Abstract
Background
The use of vasoconstrictor agents has many advantages, but its use has been limited due to a fear of systemic absorption and the induction of adverse effects in cardiac compromised patients. The aim of this study was to review the literature to assess any scientific basis for the limited use of dental anaesthesia with a vasoconstrictor agent in cardiovascular compromised patients.
Material/Methods
A comprehensive database search was executed with the use of Medline (PubMed), ISI Web of Science, and Cochrane. The inclusion criteria were: a clearly defined dose of vasoconstrictor agent and the testing of at least 1 parameter (pressure, heart rate, or saturation) or occurrence of at least 1 cardiac incident (complication).
Results
Among all complications, only 10 could be directly related to the use of local anaesthesia. It is noteworthy that 40% appeared after the administration of anaesthesia without vasoconstrictor agents. No severe adverse clinical effects were noted in the analysed studies.
Conclusions
The most frequent complications in cardiovascular compromised patients after dental local anaesthesia with a vasoconstrictor agent were disclosed in ECG arrhythmias. Most of these disclosed arrhythmias were clinically insignificant. The use of ≤4 ampules of lignocaine with epinephrine 1:100000 as a dental anaesthetic seems to be relatively safe for cardiovascular compromised patients.
MeSH Keywords: Anesthesia, Local, Dentistry, Operative, Vasoconstrictor Agents, Cardiovascular Diseases
Background
Local anaesthesia is a common requirement for the performance of most dental procedures. The market offers many types of anaesthetics, but the greatest difference between them is the addition of vasoconstrictor agents. Some authors state that plain anaesthetics do not provide sufficient anaesthesia [1–3]. Vasoconstrictor agents have many advantages, such as delaying the absorption of local anaesthetics, increasing patient welfare due to the lower doses of anaesthetic required, diminishing potential toxic risk, and providing bleeding control [4]. Despite these benefits, its use has been limited due to fear of systemic absorption and the induction of adverse effects in cardiac compromised patients; it has sometimes been controversial [5]. However pain, stress, and fear are also responsible for the systemic liberation of endogenous catecholamines that can cause an autonomic response, such as provoking acute arrhythmias [6]. It should be noted that epinephrine released endogenously is a higher dose than that used in dental anaesthesia [7–9].
According to American Heart Association (AHA) and American Dental Association (ADA) guidelines, there is no contraindication to using a vasoconstrictor agent when administrated carefully and with preliminary aspiration [10]. The maximum dose of epinephrine in local anaesthesia for a healthy subject is 0.2 mg, though this can be lowered to 0.04 mg if patient has severe cardiovascular disease (ASA III and IV) [11]. Therefore, the aim of this study was to review the literature to assess any scientific basis for the limited use of dental anaesthesia with a vasoconstrictor agent in cardiovascular compromised patients.
Material and Methods
On June 13th, 2013, a comprehensive database search was executed with the use of Medline (PubMed), ISI Web of Science, and Cochrane. No language frame was used. Only publications from the last 15 years were considered.
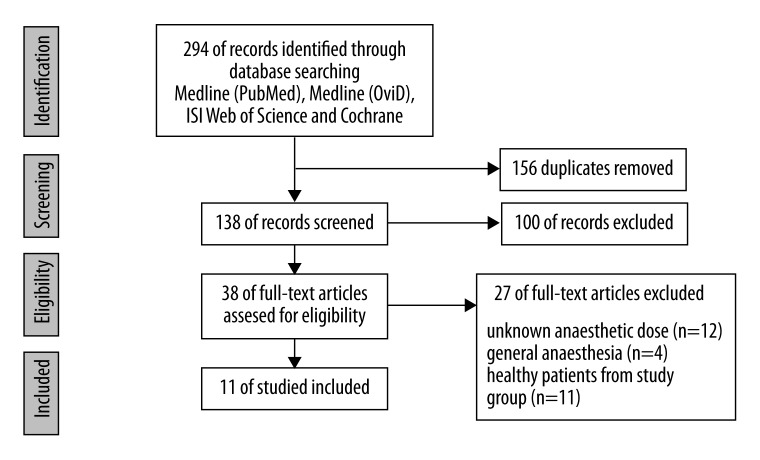
Search equations are presented in Table 1. To correctly translate the equation for other databases, the help of a senior librarian was obtained. The titles and abstracts that were found with an electronic search were screened and evaluated by 2 observers according to inclusion and exclusion criteria (Table 2). Studies that did not meet the defined criteria were excluded from further evaluation. Any discrepancies in the selection were settled through discussion. A prisma flow diagram illustrates the search and evaluation process (Figure 1).
