Abstract
BACKGROUND
Night blood pressure (BP) predicts patient outcomes. Variables associated with night BP response to antihypertensive agents have not been fully evaluated in essential hypertension.
METHODS
We sought to measure night BP responses to hydrochlorothiazide (HCTZ), atenolol (ATEN), and combined therapy using ambulatory blood pressure (ABP) monitoring in 204 black and 281 white essential hypertensive patients. Initial therapy was randomized; HCTZ and ATEN once daily doses were doubled after 3 weeks and continued for 6 more weeks with the alternate medication added for combined therapy arms. ABP was measured at baseline and after completion of each drug. Night, day, and night/day BP ratio responses (treatment − baseline) were compared in race/sex subgroups.
RESULTS
Baseline night systolic BP and diastolic BP, and night/day ratios were greater in blacks than whites (P < 0.01, all comparisons). Night BP responses to ATEN were absent and night/day ratios increased significantly in blacks (P < 0.05). At the end of combined therapy, women, blacks, and those starting with HCTZ as opposed to ATEN had significantly greater night BP responses (P < 0.01). Variables that significantly associated with ATEN response differed from those that associated with HCTZ response and those that associated with night BP response differed from those that associated with day BP response.
CONCLUSIONS
In summary, after completion of HCTZ and ATEN therapy, women, blacks, and those who started with HCTZ had greater night BP responses. Reduced night BP response and increased night/day BP ratios occured with ATEN in blacks. Given the prognostic significance of night BP, strategies for optimizing night BP antihypertensive therapy should be considered.
CLINICAL TRIAL REGISTRATION
Clinicaltrials.gov identifier NCT00246519
Keywords: ambulatory blood pressure, atenolol, blood pressure, hydrochlorothiazide, hypertension, night/day ratio.
Twenty-four hour ambulatory blood pressure (ABP) associates with cardiovascular and patient outcomes1 and improves prediction of patient mortality and cardiovascular events as compared with office blood pressure (BP).2,3 Specifically, night BP and nocturnal decline in BP provide greater prognostic information than day BP in population-based surveys in treated and untreated hypertensive patients.3–8 An increased night/day BP ratio, a reduced nocturnal decline in BP, or the absence of a nocturnal BP dip associate with poor cardiovascular outcomes and increased patient mortality, even after adjusting for 24-hour BP levels.9 The importance of night BP with regard to patient outcomes has spurred interest in chronotherapy with late-day BP medication administration.10
Increased night/day BP ratios and nondipping occur in a variety of clinical settings. Night-shift workers demonstrate abnormal circadian BP and heart rate patterns,11 and individuals with underlying renal disease demonstrate greater night/day BP ratios and reduced dipping frequency.12,13 Individuals with primary hyperaldosteronism, salt sensitivity, increased sympathetic activity, and increased sodium intake demonstrate a blunted night BP decline.14–17 Hypertensive blacks demonstrate increased night BP levels, which may account, in part, for the higher incidence of stroke, congestive heart failure, and renal disease seen in this population.18–23 Whether sex influences night BP response to therapy is unclear; however, women demonstrate greater differences between office and ABP than men,23 and black women have a blunted night BP decline, similar to black men.24–28
Night BP response to antihypertensive agents has not been fully evaluated in hypertensive patients. A small group of nondipping essential hypertensive patients who received short-term (4 week) treatment with hydrochlorothiazide (HCTZ) demonstrated a return to a dipping pattern.29 Similar reversals occur shortly after successful kidney transplantation.30 In addition, once daily nighttime ingestion of angiotensin receptor blockers and angiotensin-converting enzyme inhibitors result in greater reduction in night BP and an increased frequency of dipping.10 Importantly, the reproducibility of dipping status is poor in healthy, hypertensive, and renal disease patients, suggesting that night/day BP ratios may be more informative about the benefits of night BP response to antihypertensive agents.31
Initial analyses of our Pharmacogenomic Evaluation of Antihypertensive Responses (PEAR) population indicated that after 9 weeks of atenolol (ATEN) or HCTZ therapy, 24-hour ABP responses were similar to office and home BP responses.32 However, night and night/day BP ratio responses have not yet been evaluated. We hypothesize that night and night/day BP ratio responses to HCTZ and ATEN are sex and race specific and differ from day BP responses with regard to the magnitude of the variability accounted for and the variables associated with the drug response. Therefore, we sought to determine the night and night/day BP ratio responses to the most commonly prescribed antihypertensive agents, HCTZ and ATEN, in both mono- and combination therapy in black and white hypertensive men and women and determined the variables contributing to the BP responses found.
METHODS
Study design
The PEAR study (ClinicalTrials.gov NCT00246519, http://clinicaltrials.gov/ct2/show/NCT00246519) includes subjects aged 17–65 years with mild to moderate essential hypertension.33 BP inclusion was determined using home BP and office BP after washout from all antihypertensive medications (mean = 29±16 days).33 Race was defined based on self-identification of investigator-specified options. Exclusion criteria included use of ≥3 antihypertensive drugs; systolic BP (SBP) > 170mm Hg on active treatment; other diseases or conditions requiring treatment with antihypertensive drugs, such as known cardiovascular disease, diabetes, renal insufficiency, pregnancy or lactation, Raynaud’s syndrome, and liver dysfunction; or chronic treatment with medications known to increase BP, such as nonsteroidal anti-inflammatory agents or oral contraceptives. Target BP for this short term study was <120/70mm Hg. This target was chosen to assure the highest likelihood of using the same (maximum) dose of either ATEN or HCTZ.
