perceptions ranging from slight tingling to sharp, throbbing pain or aching that patients perceive relating to an extremity or an organ that is physically no longer a part of the body.3,4 Limb loss can occur as a result of either removal by surgical amputation or congenital limb absence. It is well known that bothersome sensations are generally perceived after amputation of an arm or a leg, but rarely, may also occur after the removal of a breast or an internal organ. Pain sensation varies from individual to individual.5–7
Although some risk factors, such as pain before the amputation, cause of amputation, prosthesis use, and years since amputation have been defined, the exact causes of painful and nonpainful phantom sensations are not known.3,8,9 Both peripheral and central occurrence mechanisms are debated on a theoretical basis.6 Phantom pain is a kind of neuropathic pain and occurs as a result of central and peripheral neuronal pathologies.10 As a suspected basic mechanism, the neuromatrix is defined as a neuronal organization that is genetically determined within individuals and modified by sensory experiences.11 According to this theory, abnormal impulses that reach the neuromatrix after an extremity amputation change the neuromatrix pattern, and this causes conversion of normal input to pain sensations, in other words, causes phantom pain. The interference of normal impulse traffic to the brain and excessive impulse discharge from damaged neurons after amputation are believed to be responsible for occurrence of phantom pain. Additionally, somatosensory pain memory can awaken after amputation, thus leading to phantom pain.12
There are many previous studies on phantom pain and sensation, mainly investigating efforts to prevent postoperative problems.13,14 However, only 2 studies exist that evaluated the effect of various anesthetic techniques on the occurrence of postoperative phantom pain, phantom sensation, and stump pain.3,15 In both studies, marked increases in phantom pain and sensation after general anesthesia were observed soon after amputation surgery. These studies compared the effects of general, spinal, and epidural anesthetic techniques. However, none of the studies compared the probable relation of peripheral nerve block with postoperative phantom pain sensation and stump pain. This study aimed to compare the impact of general anesthesia, spinal anesthesia, epidural anesthesia, and peripheral nerve block on postoperative incidence of phantom pain and sensation using our own data on this poorly researched subject.
Materials and Methods
Local ethics committee approval was provided for this study. Between April 2005 and July 2008, 92 patients who underwent lower limb amputation by general anesthesia, spinal, epidural, or peripheral nerve block were retrospectively evaluated. Other inclusion criteria were: (1) lower limb amputation within the last 1 to 24 months; (2) >18 years of age; (3) no previously performed amputation; (4) able to communicate well in the native language; (5) psychosocial assessment within normal limits; and (6) complete medical records.
Anesthetic Techniques
Anesthetic techniques used during the amputation process of all patients were investigated. The anesthesiologist decided on the choice of anesthetic method for each patient according to clinical condition. Completely standardized anesthetic techniques were used in the general, epidural, spinal anesthesia, and peripheral nerve block groups. In the general anesthesia group, anesthesia was initiated with 2.5 mg/kg propofol, 1 to 2 μg/kg fentanyl, and 0.1 mg/kg vecuronium or 0.6 mg/kg rocuronium intravenously, and then maintained with 1% to 2% sevoflurane or 5% to 6% desflurane and 70% nitrous oxide in oxygen. In the spinal anesthesia group, 3 mL of isobaric 0.5% levobupivacaine solution was aseptically and intrathecally administered to patients in a sitting or lateral position by a midline approach between the L3 and L4 intervertebral space. Epidural insertion was performed with patients in the sitting or lateral position at the Th12 to L1 intervertebral space after local infiltration of 2 to 3 mL of lignocaine 2%, using a midline approach. Epidural catheter was inserted cephalad 5 cm before patients received a 3 mL levobupivacaine 0.5% test dose. The epidural anesthesia group received 15 mL 0.5% isobaric levobupivacaine solution through epidural catheters with a single-shot in the lumbar region for surgical anesthesia. The peripheral nerve block group received 30 to 40 cc isobaric 0.5% levobupivacaine solution by popliteal block in the prone position or femoral nerve block in the supine position without catheter for surgical anesthesia. The spinal, epidural, or peripheral nerve block patients did not receive any sedative drugs, general anesthesia, or opioids intraoperatively. In other words, 2 anesthetic techniques were not applied at the same time. The spinal, epidural, or peripheral nerve block and general anesthesia patients received intramuscular nonsteroidal anti-inflammatory drugs, such as tenoxicam 20 mg first or if pain persisted, intravenous opioids (meperidine 1 mg/kg) for postoperative analgesia. The epidural catheter was removed at the end of surgery due to the procedures applied. Nonsteroidal anti-inflammatory drugs and opioids were used as a rescue analgesic if the patients requested or indicated a numeric rating scale (NRS) ≥4.
