Abstract
Purpose
To assess current practice patterns for dry eye patients in South Korea and to evaluate the preference according to the ages and clinic types of physicians.
Methods
Dry eye patients (n = 1,612) were enrolled in this multicenter cross-sectional, observational study. The severity level of dry eye patients was classified based on the Korean guidelines for dry eye treatment. The medical records of the enrolled dry eye patients were evaluated, and the practice styles and the preferences were analyzed according to the ages and clinic types of physicians.
Results
Of all patients, dry eye level 1 was most common (47.5%), followed by level 2 (33.5%), level 3 (9.1%), and level 4 (1.1%). Topical anti-inflammatory agents were used in 70.7% of patients with dry eye level 2 and in 80.6% of patients at levels 3 and 4. Topical anti-inflammatory agents were also used in 48.7% of patients with dry eye level 1. Preservative-free artificial tears were preferred at all dry eye levels. The use of topical anti-inflammatory agents did not differ with investigator ages, but older physicians preferred preserved artificial tears more than younger ones. Physicians at referral hospitals also tended to use topical anti-inflammatory agents and preservative-free artificial tears earlier, beginning at dry eye level 1, than those who worked at private eye clinics.
Conclusions
Topical anti-inflammatory agents were commonly prescribed for the treatment of dry eye patients in South Korea, even from dry eye level 1. Preservative-free artificial tears were preferred at all dry eye levels. Practice styles differed somewhat depending on the ages and clinic types of physicians.
Keywords: Anti-inflammatory agents, Cyclosporine A, Dry eye syndrome, Practice pattern
As the pathophysiology of dry eye has been established based on many studies, inflammation on the ocular surface is considered to be both a main cause as well as a consequence of dry eye disease [1,2,3,4,5]. Although topical lubricants have traditionally been a popular way to relieve the symptoms of dry eye, topical anti-inflammatory agents are now the method of choice to restore the inflamed ocular surface and to increase the goblet cell density [6,7,8]. The approval of topical cyclosporin by the United States Food and Drug Administration as a therapeutic agent of dry eye and not just a lubricant represented a paradigm shift in the treatment of dry eye. The International Task Force Delphi Panel on Dry Eye and the International Dry Eye WorkShop (DEWS) formulated guidelines for dry eye treatment and recommended the use of topical anti-inflammatory agents from dry eye level 2 [9,10].
Treatment guidelines for dry eye are not strict regulations but rather are useful methods to help physicians treat dry eye patients based on scientific evidence. In general, treatment recommendations are guided by the disease's severity. However, the available treatments for each severity level sometimes fail to relieve symptoms and signs of dry eye in patients. In these cases, treatment recommendations for higher severity levels can be used in clinical practice. Although several treatment guidelines for dry eye patients have been reported so far [9,10,11], little is known regarding the actual clinical practice pattern.
In this study, we assessed the actual clinical practice pattern for dry eye patients in South Korea and analyzed the practice styles and preferences according to the ages and clinic types of physicians.
Materials and Methods
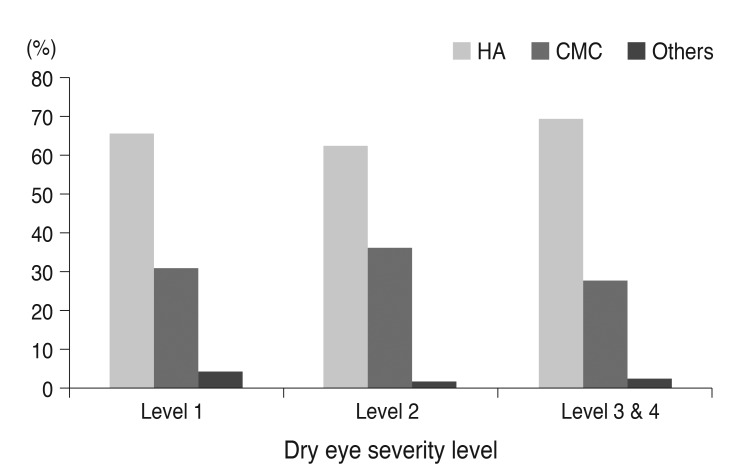
This nonrandomized multicenter study was conducted over a six-month period from March to August 2010. Fifty investigators from 37 institutions who were all cornea specialists participated in this study. Prior to the present study, these investigators established new Korean guidelines for dry eye treatment during a group discussion (Tables 1 and 2). The Korean guidelines were similar to the DEWS guidelines, which were simplified and modified according to the consensus of the Korean investigators. The Korean guidelines gave primary consideration to symptoms and clinical signs, rather than to the results of diagnostic tests. In the event of a discrepancy between symptoms and clinical signs, the severity level was mainly determined by clinical signs, especially corneal staining scores. Patients who complained of dry eye symptoms but had no clinical signs and showed normal results on diagnostic tests were categorized as dry eye suspects.
