Abstract
We report for the first time a case of bacteremia caused by Comamonas kerstersii in a 65-year-old patient with sign of diverticulosis. In addition, we review the isolation of Comamonas sp. and related organisms in our hospital over 25 years.
CASE REPORT
Comamonas kerstersii is a nonfermenting betaproteobacterium described in 2003 that has long been considered nonpathogenic (1). This organism has recently been associated with intraabdominal infection due to perforation of the digestive tract (2). Here we describe a case of polymicrobial bacteremia due to C. kerstersii and Bacteroides fragilis in a 65-year-old diabetic man who was admitted to the emergency department of a hospital because of the sudden onset of fever and chills. The patient reported episodes of vomiting and diarrhea and mentioned that he had drunk water from a small river. Stool cultures performed after the beginning of antibiotic treatment did not disclose Salmonella, Shigella, Aeromonas, Campylobacter species, or C. kerstersii. The detection of Clostridium difficile toxins A and B and glutamate dehydrogenase antigen with the commercial C. difficile detection kit from Techlab was also negative. Blood samples (two pairs of culture bottles) were drawn from a peripheral vein, and the patient was discharged under treatment with oral ciprofloxacin for gastroenteritis of unknown origin. The blood cultures were processed by a Bactec FX automated blood culture system (Becton, Dickinson, Sparks, MD). A first aerobic blood culture bottle became positive 16 h 8 min after sampling, and Gram staining revealed the presence of long, filamentous, Gram-negative bacilli (Fig. 1). Bacterial identification by matrix-assisted laser desorption ionization–time of flight (MALDI-TOF) mass spectrometry (Bruker Daltonics GmbH, Leipzig, Germany) was performed on the same day by using a protocol that we recently developed on the basis of the analyses of a bacterial pellet preparation from the blood culture bottles (3–5). The strain was identified as C. kerstersii, a Gram-negative nonfermenting bacterium, and prompted the hospitalization of the patient. The patient was afebrile at that time, but palpation of the left lower abdominal quadrant was painful. An abdominal computed tomography (CT) scan revealed diverticulosis without evidence of diverticulitis. The anaerobic blood culture bottles from the same pair of samples became positive for Bacteroides fragilis 24 h 2 min after sample collection. We determined the following MICs (mg/liter) for the C. kerstersii strain by the Etest method (bioMérieux, Lyon, France): ceftazidime, 0.75; meropenem, 0.004; imipenem, 0.06; minocycline, 0.38; levofloxacin, 4; co-trimoxazole, >32; ciprofloxacin, 32. For the B. fragilis strain, the MICs were as follows: amoxicillin-clavulanate, 1.5; piperacillin-tazobactam, 6; imipenem, 0.12; meropenem, 0.025; metronidazole, 0.25; clindamycin, 16; ciprofloxacin, 32. The patient was treated with imipenem-cilastatin for 10 days and recovered. The final diagnosis was mixed bacteremia with C. kerstersii and B. fragilis in a setting of diverticulosis.
FIG 1.