Evaluation Methods
Patients' date of amputation, demographic characteristics, associated medical disorders, main reason for amputation, region and level of amputation. and anesthetic technique used were determined from hospital records.
Standardized questionnaire NRS data for pain in the amputated limb were obtained by interviewing patients. In all cases, pain intensity was rated on an NRS ranging from 0 to 10 (0 = no pain; 10 = worst pain imaginable). Stump pain was defined as a painful feeling from the stump or the remaining part of the leg, whereas phantom sensation was defined as a nonpainful sensation from the removed part of the leg. Phantom limb pain was defined as a painful feeling from the removed part of the leg.3
Mean NRS values of pain intensity perceived during the preoperative period and the first 7 days after surgery were obtained from medical records. In the interview, patients were asked to define the number of days per month with pain symptoms during the month before the interview. They were also asked if they had any phantom sensation, phantom limb pain, or stump pain in the week preceding the interview. If a patient reported stump pain or phantom limb pain, that patient was asked if he or she was receiving any medication for analgesia. All of the patients were asked whether the pain affected his or her abilities to sleep at night, to concentrate, and to perform daily activities.
Statistical Analysis
Evaluation parameters were compared among the 4 groups according to the anesthetic techniques utilized during the amputation process. Results are expressed as mean [SD] (percentage). Normality distribution of variables was tested using the 1-sample Kolmogorov-Smirnov test. Groups were compared by 1-way ANOVA test for normally distributed data or by Kruskal-Wallis test for non-normally distributed data. Bonferroni's post hoc test was used when the significance difference was obtained. Categorical variables were compared using the χ2 test. A P value < 0.05 was considered statistically significant. Statistica 7.0 (StatSoft Inc., Tulsa, Oklahoma) statistical software was used for statistical analyses.
Results
Of the 100 patients assessed for eligibility, 8 patients were excluded because of failed spinal, epidural, or peripheral nerve block, and 2 anesthetic techniques were used for surgery. Therefore, 92 patients were analyzed according to the protocol and were included in this retrospective analysis (Figure), of whom 25 (27.1%) received general anesthesia, 25 (27.1%) spinal anesthesia, 22 (23.9%) epidural anesthesia, and 20 (20.2%) peripheral nerve block. The 4 groups were comparable in terms of age, sex, body mass index, and mean time after amputation (Table I). There was no difference among the 4 groups with regard to pain before amputation, associated medical disorders, main reason for amputation, and level and region of amputation (P > 0.05) (Table II). Although peripheral vascular disease was the most common associated medical disorder, ischemia was the main reason for amputation. More than half of the patients in all groups had an amputation below the knee. All these parameters, including region of amputation, were comparable among the groups (Table II).
Figure.
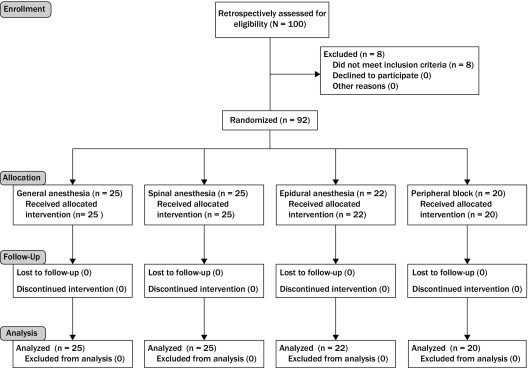
Flow diagram of study enrollment, allocation, follow-up, and analysis.
Table I.
