Abstract
Background
Coffee consumption has been linked to various beneficial and detrimental health effects, but data on the relation with mortality are sparse.
Objective
To assess the association between coffee consumption and mortality from cardiovascular disease (CVD), cancer, and all causes during 18 years of follow-up in men and 24 years of follow-up in women.
Design
Sex-specific Cox proportional hazards models were used to investigate the association between coffee consumption and incidence of death from all causes and specific mortality in a prospective cohort study.
Setting
Health Professionals Follow-up Study and Nurses' Health Study.
Participants
41,736 men and 86,214 women, without history of CVD or cancer at baseline.
Measurements
Coffee consumption was first assessed in 1986 for men and in 1980 for women, and then repeatedly every 2-4 years; the follow-up continued through 2004. We documented 6,888 deaths (2,049 due to CVD and 2,491 due to cancer) among men, and 11,095 deaths (2,368 due to CVD and 5,011 due to cancer) among women.
Results
For men, after adjustment for age, smoking, and other CVD and cancer risk factors, the relative risks (RRs) of all cause mortality across categories of coffee consumption (<1cup/mo, 1/mo-4/wk, 5-7/wk, 2-3/d, 4-5/d, and ≥6/d) were: 1.0, 1.07 (95% confidence interval: 0.99-1.16), 1.02 (0.95-1.11), 0.97 (0.89-1.05), 0.93 (0.81-1.07), and 0.80 (0.62-1.04) (p for trend= 0.008); for women, the RRs were: 1.0, 0.98 (0.91-1.05), 0.93 (0.87-0.98), 0.82 (0.77-0.87), 0.74 (0.68-0.81), and 0.83 (0.73-0.95) (p for trend<0.001). This inverse association was mainly due to a moderately reduced risk of CVD mortality, and was independent of caffeine intake. By contrast, coffee consumption was not significantly associated with risk of cancer death after adjustment for potential confounders. Decaffeinated coffee consumption was associated with a small reduction in all cause and CVD mortality.
Limitations
Some measurement error in the assessment of coffee consumption is inevitable because we estimated the consumption from self-reports.
Conclusions
Regular coffee consumption was not associated with an increased mortality in either men or women. The possibility of a modest benefit of coffee consumption on all cause and CVD mortality needs to be further investigated.
Journal Subject Heads: coffee, all causes death, cardiovascular death, cancer death, Health Professionals Follow-up Study, Nurses' Health Study
Introduction
Numerous epidemiologic studies have examined coffee consumption and risk of coronary heart disease and other chronic diseases, but data on coffee consumption in relation to total and cause-specific mortality are sparse. Some studies found an inverse association (1-5) and this has been attributed to a possible confounding effect by morbidity: those who drank coffee were the healthiest cohort members. However, it has recently been suggested that the inverse association between coffee and all cause mortality is attributable to the beneficial effect of coffee consumption on inflammation.(6)
In support of this hypothesis, we found in a previous study an inverse association between coffee consumption and several markers of inflammation and endothelial dysfunction. (7) In addition, in the Nurses' Health Study and Health Professionals Follow-up Study, consumption of 6 or more cups of coffee per day was associated with a slightly lower risk of fatal coronary heart disease in both men and women as compared to non-consumers. (8) Moreover, epidemiological studies have consistently found an association between higher coffee consumption and lower risk of type 2 diabetes. (9) Finally, several studies have suggested that coffee might decrease the risk of several types of cancer, mainly liver, colon, oral, pharyngeal, and esophageal cancer. (10-12)
The objective of this study was to assess the association of coffee consumption with total, cardiovascular (CVD), and cancer mortality. The long duration of follow-up and the use of repeated dietary measurements allowed us to assess long-term coffee consumption. In addition, information about incident diseases during the follow-up and updated measurements of main risk factors for cardiovascular disease and cancer allowed us to control for potential confounders in detail.
Methods
Study Population
The Health Professionals Follow-up Study (HPFS) was established in 1986 and the Nurses' Health Study (NHS) in 1976. Information on the cohorts, except diet, has been updated every 2 years. Further details have been published elsewhere. (13) We used 1980 as baseline for the NHS because this was the first year in which dietary information was collected in this cohort. In this study, after excluding participants with CVD or cancer at baseline or without information about coffee consumption at baseline (1183 persons in the HPFS and 879 in the NHS), we included in the analyses 41,736 men and 86,214 women who were followed until 2004. The Harvard School of Public Health and Brigham and Women's Hospital Human Subjects Committee Review Board approved the study protocol.
Assessment of coffee consumption
Dietary questionnaires were sent to the HPFS participants in 1986, 1990, 1994, and 1998 and to the NHS participants in 1980, 1984, 1986, 1990, 1994, and 1998. In each questionnaire, participants were asked how often on average during the previous year they had consumed coffee and tea. The participants could choose from 9 responses. Decaffeinated coffee and different types of caffeinated soft drinks were first assessed in 1986 in the HPFS and in 1984 in the NHS. In addition, we also inquired at baseline if the participant's consumption for each beverage had greatly increased or decreased over the preceding 10 years. Using the U.S. Department of Agriculture food composition sources, supplemented with other sources, we estimated that the caffeine content was 137 mg per cup of coffee, 47 mg per cup of tea, 46 mg per can or a 12-ounce bottle of soft drink, and 7 mg per 1-ounce serving of chocolate candy. We assessed the total intake of caffeine by summing the caffeine content for a unit of each food during the previous year multiplied by a weight proportional to the frequency of its consumption. In our validation study, we obtained high correlations between consumption of coffee and other caffeinated beverages estimated from the food frequency questionnaire and consumption estimated from repeated 1-week diet records (coffee, r=0.78; tea, r=0.93; and caffeinated soft drinks, r=0.85). (14)
Ascertainment of mortality
Deaths were reported by the next of kin or the postal authorities or were ascertained through the National Death Index. We estimated that follow-up for deaths was more than 98 percent complete.(15) For all deaths, we sought death certificates and, when appropriate, requested permission from the next of kin to review medical records. The underlying cause of death was assigned according to the International Classification of Diseases, 8th Revision (ICD-8). The primary end point in this analysis was death for any cause. We also conducted analyses according to the main causes of deaths in the cohorts, which were CVD (ICD-8 codes 390.0 through 458.9 and 795.0 to 795.9), and cancer (ICD-8 codes 140.0 through 207.9), and according to secondary causes of death: chronic liver disease and cirrhosis (ICD-8 code 571.0), chronic obstructive pulmonary disease (ICD-8 codes 492.0, 496.0, and 519.0), diabetes (ICD-8 codes 250.0, 250.1, and 250.9), neurodegenerative diseases (ICD-8 codes 331.0 and 332.0), and sudden death (ICD-8 code 798.0).
Assessment of medical history, anthropometric data and lifestyle factors
In the baseline questionnaires, we requested information about age, weight and height, smoking status, parental history with respect to myocardial infarction, menopausal status and use of hormone therapy in women, and personal history of hypertension, hypercholesterolemia, and type 2 diabetes mellitus. This information, with the exception of height and parental history, has been updated in the biennial follow-up questionnaires. Perceived health was assessed in 2000 by asking to the participants to describe their health as excellent, very good, good, fair, or poor. Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. Physical activity was also assessed biennially. In the HPFS, participants were queried about the average time spent per week during the preceding year in specific activities (e.g., walking outdoors, jogging, and bicycling). (16) The time spent in each activity in hours per week was multiplied by its typical energy expenditure, expressed in metabolic equivalent tasks and then summed over all activities to yield a metabolic equivalent task/hour score. In the NHS, physical activity was reported in hours per week of moderate (e.g., brisk walking) and vigorous exercise (e.g., strenuous sports and jogging). (17) Standard portion sizes for alcoholic drinks were specified as a can/bottle or glass for beer, 4-oz glass for wine, and one drink or shot for liquor. Detailed information on the validity and reproducibility of the information about self-reported weight, physical activity, and alcohol consumption from the questionnaires has been reported elsewhere. (18-20)
Statistical analysis
Participants were classified according to levels of coffee consumption. Person-years of exposure were calculated from the date of return of the baseline questionnaire to the date of death, or June 1, 2004, whichever came first. To reduce within-subject variation and best represent long-term diet, we used the cumulative average of coffee consumption from all available dietary questionnaires up to the start of each 2-year follow-up interval; (21) for example, in the HPFS, the average of the 1986 and 1990 intake was used for the follow-up between 1990 and 1994; and the average of the 1986, 1990, and 1994 intake was used for the follow-up between 1994 and 1998. When a food frequency questionnaire had a missing value for coffee, we used the value from the previous questionnaire.
Sex-specific Cox proportional hazards models were used to investigate the association between coffee consumption and incidence of death from all causes and specific mortality. To control as finely as possible for confounding by age and calendar time, we stratified the analysis jointly by age in months at start of follow-up and calendar year of the current questionnaire cycle. Hazard ratios were used to estimate relative risks in each category in comparison with participants in the lower category of coffee consumption. Multivariable models were adjusted for smoking status, body mass index, physical activity, alcohol intake, use of hormone therapy for women, parental history of myocardial infarction, and dietary factors (total energy intake, use of multivitamin and vitamin E supplements, polyunsaturated, saturated, n-3, and trans fat intake, glycemic load, and folic acid intake), by using categorical variables. To test for linear trends across categories, we modeled coffee consumption as a continuous variable using the median value of each level of coffee consumption. In addition, we calculated pooled relative risks of all cause mortality for men and women combined across categories of coffee consumption using a random effect method. We also examined a possible non-linear relation between coffee consumption and total and cardiovascular mortality non-parametrically with restricted cubic splines. (22)
Stratified analyses were conducted according to smoking status, alcohol consumption, and body mass index. We examined interactions between coffee and the categories of the stratification variables with mortality using likelihood-ratio tests, which compared the nested models with and without cross-product terms. We also analyzed the independent effect of total coffee consumption compared to caffeine intake on mortality through cross-classifications of both variables. Finally, we examined the association between decaffeinated coffee consumption and mortality.
In secondary analyses, we controlled the association between coffee consumption and mortality for hypertension, hypercholesterolemia, diabetes (these diseases could modify coffee consumption) and perceived health. Moreover, we analyzed the association between continuous baseline coffee consumption and mortality, correcting the relative risk obtained using the method of Rosner et al. (23) All analyses were performed using SAS software, version 9.1 (SAS Institute Inc, Cary, NC).
This manuscript follows the STROBE recommendations. (24) The authors had full access to the data and take responsibility for its integrity. All authors have read and agreed to the manuscript as written. Supported by NIH research grants CA87969, CA55075, HL34594, and HL60712. Dr. Lopez-Garcia's research is supported by a ‘Ramón y Cajal’ contract. Dr. Hu's research is partly supported by an American Heart Association Established Investigator Award. The founding sources had no role in the design and conduct of the study, analysis or interpretation of the data, or preparation or final approval of the manuscript before publication.
Results
During 18 years of follow-up in the HPFS, we identified 6,888 deaths (2,049 from CVD and 2,491 from cancer). For the NHS, during 24 years of follow-up, we identified 11,095 deaths (2,368 from CVD and 5,011 from cancer). Baseline characteristics of the population are presented by levels of coffee consumption in Table 1. Frequent coffee consumption was strongly associated with smoking. In addition, individuals who drank more coffee were more likely to drink alcohol and less likely to exercise and to use multivitamin and vitamin E supplements.
Table 1.
Baseline characteristics according to caffeinated coffee consumption levels among participants in the Health Professionals Follow-up Study and the Nurses' Health Study.
| Coffee consumption among men in HPFS (1986 baseline), cups | Coffee consumption among women in NHS (1980 baseline), cups | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| <1/mo | 1/mo-4/wk | 5-7/wk | 2-3/d | 4-5/d | ≥6/d | <1/mo | 1/mo-4/wk | 5-7/wk | 2-3/d | 4-5/d | ≥6/d | |
| Participants, n | 12168 | 7353 | 7564 | 9968 | 3468 | 1215 | 19276 | 5264 | 11672 | 28375 | 14465 | 7162 |
| Age, y | 52 | 52 | 53 | 52 | 52 | 52 | 45 | 45 | 46 | 46 | 46 | 46 |
| Current smoker, % | 5 | 7 | 8 | 11 | 18 | 29 | 19 | 20 | 19 | 27 | 40 | 56 |
| BMI, kg/m2 | 24.7 | 24.8 | 24.9 | 25.1 | 25.3 | 25.2 | 24.7 | 24.5 | 24.4 | 24.2 | 24.1 | 24.2 |
| Physical activity, h/wk | … | … | … | … | … | … | 4.0 | 4.0 | 3.9 | 3.9 | 3.8 | 3.7 |
| Physical activity, metabolic equivalent tasks h/wk | 27.5 | 25.8 | 27.2 | 24.7 | 24.1 | 20.0 | … | … | … | … | … | … |
| Alcohol consumption, g/d | 7.7 | 10.3 | 11.5 | 14.5 | 14.5 | 15.9 | 4.4 | 5.2 | 5.7 | 7.5 | 7.4 | 6.7 |
| Parental history of MI, % | 32 | 32 | 32 | 31 | 32 | 30 | 20 | 20 | 19 | 20 | 20 | 21 |
| Postmenopausal hormone use, % | … | … | … | … | … | … | 9 | 8 | 8 | 8 | 7 | 7 |
| Multivitamin use, % | 12 | 12 | 12 | 12 | 11 | 10 | 36 | 38 | 36 | 33 | 31 | 29 |
| Vitamin E supplement use, % | 10 | 11 | 10 | 9 | 8 | 7 | 14 | 15 | 14 | 12 | 11 | 11 |
| Polyunsaturated fat, % energy | 5.9 | 5.9 | 5.9 | 6.0 | 6.0 | 5.9 | 5.3 | 5.3 | 5.2 | 5.2 | 5.3 | 5.4 |
| Saturated fat, % energy | 10.6 | 10.8 | 11.0 | 11.3 | 11.9 | 12.4 | 15.3 | 15.4 | 15.4 | 15.6 | 15.9 | 16.3 |
| Fish n-3 fatty acids, % energy | 0.14 | 0.15 | 0.15 | 0.13 | 0.12 | 0.11 | 0.55 | 0.55 | 0.55 | 0.55 | 0.56 | 0.56 |
| Trans fat, % energy | 1.2 | 1.2 | 1.3 | 1.3 | 1.4 | 1.4 | 2.2 | 2.2 | 2.2 | 2.2 | 2.3 | 2.3 |
| