Abstract
Objective
The purpose of this study was to evaluate the efficacy of implant removal of percutaneous short segment fixation after vertebral fracture consolidation in terms of motion preservation.
Methods
Between May 2007 and January 2011, 44 patients underwent percutaneous short segment screw fixation due to a thoracolumbar burst fracture. Sixteen of these patients, who underwent implant removal 12 months after screw fixation, were enrolled in this study. Motor power was intact in all patients, despite significant vertebral height loss and canal compromise. The patients were divided into two groups by degree of osteoporosis : Group A (n=8), the non-osteoporotic group, and Group B (n=8), the osteoporotic group. Imaging and clinical findings including vertebral height loss, kyphotic angle, range of motion (ROM), and complications were analyzed.
Results
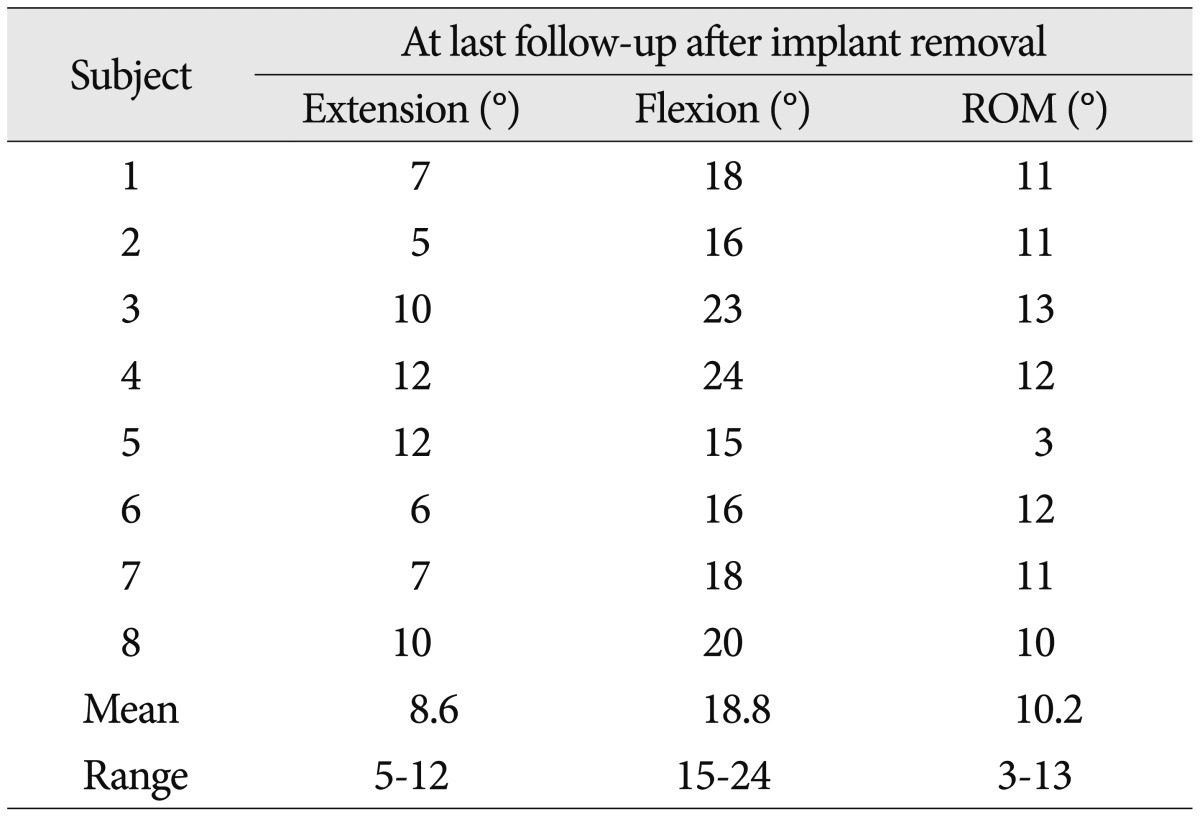
Significant pain relief was achieved in both groups at final follow-up versus preoperative values. In terms of vertebral height loss, both groups showed significant improvement at 12 months after screw fixation and restored vertebral height was maintained to final follow-up in spite of some correction loss. ROM (measured using Cobb's method) in flexion and extension in Group A was 10.5° (19.5/9.0°) at last follow-up, and in Group B was 10.2° (18.8/8.6°) at last follow-up. Both groups showed marked improvement in ROM as compared with the screw fixation state, which was considered motionless.