Table 1.
Dry eye severity grading scheme for Korean dry eye guidelines
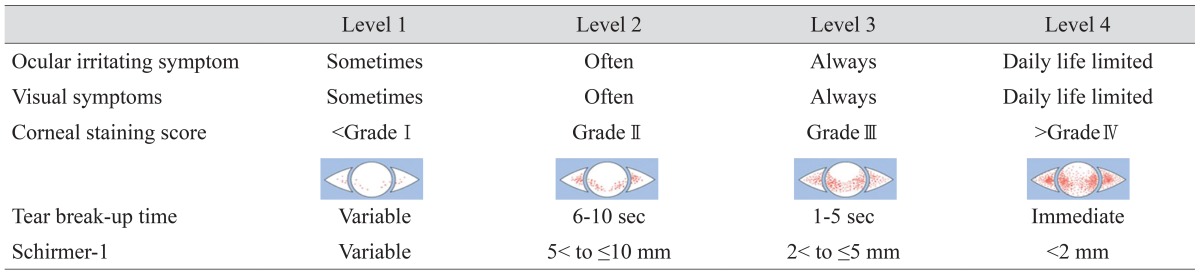
Table 2.
Treatment recommendations at each dry level for Korean dry eye guidelines
During the study period, physicians completed a medical record on each new patient with dry eye who presented to their practices, including information on the severity level and their specific therapy choices. Although treatment decisions were made with reference to the guidelines, physicians were free to recommend any therapy to any particular patient based on their clinical judgment. The medical records of dry eye patients who were treated by one of our investigators during a six-month period were evaluated, and the current practice pattern for each level was analyzed. This study was approved by the respective institutional review boards of the 37 institutions where each investigator worked.
To determine whether the treatment recommendations differed depending on the physicians' ages and clinic types, the use of topical anti-inflammatory eye drops and the choice of artificial tears were evaluated and compared. The age distribution of the investigators was 30 to 39 years (n = 6), 40 to 49 years (n = 20), 50 to 59 years (n = 22), and 60 to 69 years (n = 2). Eight investigators worked at private eye clinics, while the remainder practiced medicine at referral hospitals.
Statistical analyses were performed using Fisher exact test with the SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Results were considered statistically significant if the p-value was less than 0.05.
Results
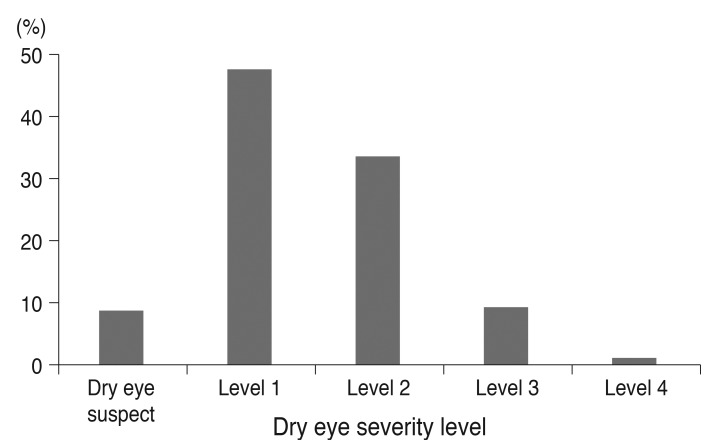
The 50 physicians enrolled 1,612 patients with dry eye during the study period. The mean age of patients was 56.9 (±13.2) years (range, 19 to 85 years), and 81% were female. The distribution of dry eye severity level is shown in Fig. 1. Level 1 was most common (47.5%), followed by level 2 (33.5%), level 3 (9.1%), and level 4 (1.1%). The percentage of dry eye suspects in the study population was 8.8%.