Table 1.
Search equations.
| “Anesthesia, Dental [MeSH Terms] AND Cardiovascular Diseases [MeSH Terms]” – Clinical Trials |
| “Anesthesia, Dental [MeSH Terms] AND Hypertension [MeSH Terms]” |
| “Anesthesia, Dental [MeSH Terms] AND Myocardial Ischemia [MeSH Terms]” |
| “Anesthesia, Dental [MeSH Terms] AND Heart Arrest [MeSH Terms]” |
| “Anesthesia, Dental [MeSH Terms] AND Cardiomyopathies [MeSH Terms]” |
| “Anesthesia, Dental [MeSH Terms] AND Arrhythmias, Cardiac [MeSH Terms]” |
| “Anesthesia, Dental [MeSH Terms] AND Heart Valve Diseases [Mesh]” |
Table 2.
Inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
Figure 1.
PRISMA flow diagram.
To provide reliable evidence, a critical appraisal of all included articles was carried out. The criteria for this purpose were applied from the “Methods Guide for Comparative Effectiveness Reviews” created by the American Agency for Healthcare Research and Quality [12]. The overall judgement was assessed as high or unclear risk, when 1 or more key domains was assessed as high or unclear. A low-risk judgement was formed when all key domains were at “low risk”. This review was registered in “PROSPERO International prospective register of systematic reviews” as CRD42013004928.
Results
Of the 294 articles initially found, an automatic rejection of duplicates in the EndNote X5 reference manager resulted in 138 articles. After screening the abstracts, 100 articles were excluded. Eligibility verification of full-text articles resulted in the final inclusion of 11 papers.
Six randomized clinical trials (RCT) and 5 controlled clinical trials (CCT) with no randomization met the inclusion criteria across all studies.
The risk of bias assessment revealed that all RCTs were low risk. Among CCTs, 2 papers had unclear risk and 3 had low risk. More detailed information is presented in Table 3.
Table 3.
Risk of bias assessment.
| Randomized clinical trails | Controlled clinical trails | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Conrado et al. | Elad et al. | Middlehurst et al. | Neves et al. | Ogunlewe et al. | Torres-Lagares et al. | Binder et al. | Chaudhry et al. | Niwa et al. | Laragnoit et al. | Silvestre et al. | ||
| Selection bias | + | + | + | + | + | + | Selection bias | + | + | + | + | + |
| Performance bias | + | + | + | + | + | + | Performance bias | + | + | + | + | + |
| Attrition bias | + | + | + | + | + | + | Attrition bias | + | + | + | + | + |
| Detection bias | + | + | + | + | + | + | Detection bias | ? | ? | + | + | + |
| Reporting bias | + | + | + | + | + | + | Reporting bias | + | + | + | + | + |
| Overall judgement | + | + | + | + | + | + | Overall judgement | ? | ? | + | + | + |
+ Low risk of bias; − high risk of bias; ? unclear risk of bias.
The total number of patients was 567. Seven patients were excluded, 1 due to missing documentation (Elad et al.) and 6 due to motion artefacts during ECG (Neves et al.). Demographic data are presented in Table 4.
Table 4.