Patients' demographic characteristics.
| Demographic Characteristics | General Anesthesia Group (n = 25) | Spinal Anesthesia Group (n = 25) | Epidural Anesthesia Group (n = 22) | Peripheral Block Group (n = 20) | P |
|---|---|---|---|---|---|
| Age, y | 61.44 (9.6) | 60.0 (12.3) | 57.18 (10.6) | 57.85 (8.6) | 0.468 |
| Gender, % male | 66.4 | 68.7 | 70.3 | 67.3 | 0.962 |
| ASA status (I/II/III) | 3/14/8 | 4/15/6 | 4/11/7 | 4/11/5 | 0.645 |
| BMI, kg/m2 | 24.81 (4.7) | 25.77 (2.9) | 25.73 (3.0) | 26.42 (3.4) | 0.455 |
| Mean time after amputation, mo | 16.36 (6.2) | 14.44 (5.0) | 15.45 (2.6) | 14.95 (2.9) | 0.287 |
ASA = American Society of Anesthesiologists; BMI = body mass index.
No statistically significant differences were obtained in any of the parameters among groups (P > 0.05).
Data are mean values (SD).
Table II.
Pain before amputation, associated medical disorders, and type of amputation.
| Characteristic | General Anesthesia Group (n = 25) | Spinal Anesthesia Group (n = 25) | Epidural Anesthesia Group (n = 22) | Peripheral Block Group (n = 20) | P |
|---|---|---|---|---|---|
| Pain before amputation (NRS) | 6.17 (2.0) | 5.76 (1.7) | 5.18 (1.2) | 5.30 (1.1) | 0.073 |
| Associated medical disorders, % | |||||
| Diabetes | 40.0 | 44.0 | 40.9 | 45.0 | 0.984 |
| Hypertension | 20.0 | 12.0 | 18.2 | 20.0 | 0.866 |
| MI | 8.0 | 12.0 | 9.1 | 10.0 | 0.970 |
| Peripheral vascular disease | 52.0 | 56.0 | 50.0 | 55.0 | 0.976 |
| Main reason for amputation, % | |||||
| Vascular infection | 12.0 | 12.0 | 18.2 | 15.0 | 0.920 |
| Trauma | 12.0 | 16.0 | 13.6 | 15.0 | 0.980 |
| Ischemia | 76.0 | 72.0 | 68.2 | 70.0 | 0.942 |
| Level of amputation, % | |||||
| Above knee | 28.0 | 20.0 | 22.7 | 15.0 | 0.761 |
| Knee | 20.0 | 28.0 | 18.2 | 20.0 | 0.845 |
| Below knee | 52.0 | 52.0 | 59.1 | 65.0 | 0.787 |
| Region of amputation, % | |||||
| Right foot | 40.0 | 48.0 | 50.0 | 50.0 | 0.885 |
| Left foot | 60.0 | 52.0 | 50.0 | 50.0 | 0.885 |
MI = myocardial infarction; NRS = numeric rating scale.
No statistically significant differences were obtained in any of the parameters among groups (P > 0.05).
Data are mean (SD).
Patients who received epidural anesthesia and peripheral nerve block perceived significantly less pain in the week after their surgery compared with patients who had received general anesthesia and spinal anesthesia (P < 0.001). Moreover, mean pain level during the first week after amputation was significantly higher in general anesthesia patients compared with spinal anesthesia patients (P < 0.001). After approximately 14 to 17 months, there was no difference in phantom limb pain, phantom sensation, or stump pain among the groups (Table III; P = 0.818, P = 0.926, P = 0.853, respectively). There was no difference among the 4 groups in terms of prosthesis usage (Table III; P = 0.971). Use of prostheses in the patients was <8 hours a day. There was no difference in phantom limb pain and stump pain parameters among the 4 anesthesia groups. Severity and frequency of phantom limb and stump pain were similar (Table III; P = 0.980, P = 0.931, P = 0.951, P = 0.936, respectively).
Table III.