Conclusion
Removal of percutaneous implants after vertebral fracture consolidation can be an effective treatment to preserve motion regardless of osteoporosis for thoracolumbar burst fractures.
Keywords: Fusion, Percutaneous, Removal
INTRODUCTION
The goal of any management regime for burst fractures is primarily to prevent neurological injury with restoration of spinal stability, whereas correction of deformity, minimizing loss of movement, and early return to daily life are secondary considerations. Thoracolumbar burst fractures result from compression failure of both the anterior and middle columns under substantial vertical load2). There is no controversy regarding the need for surgery in patients with a progressive neurological deficit, an unstable fracture with complete neurological loss, or in patients with polytrauma that require fixation for early rehabilitation. However, no consensus has been reached on the management of thoracolumbar burst fractures without neurologic deficits. In fact, some authors have reported excellent outcomes after conservative treatment despite increased residual kyphotic deformity15). The injured structures are also capable of healing naturally in time and a burst fracture, which is unstable by definition, may become stable after natural healing of the injured structures. On the other hand, surgical management provides immediate spinal stability and more reliably restore sagittal alignment and canal dimensions14). Recently, good clinical outcomes were reported for short segment fixation without bone fusion6,9,10,11). Implant-related complications were low, and early clinical outcomes were satisfactory. Furthermore, percutaneous screw fixation has been proposed and applied to minimize the negative consequences of traditional open surgery, which include muscular denervation and atrophy3). However, as far as we are aware, no study has investigated clinical outcomes and ranges of motion (ROM) after implant removal following short segment fixation using percutaneous screws. For this reason, we sought to determine whether implant removal after vertebral fracture consolidation increases ROM, and whether the presence of osteoporosis influences clinical results. The hypothesis of this study was that ROM can be achieved by screw removal after natural bone healing and consolidation of fractured vertebra.
MATERIALS AND METHODS
Between May 2007 and January 2011, 44 patients underwent percutaneous short segment fixation for a thoracolumbar burst fracture. Sixteen of these patients, who underwent implant removal after percutaneous short segment fixation were enrolled in this study. They underwent implant removal at 12 months after screw fixation when spontaneous bone healing of the fractured vertebra was achieved based on computed tomography (CT) findings. The inclusion criteria for percutaneous short segment fixation were : 1) neurologically intact patients with a single level thoracolumbar burst fracture, 2) a kyphotic angle of >30°, or an anterior vertebral height loss of >40% or canal compromise of >50%, and 3) intact bilateral pedicles, enabling screw insertion at fractured vertebra. To study whether the presence of osteoporosis influences clinical results, the 16 subjects were divided into two groups based on the presence of osteoporosis, that is, to 1) Group A (n=8) : non-osteoporotic group [T-score by bone mineral densitometry (BMD) >-2.5], or to 2) Group B (n=8) : osteoporotic group (T-score by BMD <-2.5). Bone cement augmentation using polymethylmethacrylate (PMMA) was performed in Group B. The exclusion criteria were a major neurological deficit requiring open decompression due to severe canal compromise and an accompanying pedicle fracture preventing screw insertion at the fracture level. Preoperatively, for postural reduction, patients were positioned supine with a pillow under fractured vertebra for 2-3 days. Imaging and clinical findings, level of the involved vertebra, vertebral height restoration, intersegmental ROM, clinical outcomes, and complications were analyzed. Intersegmental ROM was calculated using Cobb's flexion and extension measurements by drawing a straight line from the superior endplate of the vertebra one level above the fractured body and a straight line from the inferior endplate of the vertebra one level below the fractured body.
Safety and outcome evaluations
Clinical outcomes at different time points were evaluated using a 10 point visual analogue scale (VAS). Simple radiographs and CT and MR images were used to evaluate kyphotic angulation and instrumentation integrity at the level of operative segments preoperatively, just before implant removal, and at final follow-up.