Demographic data.
| Total number of patients | Mean age | Gender | Study | |
|---|---|---|---|---|
| 40 | 66 | M 23 F 17 | Blinder D. et al. | |
|
| ||||
| 60 | Pre-HTN 10 | 52.6±11.07 | M 32 F28 | Chaudhry S. et al. |
| HTN-1 10 | 49.33±5.85 | |||
| HTN-2 10 | 59.16±12.0 | |||
| NT 30 | 43±11.04 | |||
|
| ||||
| 54 | ME 27 | 58±7.98 | M 34 F 20 | Conrado V.C.L.S. et al. |
| PM 27 | 55.3±8.57 | |||
|
| ||||
| 49 | AE 25 | 61.8±10.6 | M 39 F11* | Elad S. et al. |
| LE 24 | 60.4±11 | |||
|
| ||||
| 59 | LE 28 | 40.3±10.9 | Laragnoit A.B. et al. | |
| PL 31 | 42.2±10.3 | – | ||
|
| ||||
| 56 | LE 27 | 58.7±8.8 | M 51 F 11* | Neves R.S. et al. |
| PL 29 | ||||
|
| ||||
| 27 | 53±15.25 | M 16 F 11 | Niwa H. et al. | |
|
| ||||
| 75 | LNEV 50 | 58.3±11.0 | M 56 F 19 | Middlehurst R.J. et al. |
| LNEV+M 25 | 57.7±13.6 | |||
|
| ||||
| 33 | LE 14 | 50.1±11.7 | M 13 F 20 | Ogunlewe M.O. et al. |
| PL19 | ||||
|
| ||||
| 97 | 60.45±9.60 | M 33 F 64 | Silvestre F.J. et al. | |
|
| ||||
| 10 | 63±12.5 | – | Torres-Lagares D. et al. | |
Before exclusion. LE – lidocaine with epinephrine; PL – (plain) lidocaine; ME – mepivacaine with epinephrine; PM – (plain)mepivacaine; AE – articaine with epinephrine; LNEV – lidocaine with norepinephrine and vasopressin; M – midazolam; Pre-HTN – pre-hypertension; HTN-1 – hypertension 1st stage; HTN-2 – hypertension 2nd stage; NT – normotensive patients.
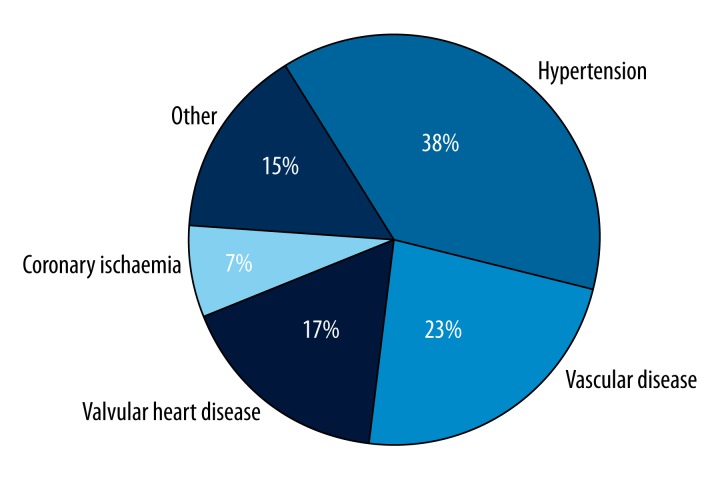
Among all of the included patients, the most frequent underlying pathology was hypertension. Other conditions are presented in Figure 2. When 1 patient was related to 2 or more categories, it was assigned to each relevant group.
Figure 2.
Cardiovascular disease distribution.
Only 3 authors reported the occurrence of any comorbid disease [16,18,21]. Neves et al. had 24 diabetic patients. Silvestre et al. had 27 with dyslipidemia and some with diabetes and stroke histories, but the exact number cannot be extracted. Additionally, Torres-Lagares et al. reported 10 more patients with different comorbidities.
The most frequently used anaesthesia was lidocaine at 2%. Three studies showed the use of articaine [14,18,21] and 3 mepivacaine [13,18,21]. The most commonly used vasoconstrictor was adrenaline (1:100000). One author reported premedication usage before the procedure. A control group appeared in 6 studies. The doses applied varied between from 1.8 to 6.9 ml (Table 5).
Table 5.