Initial pain, phantom sensations, phantom and stump limb pain, and use of prosthesis after amputation.
| Characteristics | General Anesthesia Group (n = 25) | Spinal Anesthesia Group (n = 25) | Epidural Anesthesia Group (n = 22) | Peripheral Block Group (n = 20) | P |
|---|---|---|---|---|---|
| Pain during the first week after amputation (NRS) | 5.52 (1.3) | 4.20 (1.3)⁎ | 2.68 (1.0)⁎ | 2.70 (1.0)⁎ | 0.001 |
| Patients with phantom limb sensation during the week before interview, % | 76.0 | 68.0 | 72.7 | 75.0 | 0.926 |
| Patients with phantom limb pain during the week before interview, % | 56.0 | 44.0 | 54.5 | 55.0 | 0.818 |
| Phantom limb pain severity during the week before interview (NRS) | 2.64 (2.6) | 2.40 (2.6) | 2.68 (2.6) | 2.70 (2.7) | 0.980 |
| No. of days with phantom limb pain during the month before the interview | 7.20 (8.5) | 7.16 (8.3) | 8.77 (8.5) | 8.40 (8.2) | 0.931 |
| Patients with stump pain during the week before interview, % | 36.0 | 28.0 | 27.3 | 25.0 | 0.853 |
| Stump pain severity during the week before interview (NRS) | 1.60 (2.3) | 1.44 (2.4) | 1.50 (2.7) | 1.30 (2.4) | 0.951 |
| No. of days with stump pain during the month before the interview | 3.36 (5.8) | 3.84 (6.4) | 3.82 (6.5) | 4.70 (6.8) | 0.936 |
| Use of prosthesis, % | 16.0 | 20.0 | 18.1 | 15.0 | 0.971 |
NRS = numeric rating scale.
Data are mean (SD) or number of patients.
P compared to peripheral block, epidural anesthesia, and spinal anesthesia with general anesthesia.
Twenty-two percent or more of the patients used opioids for analgesia before amputation. There was no difference among the 4 groups with regard to the use of opioid and nonopioid medications for analgesia before amputation (Table IV; P = 0.942, P = 0.971). There was no difference among the 4 groups of patients regarding receipt of opioid and nonopioid analgesic use at the time of interview (Table IV; P = 0.971, P = 0.977). The patients received opioids or nonopioid agents intravenously or intramuscularly for postoperative analgesia. Nonopioid analgesics included nonsteroidal anti-inflammatory drugs (Table IV).
Table IV.
Use of analgesics before and after amputation.
| Characteristics | General Anesthesia Group (n = 25) | Spinal Anesthesia Group (n = 25) | Epidural Anesthesia Group (n = 22) | Peripheral Block Group (n = 20) | P |
|---|---|---|---|---|---|
| Use of opioid analgesics before amputation, % | 24.0 | 28.0 | 22.7 | 30.0 | 0.942 |
| Use of nonopioid analgesics⁎ before amputation, % | 16.0 | 20.0 | 18.1 | 15.0 | 0.971 |
| Use of nonopioid analgesics⁎ at the time of interview, % | 36.0 | 32.0 | 31.8 | 30.0 | 0.977 |
| Use of opioid analgesics at the time of interview, % | 20.0 | 16.0 | 18.1 | 15.0 | 0.971 |
No statistically significant differences were obtained in any of the parameters among groups (P > 0.05).
Nonopioid analgesics included nonsteroidal anti-inflammatory drugs.
There was no difference among the 4 groups as to functions affected by stump and phantom limb pain, including frequency of sleep, concentration, and daily activities (Table V; P = 0.989, P = 0.937, P = 0.988, respectively).
Table V.
Effect of phantom and stump limb pain on functions.
| Functions Affected by Stump and Phantom Limb Pain, % | General Anesthesia Group (n = 25) | Spinal Anesthesia Group (n = 25) | Epidural Anesthesia Group (n = 22) | Peripheral Block Group (n = 20) | P |
|---|---|---|---|---|---|
| Sleep | 32.0 | 28.0 | 31.8 | 30.0 | 0.989 |
| Concentration | 28.0 | 24.0 | 22.7 | 20.0 | 0.937 |
| Daily activities | 24.0 | 24.0 | 22.7 | 20.0 | 0.988 |
No statistically significant differences were obtained in any of the parameters among groups (P > 0.05).