Statistics
Statistical analysis was performed using SAS 6.12 (SAS Institute, Inc., Cary, NC, USA). A paired Student's t-test and Mann-Whitney's U test were used to compare the measures taken at different times. Differences were considered statistically significant when p values were <0.05.
RESULTS
With respect to the anatomic fracture distribution, there were T11 (n=2), T12 (n=6), Ll (n=5), and L2 (n=3). Patient demographics, including age, gender, BMD, fracture level, and mean follow-up period are summarized in (Table 1). The composite injury severity score derived from the thoracolumbar injury classification and severity score was 4 points or greater points, which could be considered for operative intervention in all patients. The patients were postoperatively followed clinically and radiologically and we analyzed the results at 12 months after screw fixation around implant removal and at final follow-up.
Table 1.
Basic characteristics of patients
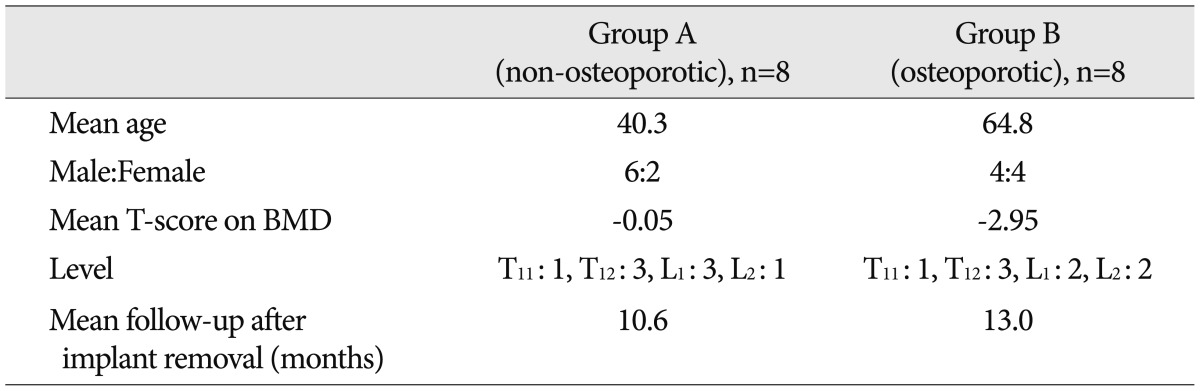
BMD : bone mineral densitometry
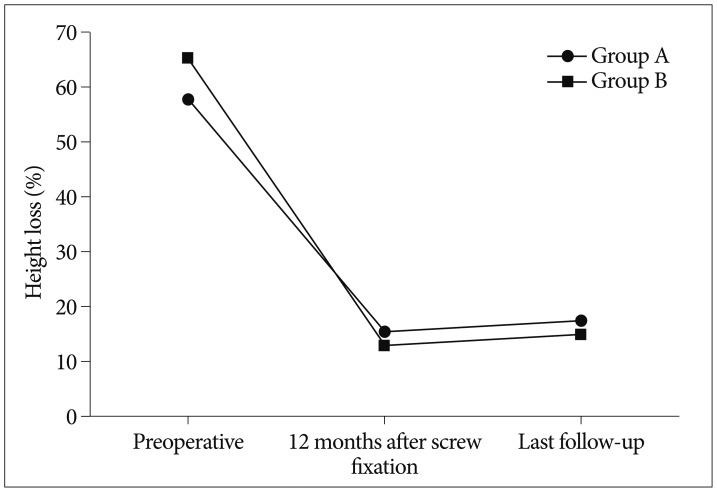
Restoration of vertebral height
Average preoperative height loss of involved vertebrae in Group A was 58.1%. Just before implant removal and final follow-up after implant removal, mean vertebral height losses in Group A were 15.3% and 17.4%, respectively. In Group B, vertebral height losses preoperatively, immediately before implant removal, and at last follow-up were 65.6%, 12.9%, and 15.1%, respectively (Fig. 1). Both groups showed significant improvements versus preoperative values despite some vertebral height loss after implant removal (p<0.01).
Fig. 1.
Restoration of vertebral height.