Fig. 1.
The distribution of dry eye severity levels.
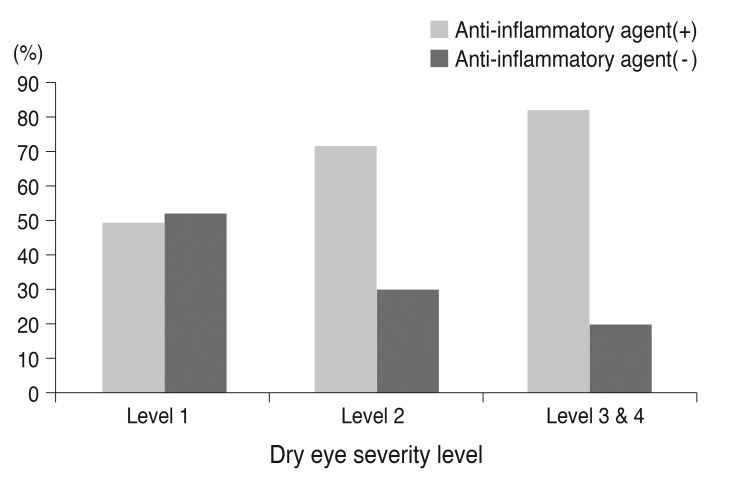
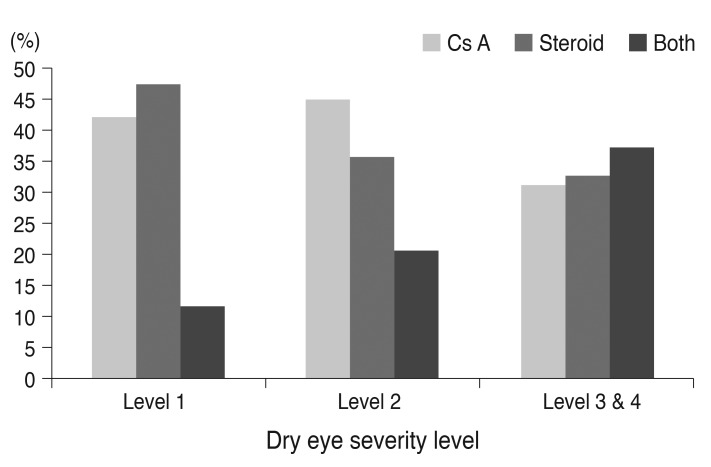
Topical anti-inflammatory agents were used in 70.7% of patients with dry eye level 2 and in 80.6% of patients at levels 3 and 4. Interestingly, topical anti-inflammatory agents were also used in 48.7% of patients with dry eye level 1 even though treatment guidelines recommend the use of topical anti-inflammatory agents only from dry eye level 2 and up (Fig. 2). In patients treated with topical anti-inflammatory agents at level 1, topical steroids were used in 46.9% of cases and 0.05% topical cyclosporine was used in 41.8% of cases. Fluorometholone acetate was the most predominantly used (90.8%) topical steroid; prednisolone acetate was 6.5%, and rimexolone was 2.7%. However, in the patients who were treated with topical anti-inflammatory agents at level 2, 0.05% topical cyclosporine was used in 44.4% of cases, topical steroid agents were given in 35.4%, and both agents were used simultaneously in 20.2%. Among topical steroid agents, fluorometholone acetate was used by 79.7%, while prednisolone acetate was given in 18%; rimexolone made up 2.3%. At levels 3 and 4, the percentage of patients who were treated with both agents increased to 36.9% (Fig. 3).
Fig. 2.
The use of topical anti-inflammatory agents at each dry eye level.
Fig. 3.
Specific choices from topical anti-inflammatory agents at each dry eye level. Cs A = topical cyclosporin.