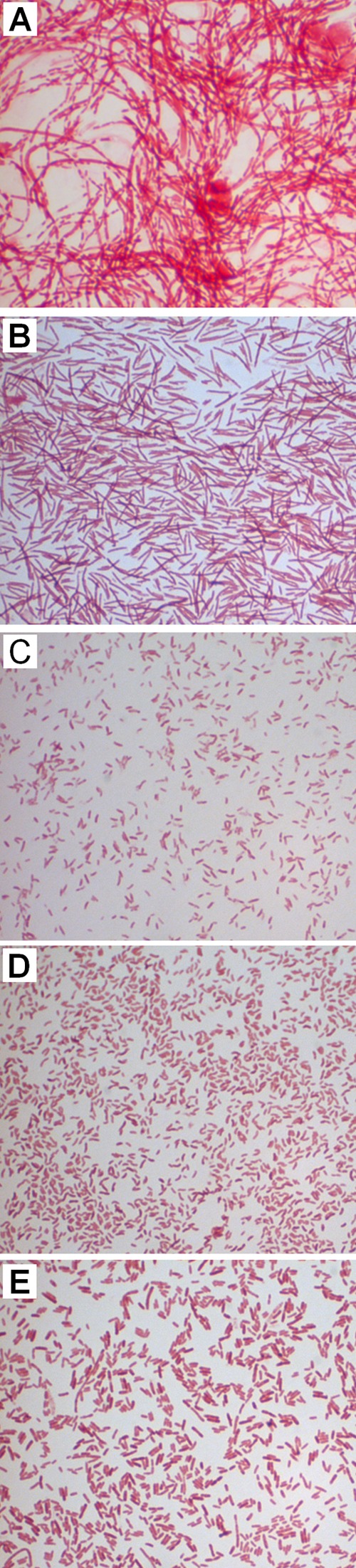
Gram staining of C. kerstersii, C. testosteroni, and D. acidovorans strains isolated in clinical samples from Lausanne University Hospital. The C. kerstersii strain in the present case report was obtained directly from a blood culture bottle (A) and after culture on blood agar medium (B). The strain displays long filaments, unlike the other strains, which appear as Gram-negative short bacilli or rods. (C) A C. kerstersii strain identified in an intraperitoneal infection of an 11-year-old child with a perforated appendix. (D) C. testosteroni involved in bacteremia in a 33-year-old man. (E) D. acidovorans identified in blood cultures from a 61-year-old man.
Comamonads are Gram-negative, nonfermenting, oxidase- and catalase-positive bacteria that are motile largely because of the presence of polar flagella. The genus Comamonas originally contained Comamonas terrigena, Comamonas testosteroni (previously Pseudomonas testosteroni), and Comamonas acidovorans (previously Pseudomonas acidovorans) (6). It now contains 17 species, while C. acidovorans has been separated from the genus on the basis of its 16S rRNA gene and is now known as Delftia acidovorans (7). In 2003, Shigematsu and colleagues described a new species, Delftia tsuruhatensis, that is known to be able to cause bacteremia (8–10). Biochemical analysis often misclassifies these two Delftia species. Since D. tsuruhatensis is absent from our MALDI-TOF database, we cannot exclude the possibility of misclassification. For this reason, D. acidovorans refers to D. acidovorans sensu lato, which includes D. tsuruhatensis. Although they are ubiquitously distributed in the environment (soil and water), Comamonas and Delftia species are rarely associated with infections in humans. However, several publications have incriminated C. testosteroni and D. acidovorans in particular in human diseases, including severe invasive infections such as bacteremia and meningitis (7, 11–17).
C. kerstersii, which was described in 2003 (1), has recently been reported as an agent of intraabdominal infection by Almuzara and colleagues (2). The present case is the first report of C. kerstersii bacteremia. We initially identified the strain at the species level directly from a positive blood culture bottle by MALDI-TOF (3–5). The MALDI-TOF spectral score for C. kerstersii was 2.176 according to the manufacturer's scoring system. Since no other species reached a score above 2.0, this identification was considered valid at the species level (18). Subsequently, it was recovered both from a blood agar plate (with a spectral score of 2.26), on which its growth was maximal, and from a “chocolate” agar plate supplemented with NAD (factor V) and hemin (factor X). The reliability of MALDI-TOF for discrimination between Comamonas species is shown by the fact that Comamonas aquatica, the closest species also present in the MALDI-TOF database, gave a score of 1.542. The database that was used contains five Comamonas species (C. kerstersii, C. testosteroni, C. aquatica, C. terrigena, and C. nitrativorans) and five strains of D. acidovorans. The recently identified species D. tsuruhatensis is absent from this database (9), and we cannot exclude the possibility that some of the D. acidovorans bacteria identified in our laboratory by MALDI-TOF were D. tsuruhatensis. In the absence of MALDI-TOF, numerous biochemical tests (at least 11) are necessary to discriminate Comamonas species (1, 2); such identification requires isolation on an agar plate and cannot be performed on the same day of positivity directly by blood culture. Because of the excellent identification obtained with MALDI-TOF, we rather proceeded to 16S rRNA gene sequencing. Using primers described in references 19 and 20, we obtained a 780-bp partial 16S rRNA gene sequence. A BLAST search for this sequence on the NCBI website revealed 99% identity (754/755 nucleotides with no gaps) with the C. kerstersii sequence (accession number AJ430348.1) submitted by Wauters and colleagues (1). The divergence corresponds to a polymorphism reported by the authors at position 298 (1). This method is limited by the low number of C. kerstersii 16S rRNA sequences. Nevertheless, the first sequence identified as C. aquatica (accession number FJ493173) displays 98% identity (749/763 with two gaps). From both the blood culture bottle and the agar plate, the strain appeared as an extremely long Gram-negative filamentous bacillus, which is a very unusual phenotype for bacteria of this genus (Fig. 1). The Comamonas and Delftia strains previously isolated in our hospital are Gram-negative short bacilli or rods (Fig. 1), which is the morphology described for these organisms (1, 7).
