Abstract
Objectives:
To determine the level of knowledge of primary health care physicians and the barriers perceived in the management of overweight and obesity in the Eastern Province of Saudi Arabia.
Setting:
Primary health care centers in Dammam and Al-Khobar cities, Saudi Arabia.
Design:
A cross-sectional study.
Materials and Methods:
One hundred and forty-nine physicians were surveyed. Data were collected with a specially made anonymous, self-administrated, structured questionnaire with a Cronbach alpha reliability of 0.85, and content validity by five experts was used to measure the knowledge and barriers from several different aspects of care provided by primary health care centers to the overweight and obese.
Results:
One hundred and thirty (87%) physicians responded. More than two-thirds of the respondents considered themselves as key players in the management of obesity. However, only one-third believed that they were well prepared to treat obesity. Eighty-three per cent of the respondents had a negative attitude toward the concept of overweight and obesity. It was noted that 76.9% of physicians advised patients to control their weight with sport and exercise together with low calorie diet. Sixty percent of the respondents used body mass index to diagnose obesity. Seventy-two percent of respondents did not use weight reduction medications to treat obesity. Lack of training, poor administrative support, and time constraints were identified as barriers in managing overweight and obesity.
Conclusion:
Respondents were aware of the magnitude of overweight and obesity as a major public health problem in Saudi Arabia, and they were also aware of the correct definition of overweight and obesity, as well as its effect in increasing mortality. Better training is required to improve some areas of awareness and management of the conditions.
Keywords: Barriers, knowledge, obesity, overweight, primary health care physicians, Saudi Arabia
INTRODUCTION
World Health Organization (WHO) defines overweight as a body mass index (BMI) of 25 to 29.9 kg/m2 and obesity as a BMI of ≥30 kg/m2.[1]
Overweight and obesity represent a rapidly growing pandemic of public health problems that affect virtually all ages and socio-economic groups.[1,2] They are associated with hypertension, ischemic heart disease, gallstones, osteoarthritis, type 2 diabetes, sleep apnea, malignancy,[3,4] emotional and social problems in children,[4] impaired quality of life,[4] self-esteem,[5] and depression.[6]
Obesity is the second leading cause of preventable death in the United States of America (USA).[7] The prevalence rate of obesity in adults in the USA is 30.5%, and the percentage of overweight was 64.5% in 2000.[8]
In Arab and gulf countries, the prevalence of obesity and overweight is increasing in both adults and children.[9,10,11] In Qatar, it is estimated that 29.3% of females and 17.4% of males are obese.[10] In Bahrain, the prevalence of obesity was more significant among females, 32%, than males, 25%, throughout all age groups.[11] In Kuwait, the prevalence of overweight and obesity increased by 20.6% and 15.4% and by 13.7 and 8.4% among men and women, respectively.[9] In Saudi Arabia, 1 in every 6 children aged 6 to 18 years old is obese.[12]
Modest weight control has been shown to improve many risk factors for cardiovascular, pulmonary, and cancer conditions.[1,7,13,14] Primary health care physicians (PHCPs) are ideally placed to play a dominant role in assessing and managing obesity. Guidelines for the management of obesity have been developed in several countries[7,15] to promote physical activity and dietary counseling. The United States Preventive Services Task Force recommends that clinicians screen patients for obesity and offer intensive counseling and behavioral interventions.[16]
Physicians are the most frequently used source of health information[17] and have been found to be more cost-effective than dietitians in nutritional counseling for obese and other patients.[18] Despite these facts, primary health care (PHC) is still underutilized for obesity counseling[19] and its capacity is usually diminished by a number of limitations[20] such as short consultation time, patients’ low motivation and non-compliance, inadequate teaching materials, lack of reimbursement, low level of physicians’ confidence, and a shortage of dietitians.[21,22]
Some studies have shown that general practitioners do not have sufficient relevant knowledge and skills to effectively manage overweight and obesity.[22,23] Inadequate knowledge of nutrition has also been reported by the physicians themselves or documented objectively.[22,24] They often fail to counsel patients on nutrition and weight management[25,26,27,28] and exhibit a lack of training and skills in managing obesity.[21,29,30,31]
It has been suggested that the management of obesity in PHC is deficient mainly as a result of the low identification of the status of patients’ weight and ineffectual efforts of physicians at intervention.[15] Less than half of obese individuals are advised by their physician[7] to lose weight.[15] Overweight and mild obesity is under-recognized and under-treated unless they are associated with other medical complications.[7]
Furthermore, health professionals, including physicians, may have a negative attitude towards obese patients,[25,32] which may be one of the reasons for the low success rate of obesity management.[33] Adequate training may increase physician involvement in overweight prevention and treatment.[34,35] Exploring physicians’ awareness is important for the design of special training programs to manage deficiencies in knowledge.
