ABSTRACT
Varicella-zoster virus (VZV) is responsible for both varicella (chickenpox) and herpes zoster (shingles). During varicella, the virus establishes latency within the sensory ganglia and can reactivate to cause herpes zoster, but the immune responses that occur in ganglia during herpes zoster have not previously been defined. We examined ganglia obtained from individuals who, at the time of death, had active herpes zoster. Ganglia innervating the site of the cutaneous herpes zoster rash showed evidence of necrosis, secondary to vasculitis, or localized hemorrhage. Despite this, there was limited evidence of VZV antigen expression, although a large inflammatory infiltrate was observed. Characterization of the infiltrating T cells showed a large number of infiltrating CD4+ T cells and cytolytic CD8+ T cells. Many of the infiltrating T cells were closely associated with neurons within the reactivated ganglia, yet there was little evidence of T cell-induced neuronal apoptosis. Notably, an upregulation in the expression of major histocompatibility complex class I (MHC-I) and MHC-II molecules was observed on satellite glial cells, implying these cells play an active role in directing the immune response during herpes zoster. This is the first detailed characterization of the interaction between T cells and neuronal cells within ganglia obtained from patients suffering herpes zoster at the time of death and provides evidence that CD4+ and cytolytic CD8+ T cell responses play an important role in controlling VZV replication in ganglia during active herpes zoster.
IMPORTANCE VZV is responsible for both varicella (chickenpox) and herpes zoster (shingles). During varicella, the virus establishes a life-long dormant infection within the sensory ganglia and can reawaken to cause herpes zoster, but the immune responses that occur in ganglia during herpes zoster have not previously been defined. We examined ganglia obtained from individuals who, at the time of death, had active herpes zoster. We found that specific T cell subsets are likely to play an important role in controlling VZV replication in ganglia during active herpes zoster.
INTRODUCTION
Varicella zoster virus (VZV) is a ubiquitous human pathogen responsible for both varicella (chickenpox) and herpes zoster (shingles). Herpes zoster results from reactivation of the virus in sensory ganglia, generally in the setting of reduced VZV-specific cell-mediated immunity (1, 2). Herpes zoster may be followed by postherpetic neuralgia (PHN), which is generally defined as pain persisting for greater than 90 days following the resolution of the herpes zoster rash (3). This pain can persist for years and can have a negative impact on patients' quality of life (4). The cause of the pain is unknown; however, it has been suggested that damage to neuronal cells plays a role (5). We have previously demonstrated that VZV-infected neurons are resistant to apoptosis (6) due to the expression of the immediate-early gene (IE) product of open reading frame 63 (ORF63) (7). Thus, rather than being a consequence of VZV-induced neuronal cell apoptosis, it is possible that immune cell-mediated injury to neurons and/or their protective satellite glial cells (SGCs) is responsible for the pain associated with herpes zoster and particularly PHN.
Sensory neurons are completely enveloped by SGCs, which provide protection and nutritional support, and they may even play a role in neuronal signaling (8, 9). In most cases, each adult neuron and its surrounding SGCs form discrete individual units; however, the number of SGCs decreases with age (9). SGCs also form an important barrier around peripheral neurons in place of a vascular barrier (9) and share many properties of antigen-presenting cells (10). Thus, SGCs are likely to play an important role in the immune response to viral infections in sensory ganglia.
The immune response has been shown to play an important role in the ganglia during infection with herpes simplex virus (HSV), an alphaherpesvirus closely related to VZV. HSV-1 latency in sensory ganglia is characterized by a persistent CD8+ T cell infiltrate (11–13), and it has been shown that the cytolytic protein granzyme B cleaves the immediate-early HSV protein, ICP4 (homolog of VZV IE62), and that this plays an important role in preventing or limiting viral reactivation (14). Furthermore, it has been demonstrated that during latency the HSV latency-associated transcript (LAT) can prevent granzyme B from cleaving caspase-3 and prevent activation of this apoptotic pathway, ensuring both neuronal and HSV survival (15).
There has been no LAT equivalent described for VZV; however, mRNA transcripts from a number of ORFs, including ORF21, ORF29, ORF62, ORF63, and ORF66, have been identified by DNA sequencing in latently infected ganglia (16–18). Previous studies examining VZV latently infected ganglia have also reported the detection of a number of VZV proteins by immunohistochemistry (11, 12, 17, 19–21), although examination of ganglia with latent VZV did not find an association between the expression of IE62 during latency and an inflammatory infiltrate, which was in contrast to HSV latency (11–13). It is important to note, however, that VZV protein expression during latency has only been demonstrated by immunohistochemistry (IHC) (3, 22), and that the expressed proteins have been detected within the cytoplasm of neurons, despite many of them typically displaying a nuclear localization within productively infected cells (22). Recently, concerns over the specificity of viral antigen immunostaining in adult human neurons have been raised. These include the presence of the neuronal pigments neuromelanin and lipofuscin and the presence of contaminating antibodies in rabbit and rat serum as well as in certain ascites-derived monoclonal antibody preparations that cross-react with blood group A antigens, expressed in a subset of neurons in patients with blood type A (23, 24). Thus, it is possible that few, if any, neurons contain VZV proteins during true latency, and any VZV proteins detected may be the result of viral reactivation or an abortive infection.
Our previous study of ganglia obtained 1 to 5 months after contracting herpes zoster demonstrated that a robust immune cell infiltrate is still present following the disappearance of the rash and is comprised largely of noncytolytic (granzyme B-negative) T cells and macrophages (25). However, to date there have been no detailed studies of ganglia obtained while the herpes zoster rash is still present; therefore, the constituents of the immune response in the ganglia during active reactivation are unknown. This study examines ganglia from 2 patients who died with a herpes zoster rash and demonstrates that CD4+ and cytolytic CD8+ T cells may play an important role in the ganglia during active herpes zoster.
MATERIALS AND METHODS
Human tissue samples.
Consecutive 5-μm paraffin-embedded sections of trigeminal and dorsal root ganglia fixed in 20% buffered formalin were obtained from the Department of Forensic Medicine, Glebe, NSW, Australia, by following appropriate ethics approval from University of Sydney, Sydney Local Health District, and the coroner. Control sections of paraffin-embedded human tonsil fixed in 10% buffered formalin were obtained from Westmead Hospital in accordance with ethical approval from the University of Sydney and Western Sydney Area Heath Service.
DNA extraction and PCR.
DNA extraction was performed using the Qiagen DNA minikit with the formalin-fixed, paraffin-embedded protocol (Qiagen, VIC, Australia) per the manufacturer's instructions. PCR was performed using GoTaq (Promega, Australia) for glyceraldehyde-3-phosphate dehydrogenase (GAPDH) to confirm successful isolation of cellular DNA, and then PCR was performed for VZV ORF9a and HSV UL42.
Immunohistochemical staining.
Standard immunohistochemical (IHC) staining was performed as previously described (25), with the exception that an additional step was incorporated using a biotin blocking system per the manufacturer's instructions (Dako, Australia) and Azure B (1% in water) was substituted for hematoxylin as a counterstain when staining for VZV antigens to reduce the confounding effect of neuromelanin and lipofuscin on specific antigen staining (24). For antibody information, see Table 1.
TABLE 1.
Antibodies used for immunohistochemistry and immunofluorescence staining
| Antibody | Type | Clonea | Dilution | Source |
|---|---|---|---|---|
| Anti-VZV IE63 | Rabbit polyclonal | NA | 1:1,000 | A gift from Ravi Mahalingam, University of Colorado, Denver, CO, USA |
| Anti-VZV gE | Mouse IgG2b | 1:100 | Millipore International | |
| Anti-VZV gE:gI | Mouse IgG2b | SG1 | 1:1,000 | Meridian Life Science, Saco, ME, USA |
| Anti-CD3 | Mouse | PS1 | 1:10 | Novocastra, Australia |
| Anti-CD4 | Polyclonal Goat | NA | 1:10 | R&D Systems, MN, USA |
| Anti-CD8 | Rabbit IgG polyclonal | NA | 1:200 | Abcam, Cambridge, UK |
| Anti-granzyme B | Mouse IgG2a | GZB01 | 1:10 | Abcam, Cambridge, UK |
| Anti-S100B | Rabbit polyclonal | NA | Predilute | Dako, Australia |
| Anti-S100B | Goat polyclonal | NA | 1:50 | R&D Systems, MN USA |
| Neural cell adhesion molecule (NCAM) | Mouse IgG1 | 123C3 | 1:10 | Cell Signaling Technologies, Boston, MA, USA |
| Cleaved caspase 3 (Asp175) | Rabbit polyclonal | NA | 1:100 | Cell Signaling Technologies, Boston, MA, USA |
| Anti-HLA-DR | Mouse | LN-3 | 1:50 | Novocastra, Australia |
| Anti-HLA-DR | Rabbit IgG1 | EPR3692 | 1:100 | Abcam, Cambridge, UK |
| Anti-β2-microglobulin | Rabbit polyclonal | NA | 1:200 | Novocastra, Melbourne, Australia |
NA, not applicable.