Discussion
This study found that anesthetic technique had no effect on phantom limb pain, phantom sensation, or stump pain approximately 14 to 17 months after lower limb amputation. However, patients had significantly less pain in the first week after amputation if they received epidural anesthesia or peripheral nerve block compared with patients who received general anesthesia and spinal anesthesia. Results were also favorable in the spinal anesthesia group compared with the general anesthesia group in terms of pain during the first week after amputation.
Complex multifactorial interactions involving peripheral nerves, the central nervous system (CNS), the sympathetic system, psychologic overlay, and genetic predisposition have all been implicated for the occurrence of phantom pain and sensations.1,16 As the exact mechanisms of this pain syndrome are still unknown, many risk factors have been identified to estimate the occurrence of phantom pain and/or sensations, such as age, gender, the cause of amputation, pain before amputation, prosthesis use, and years elapsed since amputation.17,18 However, not all of the risk factors have been consistently implicated by all previous studies. Even so, the demographic and amputation-related characteristics of the patients in the 4 groups were investigated for comparability and to erase the concern that these factors might have conflicted the final results. Fortunately, the 4 groups in this study showed homogeneous results relating to age, gender, pain before amputation, associated medical disorders, main reason for amputation, cause of amputation, level of amputation, use of opioids before amputation, prosthesis use, and years elapsed since amputation.
Phantom limb pain occurs soon after amputation and can be long lasting.19 Jensen et al17 found that phantom limb pain occurred within 8 days after amputation in 72% of adult patients. Of all our patients, 81.52% had phantom and stump pain during the first week after surgery. Nikolajsen et al18 observed that the incidence of phantom pain did not decrease 6 months after lower limb amputation, although there was a decrease in the incidence and intensity of intermittent pain attacks. Although we observed that the mean intensity of pain decreased, this group of patients continued to sense phantom pain at an average of 14 to 17 months after lower limb amputation.
The main investigation point of this study was the probable impact of various anesthetic techniques used during the amputation process on the occurrence of phantom pain and sensations. It is believed that regional anesthesia, by preventing the establishment of central sensitization, may play a role in reducing the incidence of acute and chronic pain. Moreover, because the surgical neurogenic inflammatory response may provide a source of nociceptive input into the CNS for a prolonged period, a continuous infusion of local anesthetic postoperatively may prevent the establishment of central sensitization.20 Gehling et al21 reported that perioperative epidural block was an effective prophylaxis for phantom limb pain, adding that perioperative epidural block did not completely abolish phantom limb pain, but increased the number of patients with a milder form of phantom pain. As in some other studies, this study found that one of the regional anesthesia techniques, epidural block, was advantageous for phantom limb pain, phantom sensation, or stump pain with lower pain intensities, especially during the first week after amputation. However, this advantage seemed to disappear at an average of 14 to 17 weeks after amputation.
The new finding in this study was that peripheral block technique was also beneficial, avoiding further pain and other bothersome sensations during the first week after surgery. Peripheral blocks are generally investigated for their analgesic efficacy during or after the amputation process. Despite some early benefits of epidural blocks, there was no difference in pain between the epidural block and perineural block in the postoperative period.22,23 In this study, peripheral blocks with levobupivacaine was applied in all surgical operations as an anesthetic technique. With this technique, we observed better results postoperatively compared with general and spinal anesthesia; similar results were found compared with epidural blocks. Targeting the nerves correctly by a stimulator might explain the benefits of this technique.
Only a few studies have evaluated the effect of spinal anesthesia on the occurrence of postoperative phantom pain, phantom sensation, and stump pain. The study of Ong et al3 showed that patients who received epidural anesthesia and those who received spinal anesthesia recalled less pain compared with general anesthesia in the week after surgery. In this study, we observed a similar beneficial effect of spinal anesthesia on pain in the first week after amputation compared with patients who received general anesthesia. However, patients had significantly less pain in the first week if they received epidural anesthesia or peripheral nerve block compared with patients who received spinal anesthesia.