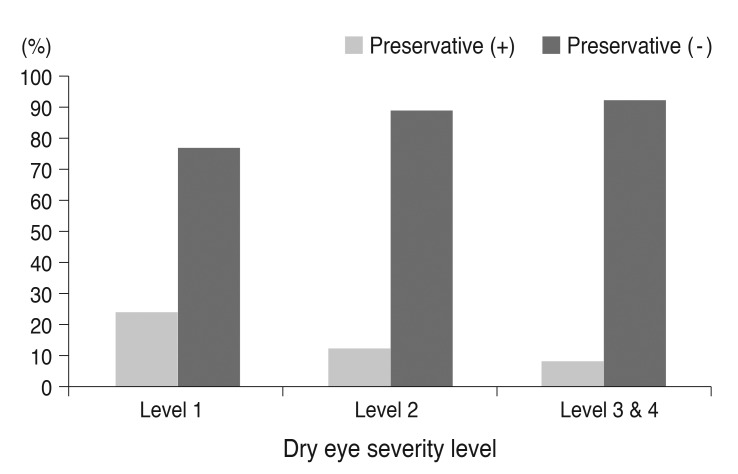
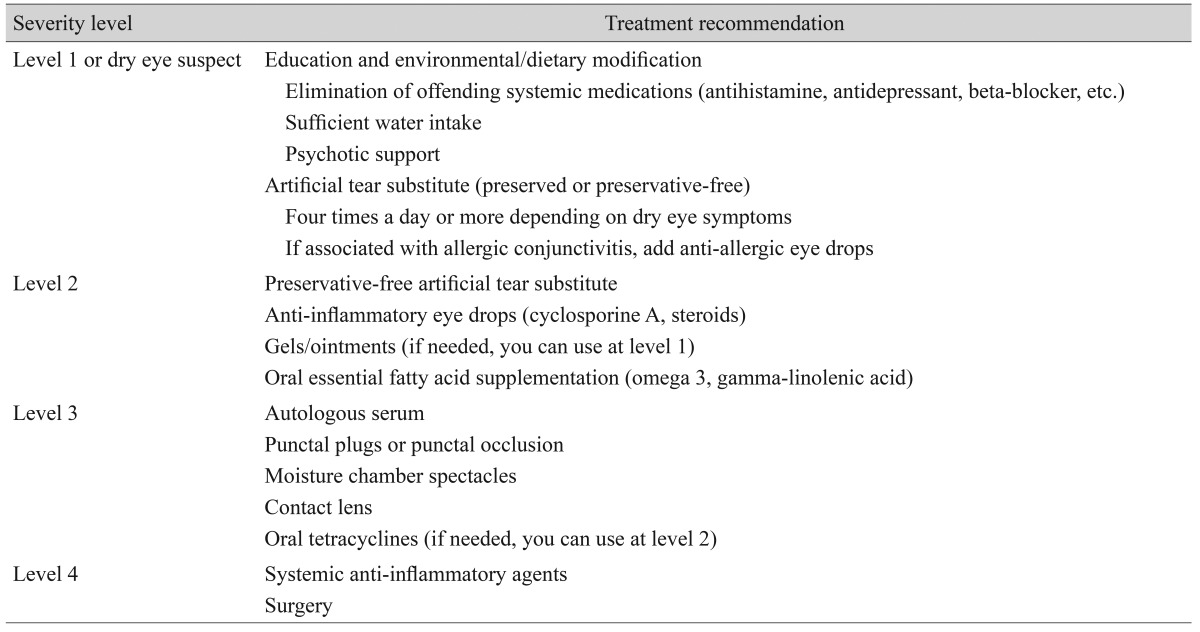
Preservative-free artificial tears were preferred at all dry eye levels (Fig. 4). As the dry eye level increased, the use of preservative-free artificial tears also increased. Preservative-free artificial tears containing 0.1% sodium hyaluronic acid were popular, being used in more than 60% of patients at all dry eye levels (Fig. 5).
Fig. 4.
The use of artificial tears with or without preservatives at each dry eye level.
Fig. 5.
Specific choices from artificial tears at each eye level. HA = hyaluronic acid; CMC = carboxymethylcellulose.