Range of motion
Intersegmental ROMs were assessed at last follow-up using Cobb's method at the superior endplates of upper fractured vertebrae and at the inferior endplates of lower fractured vertebrae. Preoperatively, due to the risk of neurologic aggravation, flexion and extension radiographs were not obtained. Table 2, 3 summarize Cobb flexion and extension measurements and provide individual patient means and ranges. In both groups, ROM improved significantly between just before implant removal, which was considered motionless and at last follow-up after implant removal (p<0.01).
Table 2.
Calculated intersegmental ranges of motion (ROM) calculated from Cobb flexion and extension measurements in Group A
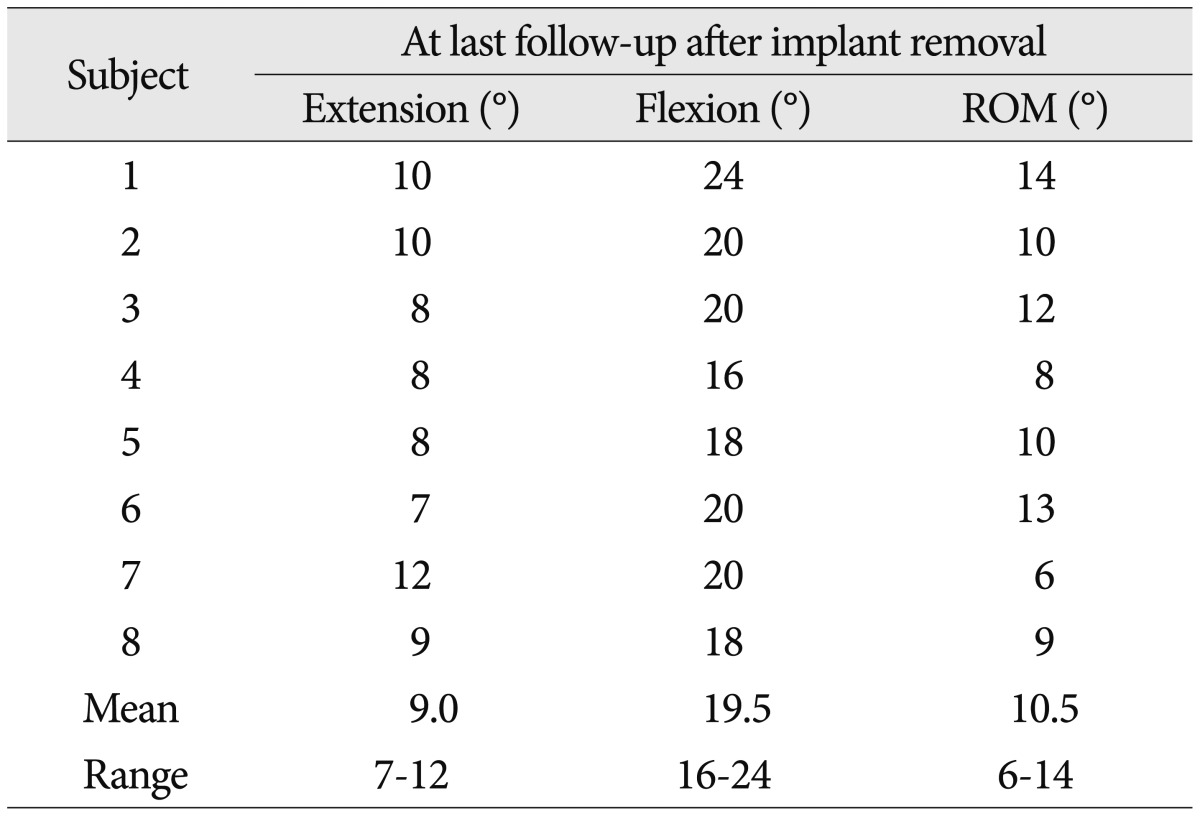
Table 3.