Immunofluorescence staining.
Single and dual immunofluorescence staining was performed as previously described (25). Sudan Black B (Sigma-Aldrich, Sydney, Australia) was used to quench autofluorescence when necessary (25).
Imaging and cell counts.
Imaging was performed using a Zeiss Axioplan 2 upright microscope with a Zeiss Axiocam HRm digital monochrome charge-coupled-device (CCD) camera (Carl Zeiss, Australia) or a Zeiss LSM 510 Meta spectral confocal microscope (Carl Zeiss, Australia). For cell counting, nonoverlapping fields were captured at ×20 magnification (or 63× for granzyme B). As the sections of reactivated ganglia on each slide were relatively large, the counts for each reactivated ganglia were done by taking greater than 20 images from each stain, manually counting the positive cells, and then averaging between the 2 stains that were performed for each immune cell marker. While this approach enabled the proportion of CD4 and CD8 cells to be determined, it is possible that some sections which were stained for CD3 contained more or fewer T cells than the sections which were stained for CD8 and CD4. Manual cell counting was performed using the Axiovision image acquisition software. Counts from 2 independent staining experiments were then averaged.
RESULTS
Histological analyses of human ganglia during herpes zoster.
A major obstacle to studying the interactions between VZV, neurons, and the immune response during herpes zoster is the difficulty in obtaining naturally infected human ganglia. We obtained multiple ganglia at postmortem from 2 patients who died with incidental herpes zoster. Control ganglia were obtained from individuals without evidence of VZV-related disease (Table 2).
TABLE 2.
Patient ganglion samples used in this study
| Parameter | Value(s) for case no.a: |
|||
|---|---|---|---|---|
| C1 | C2 | HZ1 | HZ2 | |
| Age (yr) | 73 | 9 | 93 | 63 |
| Gender | Female | Male | Male | Male |
| Cause of death and underlying conditions | Metastatic adenocarcinoma | Blunt-force head injury | Aspiration pneumonia, dementia | Acute myeloid leukemia |
| Notes on herpes zoster | NA | NA | Rash at L2 dermatome, 17 days prior to death, rash still present at autopsy | Herpes zoster in ophthalmic region and some dissemination to trunk, starting 3 weeks prior to death, still present at autopsy |
| Ganglia examined | 1 DRG | 2 DRG | LL2 DRG (reactivated, ganglionitis) | RTG (reactivated, ganglionitis) |
| LL1 DRG | 1 RC DRG | |||
| RL DRG | 1 LC DRG | |||
| LT DRG | RT DRG | |||
| RC DRG | RL DRG | |||
| 2 LL DRG | ||||
| Blood group | Non-A | Non-A | Non-A | A |
| PCR for VZV DNA | ND | ND | LL2-Pos | RTG-Pos |
| LL1-ND | RC-ND | |||
| RL-Pos | LC-ND | |||
| LT- Pos | RT-ND | |||
| LC-Pos | RL-ND | |||
| LL1-ND | ||||
| LL2-ND | ||||
Abbreviations: DRG, dorsal root ganglia; TG, trigeminal ganglia; IHC, immunohistochemistry; LL, left lumbar; RL, right lumbar; RT, right thoracic; LT, left thoracic; RC, right cervical; LC, left cervical; RTG, right trigeminal ganglia; NA, not applicable; ND, not detected; Pos, positive.
Patient 1 (HZ1) was a 93-year-old man with frontotemporal dementia who developed herpes zoster approximately 17 days before death from aspiration pneumonia. At autopsy a hemorrhagic vesicular and ulcerated rash was confined to the left L2 dermatome. The L2 dorsal root ganglion (DRG) was removed (reactivated ganglia, LL2). In addition, single left lumbar (LL1), right lumbar (RL), left thoracic (LT), and right cervical (RC) DRGs from uninvolved dermatomes were available for study.
The second patient (HZ2) was a 62-year-old man with acute myeloid leukemia (diagnosed postmortem) who developed herpes zoster ophthalmicus approximately 3 weeks prior to death. At autopsy, in addition to the rash confined to the ophthalmic division of the right trigeminal nerve, there was evidence of dissemination with isolated thoracic lesions. The right (reactivated RTG) trigeminal ganglia, as well as one right cervical (RC), one left cervical (LC1), one right thoracic (RT), one right lumbar (RL), and 2 left lumbar (LL1 and LL2) DRGs, were used in this study.
Ganglia from patients without evidence of VZV-related disease in the months preceding death or evidence of immunosuppression were also available for study. A total of three control ganglia from 2 different patients were obtained. Control patient 1 (C1) was a 73-year-old female who died from metastatic adenocarcinoma. Control patient 2 (C2) was a 9-year-old male who died due to a blunt-force head injury.
DNA extraction was performed on all ganglia, and PCR for VZV ORF9a was performed. The results are summarized in Table 2. All ganglia used within this study were negative for HSV DNA as determined by PCR (data not shown).
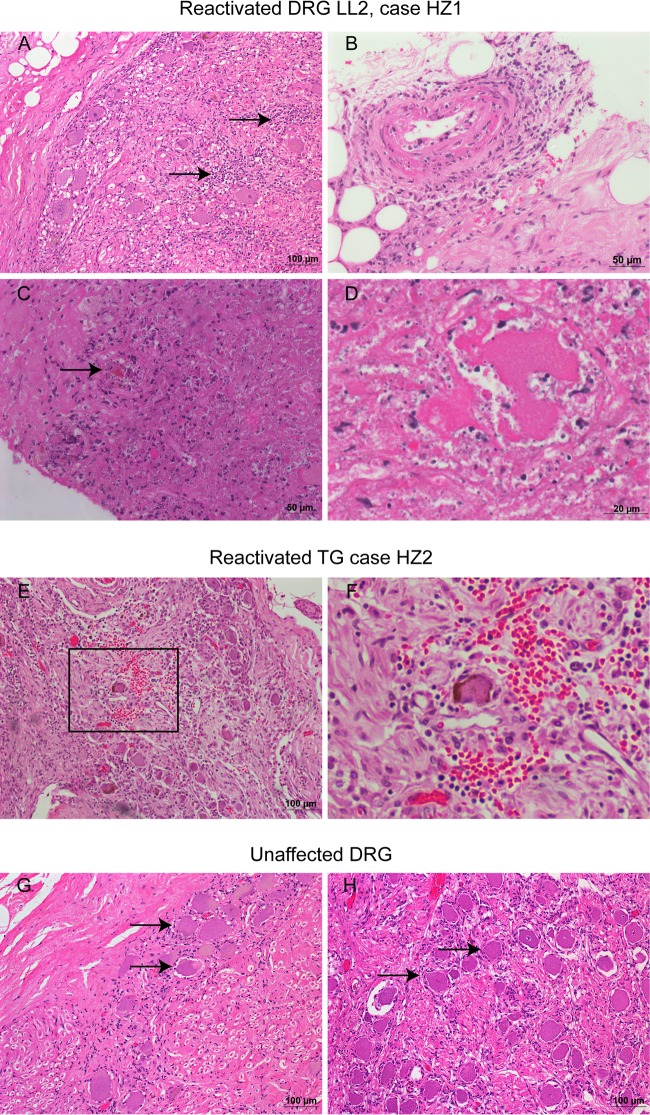
Hematoxylin and eosin staining was performed on multiple 5-μm sections from each ganglion. In the reactivated ganglion from HZ1 (LL2), a prominent, widespread infiltrate of inflammatory cells, predominantly small lymphocytes and macrophages, was evident (Fig. 1A). Focally there was perivascular and intramural inflammatory cells, with mural fibrinoid necrosis, and an adjacent area of necrosis occupying approximately 20% of the ganglion (Fig. 1B to D). Within this region there was a general loss of the typical ganglion architecture, with neuronal cell degeneration and disarray of SGCs (Fig. 1C and D). Neurons and SGCs are intact in the rest of the ganglion, although there is some perivascular lymphocytic cuffing without vasculitis. In the remaining 4 unaffected DRG from HZ1 (LL1, RL, LT, and RC) there were intact neurons and SGCs, and apart from a sparse immune cell infiltrate in the other lumbar and thoracic ganglia (data not shown), the ganglia were unremarkable without appreciable neuronal loss. The cervical DRG (RC) appeared similar to control patient ganglia (Fig. 1G to H).