Translocation from the digestive tract seems to be a predominant cause of infections by Delftia and Comamonas species. Recently, Hagiya and colleagues reported a D. acidovorans bacteremia in a 46-year-old woman caused by translocation of the bacteria after pesticide poisoning (15). Bacteremia caused by C. testosteroni was previously reported in a 22-year-old man with a perforated appendix (21). In the four cases reported by Almuzara and colleagues, the C. kerstersii strains were isolated from intraabdominal infections (2). We previously identified another C. kerstersii strain in an intraperitoneal infection of an 11-year-old child with a perforated appendix (Table 1 and Fig. 1). Herein, the digestive origin of the C. kerstersii strain is supported by the facts that (i) the patient reported abdominal pain, vomiting, and diarrhea; (ii) a CT scan revealed evidence of diverticulosis; and (iii) the enteric bacterium B. fragilis was isolated from a blood culture. B. fragilis is a gut commensal of humans that can cause severe diseases such as bacteremia and abscesses due to the production of several virulence factors such as capsule, endotoxins, and enterotoxins (22). C. kerstersii infection could originate from the water that the patient drank in the countryside.
TABLE 1.
Comamonas sp. and D. acidovorans isolates from clinical samples in the Lausanne University Hospital from 1997 to 2013
| Organism or parameter | No. of patients (no. of samples) |
Total no. of patients (samples) | % of patients | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Respiratory and ENTa | Urogenitalb | Intraabdominalc | Skin | Blood culture | Surgical wound | Otherd | |||
| D. acidovorans | 19 (20) | 12 (13) | 5 | 1 (13) | 1 (4) | 38 (55) | 54.3 | ||
| C. testosteroni | 2 (4) | 3 | 8 | 1 (4) | 1 | 4 (5) | 1 | 20 (26) | 28.57 |
| C. kerstersii | 1 | 1 | 2 | 2.86 | |||||
| C. aquatica | 1 (4) | 1 (4) | 1.43 | ||||||
| Comamonas sp.e | 2 (2) | 6 (8) | 1 (1) | 9 (14) | 12.86 | ||||
| Total no. | 23 (26) | 16 (17) | 15 (8) | 7 (5) | 3 (13) | 4 (5) | 2 (4) | 70 (99) | 100 |
| Total % | 32.86 (25.74) | 22.86 (21.78) | 21.43 (16.83) | 10 (9.9) | 4.29 (14.85) | 5.71 (4.95) | 2.85 (5.94) | 100 | |
ENT, ear, nose, and throat.
Urine, vaginal swab, and placenta.
Ascitic fluid, peritoneal fluid, penrose liquid, Kehr drain.
Stool sample (n = 1), bone fragment (n = 1), orifice smear (n = 1).
No identification at the species level.