Comparison of complication events.
| Anaesthetic | Dose of anaesthesia | Type of complication | Percent of patients | Study |
|---|---|---|---|---|
| 2% lidocaine with 1:100,000 epinephrine | 5.4 ml or less | Arrhythmia | 15% | Blinder D. et al. |
| ST-segment depression | 2.5% | |||
| Tachycardia, increased HR | 20% | |||
| 2% lignocaine with 1:100,000 epinephrine | 3.6 ml | – | – | Chaudhry S. et al. |
| 2% mepivacaine with 1:100,000 epinephrine | 1.89 cartridges | ST-segment depression | 11,1% | Conrado V.C.L.S. et al. |
| 3% mepivacaine without vasoconstrictor | 1.56 cartridges | – | – | |
| Articaine 4% and adrenalin 1:200,000 | 1.8 ml | Asymptomatic ischaemic changes (EKG) | 8% | Elad S. et al. |
| Lidocaine 2% and adrenalin 1:100,000 | 1.8 ml | Transient local neuropathy | 4.2% | |
| Asymptomatic ischaemic changes (EKG) | 4.2% | |||
| 2% lidocaine with epinephrine 1: 100,000 | 1.8 ml | – | – | Laragnoit A.B. et al. |
| 2% lidocaine | 5.4 ml for 75% of the cases | |||
| 2% lidocaine and 1:100,000 epinephrine | 1.8–3.6 ml | ST-segment depression | 14.8% | Neves R.S. et al. |
| Arrhythmia | 25.9% | |||
| 2% lidocaine without epinephrine | 1.8–3.6 ml | ST-segment depression | 20.7% | |
| Arrhythmia | 34.5% | |||
| 2% lidocaine with 1:80,000 epinephrine | 1.8 ml | – | – | Niwa H. et al. |
| Lidocaine 2%, noradrenaline 1:50,000, vasopressin 0.25 IU/mL | LNEV: 4.9±2.0 ml | Dysrhythmia | 50% | Middlehurst R.J. et al. |
| LNEV+M: 5.5±1.4 ml | Dysrhythmia | 52% | ||
| 2% lignocaine with 1:80 000 adrenaline | 3.6 ml | – | – | Ogunlewe M.O. et al. |
| 2% lignocaine | ||||
| 4% articaine with epinephrine 1: 200,000 | 1.8–5.4 ml | – | – | Silvestre F.J. et al. |
| 3% mepivacaine | ||||
| Mepivacaine 30 mg without epinephrine | 3.6 ml | – | – | Torres-Lagares D. et al. |
| Articaine 40 mg with epinephrine 0.5mg% | ||||
| Articaine 40 mg with epinephrine 1 mg% | ||||
| Mepivacaine 20 mg with epinephrine 1 mg% |
Among 560 patients after the administration of a local anaesthetic, 87 complications occurred. The most frequent complication was arrhythmia. Asymptomatic ischaemic changes were seen in 3 patients. One case of transient local neuropathy was noted (Table 5). No severe adverse clinical effects were reported.
Discussion
A mean age of over 50, being male, and the presence of comorbid disease may provide a representative group. Other increased levels of evidence and low risk of bias in the included articles could be sufficient evidence for clinical decisions to be made.
The overall complication rate across studies was 15.5%. The highest proportion of complication (43.6%) was reported by Middlehurst et al. with noradrenaline (1:50000) + vasopressin 0.25 IU/ml. Additionally, midazolam was administrated as a premedication in 1 of the study groups. This high complication rate could result from the monitoring method used. Middlehurst et al. counted and analysed ECG waves (QRS complexes) from the sedation to recovery period. However, 2.7% of waves from LNEV and 5.7% from the LNEV+M group were found to be clinically significant [15]. It should also be noted that the anaesthesia scheme presented by Middlehurst et al. is not the most commonly used method in dental practice. Excluding this study from analysis due to inability to define the number of patients with clinically significant complications, the overall complication rate decreases to 8.75%.
Moreover, the transient local neuropathy reported in the Elad et al. study cannot be related to the presence of vasoconstrictor agents. Furthermore, a temporal analysis of the ischaemic changes reveals that they were not related to timing of the LA.