FIG 1.
Histology of human ganglia during herpes zoster. Representative images of hematoxylin and eosin-stained sections from HZ1 (A to D) showing patchy inflammation (A, arrows), vasculitis (B), and an infarction with loss of defined neuron-SGC units within the area (C, arrow, and D); HZ2 (E and F) showing a localized hemorrhage (E and F, inset); and unaffected ganglia from HZ1 (RC; G) and control patient 2 (H) showing intact neurons (arrows).
In HZ2, there was a significant infiltrate of inflammatory cells, including small lymphocytes in the RTG (reactivated ganglionitis) as well as the right cervical DRG (RC1). In one region of the RTG there was a localized hemorrhage (Fig. 1E and F). In all 7 ganglia examined from this patient, neurons and SGCs appeared to be intact. There was no inflammation in the three control ganglia, and the neurons and SGCs were intact (Fig. 1H).
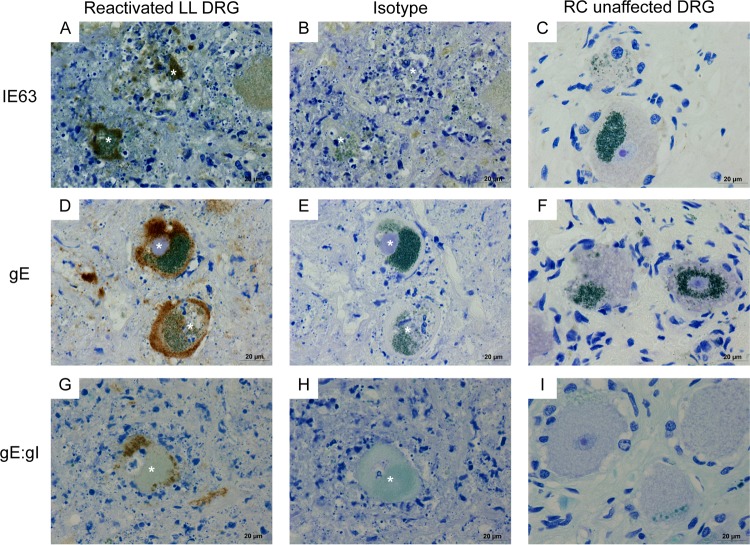
Detection of VZV antigens in human ganglia during herpes zoster.
To determine whether VZV antigen, indicative of viral replication, was present in ganglia innervating or distal to the site of the herpes zoster rash, we performed immunohistochemical staining for the VZV immediate-early protein IE63 using a rabbit polyclonal antibody (19), the late viral gene product glycoprotein E (gE; Millipore, Billerica, MA, USA), and the precursor and mature forms of gE and the gI complex (gE:gI; Meridian Life Sciences, Saco, ME).
In the reactivated ganglion from patient HZ1 (LL2), intense cytoplasmic staining for VZV IE63 (Fig. 2A) was observed in neuron-SGC units within the area of necrosis. However, precise neuronal or SGC localization was not possible due to the degenerated state of the neurons and SGCs within this region (Fig. 2A). Antibody specificity was confirmed by staining consecutive sections with the appropriate nonimmune isotype antibody (Fig. 2B). In addition, IE63 staining was identified within axons in the necrotic area (data not shown). No IE63 staining was observed in the nonreactivated ganglia from HZ1 or in the control ganglia (Fig. 2C and data not shown).
FIG 2.
Immunohistochemical detection of VZV antigens in ganglia from patients experiencing herpes zoster. Representative images from HZ1-reactivated lumbar DRG (LL2; A, D, and G) and an unaffected cervical DRG (C, F, and I) stained with VZV IE63, gE, and gE:gI antibodies. Consecutive LL2 sections were incubated with isotype control antibodies (B, E, and H). Corresponding neurons are labeled with an asterisk. Antibodies were visualized using DAB (brown) and sections were counterstained with Azure B, which stains nuclei and lipofuscin blue and neuromelanin green.
Membranous and cytoplasmic gE staining in neuron-SGC units was identified in the reactivated DRG from HZ1 (LL2). As with IE63 staining, positive neuron-SGC units were restricted to the area of necrosis (Fig. 2D). Isotype antibody staining of consecutive sections confirmed the specificity of the gE staining (Fig. 2E). Staining of nonreactivated ganglia from HZ1 or ganglia from the control cases did not yield any detectable gE staining (Fig. 2F and data not shown). In addition, a small number of gE-positive infiltrating cells were observed scattered throughout this ganglion (data not shown). Staining with the gE:gI antibody confirmed the presence of VZV glycoprotein-positive cells within the region of necrosis in the reactivated ganglion (LL2) from HZ1 (Fig. 2G). This antibody also stained membrane and cytoplasmic regions within neuron-SGC units. Staining was not observed when consecutive sections were incubated with isotype antibody (Fig. 2H) or when nonreactivated ganglia from HZ1 or ganglia from the control cases were stained for gE:gI (Fig. 2I and data not shown).
No IE63-positive cells were identified in any of the 7 ganglia, including the reactivated RTG from the second patient with herpes zoster (HZ2). Staining for gE:gI was not observed in any ganglia from HZ2, with the exception of a few small infiltrating cells which were gE:gI positive within the reactivated RTG (data not shown). The gE antibody could not be used to assess ganglia from HZ2. This is because, unlike HZ1 and all of the control cases, HZ2 was blood group A, as determined by staining of ganglionic sections from all cases with an anti-blood group A antibody (Table 2), and it has been reported that this gE antibody (which is produced from ascites fluid) can induce a mouse ascites Golgi (MAG) reaction typified by punctate cytoplasmic/trans-Golgi network localized staining within neurons in ganglia from blood group A individuals (23). It was concluded that VZV antigens were readily detectable in the reactivated ganglion LL2 from HZ1 but only rarely detectable in the reactivated ganglion RTG from HZ2.
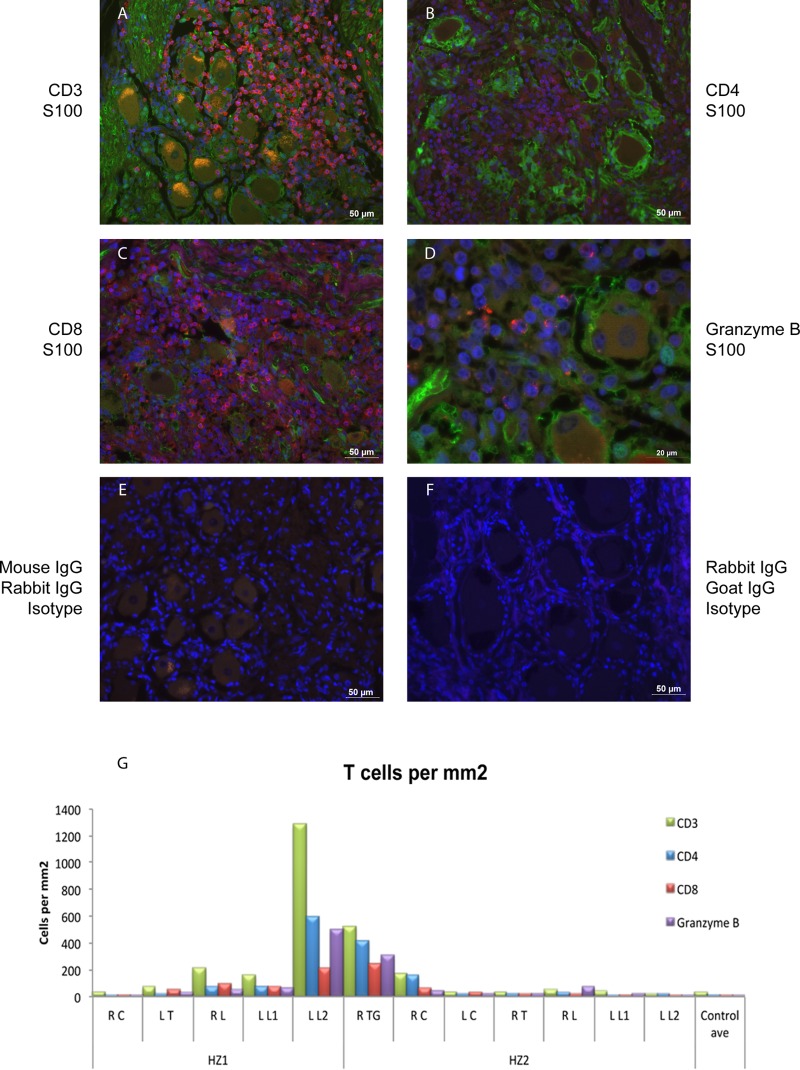
Characterization of the T cell infiltrate in human ganglia during herpes zoster.