Comamonas species have rarely been associated with infection in humans despite their ubiquitous distribution in the environment, possibly because of the difficulty in accurately distinguishing Comamonas species from Pseudomonas species in the pre-MALDI-TOF era (2). Alternatively, comamonads could have been underrecognized because of their common occurrence in a setting of a polymicrobial infection. In our 1,027-bed tertiary-care university hospital, 32 Comamonas sp. strains and 38 D. acidovorans strains where isolated from 1997 to 2013. They were isolated primarily from respiratory tract samples (33%), urogenital tract samples (23%), and digestive tract samples (21%); bacteremia represented 5% (three patients) of the cases (Table 1). The three bacteremias produced distinct clinical features but were all polymicrobial (Table 2). The first bacteremia case was due to C. testosteroni in association with Streptococcus parasanguis and Ralstonia pickettii in a 33-year-old man. A second case involved D. acidovorans in association with Streptococcus agalactiae in blood cultures from a 61-year-old man. The last case is the present C. kerstersii and B. fragilis coinfection.
TABLE 2.
Summary of clinical and microbiological bacteremia due to C. testosteroni, C. kerstersii, and D. acidovorans and of a case of intraabdominal collection of C. kerstersii
| Age (yr), sex | Site of infection | Clinical presentation | Underlying disease(s) | Predisposing factors | Pathogens | Treatment |
|---|---|---|---|---|---|---|
| 61, male | Blood | Fever | Lymphoma | Chemotherapy, agranulocytosis | D. acidovorans, S. agalactiae | Cefepime followed by imipenem and ciprofloxacin |
| 33, male | Blood | High fever, hypotension, infected phlebitis on the arm due to cocaine injection | Chronic hepatitis C, chronic alcoholism, drug addiction | None | C. testosteroni, S. parasanguis, R. pickettii | Cefepime and vancomycin followed by moxifloxacin |
| 65, malea | Blood | Fever, chills, vomiting, diarrhea | Diabetic | None | C. kerstersii, B. fragilis | Ciprofloxacin, imipenem |
| 12, male | Peritoneal fluid | Abdominal pain | None | Appendicitis | C. kerstersii, Escherichia coli, Streptococcus sp. (group anginosus/milleri) | Co-amoxicillin, metronidazole, and amikacin followed by co-amoxicillin alone |
Present case.
Like D. acidovorans, C. testosteroni is the Comamonas species associated predominantly with bacteremia (Table 1) (7, 14, 15, 17, 21). Translocation from the digestive tract and catheters is the predominant source of infection (15, 17, 21, 23). Immunocompromised children or patients with compromised immune systems such as patients with AIDS or patients with cancer or treated with aplastic chemotherapies appear to be particularly at risk of developing Comamonas sp. or D. acidovorans bacteremia (16, 23). Interestingly, Khan and colleagues reported a fatal outcome in an 4-year-old immunocompetent child with D. acidovorans bacteremia (16). The patient presented here did not display any sign of immunodeficiency, suggesting that such bacteremia may also occur in the absence of immunosuppression. The likely high inoculum concentration in the water that was drunk and the diabetic status of the patient are two significant cofactors that may explain the occurrence of bacteremia in a setting of a gastrointestinal infection. Similarly, Comamonas species bacteremia has been associated with exposure to possibly contaminated water in a fish tank (24).
C. kerstersii has long been considered nonpathogenic on the basis of a lack of association with severe infections. This could be explained in part by the recent description of this species and the difficulties in accurately identifying it. This first report of polymicrobial bacteremia involving C. kerstersii reveals that this organism can be involved in severe diseases. C. kerstersii pathogenicity could be due to the versatility of this organism, which enables it to grow under various conditions. This report highlights the usefulness of MALDI-TOF for the rapid and accurate identification of nonfermenting Gram-negative bacteria that were difficult to identify in the pre-MALDI-TOF era. This could help to redefine the epidemiology and clinical syndromes due to these organisms.
ACKNOWLEDGMENTS
We are grateful to all of the technicians of the Diagnostic Microbiology Laboratory of the University Hospital of Lausanne for their technical contribution. In particular, we thank Maria Senra-Ortiz and Christian Durussel.