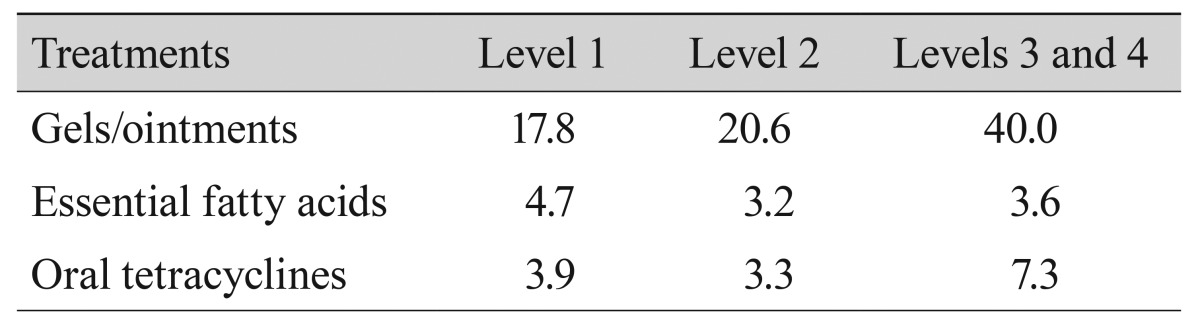
Gels or ointments were prescribed in 17.8% of patients with dry eye level 1, 20.6% of patients with dry eye level 2, and 40% of patients with dry eye levels 3 and 4. Essential fatty acids were recommended in fewer than 5% of patients at all dry eye levels. Additionally, oral tetracyclines were not used very often at dry eye levels 1 and 2, although they were prescribed to 7.3% of patients with dry eye levels 3 and 4 (Table 3).
Table 3.
Percentage of patients treated with gels or ointments, essential fatty acids, and oral tetracyclines at each dry eye level
The percentage of dry eye patients who were treated with topical anti-inflammatory agents was similar at all dry eye levels among the three different physician age groups (Table 4). However, specific therapy choices from topical anti-inflammatory agents did differ significantly among the three age groups (Table 5). Physicians in their 40s tended to use topical cyclosporin more frequently than those in other age groups. The use of preservative-free artificial tears was different at dry eye level 1 and level 2 among the three age groups (Table 6). Physicians in their 50s and 60s were more inclined to use preserved artificial tears than their younger colleagues.
Table 4.
Percentage of patients treated with topical anti-inflammatory agents at each dry eye level according to the age of physicians
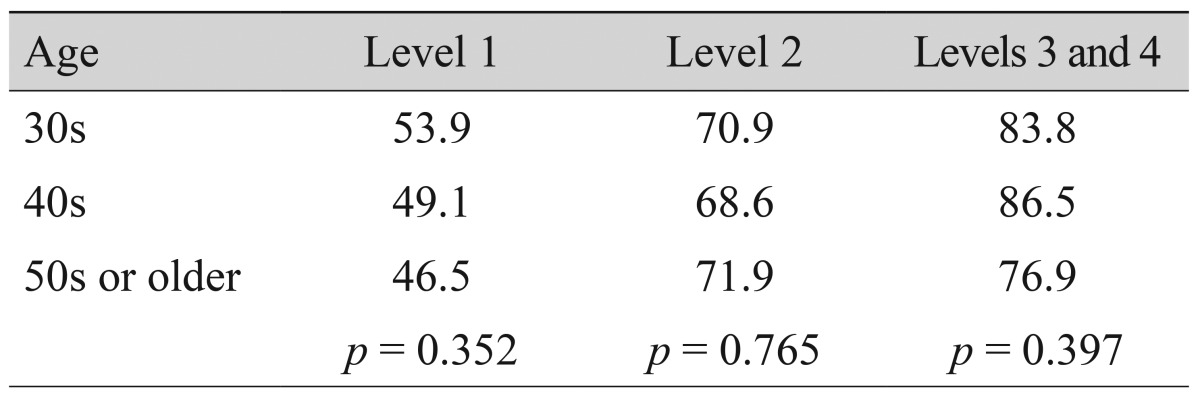
Table 5.
Specific choices for topical anti-inflammatory agents at each dry eye level according to physician age
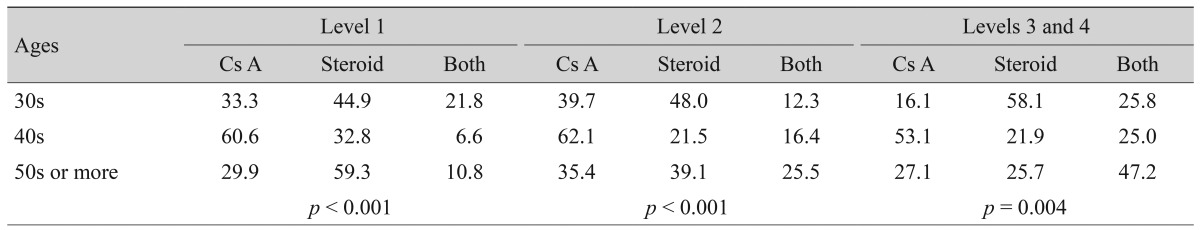
Values are presented as %.