To characterize the T cell infiltrate within ganglia during herpes zoster, serial sections were immunofluorescently stained for the T cell markers CD3, CD4, and CD8, as well as granzyme B, to identify cytotoxic T cells and NK cells. Sections were costained with S100B to identify SGCs. Sections of control DRGs (negative control) and tonsil (positive control) were stained in parallel, and antibody specificity was confirmed by staining with the appropriate nonimmune isotype antibody (Fig. 3E and F and data not shown).
FIG 3.
Characterization of T cell subsets in ganglia during herpes zoster. (A to D) Immunofluorescent staining was performed with CD3, CD4, CD8, granzyme B, and S100B. Bound antibodies were visualized using species-specific Alexa Fluor antibodies, and immune cell markers are shown in red and S100B in green. Representative images are shown for HZ2. (E and F) No specific staining was seen using isotype control antibodies. Sections were counterstained with DAPI (blue). Scale bars are indicated. (G) The number of positive cells per mm2 was determined from 2 independent stains and averaged (with the exception of HZ1 RL granzyme B counts, for which only 1 stain could be counted due to a lack of sample material).
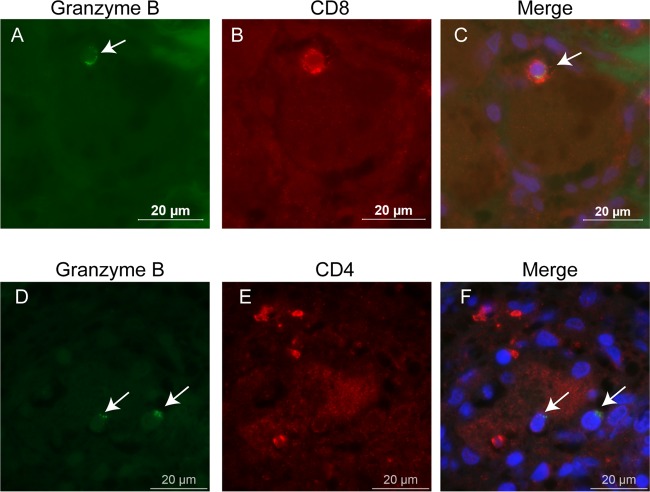
In the reactivated ganglia of HZ1 and HZ2 (LL2 and RTG, respectively), a widespread infiltrate of CD3+ T cells was apparent (Fig. 3A). Infiltrating T cells consisted of both CD4+ and CD8+ subsets (Fig. 3B and C). There were also numerous infiltrating cells that stained positive for the cytolytic marker granzyme B (Fig. 3D). The numbers of cells expressing CD3, CD4, CD8, or granzyme B were determined by counting multiple sections and averaging the results from 2 independent stains (Fig. 3G). The density of CD3+ T cells averaged across whole ganglia was highest in the reactivated ganglia, ranging from 525 cells per mm2 (RTG) to >1,200 cells per mm2 in LL2. Compared to control ganglia, CD3+ T cell densities were also slightly elevated in several ganglia in proximity to LL2 (i.e., LL1, RL, and LT) and RTG (i.e., RC) but not in more distant ganglia. Both CD4+ and CD8+ T cells were well represented in both reactivated ganglia, although there was a trend toward CD4+ T cell predominance, which was most evident in LL2. There was also an abundance of granzyme B-positive cells in the reactivated ganglia (501 per mm2 [LL2] and 307 per mm2 [RTG]). Compared to control DRGs, granzyme B-positive cells were also increased in ganglia in proximity to LL2 (LL1, RL, and LT) and RTG (RC) but not in more distant ganglia. To further characterize the granzyme B-positive cells, dual staining for granzyme B and CD8 or CD4 was performed on sections from reactivated ganglia. Many CD8+/granzyme B-positive cells were identified (Fig. 4A to C), whereas there were no CD4+/granzyme B-positive cells identified (Fig. 4D to F). The number of granzyme B-positive cells within both reactivated ganglia exceeded the number of CD8-positive T cells (Fig. 3G), and given that CD4 T cells were shown to be noncytolytic (Fig. 4D to F), this difference may be attributed to infiltrating cytolytic natural killer (NK) cells. Staining for CD16, which is present on NK cells, showed that a significant number of these cells were present within reactivated ganglia (data not shown).
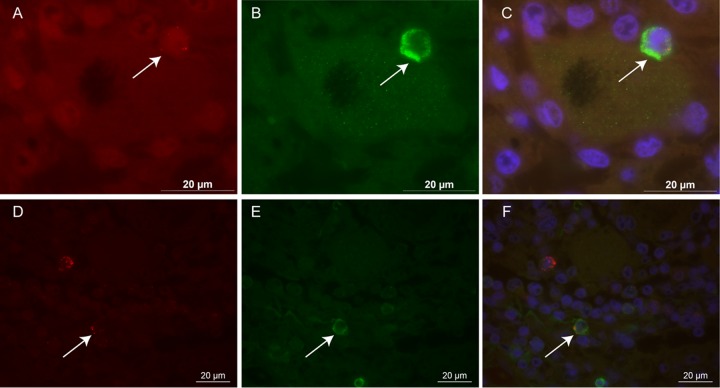
FIG 4.
Cytolytic CD8+ but not CD4+ T cells are identified in reactivated ganglia. Representative images of reactivated ganglia from HZ1 LL1 stained for granzyme B (green; A and D), CD8 (red; B), and CD4 (red; E). Merged images are shown in panels C and F. Bound antibodies were visualized with species-specific Alexa Fluor antibodies and counterstained with DAPI (blue). Arrows show granzyme B-positive cells.
These data indicate that during VZV reactivation there is extensive infiltration of CD4+ and CD8+ cytotoxic T cells into the affected ganglia. Infiltrating cells also appeared in neighboring ganglia, such as LL1 and RL (HZ1) and RC (HZ2), at numbers that were greater than what was seen in ganglia further from the site of reactivation and in control ganglia (Fig. 3G).
Proximity of T cells to neurons in ganglia during herpes zoster.
Further examination of the localization of T cells within reactivated ganglia revealed that many T cells were in close proximity to neuron-SGC units. Counts were performed on sections stained with antibodies to CD3+, CD8+, or CD4+ T cells as well as S100B (marker of SGCs) to determine the proportion of neurons with T cells in very close proximity. In reactivated ganglia from HZ1 and HZ2, 23% and 12% of neuron-SGC units, respectively, had one or more CD3+ T cells in very close proximity. In contrast, in unaffected ganglia from these patients, only 2 to 4% of neuron-SGC units had CD3+ T cells in close proximity. A breakdown of the T cell subsets involved in this association revealed that despite there being a greater number of CD4+ than CD8+ T cells in both reactivated ganglia, CD8+ T cells appeared more likely to be associated with neuron-SGC units, as 9.9% (73/740) of neurons had a CD8+ T cell in close proximity, whereas 4.3% (28/651) of neurons had a CD4+ T cell in close proximity in HZ2 RTG.
Confocal microscopy was used to examine the relationship between neurons and T cells in closer detail. In some neuron-SGC units there was a focal absence of S100B staining, and, as a result, SGC cytoplasm, separating the CD3+ T cells from the neuron (Fig. 5A to C). This suggests that the protective SGC layer was breached, which could allow interactions between neurons and T cells to occur in reactivated ganglia during herpes zoster.