Calculated intersegmental ranges of motion (ROM) calculated from Cobb flexion and extension measurements in Group B
Clinical outcome
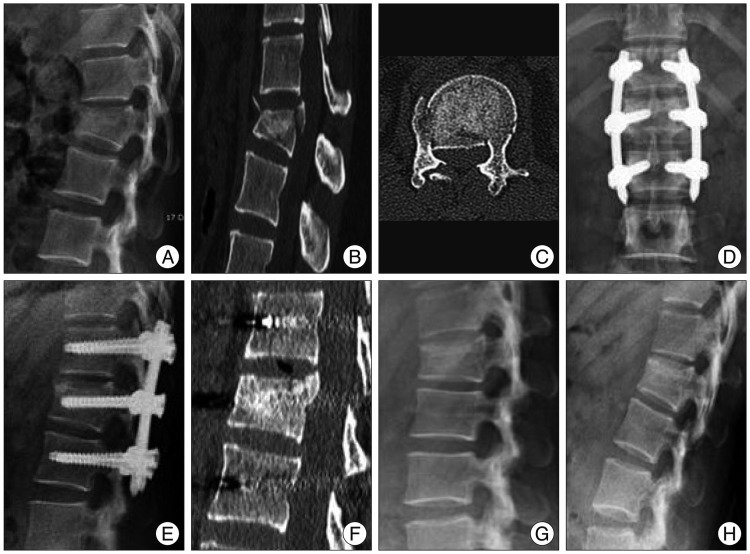
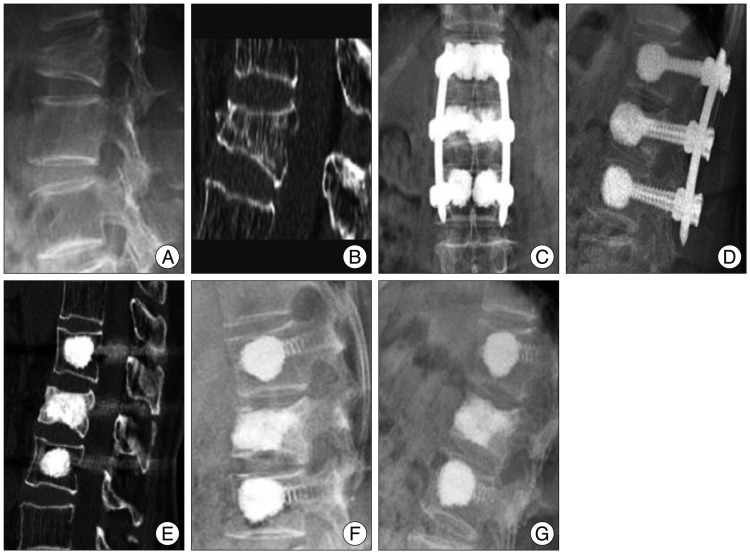
At the time of implant removal, there were no failures of posterior instrumentation, including breakage, bending, or loosening of any screw. Significant pain relief was achieved in both groups at final follow-up versus preoperative values (p<0.005). In Group A (the non-osteoporotic group), mean VAS score was 7.9 before surgery and 2.5 at final follow-up, and in Group B, mean VAS was 8.0 before surgery and 2.4 at last follow-up. One case of asymptomatic cement leakage into the paravertebral area was observed in Group B. However, no major complications, such as, neurological deterioration, aggravation of vertebral height, or canal compromise occurred during follow-up after implant removal in either group (Fig. 2, 3).
Fig. 2.
A case of a neurologically intact 29-year-old woman with a L1 burst fracture (Group A). A, B, and C : Preoperative simple radiograph and computed tomography images showing about 40% height loss and 50% canal compromise. D, E, and F : Simple radiographs and a computed tomography image taken at 12 months after percutaneous screw fixation showing consolidation of the fractured body and improved kyphosis. G and H : Simple flexion and extension radiographs taken at 11 months after screws removal revealing well-maintained range of motion, which coincided with a completely pain free status.
Fig. 3.
A case of a neurologically intact 72-year-old woman with a L1 burst fracture (Group B). A and B : Preoperative simple radiograph and computed tomography image showing about 60% height loss. C, D, and E : Simple radiographs and a computed tomography image taken at 12 months after percutaneous screw fixation showing consolidation of the fractured body and restored vertebral height. F and G : Simple flexion and extension radiographs taken at 13 months after screw removal reveal a well-maintained range of motion, which coincided with a completely pain free status.