Footnotes
Published ahead of print 26 December 2013
REFERENCES
- 1.Wauters G, De Baere T, Willems A, Falsen E, Vaneechoutte M. 2003. Description of Comamonas aquatica comb. nov. and Comamonas kerstersii sp. nov. for two subgroups of Comamonas terrigena and emended description of Comamonas terrigena. Int. J. Syst. Evol. Microbiol. 53:859–862. 10.1099/ijs.0.02450-0 [DOI] [PubMed] [Google Scholar]
- 2.Almuzara MN, Cittadini R, Vera Ocampo C, Bakai R, Traglia G, Ramirez MS, del Castillo M, Vay CA. 2013. Intra-abdominal infections due to Comamonas kerstersii. J. Clin. Microbiol. 51:1998–2000. 10.1128/JCM.00659-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Croxatto A, Prod'hom G, Greub G. 2012. Applications of MALDI-TOF mass spectrometry in clinical diagnostic microbiology. FEMS Microbiol. Rev. 36:380–407. 10.1111/j.1574-6976.2011.00298.x [DOI] [PubMed] [Google Scholar]
- 4.Prod'hom G, Bizzini A, Durussel C, Bille J, Greub G. 2010. Matrix-assisted laser desorption ionization-time of flight mass spectrometry for direct bacterial identification from positive blood culture pellets. J. Clin. Microbiol. 48:1481–1483. 10.1128/JCM.01780-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prod'hom G, Durussel C, Greub G. 2013. A simple blood-culture bacterial pellet preparation for faster accurate direct bacterial identification and antibiotic susceptibility testing with the VITEK 2 system. J. Med. Microbiol. 62:773–777. 10.1099/jmm.0.049361-0 [DOI] [PubMed] [Google Scholar]
- 6.De Vos P, Kersters K, Falsen E, Pot B, Gillis M, Segers P, De Ley J. 1985. Comamonas Davis and Park 1962 gen. nov., nom. rev. emend., and Comamonas terrigena Hugh 1962 sp. nov. Int. J. Syst. Bacteriol. 35:443–453. 10.1099/00207713-35-4-443 [DOI] [Google Scholar]
- 7.Wen A, Fegan M, Hayward C, Chakraborty S, Sly LI. 1999. Phylogenetic relationships among members of the Comamonadaceae and description of Delftia acidovorans (den Dooren de Jong 1926 and Tamaoka et al. 1987 gen. nov., comb. nov. Int. J. Syst. Bacteriol. 49(Pt 2):567–576. 10.1099/00207713-49-2-567 [DOI] [PubMed] [Google Scholar]
- 8.Preiswerk B, Ullrich S, Speich R, Bloemberg GV, Hombach M. 2011. Human infection with Delftia tsuruhatensis isolated from a central venous catheter. J. Med. Microbiol. 60:246–248. 10.1099/jmm.0.021238-0 [DOI] [PubMed] [Google Scholar]
- 9.Shigematsu T, Yumihara K, Ueda Y, Numaguchi M, Morimura S, Kida K. 2003. Delftia tsuruhatensis sp. nov., a terephthalate-assimilating bacterium isolated from activated sludge. Int. J. Syst. Evol. Microbiol. 53:1479–1483. 10.1099/ijs.0.02285-0 [DOI] [PubMed] [Google Scholar]
- 10.Tabak O, Mete B, Aydin S, Mandel NM, Otlu B, Ozaras R, Tabak F. 2013. Port-related Delftia tsuruhatensis bacteremia in a patient with breast cancer. New Microbiol. 36:199–201 http://www.newmicrobiologica.org/PUB/allegati_pdf/2013/2/199.pdf [PubMed] [Google Scholar]
- 11.Arda B, Aydemir S, Yamazhan T, Hassan A, Tunger A, Serter D. 2003. Comamonas testosteroni meningitis in a patient with recurrent cholesteatoma. APMIS 111:474–476. 10.1034/j.1600-0463.2003.1110404.x [DOI] [PubMed] [Google Scholar]
- 12.Chotikanatis K, Backer M, Rosas-Garcia G, Hammerschlag MR. 2011. Recurrent intravascular-catheter-related bacteremia caused by Delftia acidovorans in a hemodialysis patient. J. Clin. Microbiol. 49:3418–3421. 10.1128/JCM.00625-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cooper GR, Staples ED, Iczkowski KA, Clancy CJ. 2005. Comamonas (Pseudomonas) testosteroni endocarditis. Cardiovasc. Pathol. 14:145–149. 10.1016/j.carpath.2005.01.008 [DOI] [PubMed] [Google Scholar]
- 14.Ender PT, Dooley DP, Moore RH. 1996. Vascular catheter-related Comamonas acidovorans bacteremia managed with preservation of the catheter. Pediatr. Infect. Dis. J. 15:918–920. 10.1097/00006454-199610000-00021 [DOI] [PubMed] [Google Scholar]
- 15.Hagiya H, Murase T, Sugiyama J, Kuroe Y, Nojima H, Naito H, Hagioka S, Morimoto N. 2013. Delftia acidovorans bacteremia caused by bacterial translocation after organophosphorus poisoning in an immunocompetent adult patient. J. Infect. Chemother. 19:338–341. 10.1007/s10156-012-0472-x [DOI] [PubMed] [Google Scholar]
- 16.Khan S, Sistla S, Dhodapkar R, Parija SC. 2012. Fatal Delftia acidovorans infection in an immunocompetent patient with empyema. Asian Pac. J. Trop. Biomed. 2:923–924. 10.1016/S2221-1691(12)60254-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nseir W, Khateeb J, Awawdeh M, Ghali M. 2011. Catheter-related bacteremia caused by Comamonas testosteroni in a hemodialysis patient. Hemodial. Int. 15:293–296. 10.1111/j.1542-4758.2010.00524.x [DOI] [PubMed] [Google Scholar]
- 18.Bizzini A, Durussel C, Bille J, Greub G, Prod'hom G. 2010. Performance of matrix-assisted laser desorption ionization-time of flight mass spectrometry for identification of bacterial strains routinely isolated in a clinical microbiology laboratory. J. Clin. Microbiol. 48:1549–1554. 10.1128/JCM.01794-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zucol F, Ammann RA, Berger C, Aebi C, Altwegg M, Niggli FK, Nadal D. 2006. Real-time quantitative broad-range PCR assay for detection of the 16S rRNA gene followed by sequencing for species identification. J. Clin. Microbiol. 44:2750–2759. 10.1128/JCM.00112-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goldenberger D, Schmidheini T, Altwegg M. 1997. Detection of Bartonella henselae and Bartonella quintana by a simple and rapid procedure using broad-range PCR amplification and direct single-strand sequencing of part of the 16S rRNA gene. Clin. Microbiol. Infect. 3:240–245. 10.1111/j.1469-0691.1997.tb00604.x [DOI] [PubMed] [Google Scholar]
- 21.Gul M, Ciragil P, Bulbuloglu E, Aral M, Alkis S, Ezberci F. 2007. Comamonas testosteroni bacteremia in a patient with perforated acute appendicitis. Short communication. Acta Microbiol. Immunol. Hung. 54:317–321. 10.1556/AMicr.54.2007.3.6 [DOI] [PubMed] [Google Scholar]
- 22.Wexler HM. 2007. Bacteroides: the good, the bad, and the nitty-gritty. Clin. Microbiol. Rev. 20:593–621. 10.1128/CMR.00008-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Le Moal G, Paccalin M, Breux JP, Roblot F, Roblot P, Becq-Giraudon B. 2001. Central venous catheter-related infection due to Comamonas testosteroni in a woman with breast cancer. Scand. J. Infect. Dis. 33:627–628. 10.1080/00365540110026827 [DOI] [PubMed] [Google Scholar]
- 24.Smith MD, Gradon JD. 2003. Bacteremia due to Comamonas species possibly associated with exposure to tropical fish. South. Med. J. 96:815–817. 10.1097/01.SMJ.0000051869.86765.D9 [DOI] [PubMed] [Google Scholar]