Risk factors for exacerbation of phantom pain after regional anesthesia are poorly understood, because there are few studies addressing this issue.24,25 In patients with diabetes and leprosy, spinal anesthesia carries more risk than epidural anesthesia for further phantom pain and sensations.24 In this study, diabetes-associated amputation using spinal anesthesia was recorded at a rate of 44%. Although the 4 groups in this study showed homogeneous results relating to risk factors, this coincidence of spinal anesthesia and diabetes might simultaneously constitute phantom pain.
The study was limited by several factors, particularly the sample size. A larger sample size might have provided power to detect differences not observed in this analysis. Another limitation resulted from having multiple anesthesiologists deciding the choice of anesthesia according to the clinical condition of the patient. Although standard evaluation criteria exist for the determination of anesthetic requirements, bias might have been introduced, and the results of the study might have been affected. In addition, the retrospective study design might have resulted in significant bias for frequencies and severity of pain symptoms. However, the results are consistent with data of other prospective studies.3,15
Conclusions
Patients experienced significantly less pain during the first week after their amputation if they received epidural or peripheral nerve block compared with patients who received general anesthesia or spinal anesthesia. Anesthetic technique might not affect stump pain, phantom sensation, or phantom limb pain at approximately 14 to 17 months after lower limb amputation. Further studies are needed to determine whether patients undergoing lower limb amputation may benefit from epidural or peripheral blocks instead of general anesthesia or spinal blocks.
Acknowledgments
The authors have indicated that they have no other conflicts of interest regarding the content of this article. Drs. Sahin, Colak, Arar, and Birtane coordinated the study. Drs. Sahin, Tutunculer, and Yılmaz collected the data. Sahin, Birtane, and Sut helped draft the manuscript. Drs. Sahin and Sut conceived and designed the study and performed the statistical analysis. All of the authors read and approved the final manuscript.
References
- 1.Sherman R.A., Sherman C.J., Parker L. Chronic phantom and stump pain among American veterans: results of a survey. Pain. 1984;18:83–95. doi: 10.1016/0304-3959(84)90128-3. [DOI] [PubMed] [Google Scholar]
- 2.Kalauokalani D.A.K., Loeser J.D. Phantom limb pain. In: Crombie I.K., editor. Epidemiology of Pain. IASP Press; Seattle, WA: 1999. pp. 143–153. [Google Scholar]
- 3.Ong B.Y., Arneja A., Ong E.W. Effects of anesthesia on pain after lower-limb amputation. J Clin Anesth. 2006;18:6000–6004. doi: 10.1016/j.jclinane.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 4.Ehde D.M., Czerniecki J.M., Smith D.G. Chronic phantom sensations, phantom pain, residual limb pain, and other regional pain after lower limb amputation. Arch Phys Med Rehabil. 2000;81:1039–1044. doi: 10.1053/apmr.2000.7583. [DOI] [PubMed] [Google Scholar]
- 5.Dijkstra P.U., Geertzen J.H.B., Stewart R., Van der Schans C.P. Phantom pain and risk factors: a multivariate analysis. J Pain Symptom Manage. 2002;24:578–585. doi: 10.1016/s0885-3924(02)00538-9. [DOI] [PubMed] [Google Scholar]
- 6.Sherman R.A., Katz J., Marbach J.J., Heermann-Do K. Locations, characteristics, and descriptions. In: Sherman R.A., editor. Phantom Pain. Plenum Press; New York: 1997. pp. 1–31. [Google Scholar]