DISCUSSION
Burst fractures are common at the thoracolumbar junction because the region constitutes a transitional zone between the relatively fixed kyphotic thoracic area and the mobile lordotic lumbar region4). Restoration of stability, prevention of neurological deterioration, attainment of canal clearance, prevention of kyphosis, and rapid pain relief are the most commonly cited reasons for surgical intervention12). Burst fractures are 2 or 3 column injuries that may lead to spinal column instability when they present with severe canal compromise of >50%, vertebral height loss of >40%, angular deformity of >30°, multiple contiguous fractures or any neurologic injury. Symptomatic, unstable burst fractures typically require surgical reduction and stabilization, but decision-making regarding conservative versus operative treatment for unstable thoracolumbar burst fractures in the absence of any neurologic deficit remains controversial, as many authors have reported satisfactory results for the conservative treatment of such fractures1,17). However, conservative treatment may lead to ongoing neurogenic pain and progressive kyphotic deformity. On the other hand, screw fixation with bone fusion more reliably restores sagittal alignment, kyphotic deformity, and canal dimensions9). Nevertheless, despite its advantages, this technique is associated with risks of complications and inevitable motion limitation. Wang et al.16) reported satisfactory results for short-segment fixation without fusion of surgically-treated thoracolumbar burst fractures. It was found that low back outcome scores were similar for burst fractures treated surgically in those with or without bone fusion16). Recently, some good clinical outcomes were also reported with short segment fixation and anterior body augmentation using injectable calcium sulphate cement or calcium phosphate cement without bone fusion10,11). The procedures were effective for correcting deformity and maintaining adequate body height and alignment.
Theoretically, when natural bone healing and consolidation of fractured vertebrae has occurred, implant removal should allow complete motion segment preservation. The advantages of implant removal after screw fixation without fusion are the elimination of donor site complications, the preservation of motion segments, reduced blood loss, and shorter operation time. More recently, some investigators have reported successful surgical outcomes for percutaneous short segment fixation without fusion5,8). In the present study, short segment fixation without bone fusion followed by screw removal after bone consolidation was found to have the advantages of early ambulation, minimizing tissue injury, and complete motion preservation regardless of osteoporosis. Furthermore, segmental stability was obtained by screw fixation before fracture consolidation, and after natural bone healing, implant removal made it possible to preserve motion. However, screw loosening or vertebral collapse may occur after percutaneous screwing procedures, and these problems may be more significant for osteoporotic spines. Failure to support the anterior column can lead to the eventual loss of correction and high rate of posterior instrument failure. Thus, bone cement augmentation at fractured bodies and adjacent vertebrae was performed to address these limitations. In addition, the insertion of bone cement-augmented pedicle screws results in segmental constructs with improved biomechanical stability due to the protection afforded to fractured vertebra and indirect support of the anterior column13). The insertion of bone cement-augmented pedicle screws can significantly reduce pedicle screw bending and increase initial stiffness in the flexion-extension plane7). Our findings support motion preservation by percutaneous short segment screw fixation without bone fusion and implant removal after fractured body consolidation for neurologically intact thoracolumbar burst fractures regardless of the presence of osteoporosis.
In the present study, we addressed the question as to whether osteoporosis influences clinical and radiological results, and we found that bone cement augmentation made it possible to maintain stability even in osteoporotic spines. However, in spite of acceptable clinical and radiological outcome, this study has some limitations. There is no control group to compare range of motion radiologically. In spite of statistically significance, sixteen patients are rather small group for such a clinical study. The timing of the removal of the implant still remains as an open question. Although PMMA was used for the augmentation of the fractured vertebral body in osteoporotic group, the study using alternative materials such as hydroxyapatite is mandatory and randomized prospective clinical trials with longer observation periods in larger populations are necessary to confirm our results.
CONCLUSION
Percutaneous short segment fixation without bone fusion followed by screw removal after fractured body consolidation appears to provide a safe and effective treatment that allows achievement of complete ROM. Even in the osteoporotic thoracolumbar burst fractures, satisfactory result can be obtained by bone cement augmentation procedure using PMMA.
Acknowledgements
The present study was supported by grants from the Clinical Medicine Research Institute at Chosun University Hospital 2013.