Neves et al. reported that 41.2% arrhythmias occurred during the procedure and the frequency of arrhythmias in a group with/without vasoconstrictor agents did not reveal a significant difference. Interestingly, arrhythmias have been reported in 37.5% of healthy patients who undergo multiple dental extractions under a local anaesthetic with a vasopressor agent [22]. In the Neves et al. study it was impossible to extract data about pre-anaesthesia ECG records. Therefore, the aforementioned data cannot be interpreted as stemming from the use of a vasoconstrictor agent. Another complication (ST-segment depression) occurred more than 2 hours after the procedure was completed. Additionally, complications reported by Blinder et al. took place 2 hours after the dental procedure. This relatively long time period is clearly not enough to establish a direct relationship between the vasoconstrictor agent and ECG records.
Among all complications, only 10 may be directly related to the use local anaesthesia. It is noteworthy that 40% appeared after the administration of anaesthesia without vasoconstrictor agents. No severe adverse clinical effects were noted in the analysed studies.
Conclusions
The most frequent complications in cardiovascular compromised patients after dental local anaesthesia with vasoconstrictor agent were disclosed in ECG arrhythmias.
The range of diagnostic criteria complication frequency depends on application by different authors and ranges from 0% to 50%.
A major part of the disclosed arrhythmias were clinically insignificant.
The use of ≤4 ampules of lignocaine with epinephrine 1:100000 as a dental anaesthetic seems to be relatively safe for cardiovascular compromised patients.
During the application of higher doses of anaesthesia or a higher concentration of an anaesthetic agent in cardiovascular compromised patients, ECG monitoring should be considered due to insufficient evidence of the safety of higher dosage use.
Footnotes
Source of support: Self financing
References
- 1.Holm SW, Cunningham LL, Bensadoun JE, Madsen MJ. Classification, pathophysiology, and management during outpatient sedation and local anesthesia. J Oral Maxillofac Surg. 2006;64:111–21. doi: 10.1016/j.joms.2005.09.023. [DOI] [PubMed] [Google Scholar]
- 2.Kabambe WM, Rood JP, Sowray JH. A comparison of plain 2 percent lignocaine and 2 percent lignocaine with adrenaline in local analgesia for minor oral surgery. J Dent. 1982;10:136–39. doi: 10.1016/s0300-5712(82)80007-9. [DOI] [PubMed] [Google Scholar]
- 3.Davenport RE, Porcelli RJ, Iacono VJ, et al. Effects of anesthetics containing epinephrine on catecholamine levels during periodontal surgery. J Periodontol. 1990;61:553–58. doi: 10.1902/jop.1990.61.9.553. [DOI] [PubMed] [Google Scholar]
- 4.Niwa H, Sugimura M, Satoh Y, Tanimoto A. Cardiovascular response to epinephrine-containing local anesthesia in patients with cardiovascular disease. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:610–16. doi: 10.1067/moe.2001.118903. [DOI] [PubMed] [Google Scholar]
- 5.Bader JD, Bonito AJ, Shugars DA. A systematic review of cardiovascular effects of epinephrine on hypertensive dental patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:647–53. doi: 10.1067/moe.2002.123866. [DOI] [PubMed] [Google Scholar]
- 6.Blinder D, Manor Y, Shemesh J, Taicher S. Electrocardiographic changes in cardiac patients having dental extractions under a local anesthetic containing a vasopressor. J Oral Maxillofac Surg. 1998;56:1399–402. doi: 10.1016/s0278-2391(98)90403-7. [DOI] [PubMed] [Google Scholar]
- 7.Meyer FU. Haemodynamic changes under emotional stress following a minor surgical procedure under local anaesthesia. Int J Oral Maxillofac Surg. 1987;16:688–94. doi: 10.1016/s0901-5027(87)80054-1. [DOI] [PubMed] [Google Scholar]