- 7.Kroner K., Knudsen U.B., Lundby L., Hvid H. Long-term phantom breast syndrome after mastectomy. Clin J Pain. 1992;8:346–350. doi: 10.1097/00002508-199212000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Wartan S.W., Hamann W., Wedley J.R., McColl I. Phantom pain and sensation among British veteran amputees. Br J Anaesth. 1997;78:652–659. doi: 10.1093/bja/78.6.652. [DOI] [PubMed] [Google Scholar]
- 9.Kooijman C.M., Dijkstra P.U., Geertzen J.H. Phantom pain and phantom sensations in upper limb amputees: An epidemiological study. Pain. 2000;87:33–41. doi: 10.1016/S0304-3959(00)00264-5. [DOI] [PubMed] [Google Scholar]
- 10.Flor H. Phantom-limb pain: characteristics, causes, and treatment. Lancet Neurol. 2002;1:182–189. doi: 10.1016/s1474-4422(02)00074-1. [DOI] [PubMed] [Google Scholar]
- 11.Hill A. Phantom limb pain: a review of the literature on attributes and potential mechanisms. J Pain Symptom Manage. 1999;17:125–142. doi: 10.1016/s0885-3924(98)00136-5. [DOI] [PubMed] [Google Scholar]
- 12.Melzack R. Pain–an overview. Acta Anesthesiol Scand. 1999;43:880–884. doi: 10.1034/j.1399-6576.1999.430903.x. [DOI] [PubMed] [Google Scholar]
- 13.Nikolajsen L., Ilkjaer S., Christensen J.H. Randomised trial of epidural bupivacaine and morphine in prevention of stump and phantom pain in lower-limb amputation. Lancet. 1997;350:1353–1357. doi: 10.1016/S0140-6736(97)06315-0. [DOI] [PubMed] [Google Scholar]
- 14.Jahangiri M., Jayatunga A.P., Bradley J.W., Dark C.H. Prevention of phantom pain after major lower limb amputation by epidural infusion of diamorphine, clonidine and bupivacaine. Ann R Coll Surg Engl. 1994;76:324–326. [PMC free article] [PubMed] [Google Scholar]
- 15.Ugur F., Esmaoglu A., Akin A. Does spinal anesthesia decrease the incidence of phantom pain? Pain Clinic. 2006;18:187–193. [Google Scholar]
- 16.Postone N. Phantom limb pain: A review. Int J Psychiatry Med. 1987;17:57–70. doi: 10.2190/pkg8-mduw-urcq-h2q2. [DOI] [PubMed] [Google Scholar]
- 17.Jensen T.S., Krebs B., Nielsen J., Rasmussen P. Phantom limb, phantom pain and stump pain in amputees during the first six months following amputation. Pain. 1983;17:243–256. doi: 10.1016/0304-3959(83)90097-0. [DOI] [PubMed] [Google Scholar]
- 18.Nikolajsen L., Ilkjaer S., Kroner K. The influence of pre-amputation pain on postamputation stump and phantom pain. Pain. 1997;72:393–405. doi: 10.1016/s0304-3959(97)00061-4. [DOI] [PubMed] [Google Scholar]
- 19.Melzack R. Phantom limb pain: implications for treatment of pathologic pain. Anesthesiology. 1971;35:409–419. [PubMed] [Google Scholar]
- 20.Cousins M.J., Power I., Smith G. Labat lecture: pain—a persistent problem. Reg Anesth Pain Med. 2000;25:6–21. doi: 10.1016/s1098-7339(00)80005-x. [DOI] [PubMed] [Google Scholar]
- 21.Gehling M., Tryba M. Prophylaxis of phantom pain: is regional analgesia ineffective? Schmerz. 2003;17:11–19. doi: 10.1007/s00482-002-0198-2. [DOI] [PubMed] [Google Scholar]
- 22.Fisher A., Meller Y. Continuous postoperative regional analgesia by nerve sheath block for amputation surgery—A pilot study. Anesth Analg. 1991;72:300–303. doi: 10.1213/00000539-199103000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Lambert A.W., Dashfield A.K., Cosgrove C. Randomized prospective study comparing preoperative epidural and intraoperative perineural analgesia for the prevention of postoperative stump and phantom limb pain following major amputation. Reg Anesth Pain Med. 2001;26:316–321. doi: 10.1053/rapm.2001.23934. [DOI] [PubMed] [Google Scholar]
- 24.Kato M., Tada F., Abe T. Severe lightning pain during spinal anesthesia in a patient with diabetic neuropathy. Masui. 2000;49:1021–1023. [PubMed] [Google Scholar]
- 25.Schmidt A.P., Takahashi M.E., Posso I.P. Phantom limb pain induced by spinal anesthesia. Clinics (Sao Paulo) 2005;60:263–264. doi: 10.1590/s1807-59322005000300014. [DOI] [PubMed] [Google Scholar]