References
- 1.Chow GH, Nelson BJ, Gebhard JS, Brugman JL, Brown CW, Donaldson DH. Functional outcome of thoracolumbar burst fractures managed with hyperextension casting or bracing and early mobilization. Spine (Phila Pa 1976) 1996;21:2170–2175. doi: 10.1097/00007632-199609150-00022. [DOI] [PubMed] [Google Scholar]
- 2.Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983;8:817–831. doi: 10.1097/00007632-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Gahr RH, Strasser S, Strasser E, Schmidt OI. Percutanous internal fixation of thoracolumbar spine fractures. Top Spinal Cord Inj Rehabil. 2006;12:45–54. [Google Scholar]
- 4.Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine (Phila Pa 1976) 1992;17:528–540. doi: 10.1097/00007632-199205000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Huang QS, Chi YL, Wang XY, Mao FM, Lin Y, Ni WF, et al. [Comparative percutaneous with open pedicle screw fixation in the treatment of thoracolumbar burst fractures without neurological deficit] Zhonghua Wai Ke Za Zhi. 2008;46:112–114. [PubMed] [Google Scholar]
- 6.Jang KS, Ju CI, Kim SW, Lee SM. Screw fixation without fusion for low lumbar burst fracture : a severe canal compromise but neurologically intact case. J Korean Neurosurg Soc. 2011;49:128–130. doi: 10.3340/jkns.2011.49.2.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jung HJ, Kim SW, Ju CI, Kim SH, Kim HS. Bone cement-augmented short segment fixation with percutaneous screws for thoracolumbar burst fractures accompanied by severe osteoporosis. J Korean Neurosurg Soc. 2012;52:353–358. doi: 10.3340/jkns.2012.52.4.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim HS, Kim SW, Ju CI, Lee SM, Shin H. Short segment fixation for thoracolumbar burst fracture accompanying osteopenia : a comparative study. J Korean Neurosurg Soc. 2013;53:26–30. doi: 10.3340/jkns.2013.53.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim HY, Kim HS, Kim SW, Ju CI, Lee SM, Park HJ. Short segment screw fixation without fusion for unstable thoracolumbar and lumbar burst fracture : a prospective study on selective consecutive patients. J Korean Neurosurg Soc. 2012;51:203–207. doi: 10.3340/jkns.2012.51.4.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Korovessis P, Repantis T, George P. Treatment of acute thoracolumbar burst fractures with kyphoplasty and short pedicle screw fixation : transpedicular intracorporeal grafting with calcium phosphate : a prospective study. Indian J Orthop. 2007;41:354–361. doi: 10.4103/0019-5413.37000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liao JC, Fan KF, Chen WJ, Chen LH. Posterior instrumentation with transpedicular calcium sulphate graft for thoracolumbar burst fracture. Int Orthop. 2009;33:1669–1675. doi: 10.1007/s00264-008-0677-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 13.Mahar A, Kim C, Wedemeyer M, Mitsunaga L, Odell T, Johnson B, et al. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine (Phila Pa 1976) 2007;32:1503–1507. doi: 10.1097/BRS.0b013e318067dd24. [DOI] [PubMed] [Google Scholar]
- 14.Mueller LA, Mueller LP, Schmidt R, Forst R, Rudig L. The phenomenon and efficiency of ligamentotaxis after dorsal stabilization of thoracolumbar burst fractures. Arch Orthop Trauma Surg. 2006;126:364–368. doi: 10.1007/s00402-005-0065-6. [DOI] [PubMed] [Google Scholar]
- 15.Mumford J, Weinstein JN, Spratt KF, Goel VK. Thoracolumbar burst fractures. The clinical efficacy and outcome of nonoperative management. Spine (Phila Pa 1976) 1993;18:955–970. [PubMed] [Google Scholar]
- 16.Wang ST, Liu CL, Yu WK, Chang MC, Chen TH. Is fusion necessary for surgically treated burst fractures of the thoracolumbar and lumbar spine? : a prospective, randomized study. Spine (Phila Pa 1976) 2006;31:2646–2652. doi: 10.1097/01.brs.0000244555.28310.40. discussion 2653. [DOI] [PubMed] [Google Scholar]
- 17.Weinstein JN, Collalto P, Lehmann TR. Thoracolumbar "burst" fractures treated conservatively : a long-term follow-up. Spine (Phila Pa 1976) 1988;13:33–38. doi: 10.1097/00007632-198801000-00008. [DOI] [PubMed] [Google Scholar]