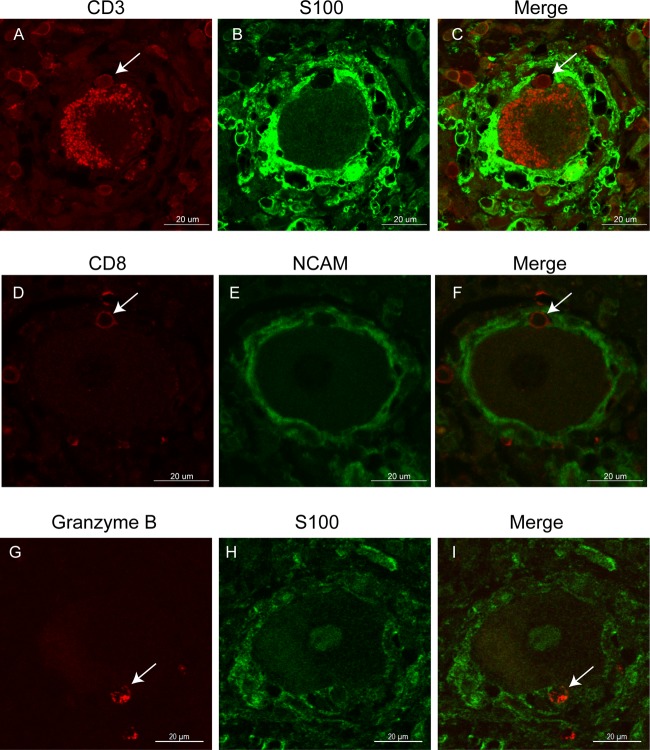
FIG 5.
T cells interact with neuron-satellite glial cell units. Representative images of sections stained for CD3 (red; A), S100 (green; B), a merge for HZ1 LL2 (C), CD8 (red; D), NCAM (green; E), a merge for HZ2 RTG (F), granzyme B (red; G), S100B (green; H), and a merge for HZ1 LL2 (I). Potential neuron-interacting cells are labeled with an arrow. Autofluorescence is visible within the neuron due to the presence of lipofuscin (A and C). Bound antibodies were detected with species-specific Alexa Fluor antibodies. Nonspecific lipofuscin staining can be seen in the neuron (A and C).
This observation was confirmed with dual immunofluorescence staining for NCAM (expressed on the surface of the neurons and satellite cells) and CD8. In both reactivated ganglia, for some neuron-SCG units the NCAM membrane was discontinuous and gaps could be observed when an infiltrating CD8+ cell appeared adjacent to a neuron (Fig. 5D to F). These data suggest that there is potential for direct interaction between neurons and CD8+ T cells in reactivated ganglia during herpes zoster. Furthermore, staining for granzyme B and S100B also showed that cells with cytolytic potential could be found in close proximity to some neurons (Fig. 5G to I).
Cleaved caspase-3 detection in ganglia during herpes zoster.
In order to determine if the infiltrating cytotoxic CD8+ T cells contribute to increased neuron apoptosis, in herpes zoster, dual immunofluorescent staining for cleaved caspase-3 and granzyme B was performed. Interestingly, within all ganglia, including both reactivated ganglia, the majority of neurons and satellite glial cells did not stain for cleaved caspase-3. However, some of the nonneuronal cells, particularly those in close proximity to neurons, were dual positive for cleaved caspase-3 and granzyme B (Fig. 6). Counting of 30 nonoverlapping images taken (representing 0.486 mm2) from a single stain from the reactivated ganglia from HZ2 showed 11 small cells which were positive for cleaved caspase-3, 7 of which (64%) were also granzyme B positive (Fig. 6). Thus, the cleavage of caspase-3 does not appear to be a feature in neurons in affected ganglia during VZV reactivation, despite the abundance of cells expressing cytolytic markers.
FIG 6.
Infiltrating cells rather than neurons undergo apoptosis. Representative images are shown from HZ2 RTG of small infiltrating cells (arrow) positive for granzyme B (red; A and D) and cleaved caspase-3 (green; B and E). (C and F) Merged images. Bound antibodies were detected with species-specific Alexa Fluor-conjugated antibodies and counterstained with DAPI (blue).
MHC-I and -II are upregulated in human ganglia during herpes zoster.
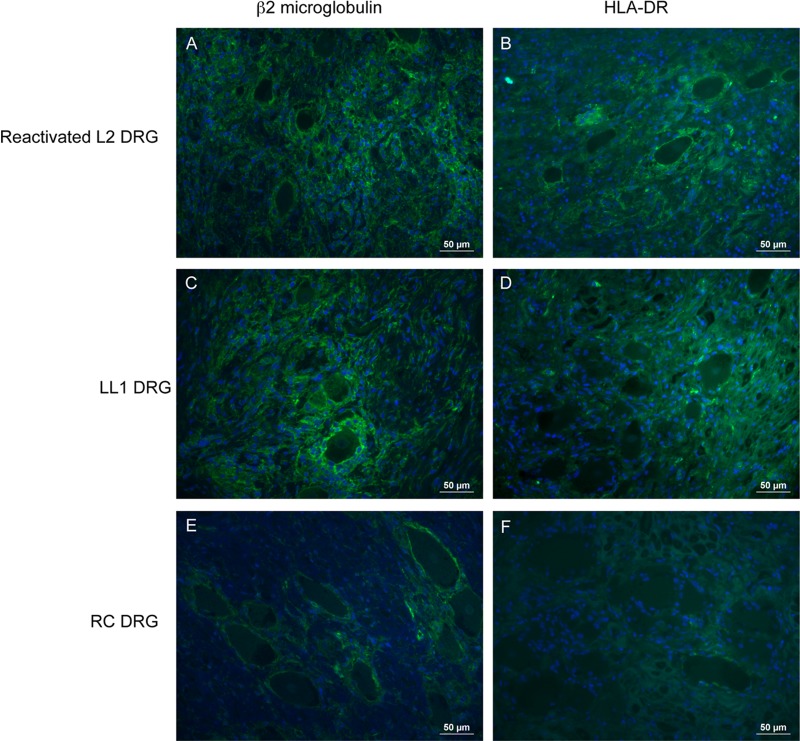
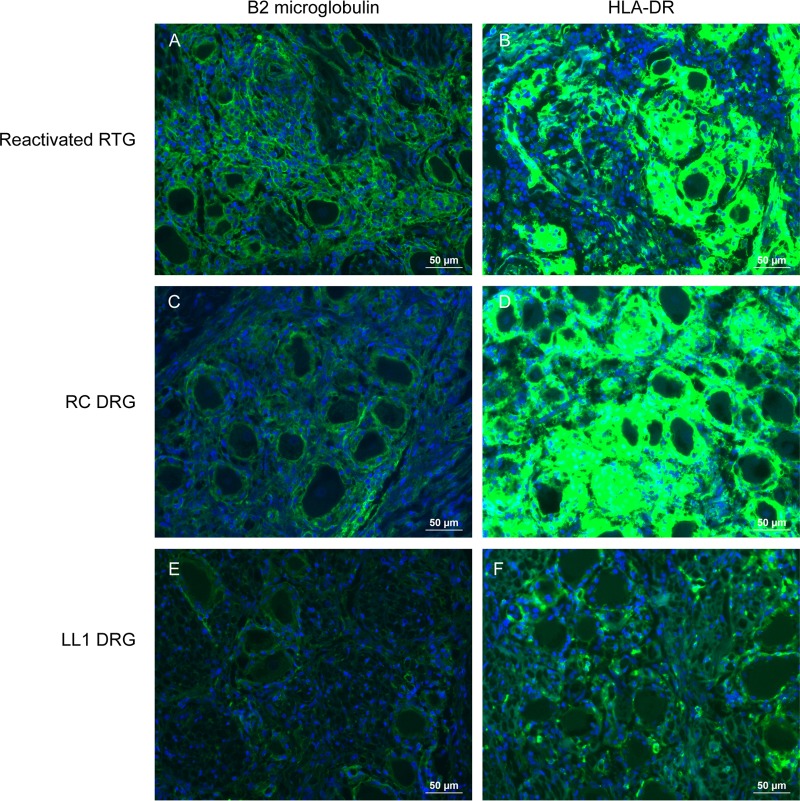
Sensory neurons typically lack expression of major histocompatibility complex (MHC) molecules; however, expression is upregulated following HSV-1 infection of mouse sensory neurons (26), which may facilitate neuron-T cell interactions. In order to determine if MHC molecules are expressed in ganglia during active VZV reactivation, immunofluorescent staining was performed on all ganglia for β2-microglobulin (β2m) and the human leukocyte DR (HLA-DR) antigen as markers of MHC class I (MHC-I) and MHC-II, respectively. No neuronal β2m or HLA-DR expression was detected in ganglia from both HZ1 and HZ2 or in control ganglia. However, β2m expression was observed on all other cell types within the ganglia, and HLA-DR was expressed on SGCs as well as on some infiltrating inflammatory cells. Compared to control ganglia, there was marked upregulation of β2m and HLA-DR expression on SGCs in both reactivated ganglia (RTG and LL2) (Fig. 7 and 8). In HZ1, herpes zoster was confined to a single dermatome without clinical evidence of dissemination, which suggests that ganglia in proximity to the site of reactivation also undergo some degree of immune activation despite the lack of demonstrable viral antigens.