Cs A = topical cyclosporin.
Table 6.
Use of artificial tears at each dry eye level according to physician age
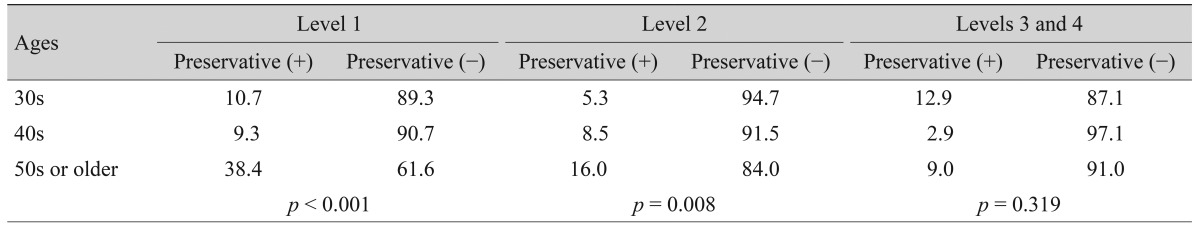
Values are presented as %.
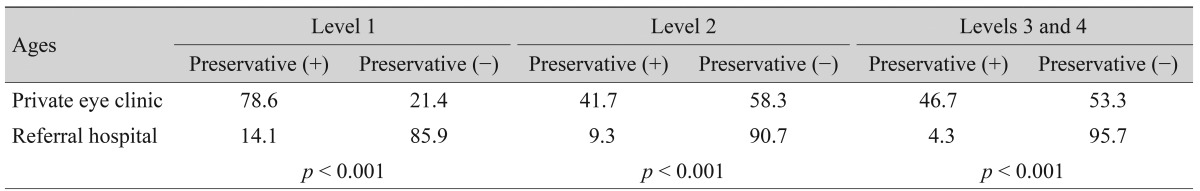
The use of topical anti-inflammatory agents was significantly different at dry eye level 1 and level 2 depending on the clinic type of the participating physicians (Table 7). Physicians who worked at referral hospitals used topical anti-inflammatory agents more frequently than those working at private eye clinics. However, specific therapy choices from topical anti-inflammatory agents were not different. The use of preservative-free artificial tears was significantly different depending on the clinic types of the physicians (Table 8). Physicians working at referral hospitals used preservative-free artificial tears more frequently than those working at private eye clinics.
Table 7.
Use of topical anti-inflammatory agents at each dry eye level according to the clinic types of physicians
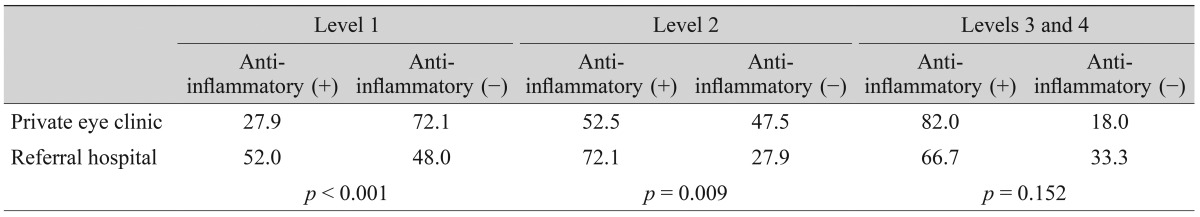
Values are presented as %.
Table 8.
Choice of artificial tears at each dry eye level according to the clinic types of physicians
Values are presented as %.