- 8.Meyer FU. Hemodynamic changes of local dental anaesthesia in normotensive and hypertensive subjects. Int J Clin Pharmacol Ther Toxicol. 1986;24:477–81. [PubMed] [Google Scholar]
- 9.Brand HS, Gortzak RA, Palmer-Bouva CC, et al. Cardiovascular and neuroendocrine responses during acute stress induced by different types of dental treatment. Int Dent J. 1995;45:45–48. [PubMed] [Google Scholar]
- 10.Akutsu A, Chiba T, Takahashi H, et al. Management of dental problems in patients with cardiovascular disease. J Am Dent Assoc. 1964;68:333–42. doi: 10.14219/jada.archive.1964.0104. [DOI] [PubMed] [Google Scholar]
- 11.Budentz AW. Local anesthetics and medically complex patients. J Calif Dent Assoc. 2000;28:611–19. [PubMed] [Google Scholar]
- 12.Viswanathan M, Ansari MT, Berkman ND, et al. Methods Guide for Effectiveness and Comparative Effectiveness Reviews [Internet] Rockville: Agency for Healthcare Research and Quality; 2012. Mar 8, Assessing the Risk of Bias of Individual Studies in Systematic Reviews of Health Care Interventions. Available from: http://www.ncbi.nlm.nih.gov/books/NBK91433/ [PubMed] [Google Scholar]
- 13.Conrado VC, De Andrade J, De Angelis GA, et al. Cardiovascular Effects of Local Anesthesia with Vasoconstrictor during Dental Extraction in Coronary Patients. Arq Bras Cardiol. 2007;88:507–13. doi: 10.1590/s0066-782x2007000500002. [DOI] [PubMed] [Google Scholar]
- 14.Elad S, Admon D, Kedmi M, et al. The cardiovascular effect of local anesthesia with articaine plus 1: 200,000 adrenalin versus lidocaine plus 1: 100,000 adrenalin in medically compromised cardiac patients: a prospective, double blinded study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:725–30. doi: 10.1016/j.tripleo.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 15.Middlehurst RJ, Gibbs A, Walton G. Cardiovascular risk: the safety of local anesthesia, vasoconstrictors, and sedation in heart disease. Anesth Prog. 1999;46:118–23. [PMC free article] [PubMed] [Google Scholar]
- 16.Neves RS, Neves IL, Giorgi DM, et al. Effects of epinephrine in local dental anesthesia in patients with coronary artery disease. Arq Bras Cardiol. 2007;88:482–87. doi: 10.1590/s0066-782x2007000500008. [DOI] [PubMed] [Google Scholar]
- 17.Ogunlewe MO, James O, Ajuluchukwu JN, et al. Evaluation of haemodynamic changes in hypertensive patients during tooth extraction under local anaesthesia. West Indian Med J. 2011;60:91–95. [PubMed] [Google Scholar]
- 18.Torres-Lagares D, Serrera-Figallo MÁ, Machuca-Portillo G, et al. Cardiovascular effect of dental anesthesia with articaine (40 mg with epinefrine 0.5 mg% and 40 mg with epinefrine 1 mg%) versus mepivacaine (30 mg and 20 mg with epinefrine 1 mg%) in medically compromised cardiac patients: a cross-over, randomized, single blinded study. Med Oral Patol Oral Cir Bucal. 2012;17:655–60. doi: 10.4317/medoral.17892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chaundhry S, Iqbal HA, Izhar F, et al. Effect on blood pressure and pulse rate after administration of an epinephrine containing dental local anaesthetic in hypertensive patients. J Pak Med Assoc. 2011;61:1088–91. [PubMed] [Google Scholar]
- 20.Laragnoit AB, Neves RS, Neves IL, Vieira JE. Locoregional anesthesia for dental treatment in cardiac patients: a comparative study of 2% plain lidocaine and 2% lidocaine with epinephrine (1:100,000) Clinics. 2009;64:177–82. doi: 10.1590/S1807-59322009000300005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Silvestre FJ, Salvador-Martinez I, Bautista D, Silvestre-Rangil J. Clinical study of hemodynamic changes during extraction in controlled hypertensive patients. Med Oral Patol Oral Cir Bucal. 2011;16:354–58. doi: 10.4317/medoral.16.e354. [DOI] [PubMed] [Google Scholar]
- 22.Driscoll EJ, Smilack ZH, Lightbody PM, Fiorucci RD. Sedation with intravenous diazepam. J Oral Surg. 1972;30:332–43. [PubMed] [Google Scholar]