FIG 7.
Upregulation of MHC-I and -II in human ganglia during herpes zoster. Representative images stained for β2 microglobulin (A, C, and E) and HLA-DR (B, D, and F) in the reactivated LL2 ganglion, a neighboring lumbar ganglion (LL1), and a cervical ganglion (RC) from HZ1. Bound antibodies were visualized with Alexa Fluor antibodies (green), and sections were counterstained with DAPI (blue). Corresponding images were taken with identical exposure times.
FIG 8.
Upregulation of MHC-I and -II in human ganglia during herpes zoster. Representative images were stained for β2 microglobulin (A, C, and E) and HLA-DR (B, D, and F) in the reactivated RTG ganglion, a neighboring cervical ganglia (RC), and a lumbar ganglion (LL1) from HZ2. Bound antibodies were visualized with Alexa Fluor antibodies (green), and sections were counterstained with DAPI (blue). Corresponding images were taken with identical exposure times.
DISCUSSION
VZV reactivation (herpes zoster) is associated with pain and postherpetic neuralgia with severe pain, persisting for months to years following the resolution of the herpes zoster rash. Neither the cellular mechanisms involved in viral reactivation from latency nor the cause of postherpetic neuralgia is known. The strict species specificity of VZV, coupled with the difficulty of obtaining ganglia from patients with herpes zoster or fresh human ganglia for experimental infection, have contributed to the paucity of information about these key aspects of VZV infection. Previously, we reported the first detailed characterization of the immune response in naturally infected ganglia from 3 patients who died 1 to 5 months after contracting herpes zoster (25). However, no detailed studies of ganglia obtained during acute herpes zoster while the rash was still present have been reported; consequently, the constituents of the immune response in these ganglia have not been defined. In this study, we analyzed multiple ganglia from 2 patients (HZ1 and HZ2) with active herpes zoster at the time of death. While direct quantitative comparisons between the current study using ganglia during active herpes zoster and our previous study using ganglia after recovery from herpes zoster (25) are complicated by the different approaches used to stain and enumerate different cell types, there were several apparent differences of note. During active herpes zoster, there was a large infiltrate of cytotoxic T cells, and the predominant infiltrating cells were CD4+ T cells and, to a lesser degree, CD8+ T cells, whereas following resolution of the rash (i.e., 1 to 5 months after contracting herpes zoster) the predominant infiltrating cells are CD8+ T cells, yet the majority lack cytotoxic markers (25). Further, the current study demonstrates that despite an abundance of cytotoxic CD8+ T cells, some of which were in close proximity to neurons and may have breached the SGC barrier, cleaved caspase 3 was not identified, indicating that neurons and SGCs were unlikely to be undergoing apoptosis. The strong upregulation of MHC class I and II molecules on SGCs suggests that these cells play an important role in directing the immune response during herpes zoster.
Previous histological studies of ganglia from patients with herpes zoster close to the time of death noted necrosis in part or the whole of the ganglia, with some hemorrhage and lymphocytic infiltration (27–32). Some cases also showed vascular involvement with perivascular lymphocytic cuffing and thrombosis noted (28, 31). Similar features were noted in ganglia from the current study, particularly in the reactivated ganglia of HZ1, where focal necrosis was apparent. Given the case history for this patient as well as the histology, the observed necrosis was most likely an infarct caused by vasculitis rather than by vascular occlusion from an embolus or other cause. A localized hemorrhage was also noted in the reactivated ganglia from HZ2, and both reactivated ganglia contained a dense lymphoid infiltrate.
Our finding that VZV antigens were detected only in neuron-SGC units within the area of necrosis in HZ1 and not within the adjacent viable ganglia or in ganglia from HZ2 was unexpected, given that both patients had active herpes zoster with a rash at their time of death, 17 (HZ1) and 21 (HZ2) days after the onset of the rash. It is possible that following a burst of viral replication within the ganglia with transport of new virus particles to the skin resulting in a vesicular rash, VZV replication is rapidly contained within the ganglia, resulting in the loss of viral antigen staining. This is supported by the observation that herpes zoster skin lesions begin to resolve in less than a week (3), implying little reseeding of the skin from the ganglia. Also, antiviral treatment is most effective when administered within 72 h of the onset of the rash (33–36), suggesting that this is when the majority of virus replication occurs. Alternatively, low levels of viral replication may persist but are below the level of detection by immunohistochemistry, or viral replication is ongoing but is not uniform within the ganglia and was not present in the sections of the ganglia we examined. A persistent low level of virus replication may also explain our previous results where a persistent immune infiltrate was evident in ganglia several months after clinical resolution of herpes zoster (25). Ongoing viral replication was also suggested by Schmidbauer et al. (29), who detected viral antigens (gH and nucleoprotein) and VZV DNA in ganglia from 7 patients up to 7 weeks after the onset of the herpes zoster rash. Interestingly, as in our study, they only identified viral antigens in necrotic regions of the ganglia (29). We have previously shown that VZV-infected neurons expressing IE63 are resistant to apoptosis (7). Therefore, the necrosis of neuronal cells may be due to the inflammatory response to viral reactivation, which may also lead to vasculitis with or without an infarction. Alternatively, the viral antigens, which were observed in necrotic cells, may be the result of secondary viral reactivation occurring subsequent to infarction. Studies have shown that a loss of connection between a sensory ganglion and the central nervous system results in HSV reactivation (37–41); thus, it is possible that by disrupting the architecture and function of the ganglion, necrosis triggers viral reactivation.
In the reactivated ganglia in the current study, a dense T cell infiltrate was observed, although there were relatively more CD4+ than CD8+ T cells identified and most of the CD8+ T cells were cytotoxic (granzyme B positive). Given the expression of MHC-II molecules on SGCs and their phagocytic capacity (10), they may play an important role in presenting exogenous VZV antigens to CD4+ T cells (13). However, although cytotoxic CD4+ T cells expressing granzyme B play an important role in controlling herpesvirus infections independent of CD8+ T cells and B cells (reviewed in reference 42) and VZV-specific CD4+ T cells are capable of controlling VZV infection in human retinal pigment epithelial cells (43), we did not identify any CD4+/granzyme B+ cells. The temporal profile of the immune response to VZV reactivation is poorly understood, and it is possible that significant numbers of cytotoxic CD4+ cells are present only for a short period during reactivation. We were able to study ganglia taken 17 (HZ1) and 21 (HZ2) days after the onset of the rash, which may be outside this period. The observed infiltrating CD4+ T cells may still play an important role in controlling VZV replication through the secretion of cytokines or via FAS-FAS ligand interactions. Further characterization of the cytokine and chemokine profile within reactivated ganglia and the expression of immune-inhibitory molecules will form a part of future studies.
With the currently available tools it is not possible to determine what proportion of the infiltrating T cells are VZV antigen specific or whether the majority of the infiltrating cells are not VZV specific but are recruited following secretion of chemokines released in response to VZV infection. Previously we have reported CXCL10 production and the presence of CXCR3-positive cells in both human fetal DRG explants experimentally infected with VZV and in one of the reactivated ganglia used in the present study (LL2) (40). It is likely that other chemokines also play an important role in immune cell recruitment into ganglia following VZV reactivation, and their identification remains to be determined.
A number of neurons within both reactivated ganglia from HZ1 and HZ2 were shown to have at least one T cell within close proximity, which in many cases appeared to have breached the protective SGC layer, as evidenced by focal loss of S100B and NCAM staining. Many of these cells were cytotoxic (granzyme B+) (Fig. 5G to I). Although neuronal expression of MHC-I and -II molecules was not detected, expression may have been below the limit of detection by immunohistochemistry. Similarly, β2m expression was not identified on neurons within ganglia several months after herpes zoster reactivation (25).
It is currently not possible to determine if an immunological synapse between the T cells and neurons is occurring within the ganglia. In vitro studies have shown that neurons are susceptible to T cell-mediated contact-dependent cytotoxicity that does not require MHC-I expression (44). Interestingly, although granzyme B-positive CD8+ cells appeared in close proximity to neurons in the reactivated ganglia, no neuronal staining for cleaved caspase-3 was identified in either the reactivated or unaffected ganglia. A small number of small infiltrating cells, often granzyme B positive, were cleaved caspase-3 positive. The phenotype of these cells remains to be determined. A similar phenotype has also been observed in rabbit TG experimentally infected with another alphaherpesvirus, bovine herpesvirus type 1. Two days after infection, the infiltrating mononuclear cells surrounding many of the neurons were terminal deoxynucleotidyltransferase-mediated dUTP-biotin nick end labeling (TUNEL) positive, although only rare TUNEL-positive neurons were observed (45). While this may reflect the presence of an innate protective mechanism within sensory ganglia to prevent the irreversible loss of neurons, the presence of replicating or latent VZV may protect neurons from T cell-mediated apoptosis.
It is possible that the neurons we observed with T cells in close proximity harbored latent VZV. Unfortunately, degradation of nucleic acids due to the fixation conditions and the age of our samples did not allow us to perform in situ hybridization to detect VZV nucleic acid. Studies of trigeminal ganglia harboring latent HSV-1 have shown that antigen-specific granzyme B+ CD8+ T cells preferentially surround LAT+ neurons (13). It has also been demonstrated that granzyme B cleaves the HSV-1 immediate-early protein ICP4, which may play a role in limiting viral reactivation (14). Similarly, expression of LAT protects neuroblastoma cells from granzyme B-mediated apoptosis (15). Further studies are required to determine if similar protective mechanisms exist for VZV during productive infection and/or latency.
The expression of MHC-I and particularly MHC-II was increased on SGCs within both reactivated and neighboring ganglia. Kennedy et al. (46) examined ganglia from patients with a history of herpes zoster near the time of death and also found intense staining for MHC-II in areas with infiltrating lymphocytes. These findings suggest a role for SGCs in controlling the immune response, and combined with our results demonstrating that T cell counts were higher in ganglia close to the primary site of reactivation, they suggest that the effects of viral reactivation are not limited to a single ganglion. Further studies into the role of SGCs and bystander neurons during VZV reactivation are warranted.
In summary, this study has identified VZV antigen staining using 3 independent antibodies in necrotic neurons during VZV reactivation. This is similar to other studies and shows that this may be a common feature of herpes zoster, which has implications regarding the development of PHN. Further, infiltrating CD4+ and cytotoxic CD8+ T cells were also a hallmark of the host immune response within the ganglia during herpes zoster, and some of these T cells appeared in close proximity with neurons but did not appear to be inducing apoptosis. Upregulation of MHC-I and -II molecules on SGCs suggests that these cells play a role in directing the immune response during viral reactivation. Further studies are required to elucidate the mechanisms that may lead to or prevent neuronal necrosis during herpes zoster and the role of SGCs during viral reactivation.
ACKNOWLEDGMENTS
This work was supported by a National Health and Medical Research Council Project grant awarded to A.A. and B.S.
We thank Jane Radford from the Department of Histology, The University of Sydney, for assistance with cutting and staining sections, Louise Cole from the Bosch Institute, The University of Sydney, for assistance with microscopy, and Ravi Mahalingam (University of Colorado) for supplying the IE63 antibody.
Footnotes
Published ahead of print 18 December 2013
REFERENCES
- 1.Arvin AM, Moffat JF, Redman R. 1996. Varicella-zoster virus: aspects of pathogenesis and host response to natural infection and varicella vaccine. Adv. Virus Res. 46:263–309. 10.1016/S0065-3527(08)60074-3 [DOI] [PubMed] [Google Scholar]
- 2.Burke BL, Steele RW, Beard OW, Wood JS, Cain TD, Marmer DJ. 1982. Immune responses to varicella-zoster in the aged. Arch. Intern. Med. 142:291–293 [PubMed] [Google Scholar]
- 3.Gilden D, Mahalingam R, Nagel MA, Pugazhenthi S, Cohrs RJ. 2011. Review: the neurobiology of varicella zoster virus infection. Neuropathol. Appl. Neurobiol. 37:441–463. 10.1111/j.1365-2990.2011.01167.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oxman MN. 2009. Herpes zoster pathogenesis and cell-mediated immunity and immunosenescence. J. Am. Osteopath. Assoc. 109(Suppl 6):S13–S17 [PubMed] [Google Scholar]
- 5.Watson CP, Deck JH, Morshead C, Van der Kooy D, Evans RJ. 1991. Post-herpetic neuralgia: further post-mortem studies of cases with and without pain. Pain 44:105–117. 10.1016/0304-3959(91)90124-G [DOI] [PubMed] [Google Scholar]
- 6.Hood C, Cunningham AL, Slobedman B, Boadle RA, Abendroth A. 2003. Varicella-zoster virus-infected human sensory neurons are resistant to apoptosis, yet human foreskin fibroblasts are susceptible: evidence for a cell-type-specific apoptotic response. J. Virol. 77:12852–12864. 10.1128/JVI.77.23.12852-12864.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hood C, Cunningham AL, Slobedman B, Arvin AM, Sommer MH, Kinchington PR, Abendroth A. 2006. Varicella-zoster virus ORF63 inhibits apoptosis of primary human neurons. J. Virol. 80:1025–1031. 10.1128/JVI.80.2.1025-1031.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hanani M. 2005. Satellite glial cells in sensory ganglia: from form to function. Brain Res. Brain Res. Rev. 48:457–476. 10.1016/j.brainresrev.2004.09.001 [DOI] [PubMed] [Google Scholar]
- 9.Pannese E. 2010. The structure of the perineuronal sheath of satellite glial cells (SGCs) in sensory ganglia. Neuron Glia Biol. 6:3–10. 10.1017/S1740925X10000037 [DOI] [PubMed] [Google Scholar]
- 10.van Velzen M, Laman JD, Kleinjan A, Poot A, Osterhaus AD, Verjans GM. 2009. Neuron-interacting satellite glial cells in human trigeminal ganglia have an APC phenotype. J. Immunol. 183:2456–2461. 10.4049/jimmunol.0900890 [DOI] [PubMed] [Google Scholar]
- 11.Theil D, Derfuss T, Paripovic I, Herberger S, Meinl E, Schueler O, Strupp M, Arbusow V, Brandt T. 2003. Latent herpesvirus infection in human trigeminal ganglia causes chronic immune response. Am. J. Pathol. 163:2179–2184. 10.1016/S0002-9440(10)63575-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hufner K, Derfuss T, Herberger S, Sunami K, Russell S, Sinicina I, Arbusow V, Strupp M, Brandt T, Theil D. 2006. Latency of alpha-herpes viruses is accompanied by a chronic inflammation in human trigeminal ganglia but not in dorsal root ganglia. J. Neuropathol. Exp. Neurol. 65:1022–1030. 10.1097/01.jnen.0000235852.92963.bf [DOI] [PubMed] [Google Scholar]
- 13.Verjans GM, Hintzen RQ, van Dun JM, Poot A, Milikan JC, Laman JD, Langerak AW, Kinchington PR, Osterhaus AD. 2007. Selective retention of herpes simplex virus-specific T cells in latently infected human trigeminal ganglia. Proc. Natl. Acad. Sci. U. S. A. 104:3496–3501. 10.1073/pnas.0610847104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knickelbein JE, Khanna KM, Yee MB, Baty CJ, Kinchington PR, Hendricks RL. 2008. Noncytotoxic lytic granule-mediated CD8+ T cell inhibition of HSV-1 reactivation from neuronal latency. Science 322:268–271. 10.1126/science.1164164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jiang X, Chentoufi AA, Hsiang C, Carpenter D, Osorio N, Ben Mohamed L, Fraser NW, Jones C, Wechsler SL. 2011. The herpes simplex virus type 1 latency-associated transcript can protect neuron-derived C1300 and Neuro2A cells from granzyme B-induced apoptosis and CD8 T-cell killing. J. Virol. 85:2325–2332. 10.1128/JVI.01791-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohrs RJ, Barbour M, Gilden DH. 1996. Varicella-zoster virus (VZV) transcription during latency in human ganglia: detection of transcripts mapping to genes 21, 29, 62, and 63 in a cDNA library enriched for VZV RNA. J. Virol. 70:2789–2796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohrs RJ, Gilden DH, Kinchington PR, Grinfeld E, Kennedy PG. 2003. Varicella-zoster virus gene 66 transcription and translation in latently infected human ganglia. J. Virol. 77:6660–6665. 10.1128/JVI.77.12.6660-6665.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohrs RJ, Srock K, Barbour MB, Owens G, Mahalingam R, Devlin ME, Wellish M, Gilden DH. 1994. Varicella-zoster virus (VZV) transcription during latency in human ganglia: construction of a cDNA library from latently infected human trigeminal ganglia and detection of a VZV transcript. J. Virol. 68:7900–7908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahalingam R, Wellish M, Cohrs R, Debrus S, Piette J, Rentier B, Gilden DH. 1996. Expression of protein encoded by varicella-zoster virus open reading frame 63 in latently infected human ganglionic neurons. Proc. Natl. Acad. Sci. U. S. A. 93:2122–2124. 10.1073/pnas.93.5.2122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lungu O, Panagiotidis CA, Annunziato PW, Gershon AA, Silverstein SJ. 1998. Aberrant intracellular localization of varicella-zoster virus regulatory proteins during latency. Proc. Natl. Acad. Sci. U. S. A. 95:7080–7085. 10.1073/pnas.95.12.7080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grinfeld E, Kennedy PG. 2004. Translation of varicella-zoster virus genes during human ganglionic latency. Virus Genes 29:317–319. 10.1007/s11262-004-7434-z [DOI] [PubMed] [Google Scholar]
- 22.Azarkh Y, Gilden D, Cohrs RJ. 2010. Molecular characterization of varicella zoster virus in latently infected human ganglia: physical state and abundance of VZV DNA, quantitation of viral transcripts and detection of VZV-specific proteins. Curr. Top. Microbiol. Immunol. 342:229–241. 10.1007/82_2009_2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zerboni L, Sobel RA, Lai M, Triglia R, Steain M, Abendroth A, Arvin A. 2012. Apparent expression of varicella-zoster virus proteins in latency resulting from reactivity of murine and rabbit antibodies with human blood group A determinants in sensory neurons. J. Virol. 86:578–583. 10.1128/JVI.05950-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zerboni L, Sobel RA, Ramachandran V, Rajamani J, Ruyechan W, Abendroth A, Arvin A. 2010. The expression of varicella-zoster virus immediate early regulatory protein IE63 in neurons of latently infected human sensory ganglia. J. Virol. 84:3421–3430. 10.1128/JVI.02416-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gowrishankar K, Steain M, Cunningham AL, Rodriguez M, Blumbergs P, Slobedman B, Abendroth A. 2010. Characterization of the host immune response in human ganglia after herpes zoster. J. Virol. 84:8861–8870. 10.1128/JVI.01020-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pereira RA, Tscharke DC, Simmons A. 1994. Upregulation of class I major histocompatibility complex gene expression in primary sensory neurons, satellite cells, and Schwann cells of mice in response to acute but not latent herpes simplex virus infection in vivo. J. Exp. Med. 180:841–850. 10.1084/jem.180.3.841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Head H, Campbell W. 1900. The pathology of herpes zoster and its bearing on sensory localization. Brain 23:353–523. 10.1093/brain/23.3.353 [DOI] [PubMed] [Google Scholar]
- 28.Denny-Brown D, Adams RD, Fitzgerald P. 1944. Pathological features of herpes zoster. Arch. Neurol. Psychiatry 51:216–231. 10.1001/archneurpsyc.1944.02290270005002 [DOI] [Google Scholar]
- 29.Schmidbauer M, Budka H, Pilz P, Kurata T, Hondo R. 1992. Presence, distribution and spread of productive varicella zoster virus infection in nervous tissues. Brain 115(Part 2):383–398. 10.1093/brain/115.2.383 [DOI] [PubMed] [Google Scholar]
- 30.Esiri MM, Tomlinson AH. 1972. Herpes zoster. Demonstration of virus in trigeminal nerve and ganglion by immunofluorescence and electron microscopy. J. Neurol. Sci. 15:35–48 [DOI] [PubMed] [Google Scholar]
- 31.Nagashima K, Nakazawa M, Endo H. 1975. Pathology of the human spinal ganglia in varicella-zoster virus infection. Acta Neuropathol. 33:105–117. 10.1007/BF00687537 [DOI] [PubMed] [Google Scholar]
- 32.Lungu O, Annunziato PW, Gershon A, Staugaitis SM, Josefson D, LaRussa P, Silverstein SJ. 1995. Reactivated and latent varicella-zoster virus in human dorsal root ganglia. Proc. Natl. Acad. Sci. U. S. A. 92:10980–10984. 10.1073/pnas.92.24.10980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wood MJ, Kay R, Dworkin RH, Soong SJ, Whitley RJ. 1996. Oral acyclovir therapy accelerates pain resolution in patients with herpes zoster: a meta-analysis of placebo-controlled trials. Clin. Infect. Dis. 22:341–347. 10.1093/clinids/22.2.341 [DOI] [PubMed] [Google Scholar]
- 34.Tyring S, Barbarash RA, Nahlik JE, Cunningham A, Marley J, Heng M, Jones T, Rea T, Boon R, Saltzman R. 1995. Famciclovir for the treatment of acute herpes zoster: effects on acute disease and postherpetic neuralgia. A randomized, double-blind, placebo-controlled trial. Collaborative Famciclovir Herpes Zoster Study Group. Ann. Intern. Med. 123:89–96 [DOI] [PubMed] [Google Scholar]
- 35.Tyring SK, Beutner KR, Tucker BA, Anderson WC, Crooks RJ. 2000. Antiviral therapy for herpes zoster: randomized, controlled clinical trial of valacyclovir and famciclovir therapy in immunocompetent patients 50 years and older. Arch. Fam. Med. 9:863–869. 10.1001/archfami.9.9.863 [DOI] [PubMed] [Google Scholar]
- 36.Fashner J, Bell AL. 2011. Herpes zoster and postherpetic neuralgia: prevention and management. Am. Fam. Physician 83:1432–1437 [PubMed] [Google Scholar]
- 37.Ellison SA, Carton CA, Rose HM. 1959. Studies of recurrent herpes simplex infections following section of the trigeminal nerve. J. Infect. Dis. 105:161–167. 10.1093/infdis/105.2.161 [DOI] [PubMed] [Google Scholar]
- 38.Behrman S, Knight G. 1954. Herpes simplex associated with trigeminal neuralgia. Neurology 4:525–530. 10.1212/WNL.4.7.525 [DOI] [PubMed] [Google Scholar]
- 39.Carton CA, Kilbourne ED. 1952. Activation of latent herpes simplex by trigeminal sensory-root section. N. Engl. J. Med. 246:172–176. 10.1056/NEJM195201312460503 [DOI] [PubMed] [Google Scholar]
- 40.Steain M, Gowrishankar K, Rodriguez M, Slobedman B, Abendroth A. 2011. Upregulation of CXCL10 in human dorsal root ganglia during experimental and natural varicella-zoster virus infection. J. Virol. 85:626–631. 10.1128/JVI.01816-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Walz MA, Price RW, Notkins AL. 1974. Latent ganglionic infection with herpes simplex virus types 1 and 2: viral reactivation in vivo after neurectomy. Science 184:1185–1187. 10.1126/science.184.4142.1185 [DOI] [PubMed] [Google Scholar]
- 42.Heller KN, Gurer C, Munz C. 2006. Virus-specific CD4+ T cells: ready for direct attack. J. Exp. Med. 203:805–808. 10.1084/jem.20060215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Milikan JC, Baarsma GS, Kuijpers RW, Osterhaus AD, Verjans GM. 2009. Human ocular-derived virus-specific CD4+ T cells control varicella zoster virus replication in human retinal pigment epithelial cells. Investig. Ophthalmol. Vis. Sci. 50:743–751. 10.1167/iovs.08-2611 [DOI] [PubMed] [Google Scholar]
- 44.Giuliani F, Goodyer CG, Antel JP, Yong VW. 2003. Vulnerability of human neurons to T cell-mediated cytotoxicity. J. Immunol. 171:368–379 [DOI] [PubMed] [Google Scholar]
- 45.Delhon GA, Gonzalez MJ, Murcia PR. 2002. Susceptibility of sensory neurons to apoptosis following infection by bovine herpesvirus type 1. J. Gen. Virol. 83:2257–2267 [DOI] [PubMed] [Google Scholar]
- 46.Kennedy PG, Barrass JD, Graham DI, Clements GB. 1990. Studies on the pathogenesis of neurological diseases associated with varicella-zoster virus. Neuropathol. Appl. Neurobiol. 16:305–316. 10.1111/j.1365-2990.1990.tb01265.x [DOI] [PubMed] [Google Scholar]