Discussion
This study is the first multicenter study for dry eye patients in South Korea. Fifty cornea specialists from 37 institutions participated in this study, and 1,612 patients with dry eye were enrolled over a six-month period. The distribution of dry eye severity levels showed a predominance of levels 1 and 2: 81.0% of patients fit into these two groups, with 47.5% for level 1 and 33.5% for level 2. A previous study of 183 enrolled patients with dry eye reported that severity level 2 was most frequent (59%), followed by level 1 (35%) [12]. Although most patients with dry eye were at either level 1 or level 2 in both studies, severity level 1 was most common in our study. Race differences, different severity grading schemes and the relatively small number of patients in the prior study are possible reasons for the discrepancy between the two studies. In the present study, we defined patients who complained of dry eye symptoms but had no clinical signs and no abnormal results of diagnostic tests as dry eye suspects, and they consisted of 8.8% of dry eye patients. Further studies will be needed to determine whether such patients were diagnosed at a very early stage prior to their progression to higher levels.
Although most treatment guidelines for dry eye recommend the use of topical anti-inflammatory agents from dry eye level 2, topical anti-inflammatory agents were used for many patients with level 1 dry eye in actual clinical practice. This study showed that topical anti-inflammatory agents were used in 48.7% of patients with dry eye level 1. The aforementioned study also reported that level 2 treatments were prescribed for 43% of patients diagnosed at severity level 1 and suggested that this might be a consequence of physicians' increased awareness that aggressive, early treatment might slow or prevent the disease's progression [12]. These current practice patterns demonstrate that artificial tears and patient education often fail to resolve symptoms of level 1 patients. Except for artificial tears and topical anti-inflammatory agents, the number of available treatments for dry eye level 1 or level 2 is very limited. Most physicians appear to be looking forward to using new topical agents with different treatment modalities for their unsatisfied dry eye patients.
In the Korean guidelines for dry eye, level 1 treatment options include patient education and preserved or non-preserved artificial tears, whereas level 2 treatment choices range from preservative-free artificial tears to topical anti-inflammatory agents, gels or ointments, and oral essential fatty acid supplementation. Although preserved or non-preserved artificial tears could be used for patients with dry eye level 1, 76.3% of patients were prescribed non-preserved artificial tears. The percentage of non-preserved artificial tears increased as the dry eye severity level increased. Benzalkonium chloride is most frequently used in topical ophthalmic preparations as well as in topical lubricants, and its epithelial toxicity has been well established [13,14,15]. Preservative toxicity has a higher potential in patients with moderate-to-severe dry eye due to their decreased tear secretion and reduced turnover [16]. However, this study showed that physicians prefer preservative-free artificial tears even in patients with mild dry eye, presumably because of the concern for preservative toxicity.
Practice styles differed somewhat depending on physician age and clinic types. The use of topical anti-inflammatory agents was not different between the three age groups, whereas specific therapy choices among topical anti-inflammatory agents were significantly different. Although physicians in their 40s showed a tendency to use 0.05% topical cyclosporine more often than those in other age groups, there was no specific pattern as a physician aged. However, older physicians used preserved artificial tears more frequently. This may reflect a tendency of older physicians to continue the use of their past practice styles, even though the elimination of preservatives from lubricants is one of the most critical advances in the treatment of dry eye. The use of topical anti-inflammatory agents and the choice of artificial tears were significantly different depending on the clinic types of physicians. Physicians working at referral hospitals tended to use topical anti-inflammatory agents and preservative-free artificial tears earlier, beginning at dry eye level 1. This trend may be because most of the patients who had been referred had not responded to treatment with preserved artificial tears at the private eye clinics that referred them.
This study had a limitation. Although multicenter studies have several benefits, such as a large number of participants, different geographic locations and the ability to compare results among centers, they often lack conformity of data, which may compromise the ability to pool data in a standardized manner. In this study, the severity level of dry eye might differ somewhat according to diagnosing physicians even though the Korean guidelines for dry eye treatment were exclusively used for standardization.
In conclusion, topical anti-inflammatory agents are often used in the treatment of dry eye patients in South Korea, even beginning at dry eye level 1. Preservative-free artificial tears are preferred at all dry eye levels. Practice styles are somewhat different depending on the age and clinic type of physicians.