Eligible participants had ABP monitors (Spacelabs model 90207; Spacelabs, Redmond, WA) placed at their baseline visit as well at the end of each treatment period, and ABP and heart rate were recorded. Before the recording period, coordinators took 2 sphygmomanometer measurements following a standardized protocol. An appropriately sized cuff was placed on the participant’s nondominant arm, and 2 readings were manually initiated. Readings were repeated if SBP, diastolic BP (DBP), or heart rate fell outside the predefined acceptable ranges (SBP = 70–240mm Hg; DBP = 30–150mm Hg; heart rate = 20–150 bpm). After the initial 2 BP readings, duplicate readings were performed in the supine, sitting, and standing position. If SBP or mean arterial pressure (MAP) deviated by >8mm Hg, BP readings were repeated, and if discrepancies remained, the 24-hour ABP monitoring was not conducted. Once the subject was cleared to complete the ABP monitoring, they were instructed to keep their arms still and in an extended position during BP recordings. The ABP monitors were programmed to record BP and heart rate every 15 minutes from 6:00 am to 10:00 pm (daytime) and every 30 minutes from 10:00 pm until 6:00 am (nighttime). Subjects were instructed to conduct their usual daily activities during monitoring. Subjects were then randomized to receive either HCTZ 12.5mg daily or ATEN 50mg daily. Subjects were instructed by the coordinators at each study visit to take their medications upon rising before beginning their activities. After 3 weeks, the initial dose was doubled in all individuals with an average home or office BP >120/70mm Hg. They were maintained on this dose for a minimum of 6 additional weeks, after which ABP, home BP, and office BP response assessments were performed. Those with BP ≤120/70mm Hg at the end of 3 weeks of therapy completed these measurements at a minimum of 6 weeks on the initial dose of antihypertensive therapy. During the second phase of the study, which involved the addition of the alternative drug, subjects continued through the protocol in identical fashion to the first phase, after which response assessment studies were repeated in identical fashion.
Data analysis
After the 24-hour recording period, each monitor was downloaded to a computer (Spacelabs 90121, version 1.1; Spacelabs). Only ABP data that contained 70% acceptable readings were used for analysis, and no more than 24 hours of readings were included. Hourly BP averages were calculated from the readings taken within each hour. Although participants with abnormal self-reported sleep cycles (night-shift workers) were eligible to participate fully in PEAR, they were excluded from this analysis. Daytime and nighttime SBP and DBP were calculated as the mean of the hourly SBP and DBP values between 6:00 am and 10:00 pm and 10:00 pm and 6:00 am, respectively. Mean ± SE of hourly SBP and DBP for the 24-hour, the day, and the night period were determined at each study visit, and the change in SBP and DBP from baseline and from the previous visit within each treatment was analyzed.
Baseline characteristics are presented as the mean ± SE and were compared between race, sex, and initial drug therapy groups using t tests or χ2 tests. Significant P values are provided and presented to no lower than P < 0.01. P values <0.10 and >0.05 are also provided. Race and sex differences for each hour were tested using mixed-model repeated measures analysis of variance (ANOVA). At each time point, whites and blacks were compared. Bonferroni adjustments were made to take into account the 24 comparisons that were done. One-way ANOVA was used to determine race and sex differences in the SBP and DBP response from baseline in each treatment and for each time period. Bonferroni post hoc methods were used to test whether there was a change from previous treatment period that contributed to the subsequent BP response within each sex and race group.34 Change in SBP and DBP from the previous treatment period was compared between men and women within race and between blacks and whites within sex using similar Bonferroni methods. The potential effect of order of drug treatment and the interaction between gender and sex and order of treatment were investigated using a 2-way ANOVA.
Night/day BP ratio means ± SEs were evaluated at each treatment period and stratified by drug treatment and race. A mixed-model repeated measures ANOVA was used to compare the means between study visits within treatment and race. Tukey’s post hoc procedures were used when indicated.34 SAS version 9.2 (Cary, NC) was used for all statistical analyses.
Pearson correlations were used to investigate the associations between the change in SBP and DBP from baseline and from the previous visit within each treatment vs. demographic, body size, environmental exposures, biochemical, hematological, and hormonal variables obtained during PEAR visits. Variables with P values <0.10 were then entered into stepwise linear regression models. Given the known different impact of sex and race on BP response to the 2 classes of antihypertensive agents studied, these covariables were included in all models. Other potential variables for change from baseline were the corresponding baseline SBP or DBP values for change from baseline or monotherapy to combination therapy. Individual variables were entered into the final model if their P values were <0.05, and variables were removed if their P values were >0.05. R 2 values and the magnitude of contribution of each variable were included in each model. Total R 2 values for both day and night SBP, DBP, and night/day ratio responses were compared between groups starting therapy with HCTZ vs. ATEN. The differences in the R 2 and the SE of the differences were calculated. The ratio of the difference/SE was estimated, and a P value was calculated.35
RESULTS
Baseline assessment
Four hundred eighty-five of 810 PEAR participants (69%) successfully completed all ABP measures. Of these, 41 were shift workers, and 21 reported ethnicity as not white or black, leaving 485 (60%) participants available for this analysis. Two hundred four (42%) were black (148 (73%) women; 56 (27%) men), and 281 (58%) were white (125 (44%) women; 156 (56%) men). Of the participants, 92.6% received maximum doses of the first drug (HCTZ or ATEN), and 76.2% reached maximum dose of the second, add-on drug.
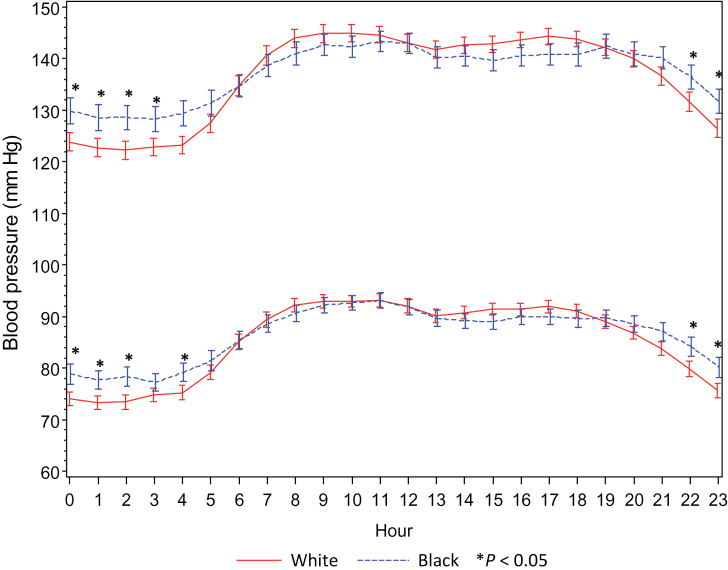
Baseline 24-hour, day, and night BPs were similar between groups randomized to initially receive HCTZ vs. ATEN (Table 1). Weight, waist circumference, and waist/hip ratios were significantly different in men vs. women (Table 1). Night and night/day SBP and DBP ratios were significantly greater in blacks vs. whites, and dipping status was less frequent in blacks. Mean hourly night and day SBP and DBP differed significantly in blacks vs. whites. Blacks demonstrated greater night SBP and DBP vs. whites (Figure 1), accounting for the differences in night/day BP ratios seen between races. White and black women demonstrated significantly lower night SBP and DBP vs. men (data not shown).
Table 1.
Baseline characteristics of male and female and white and black Pharmacogenomic Evaluation of Antihypertensive Responses study participants randomized to initial treatment with atenolol or hydrochlorothiazide
| Characteristic | Male (n = 212) | Female (n = 273) | P value male vs. female | White (n = 281) | Black (n = 204) | P value white vs. black |
|---|---|---|---|---|---|---|
| Age, y | 49.7±0.6 | 49.4±0.5 | 0.71 | 50.5±0.6 | 48.2±0.6 | <0.01 |
| Duration hypertension, y | 6.5±0.5 | 7.0±0.4 | 0.47 | 6.8±0.4 | 6.7±0.5 | 0.84 |
| SBP 24h, mm Hg | 138±0.7 | 139±0.7 | 0.42 | 139±0.6 | 139±0.8 | 0.96 |
| DBP 24h, mm Hg | 88±0.6 | 87±0.5 | 0.55 | 87±0.5 | 88±0.5 | 0.45 |
| SBP day, mm Hg | 141±0.8 | 142±0.7 | 0.33 | 142±0.6 | 141±0.8 | 0.31 |
| DBP day, mm Hg | 90±0.6 | 90±0.5 | 0.80 | 90±0.5 | 90±0.5 | 0.88 |
| SBP night, mm Hg | 127±0.9 | 127±0.8 | 0.73 | 125±0.7 | 130±1.0 | <0.01 |
| DBP night, mm Hg | 78±0.7 | 77±0.6 | 0.25 | 75±0.5 | 79±0.7 | <0.01 |
| Dipper, No. (%) | 102 (50.5) | 143 (52.4) | 0.68 | 171 (62.6) | 74 (36.6) | <0.01 |
| SBP ratio | 0.90±0.01 | 0.90±0.00 | 0.83 | 0.88±0.00 | 0.92±0.00 | <0.01 |
| DBP ratio | 0.86±0.01 | 0.86±0.01 | 0.42 | 0.84±0.01 | 0.88±0.01 | <0.01 |
| Weight, kg | 96.3±1.0 | 83.5±1.1 | <0.01 | 88.9±1.0 | 89.1±1.3 | 0.91 |
| BMI, m2 | 30.8±0.3 | 31.1±0.4 | 0.54 | 30.4±0.3 | 31.7±0.4 | 0.02 |
| Waist circumference, cm | 102.7±0.8 | 94.9±0.8 | <0.01 | 98.7±0.8 | 97.6±0.9 | 0.39 |
| Hip circumference, cm | 109.4±0.6 | 112.4±0.8 | <0.01 | 109.2±0.6 | 113.8±0.9 | <0.01 |
| Waist/hip ratio | 0.94±0.00 | 0.85±0.00 | <0.01 | 0.90±0.00 | 0.86±0.01 | <0.01 |
| Reached menopause, No. (%) | NA | 156 (56.7) | NA | 71 (55.0) | 85(58.2) | 0.60 |
Data are mean +/- SE unless otherwise noted. Bolded values indicate P values <0.05.
Abbreviations: BMI, body mass index; DBP, diastolic blood pressure; NA, not applicable; SBP, systolic blood pressure.
Figure 1.
Hourly mean systolic and diastolic baseline blood pressures in 281 white and 204 black Pharmacogenomic Evaluation of Antihypertensive Responses study participants. Hourly mean values that are significantly different across race are shown with an asterisk (P < 0.05).
At baseline, men and whites demonstrated a significantly greater frequency of alcohol exposure, had greater serum potassium, magnesium, and triglyceride concentrations, and had greater plasma renin activity than women and blacks. They also demonstrated significantly lower platelet counts and lower high-density lipoprotein levels (P < 0.01) (Table 2).
Table 2.
Baseline clinical variables tested as potential covariables with regard to nighttime systolic and diastolic blood pressure response to atenolol and hydrochlorothiazide in white and black Pharmacogenomic Evaluation of Antihypertensive Responses study participants randomized to initial treatment with atenolol or hydrochlorothiazide
| Characteristic | Male (n = 212) | Female (n = 273) | P value male vs. female | White (n = 281) | Black (n = 204) | P value white vs. black |
|---|---|---|---|---|---|---|
| Any exercise, no. (%) | 134 (64.4) | 186 (67.1) | 0.53 | 182 (64.8) | 138 (67.6) | 0.51 |
| Any drink, no. (%) | 156 (75.0) | 182 (65.7) | 0.03 | 224 (79.7) | 114 (55.9) | <0.01 |
| Any cigarettes, no. (%) | 93 (44.9) | 86 (31.2) | <0.01 | 113 (40.5) | 66 (32.4) | 0.07 |
| Serum creatinine, mg/dl | 1.01±0.01 | 0.82±0.01 | <0.01 | 0.91±0.01 | 0.88±0.01 | 0.10 |
| eGFR, ml/min | 92.2±1.6 | 91.5±1.3 | 0.74 | 85.9±1.2 | 100.1±1.6 | <0.01 |
| Sodium, mEq/L | 139.8±0.2 | 140.1±0.1 | 0.19 | 140.3±0.1 | 139.5±0.2 | <0.01 |
| Potassium, mEq/L | 4.32±0.03 | 4.11±0.03 | <0.01 | 4.30±0.02 | 4.07±0.03 | <0.01 |
| Magnesium, mg/dl | 2.12±0.02 | 2.00±0.02 | <0.01 | 2.19±0.01 | 1.86±0.02 | <0.01 |
| Serum uric acid, mg/dl | 6.32±0.09 | 4.91±0.07 | <0.01 | 5.57±0.08 | 5.43±0.10 | 0.28 |
| Hemoglobin, g/L | 15.1±0.1 | 13.2±0.1 | <0.01 | 14.6±0.1 | 13.3±0.1 | <0.01 |
| WBC, 1,000/cc3 | 5.8±3.1 | 5.8 ± .38 | 0.87 | 6.6 ± .34 | 4.7 ± .47 | <0.01 |
| Platelets, 1,000/cc3 | 254±4.1 | 289±4.1 | <0.01 | 264±3.7 | 288±4.9 | <0.01 |
| Serum Glucose, mg/dl | 94.3±0.8 | 89.6±0.7 | <0.01 | 92.3±0.7 | 90.8±0.9 | 0.19 |
| Insulin, IU | 9.56±0.63 | 8.86±0.53 | 00.39 | 8.58±0.41 | 9.96±0.78 | 0.09 |
| HOMA | 2.36±0.19 | 2.08±0.16 | 00.27 | 2.04±0.12 | 2.43±0.24 | 0.12 |
| Plasma renin activity, ng/dl/min | 1.13±0.09 | 0.88±0.07 | <0.01 | 1.28±0.09 | 0.58±0.04 | <0.01 |
| HDL, mg/dl | 45.3±0.9 | 53.4±0.8 | <0.01 | 48.9±0.8 | 51.4±1.0 | 0.06 |
| LDL, mg/dl | 120.7±2.2 | 119.7±1.8 | 0.73 | 118.0±1.7 | 123.1±2.4 | 0.07 |
| Total cholesterol, mg/dl | 194.5±2.5 | 195.1±2.1 | 0.85 | 194.9±2.0 | 194.7±2.7 | 0.96 |
| Serum triglycerides, mg/dLl | 142.1±7.6 | 109.5±4.4 | <0.01 | 139.6±5.5 | 101.2±6.1 | <0.01 |
Data are mean +/- SE unless otherwise noted. Bolded values indicate P values <0.05.
Abbreviations: eGFR, estimated glomerular filatration rate; HDL, high-density lipoprotein; HOMA, homeostasis model assessment; LDL, low-density lipoprotein; WBC, white blood cell.
BP responses to ATEN and HCTZ monotherapy
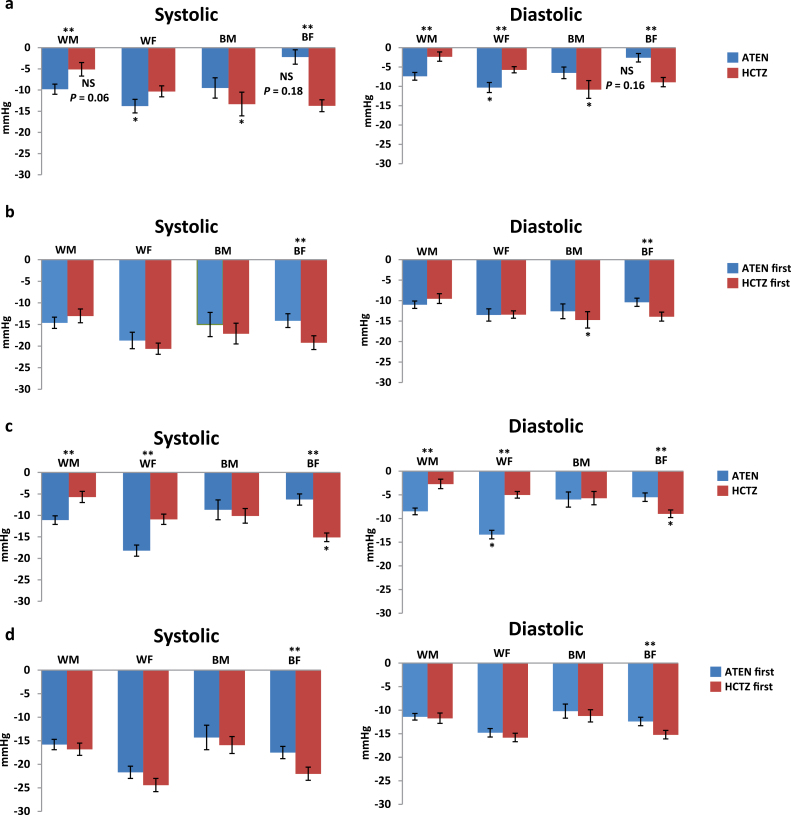
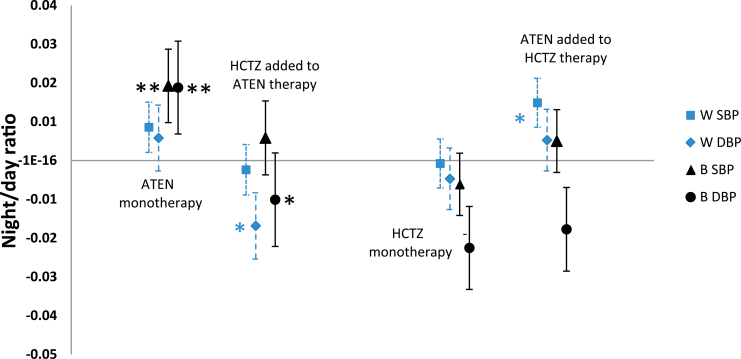
There was no significant night SBP (P = 0.18) or DBP (P = 0.16) response to ATEN monotherapy in black women (Figure 2a); however, a significant day SBP and DBP response to ATEN was seen in all race and sex subgroups (Figure 2b). A significant increase in night/day SBP and DBP ratio after ATEN therapy was seen in blacks (SBP = 0.95±0.01 vs. 0.92±0.01; DBP = 0.89±0.01 vs. 0.87±0.01; P < 0.05) (Figure 3). Whites demonstrated significant night and day SBP and DBP responses to ATEN (Figure 2a,b), with no change in night/day BP ratios (Figure 3). Black men demonstrated signficantly lower night SBP and DBP response to ATEN than white men (Figure 2a), and overall blacks demonstrated significantly less night BP response to ATEN than whites (P < 0.01). Dipping status was unchanged with ATEN monotherapy in all race and sex subgroups (data not shown).
Figure 2.
Systolic and diastolic blood pressure response to atenolol (ATEN) and hydrochlorothiazide (HCTZ) monotherapy and combined therapy in white (W) and black (B) male (M) and female (F) Pharmacogenomic Evaluation of Antihypertensive Responses study participants. (a) Nighttime monotherapy. (b) Nighttime combined therapy. (c) Daytime monotheraphy. (d) Daytime combined therapy. *P <0.05 between whites and blacks. **P < 0.05 between ATEN and HCTZ treatment within a race/sex subgroup. Abbreviation: NS, not significant.
Figure 3.
Change in night/day systolic blood pressure (SBP) and diastolic blood pressure (DBP) ratios after each step of drug therapy in white (W) and black (B) Pharmacogenomic Evaluation of Antihypertensive Responses study participants. Night/day SBP and DBP ratios were determined using mean night BP values divided by mean day BP values. *P < 0.05 for add-on theraphy vs. end of monotherapy. **P < 0.05 for atenolol monotherapy vs. baseline. Abbreviations: ATEN, atenolol; HCTZ, hydrochlorothiazide.
Variability (R2) of night BP and night/day ratio BP responses to ATEN (R2 = 0.21 -0.36) accounted for significantly less than for HCTZ (R 2 = 0.45–0.53; P < 0.05) (Supplementary Table S3a). White women demonstrated the greatest and black women the least night SBP and DBP response to ATEN. Increased baseline plasma renin activity was associated with a greater night SBP and DBP response to ATEN. Variables that were associated with day BP response to ATEN did not differ from those associated with night BP response (Supplementary Table 3b).
There was a significantly greater night SBP and DBP response to HCTZ in black men than in white men (P < 0.05) (Figure 2a), but men of both races had similar day SBP and DBP responses. White men failed to demonstrate a significant night DBP response to HCTZ (P = 0.06). Black and white women demonstrated similar night BP response to HCTZ; however, SBP and DBP responses during the day were greater in black women than in white women (P < 0.05) (Figure 2b). SBP and DBP night/day ratio responses and dipping status did not change with HCTZ therapy. Variables associating with night BP response to HCTZ differed from those associating with day BP response. (Supplementary Table 3a,b). The overall R 2 (0.53) accounted for in night BP responses was significantly greater than accounted for in day BP responses(R 2= 0.38–0.41; P < 0.05) (Supplementary Table 3a,b).
BP responses to ATEN and HCTZ add-on therapy
Serum magnesium concentration, race, estimated glomerular filtration rate, cigarette exposure, and platelet count accounted for night HCTZ add-on BP response, whereas only baseline BP contributed to night ATEN add-on BP response (Supplementary Table 3c). The increased night/day SBP and DBP ratios after ATEN monotherapy in blacks decreased significantly (P < .05) with HCTZ add-on therapy (Figure 3). Different variables accounted for night vs. day add-on BP response, with age contributing to the ATEN add-on day BP response and increased waist/hip ratio contributing to the day HCTZ BP response (Supplementary Table 3c,d).
BP response to combination therapy
At the end of combination therapy, blacks demonstrated an overall greater night SBP and DBP response when they initiated therapy with HCTZ vs. ATEN (P < 0.05) (Figure 2c,d). No changes were seen with regard to dipping frequency or night/day SBP and DBP ratios at the end of combination therapy compared with baseline. Those initiating therapy with HCTZ first had the greatest overall night SBP and DBP response (SBP = Δ3.2mm Hg, HCTZ vs. ATEN first; DBP = Δ4.1mm Hg, HCTZ vs. ATEN first; P < 0.01).
The variables contributing to the BP response differed by drug and night vs. day, with alcohol exposure significant for those starting with HCTZ and white blood cell count significant for those starting with ATEN (Supplementary Table 3e,f). Importantly, black race contributed significantly to night SBP response to combination therapy. Night DBP response variability accounted for combined ATEN/HCTZ therapy (R 2 = 0.49) was significantly greater than day DBP response variability (R 2 = 0.27; P < 0.01).
DISCUSSION
Night BP carries prognostic information in essential hypertensive patients. This study provides new data from a large (n = 485) biracial population of essential hypertensive patients who successfully underwent 3 ABP recordings. In this study, we focused on the night and night/day ratio SBP and DBP response to 2 classes of antihypertensive agents commonly prescribed: thiazide diuretics and β-blockers. In contrast with studies where the frequency of nocturnal dipping was evaluated as a measure of a favorable night response to antihypertensive agents, we chose to evaluate night/day SBP and DBP ratio response. By using this approach we were able to avoid the inconsistent categorical classification of dipping vs. nondipping status, and we evaluated the impact of antihypertensive therapy in a continuous fashion on night vs. day BP responses.
A number of clinically relevant and important observations were obtained from this study. ATEN therapy induced a significant increase in night/day SBP and DBP ratios in blacks. A similar increase in night/day ratio BP response with ATEN has been reported in a smaller study involving primarily blacks.36 Importantly, at the end of combination therapy, night/day SBP and DBP ratios were not different from baseline. Other studies evaluating the effects of timing of antihypertensive medication administration have shown an improvement in dipping status when angiotensin-converting enzyme inhibitors and angiotensin receptor blocking agents are administered in the evening before bedtime.10 The lack of improvement in night/day BP ratio by the end of 18 weeks of treatment in this study suggests that improvement in night/day BP ratios require either a longer duration of therapy, different antihypertensive agents, or most likely a different time of medication administration. It is possible that potential improvement in night/day BP ratios due to HCTZ were masked by the administration of ATEN.
Given that β-blockers inhibit the renin-angiotensin aldosterone system and that angiotensin-converting enzyme inhibitors and angiotensin receptor blocking agents have both been shown to reduce night as compared with day BP, other factors, including possibly increased nighttime sodium retention, are selectively affected by ATEN therapy. Given that ATEN has a relatively short half-life and it was administered once a day in this study, the increased night/day BP ratios observed might be eliminated with more frequent dosing in a 24-hour period or with administration of a longer acting β-blocker. However, both heart rate and morning plasma renin activity were affected by ATEN administration, indicating that the pharmacokinetic profile of ATEN is not the only contributing factor to the changes in night/day BP ratios seen. Whether the increase in night/day BP ratio found with ATEN is a drug class effect related to all β-blockers is unclear. However, given that night BP and night/day BP ratios have significant prognostic impact with regard to patient outcome,37 the potential negative impact of ATEN deserves further evaluation.
Differences in night BP responses to ATEN vs. HCTZ were seen between whites and blacks.38,39 In addition, the variability of the BP response accounted for was significantly greater with HCTZ vs. ATEN and with night vs. day responses. The order of drug administration contributed to the magnitude of the BP response at the end of combination therapy, with those starting with HCTZ demonstrating the greatest BP response. It is important to note that those receiving HCTZ first received this drug for 18 weeks, whereas those who were given HCTZ as add on therapy were exposed for 9 weeks. It is possible that HCTZ-specific changes in total body sodium or vascular smooth muscle intracellular calcium concentrations accrue over a longer period of time.
A significantly greater night BP response to ATEN was found in whites, and a greater night BP response to HCTZ was found in blacks. Importantly, there was no significant night BP response found in black women receiving ATEN and in white men receiving HCTZ (P = 0.06). This was in contrast to significant day BP responses found. Previous studies have demonstrated a greater day vs. night SBP and DBP response to the calcium channel blockers verapamil and amlodipine in women.26 In our previous work, women demonstrated greater office BP response vs. men; however, differences in day vs. night response were not evaluated.40
Increased night BP or night/day BP ratios associate with social stressors, quality of sleep, and movement-related disorders at night.10,41 During this study, no assessment of sleep quality was obtained; however, variables were identified that associated with night and night/day BP ratio responses (Supplementary Tables). Importantly, day and night BP responses associated with different variables. These differences highlight potential areas for therapeutic interventions through both timing of medication administration and lifestyle modifications.
In summary, night/day BP ratios and night SBP and DBP response to therapy differ across race and sex and are affected by the class and order of antihypertensive drug administration. Traditional variables such as baseline BP accounted for a significant portion of the variability of all BP responses, whereas specific variables were associated with the class of antihypertensive agent administered and with night vs. day BP responses, elucidating potential strategies to maximize 24-hour BP responses to antihypertensive medications. Importantly, reduced night BP response to ATEN therapy resulted in an increase in night/day BP ratios, which may negatively impact patient outcomes.37 Our data suggest that evaluation of the night BP period with regard to response to antihypertensive agents provides valuable and clinically relevant information and will help to address issues contributing to the patient outcomes related to hypertension.
SUPPLEMENTARY MATERIAL
Supplementary materials are available at American Journal of Hypertension (http://ajh.oxfordjournals.org).
DISCLOSURE
The authors declared no conflict of interest.
Supplementary Material
ACKNOWLEDGMENTS
We acknowledge and thank the valuable contributions of the study participants, support staff, and study physicians: Drs George Baramidze, Carmen Bray, Kendall Campbell, R. Whit Curry, Karen Hall, Frederic Rahbari-Oskoui, Vishal Parekh, Dan Rubin, and Siegfried Schmidt. This work was supported by a grant from the National Institutes of Health (U01 GM074492), funded as part of the Pharmacogenetics Research Network. Additionally this work was supported by grants from the National Institutes of Health, National Center for Research Resources (UL1 RR029890 and M01 RR00082 to the University of Florida; UL1 RR025008 and M01 RR00039 to Emory University; and UL1 RR024150 to Mayo Clinic). The study sponsors had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. A.B.C. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1. White WB, Schulman P, McCabe EJ, Dey HM. Average daily blood pressure, not office blood pressure, determines cardiac function in patients with hypertension. JAMA 1989; 261:873–877 [PubMed] [Google Scholar]
- 2. Hansen TW, Jeppesen J, Rasmussen S, Ibsen H, Torp-Pedersen C. Ambulatory blood pressure and mortality: a population-based study. Hypertension 2005; 45:499–504 [DOI] [PubMed] [Google Scholar]
- 3. Verdecchia P, Reboldi G, Porcellati C, Schillaci G, Pede S, Bentivoglio M, Angeli F, Norgiolini S, Ambrosio G. Risk of cardiovascular disease in relation to achieved office and ambulatory blood pressure control in treated hypertensive subjects. J Am Coll Cardiol 2002; 39:878–885 [DOI] [PubMed] [Google Scholar]
- 4. Staessen JA, Thijs L, Fagard R, O’Brien ET, Clement D, de Leeuw PW, Mancia G, Nachev C, Palatini P, Parati G, Tuomilehto J, Webster J. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Systolic Hypertension in Europe Trial Investigators. JAMA 1999; 282:539–546 [DOI] [PubMed] [Google Scholar]
- 5. Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, De Bacquer DA. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension 2008; 51:55–61 [DOI] [PubMed] [Google Scholar]
- 6. Harshfield GA, Wilson ME, Treiber FA, Alpert BS. A comparison of ambulatory blood pressure patterns across populations. Blood Press Monit 2002; 7:265–269 [DOI] [PubMed] [Google Scholar]
- 7. Clement DL, De Buyzere ML, De Bacquer DA, de Leeuw PW, Duprez DA, Fagard RH, Gheeraert PJ, Missault LH, Braun JJ, Six RO, Van Der Niepen P, O’Brien E. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med 2003; 348:2407–2415 [DOI] [PubMed] [Google Scholar]
- 8. Redon J, Campos C, Narciso ML, Rodicio JL, Pascual JM, Ruilope LM. Prognostic value of ambulatory blood pressure monitoring in refractory hypertension: A prospective study. Hypertension 1998; 31:712–718 [DOI] [PubMed] [Google Scholar]
- 9. White WB. Ambulatory blood pressure monitoring: dippers compared with non-dippers. Blood Press Monit 2000; 5:S17–S23 [PubMed] [Google Scholar]
- 10. Hermida RC, Ayala DE, Fernandez JR, Portaluppi F, Fabbian F, Smolensky MH. Circadian rhythms in blood pressure regulation and optimization of hypertension treatment with ACE inhibitor and ARB medications. Am J Hypertens 2011; 24:383–391 [DOI] [PubMed] [Google Scholar]
- 11. Lo SH, Liau CS, Hwang JS, Wang JD. Dynamic blood pressure changes and recovery under different work shifts in young women. Am J Hypertens 2008; 21:759–764 [DOI] [PubMed] [Google Scholar]
- 12. Routledge FS, McFetridge-Durdle JA, Dean CR. Night-time blood pressure patterns and target organ damage: a review. Can J Cardiol 2007; 23:132–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Portaluppi F, Montanari L, Massari M, Di Chiara V, Capanna M. Loss of nocturnal decline of blood pressure in hypertension due to chronic renal failure. Am J Hypertens 1991; 4:20–26 [DOI] [PubMed] [Google Scholar]
- 14. van Berge-Landry HM, Bovbjerg DH, James GD. Relationship between waking-sleep blood pressure and catecholamine changes in African-American and European-American women. Blood Press Monit 2008; 13:257–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pogue V, Rahman M, Lipkowitz M, Toto R, Miller E, Faulkner M, Rostand S, Hiremath L, Sika M, Kendrick C, Hu B, Greene T, Appel L, Phillips RA. Disparate estimates of hypertension control from ambulatory and clinic blood pressure measurements in hypertensive kidney disease. Hypertension 2009; 53:20–27 [DOI] [PubMed] [Google Scholar]
- 16. Uzu T, Kazembe FS, Ishikawa K, Nakamura S, Inenaga T, Kimura G. High sodium sensitivity implicates nocturnal hypertension in essential hypertension. Hypertension 1996; 28:139–142 [DOI] [PubMed] [Google Scholar]
- 17. James GD. Race and perceived stress independently affect the diurnal variation of blood pressure in women. Am J Hypertens 1991; 4:382–384 [DOI] [PubMed] [Google Scholar]