The aim of the present study was to determine the knowledge level of PHCPs in the Eastern Province of Saudi Arabia and the perceived possible barriers in managing overweight and obesity.
MATERIALS AND METHODS
This cross-sectional study was conducted to include all (149) PHCPs at 30 primary health care centers (PHCCs) in Al-Dammam city (22 centers with 76 physicians) and Al-Khobar city (8 centers with 73 physicians), in the Eastern Province of Saudi Arabia.
Data were collected during the period December 2009 to March 2010, by using an anonymous, self-administrated, structured questionnaire to find-out PHCPs’ knowledge of overweight and obesity and the possible barriers to successful intervention. The questionnaire was piloted on 35 family medicine residents to test its application for the main study. Based on the focus group discussion and questionnaire analysis, some relevant changes were made. The questionnaire consisted of three parts: Part one included: Personal data comprising age, gender, marital status, nationality, language, experience, average number of patients seen per week, position, last qualification, training of weight management and duration, exercise counseling and duration, source of information, and the weight and height. Part two included: Seventeen statements testing knowledge of health risk of obesity, diagnosis, lifestyle (nutrition, physical exercise). The answers to the statements were categorized into (Yes, which indicated the correct answer, No, which indicated the wrong answer, and I don’t know, as judged by PHCPs). Part three consisted of nine statements to measure the responses on a 5-point Likert scale (“strongly agree,” “agree,” “Neutral,” “disagree,” and “strongly disagree.”) regarding barriers to proper overweight and obesity management. Agreement scores for the items were calculated on the scale (minimum mean = 1 for strongly disagree and maximum mean = 5 for strongly agree). Agree indicated 4 or 5 (agree and strongly agree), and disagree indicated 1 or 2 (disagree and strongly disagree), and 3 for neutral responses.
These barriers were: Lack of training, administrative support, poor system, failure rate, facilities, dietician, time constraints, patient adherence to the plan, and physician confidence in management. The mean agreement scores were calculated.
Cronbach alpha reliability test was used to test the internal consistency of the items. Content validity was tested by experts. The collected data were recorded, coded, and verified, and statistical analysis was done using Statistical Package for Social Sciences (SPSS) version 16.0. Descriptive statistics (means, standard deviations, frequencies, and percentages) were calculated. As the tables are categorical, the Chi-square was used to test for the differences between qualitative data. Differences were considered significant at P < 0.05 at 95% confidence interval. Ethical considerations were considered by obtaining approval to conduct the study and assuring all participants of confidentiality.
RESULTS
One hundred and thirty questionnaires were returned yielding a response rate of 87%. Cronbach alpha reliability test was 0.85. The mean age of participants was 40.77 (± SD 8.26) years with a minimum age of 23 years and a maximum of 61 years.
The socio-demographic characteristics of the primary care physicians are shown in Table 1. Seventy participants (53.8%) were males, most of whom (70.8%) were married, and non-Saudis were 64.6%. Participants were predominantly Arabic speakers (76.9%). Seventy-five of the participants (57.7%) had a bachelors degree only, 8.5% were family physicians, and 24.6% were from other specialties.
Table 1.
Characteristics of responding primary health care physicians, Eastern Province of Saudi Arabia, 2010
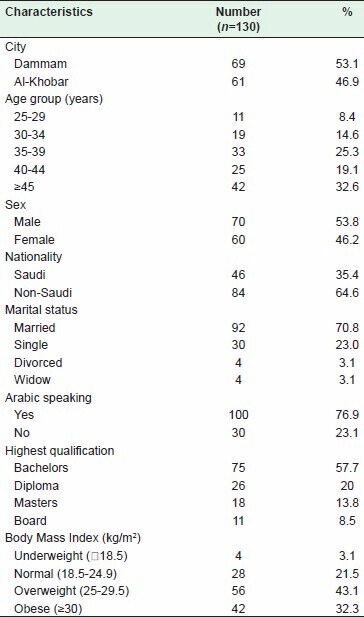
Participants had been in practice for an average of 12 (± SD 7.60) years. The average patient encounter was 281.82 (± SD 142.88) patients per week with a maximum of 700 patients encounter and minimum of 20 patients per week. The majority of the respondents (80%) reported that they had not received any training on overweight or obesity management, and 81.5% were not trained on physical exercise counseling. Based on their self-reported weights and heights, 43.1% of the participants were themselves overweight and 32.3% were obese.
Comparing the responses of obese and overweight physicians to those with normal BMI, it was found that the obese and overweight physicians were more in agreement with the statements “lack of physicians’ confidence in managing overweight and obesity” than those with normal BMI (P = 0.040); “I consider myself overweight” (P < 0.05). On the other hand, more of them disagreed with the statement “I feel that primary health care centers are well prepared to manage overweight and obesity (P = 0.047).
The majority of respondents (73.8%) used textbooks as a source of information, 63.9% used the Internet, 55.4% attended CME, and 28.5% read medical journals.
Table 2 shows that 69.2% of the respondents answered correctly that the prevalence of obesity in Saudi Arabia was high; 81.5% of the respondents answered correctly that obesity increased mortality rate; 63.1% were aware of the correct definition of obesity (BMI = 30 kg/m2 ), and 60.8% correctly identified abdominal obesity (waist circumference >102 cm for males and >88 cm for females). Only 65.4% of respondents correctly answered that in the absence of cardiovascular risk, physicians were not supposed to use weight reduction medication on their patients with BMI of less than 30. The differences were found to be statistically significant (P < 0.05).
Table 2.
Comparison between correct and wrong answers regarding primary care physicians’ knowledge about overweight and obesity, Eastern Province of Saudi Arabia, 2010 (n=130)
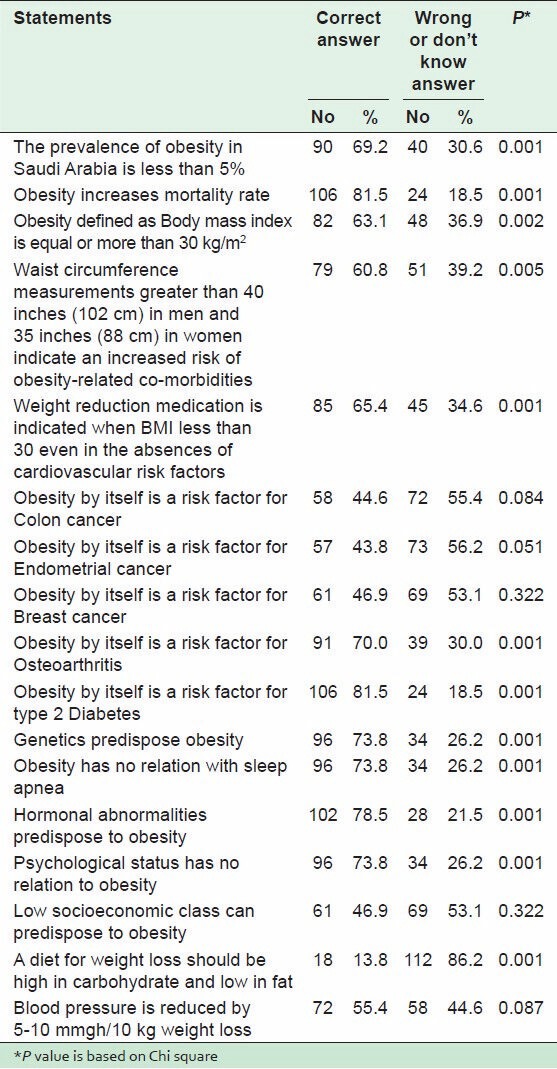
Regarding diseases associated with obesity, physicians were aware that obesity was a risk factor for osteoarthritis (70% responded correctly) and for type 2 diabetes (81.5% responded correctly). The differences were statistically significant (P < 0.05).
In terms of factors contributing to obesity, 73.8% of respondents identified genetic factors and sleep apnea as determinants for obesity, 78.5% of physician identified hormonal abnormalities as risk factors for obesity and 73.1% knew that psychological status was a predisposing factor for obesity, and less than 50% of respondents knew that low socio-economic status was one of the determinants of obesity.
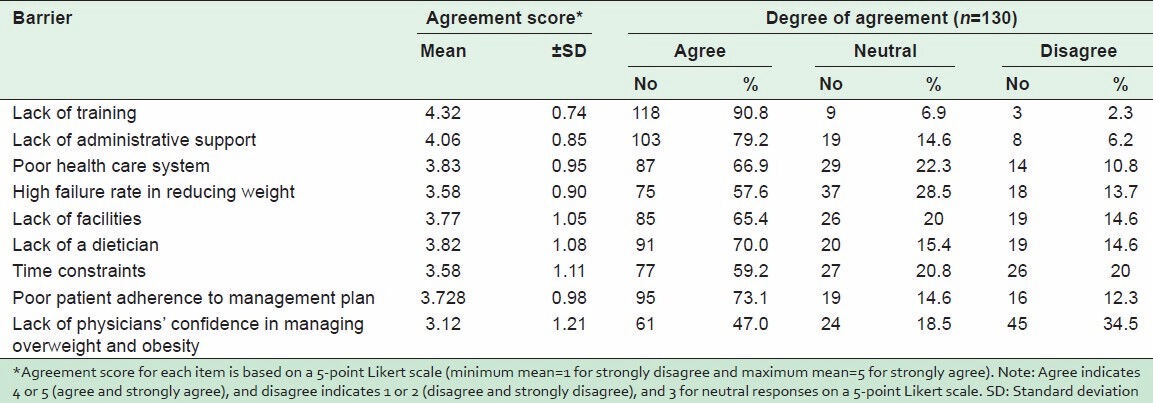
Table 3 shows the mean agreement scores, numbers, and percentages of possible barriers for managing overweight and obesity. The respondents were in agreement that lack of training (mean score of 4.32 ± 0.74) and lack of administrative support (mean score of 4.06 ± 0.85) were the top main barriers to effective management of obesity. However, they were neutral (mean score of 3.12 ± 1.21) in reporting the lack of physicians’ confidence in managing obesity as a barrier.
Table 3.
Mean agreement scores, numbers, and percentages of possible barriers for managing overweight and obesity as perceived by the respondents, Eastern Province of Saudi Arabia, 2010
DISCUSSION
Obesity is a global health problem, especially in the developing world.[12] PHCPs working in Dammam and Al-Khobar cities in the present study were in a ratio of 1.1:1. Their mean age of 41 years and the average work experience of 12 years at PHCCs indicate a young physician population who has to deal with the recent trends in managing overweight and obesity. Therefore, they are suitable as targets for educational programs for improving obesity care in their work.
The study findings indicate that less than 20% of the participants had received any training in the management of obesity. This is consistent with other studies that have reported a lack of training and competence in obesity management.[21,29,30,31] Training is essential to maintaining physicians’ knowledge and skills up to date and in helping them in their practice of weight control programs. Despite guidelines on the counseling and management of obesity,[7,36] only one-third of obese patients reported having received a diagnosis that they were obese or being given any weight-related counseling by their physicians.[37] Physicians who had good training on obesity screening and counseling during their residency training were more likely to report that they always discussed diet and exercise with their obese patients.[30] Also, patients who get counseling on weight control are twice more likely to report that they were currently trying to lose weight.[27,38] However, many overweight and obese patients reported their desire to get more intensive management for weight loss than what their physicians were providing.[39]
Physicians have to have normal BMI so that they can be role models for their patients to encourage them in their adherence to the recommendations on obesity management. In addition, physicians with normal BMI were more likely to engage their obese patients in weight loss discussions and have greater confidence in providing diet and exercise counseling than overweight and obese physicians.[40] These findings of the study demonstrate that more than 75% of the participants had abnormally high BMI, which could affect the outcome of obesity management. This high prevalence is much more than in all other reported studies.[8,9,10,11] An in-depth study is needed to investigate this issue.
Interestingly, 42% of the respondents had post-graduate qualifications. A postgraduate qualification is beneficial in managing overweight and obesity competently. This lack of post-graduate qualification might be a contributing factor to the less than satisfactory knowledge level.
The finding that only 28.5% of participants consulted medical journals for information may indicate the lack of the proper use of literature in managing overweight and obesity. This may be the result of poor training and lack of proper resources made available to help physicians access recent articles in the field.
It is obvious that respondents were aware of the magnitude of obesity as a major public health problem in Saudi Arabia. In fact, a large proportion of the physicians were also aware of the correct definition of obesity as well as increased mortality with obesity [Table 2]. Moreover, less than 70% of physicians correctly gave the answer that when BMI was less than 30 and there was no cardiovascular risk, physicians were not supposed to give weight reduction medication to their patients even if the weight-loss program seemed ineffective and patients were unable to maintain the lost weight. The reasons for the disparity between the level of knowledge shown by physicians in the management of obesity and their perceived low level of effectiveness are not clear. Whether this is the result of real experience or from published literature on long-term obesity treatment[41] remains to be established. The majority of physicians were aware of the factors that contribute to obesity such as genetic, hormonal abnormalities, and the psychological status [Table 2]; this is similar to what was found in an earlier study.[42]
The major constraints identified by PHCPs against the management of obesity were related to a lack of primary health care administrative support and poor health care system, lack of training, high failure rate in weight reduction, lack of facilities, and lack of dieticians, time constraints, and poor patient adherence to management plans. These findings are similar to those of other reported studies.[30,43,44] Physicians’ confidence in managing overweight and obesity is just average [Table 3]. The major constraints identified by physicians in their management of obesity related to the PHC system and/or factors related to patients. Short consultation time reported by the majority of physicians in other studies[34,45,46] is a well-known barrier to the management of the preventive services in primary health care centers. The absence of clinical guidelines was reported as an important limiting factor; however, in some developed countries where there are national guidelines, only a few practitioners demonstrated good awareness of them.[45,46]
The limitations of this study are the subjectivity of a self-administered questionnaire and the possibility that PHCPs discussed the answers with each other. In addition, this study was limited to the population of primary care physicians in Dammam and Al-Khobar cities; so, any generalization to other populations may be inappropriate.
CONCLUSION
Based on these findings, the PHCPs in general exhibited correct knowledge of overweight and obesity, except on the items that stated that obesity by itself was a risk factor for colon cancer, for endometrial cancer, for breast cancer and that low socio-economic class could predispose to obesity. There is a need for better physician training and greater administrative support within the primary health care system to improve overweight and obesity management in Saudi Arabia.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.WHO. Report of the WHO consultation on obesity. Geneva: WHO; 1998. [Last accessed on 2013 Apr 16]. Prevention and management of the global epidemic of obesity. Available from: http://whqlibdoc.who.int/hq/1998/WHO_NUT_NCD_98.1_(p1.158).pdf . [Google Scholar]
- 2.Flegal KM, Troiano RP. Changes in the distribution of body massindex of adults and children in the US population. Int J Obes Relat Metab Disord. 2000;24:807–18. doi: 10.1038/sj.ijo.0801232. [DOI] [PubMed] [Google Scholar]
- 3.Mikhail N, Tuck ML. Epidemiological and clinical aspects of obesity related hypertension. J Clin Hypertens. 2000;2:41–5. [PubMed] [Google Scholar]
- 4.Schwimmer JB, Burwinkle TM, Varni JW. Health- related quality of life in severely obese children and adolescents. JAMA. 2003;289:1813–9. doi: 10.1001/jama.289.14.1813. [DOI] [PubMed] [Google Scholar]
- 5.French SA, Story M, Pery SL. Self esteem and obesity in children and adolescents: A literature review. Obes Res. 1995;3:479–90. doi: 10.1002/j.1550-8528.1995.tb00179.x. [DOI] [PubMed] [Google Scholar]
- 6.Needham B, Crosnone R. Overweight and depression during adolescence. J Adolesc Health. 2004;36:48–55. doi: 10.1016/j.jadohealth.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 7.Clinical guidelines on the identification evaluation and treatment of overweight and obesity in adults: The evidence report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51–210S. [PubMed] [Google Scholar]
- 8.Flegal K, Carroll M, Ogden C, Johnson C. Prevalence and trends in obesity among US adults, 1999-2000. J Am Med Assoc. 2002;288:1723–7. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 9.Al-Jeheidli AH, Moquddan FI, Al-Rumh MK, Salmin NN. General Practitioners Attitudes and Practices toward Managing Obesity. Kuwait Med J. 2007;39:138–43. [Google Scholar]
- 10.Al-Muraikhi AE, Al-Kuwari MG. Primary Care physicians’ knowledge, attitude, and practice toward obesity management in Qatar. Middle East J Fam Med. 2008;10:3–7. [Google Scholar]
- 11.James PT, Leach R, Kalamara E, Shayeghi M. The worldwide obesity epidemic. Obes Res. 2001;9(Suppl 4):228–33S. doi: 10.1038/oby.2001.123. [DOI] [PubMed] [Google Scholar]
- 12.Al-Nozha MM, Al-Mazrou YY, Al-Maatouq MA, Arafah MR, Khalil MZ, Khan NB, et al. Obesity in Saudi Arabia. Saudi Med J. 2005;26:824–9. [PubMed] [Google Scholar]
- 13.Blackburn GL. Effects of weight loss on weightrelated risk factors. In: Brownell KD, Fairburn CG, editors. Eating disorders and obesity: A comprehensive handbook. New York: The Guilford Press; 1995. pp. 406–10. [Google Scholar]
- 14.McTigue KM, Harris R, Hemphill B, Lux L, Sutton S, Bunton AJ, et al. Screening and interventions for obesity in adults: Summary of the evidence for the US Preventive Services Task Force. Ann Intern Med. 2003;139:933–49. doi: 10.7326/0003-4819-139-11-200312020-00013. [DOI] [PubMed] [Google Scholar]
- 15.Basdevant A, Laville M, Ziegler O Association Française d’Etudes et de Recherches sur l’Obésité (AFERO); Association de Langue Française pour l’Etude du Diabète et des Maladies Metaboliques (ALFEDIAM); Société de Nutrition et de Diététique de Langue Française (SNDLF) Recommendations for the diagnosis, the prevention and the treatment of obesity. Diabetes Metab. 2002;28:146–50. [PubMed] [Google Scholar]
- 16.U.S. Preventive Services Task Force. Screening for obesity in adults: Recommendations and rationale. Ann Intern Med. 2003;139:90–2. doi: 10.7326/0003-4819-139-11-200312020-00012. [DOI] [PubMed] [Google Scholar]
- 17.Truswell AS, Hiddink GJ, Blom J. Nutrition guidance by family doctors in a changing world: Problems, opportunities, and future possibilities. Am J Clin Nutr. 2003;77:1089–92S. doi: 10.1093/ajcn/77.4.1089S. [DOI] [PubMed] [Google Scholar]
- 18.Olsen J, Willaing I, Ladelund S, Jorgensen T, Gundgaard J, Sorensen J. Cost-effectiveness of nutritional counseling for obese patients and patients at risk of ischemic heart disease. Int J Technol Assess Health Care. 2005;21:194–202. [PubMed] [Google Scholar]
- 19.Mercer SL, Green LW, Rosenthal AC, Husten CG, Khan LK, Dietz WH. Possible lessons from the tobacco experience for obesity control. Am J Clin Nutr. 2003;77(Suppl 4):1073–82S. doi: 10.1093/ajcn/77.4.1073S. [DOI] [PubMed] [Google Scholar]
- 20.Glanz K. Review of nutritional attitudes and counseling practices of primary care physicians. Am J Clin Nutr. 1997;65(Suppl 6):2016–9S. doi: 10.1093/ajcn/65.6.2016S. [DOI] [PubMed] [Google Scholar]
- 21.Kushner RF. Barriers to providing nutrition counseling by physicians: A survey of primary care practitioners. Prev Med. 1995;24:546–52. doi: 10.1006/pmed.1995.1087. [DOI] [PubMed] [Google Scholar]
- 22.Murray S, Narayan V, Mitchell M, Witte H. Study of dietetic knowledge among members of the primary health care team. Br J Gen Pract. 1993;43:229–31. [PMC free article] [PubMed] [Google Scholar]
- 23.Price JH, Desmond SM, Krol RA, Snyder FF, O’Connell JK. Family practice physicians’ beliefs, attitudes, and practices regarding obesity. Am J Prev Med. 1987;3:339–45. [PubMed] [Google Scholar]
- 24.Al-Numair KS. Nutrition knowledge of primary care physicians in Saudi Arabia. Pakistan J Nutr. 2004;3:344–7. [Google Scholar]
- 25.O’Brien SH, Holubkov R, Reis EC. Identification, evaluation, and management of obesity in an academic primary care center. Pediatrics. 2004;114:154–9. doi: 10.1542/peds.114.2.e154. [DOI] [PubMed] [Google Scholar]
- 26.Ruser CB, Sanders L, Brescia GR, Talbot M, Hartman K, Vivieros K, et al. Identification and management of overweight and obesity by internal medicine residents. J Gen Intern Med. 2005;20:1139–41. doi: 10.1111/j.1525-1497.2005.0263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nawaz H, Adams ML, Katz DL. Weight loss counseling by health care providers. Am J Public Health. 1999;89:764–7. doi: 10.2105/ajph.89.5.764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Loureiro ML, Nayga RM., Jr Obesity, weight loss, and physician’s advice. Soc Sci Med. 2006;62:2458–68. doi: 10.1016/j.socscimed.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 29.Jay M, Gillespie C, Ark T, Richter R, McMacken M, Zabar S, et al. Do internists, pediatricians, and psychiatrists feel competent in obesity care. Using a needs assessment to drive curriculum design? J Gen Intern Med. 2008;23:1066–70. doi: 10.1007/s11606-008-0519-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Forman-Hoffman V, Little A, Wahls T. Barriers to obesity management: A pilot study of primary care clinicians. BMC Fam Pract. 2006;7:35. doi: 10.1186/1471-2296-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goff SL, Holmboe ES, Curry L. Barriers to obesity training for pediatric residents: A qualitative exploration of residency director perspectives. Teach Learn Med. 2006;18:348–55. doi: 10.1207/s15328015tlm1804_13. [DOI] [PubMed] [Google Scholar]
- 32.Puhl R, Brownell KD. Bias, discrimination, and obesity. Attitudes of medical professionals toward obese individuals. Obes Res. 2001;9:788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 33.Ogden J, Bandara I, Cohen H, Farmer D, Hardie J, Minas H, et al. General practitioners’ and patients’ models of obesity: Whose problem is it? Patient Educ Couns. 2001;44:227–33. doi: 10.1016/s0738-3991(00)00192-0. [DOI] [PubMed] [Google Scholar]
- 34.Al-Ghawi A, Ricardo U. Study of the knowledge, attitudes and practices of physicians toward obesity management in primary health care in Bahrain. Public Health Nutr. 2009;12:1791–8. doi: 10.1017/S1368980008004564. [DOI] [PubMed] [Google Scholar]
- 35.Holt N, Schetzina KE, Dalton WT, 3rd, Tudiver F, Fulton-Robinson H, Wu T. Primary care practice addressing child overweight and obesity: A survey of primary care physicians at four clinics in southern Appalachia. South Med J. 2011;104:14–9. doi: 10.1097/SMJ.0b013e3181fc968a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.North American Association for the Study of Obesity (NAASO) and the National Heart Lung and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51–209S. [PubMed] [Google Scholar]
- 37.Bleich SN, Pickett-Blakely O, Cooper LA. Physician practice patterns of obesity diagnosis and weight-related counseling. Patient Educ Couns. 2011;82:123–9. doi: 10.1016/j.pec.2010.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Galuska DA, Will JC, Serdula MK. Are health care professionals advising obese patients to lose weight? JAMA. 1999;282:1576–8. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- 39.Potter MB, Vu JD, Croughan-Minihane M. Weight management: What patients want from their primary care physicians. J Fam Pract. 2001;50:513–8. [PubMed] [Google Scholar]
- 40.Bleich SN, Bennett WL, Gudzune KA, Lisa A, Cooper LA. Impact of physician BMI on obesity care and beliefs. Obesity. 2012;20:999–1005. doi: 10.1038/oby.2011.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Foster GD, Wadden TA, Makris AP, Davidson D, Sanderson RS, Allison DB, et al. Primary care physicians’ attitudes about obesity and its treatment. Obes Res. 2003;11:1168–77. doi: 10.1038/oby.2003.161. [DOI] [PubMed] [Google Scholar]
- 42.Brotons C, Ciurana R, Piñeiro R, Kloppe P, Godycki-Cwirko M, Sammut MR. Dietary advice in clinical practice: The views of general practitioners in Europe. Am J Clin Nutr. 2003;77(Suppl 4):1048–51S. doi: 10.1093/ajcn/77.4.1048S. [DOI] [PubMed] [Google Scholar]
- 43.Mauro M, Taylor V, Wharton S, Sharma AM. Barriers to obesity treatment. Eur J Intern Med. 2008;19:173–80. doi: 10.1016/j.ejim.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 44.Almajwal A, William P, Batterman M. Current dietetic practices of obesity management in Saudi Arabia and comparison with Australian practices and best practice criteria. J Nutr Diet. 2009;66:94–100. [Google Scholar]
- 45.Bocquier A, Verger P, Basdevant A, Andreotti G, Baretge J, Villani P, et al. Overweight and obesity: Knowledge, attitudes, and practices of general practitioners in France. Obes Res. 2005;13:787–95. doi: 10.1038/oby.2005.89. [DOI] [PubMed] [Google Scholar]
- 46.Truswell AS. Family physicians and patients: Is effective nutrition interaction possible? Am J Clin Nutr. 2000;71:6–12. doi: 10.1093/ajcn/71.1.6. [DOI] [PubMed] [Google Scholar]