Acknowledgements
This study was supported by an unrestricted educational grant from Allergan Inc. (Irvine, CA, USA).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Pflugfelder SC, Jones D, Ji Z, et al. Altered cytokine balance in the tear fluid and conjunctiva of patients with Sjogren's syndrome keratoconjunctivitis sicca. Curr Eye Res. 1999;19:201–211. doi: 10.1076/ceyr.19.3.201.5309. [DOI] [PubMed] [Google Scholar]
- 2.Tsubota K, Fujihara T, Saito K, et al. Conjunctival epithelium expression of HLA-DR in dry eye patients. Ophthalmologica. 1999;213:16–19. doi: 10.1159/000027387. [DOI] [PubMed] [Google Scholar]
- 3.Li DQ, Chen Z, Song XJ, et al. Stimulation of matrix metalloproteinases by hyperosmolarity via a JNK pathway in human corneal epithelial cells. Invest Ophthalmol Vis Sci. 2004;45:4302–4311. doi: 10.1167/iovs.04-0299. [DOI] [PubMed] [Google Scholar]
- 4.De Paiva CS, Corrales RM, Villarreal AL, et al. Corticosteroid and doxycycline suppress MMP-9 and inflammatory cytokine expression, MAPK activation in the corneal epithelium in experimental dry eye. Exp Eye Res. 2006;83:526–535. doi: 10.1016/j.exer.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 5.Baudouin C. The pathology of dry eye. Surv Ophthalmol. 2001;45(Suppl 2):S211–S220. doi: 10.1016/s0039-6257(00)00200-9. [DOI] [PubMed] [Google Scholar]
- 6.Turner K, Pflugfelder SC, Ji Z, et al. Interleukin-6 levels in the conjunctival epithelium of patients with dry eye disease treated with cyclosporine ophthalmic emulsion. Cornea. 2000;19:492–496. doi: 10.1097/00003226-200007000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Brignole F, Pisella PJ, De Saint Jean M, et al. Flow cytometric analysis of inflammatory markers in KCS: 6-month treatment with topical cyclosporin A. Invest Ophthalmol Vis Sci. 2001;42:90–95. [PubMed] [Google Scholar]
- 8.Kunert KS, Tisdale AS, Gipson IK. Goblet cell numbers and epithelial proliferation in the conjunctiva of patients with dry eye syndrome treated with cyclosporine. Arch Ophthalmol. 2002;120:330–337. doi: 10.1001/archopht.120.3.330. [DOI] [PubMed] [Google Scholar]
- 9.Behrens A, Doyle JJ, Stern L, et al. Dysfunctional tear syndrome: a Delphi approach to treatment recommendations. Cornea. 2006;25:900–907. doi: 10.1097/01.ico.0000214802.40313.fa. [DOI] [PubMed] [Google Scholar]
- 10.Management and therapy of dry eye disease: report of the Management and Therapy Subcommittee of the International Dry Eye WorkShop (2007) Ocul Surf. 2007;5:163–178. doi: 10.1016/s1542-0124(12)70085-x. [DOI] [PubMed] [Google Scholar]
- 11.Jackson WB. Management of dysfunctional tear syndrome: a Canadian consensus. Can J Ophthalmol. 2009;44:385–394. doi: 10.3129/i09-015. [DOI] [PubMed] [Google Scholar]
- 12.Wilson SE, Stulting RD. Agreement of physician treatment practices with the international task force guidelines for diagnosis and treatment of dry eye disease. Cornea. 2007;26:284–289. doi: 10.1097/ICO.0b013e31802dffc7. [DOI] [PubMed] [Google Scholar]
- 13.Gasset AR, Ishii Y, Kaufman HE, et al. Cytotoxicity of ophthalmic preservatives. Am J Ophthalmol. 1974;78:98–105. doi: 10.1016/0002-9394(74)90016-6. [DOI] [PubMed] [Google Scholar]
- 14.Wilson FM., 2nd Adverse external ocular effects of topical ophthalmic medications. Surv Ophthalmol. 1979;24:57–88. doi: 10.1016/0039-6257(79)90125-5. [DOI] [PubMed] [Google Scholar]
- 15.Burstein NL. Corneal cytotoxicity of topically applied drugs, vehicles and preservatives. Surv Ophthalmol. 1980;25:15–30. doi: 10.1016/0039-6257(80)90072-7. [DOI] [PubMed] [Google Scholar]
- 16.Nelson JD. Simultaneous evaluation of tear turnover and corneal epithelial permeability by fluorophotometry in normal subjects and patients with keratoconjunctivitis sicca (KCS) Trans Am Ophthalmol Soc. 1995;93:709–753. [PMC free article] [PubMed] [Google Scholar]