- 18. Jamerson KA. The disproportionate impact of hypertensive cardiovascular disease in African Americans: getting to the heart of the issue. J Clin Hypertens (Greenwich) 2004; 6:4–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Appel LJ, Wright JT, Jr, Greene T, Kusek JW, Lewis JB, Wang X, Lipkowitz MS, Norris KC, Bakris GL, Rahman M, Contreras G, Rostand SG, Kopple JD, Gabbai FB, Schulman GI, Gassman JJ, Charleston J, Agodoa LY. Long-term effects of renin-angiotensin system-blocking therapy and a low blood pressure goal on progression of hypertensive chronic kidney disease in African Americans. Arch Intern Med 2008; 168:832–839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pathak EB, Sloan MA. Recent racial/ethnic disparities in stroke hospitalizations and outcomes for young adults in Florida, 2001–2006. Neuroepidemiology 2009; 32:302–311 [DOI] [PubMed] [Google Scholar]
- 21. Harshfield GA, Treiber FA, Wilson ME, Kapuku GK, Davis HC. A longitudinal study of ethnic differences in ambulatory blood pressure patterns in youth. Am J Hypertens 2002; 15:525–530 [DOI] [PubMed] [Google Scholar]
- 22. Gretler DD, Fumo MT, Nelson KS, Murphy MB. Ethnic differences in circadian hemodynamic profile. Am J Hypertens 1994; 7:7–14 [DOI] [PubMed] [Google Scholar]
- 23. Sherwood A, Steffen PR, Blumenthal JA, Kuhn C, Hinderliter AL. Nighttime blood pressure dipping: the role of the sympathetic nervous system. Am J Hypertens 2002; 15:111–118 [DOI] [PubMed] [Google Scholar]
- 24. Kotsis V, Stabouli S, Pitiriga V, Papamichael C, Toumanidis S, Zakopoulos N. Impact of gender on 24-h ambulatory blood pressure and target organ damage. J Hum Hypertens 2006; 20:658–665 [DOI] [PubMed] [Google Scholar]
- 25. Kagan A, Faibel H, Ben-Arie G, Granevitze Z, Rapoport J. Gender differences in ambulatory blood pressure monitoring profile in obese, overweight and normal subjects. J Hum Hypertens 2007; 21:128–134 [DOI] [PubMed] [Google Scholar]
- 26. Banegas JR, Segura J, de la Sierra A, Gorostidi M, Rodriguez-Artalejo F, Sobrino J, de la Cruz JJ, Vinyoles E, del Rey RH, Graciani A, Ruilope LM. Gender differences in office and ambulatory control of hypertension. Am J Med 2008; 121:1078–1084 [DOI] [PubMed] [Google Scholar]
- 27. de la Sierra A, Redon J, Banegas JR, Segura J, Parati G, Gorostidi M, de la Cruz JJ, Sobrino J, Llisterri JL, Alonso J, Vinyoles E, Pallares V, Sarria A, Aranda P, Ruilope LM. Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension 2009; 53:466–472 [DOI] [PubMed] [Google Scholar]
- 28. Khoury S, Yarows SA, O’Brien TK, Sowers JR. Ambulatory blood pressure monitoring in a nonacademic setting. Effects of age and sex. Am J Hypertens 1992; 5:616–623 [DOI] [PubMed] [Google Scholar]
- 29. Uzu T, Kimura G. Diuretics shift circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation 1999; 100:1635–1638 [DOI] [PubMed] [Google Scholar]
- 30. Gatzka CD, Schobel HP, Klingbeil AU, Neumayer HH, Schmieder RE. Normalization of circadian blood pressure profiles after renal transplantation. Transplantation 1995; 59:1270–1274 [PubMed] [Google Scholar]
- 31. Cuspidi C, Meani S, Salerno M, Valerio C, Fusi V, Severgnini B, Lonati L, Magrini F, Zanchetti A. Reproducibility of nocturnal blood pressure fall in early phases of untreated essential hypertension: a prospective observational study. J Hum Hypertens 2004; 18:503–509 [DOI] [PubMed] [Google Scholar]
- 32. Beitelshees AL, Gong Y, Bailey KR, Turner ST, Chapman AB, Schwartz GL, Gums JG, Boerwinkle E, Johnson JA. Comparison of office, ambulatory, and home blood pressure antihypertensive response to atenolol and hydrochlorthiazide. J Clin Hypertens (Greenwich) 2010; 12:14–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Johnson JA, Boerwinkle E, Zineh I, Chapman AB, Bailey K, Cooper-DeHoff RM, Gums J, Curry RW, Gong Y, Beitelshees AL, Schwartz G, Turner ST. Pharmacogenomics of antihypertensive drugs: rationale and design of the Pharmacogenomic Evaluation of Antihypertensive Responses (PEAR) study. Am Heart J 2009; 157:442–449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Neter J, Kutner MH, Nachtsheim CJ, Wasserman W. Applied Linear Statistical Models. WCB McGraw-Hill: Boston, 1996. [Google Scholar]
- 35. Olkin I, Finn JD. Correlations redux. Psychol Bull 1995; 118:155–164 [Google Scholar]
- 36. Johnson JA, Akers WS, Miller ST, Applegate WB. Metoprolol minimizes nighttime blood pressure dip in hypertensive black males. Am J Hypertens 1995; 8:254–259 [DOI] [PubMed] [Google Scholar]
- 37. Hermida RC, Ayala DE, Fernandez JR, Mojon A. Sleep-time blood pressure: prognostic value and relevance as a therapeutic target for cardiovascular risk reduction. Chronobiol Int 2013; 30:68–86 [DOI] [PubMed] [Google Scholar]
- 38. Dhakam Z, Yasmin McEniery CM, Burton T, Brown MJ, Wilkinson IB. A comparison of atenolol and nebivolol in isolated systolic hypertension. J Hypertens 2008; 26:351–356 [DOI] [PubMed] [Google Scholar]
- 39. Fuchs FD. Diuretics: still essential drugs for the management of hypertension. Expert Rev Cardiovasc Ther 2009; 7:591–598 [DOI] [PubMed] [Google Scholar]
- 40. Turner ST, Schwartz GL, Chapman AB, Boerwinkle E. C825T polymorphism of the G protein beta(3)-subunit and antihypertensive response to a thiazide diuretic. Hypertension 2001; 37:739–743 [DOI] [PubMed] [Google Scholar]
- 41. Tomfohr L, Cooper DC, Mills PJ, Nelesen RA, Dimsdale JE. Everyday discrimination and nocturnal blood pressure dipping in black and white americans. Psychosom Med 2010; 72:266–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.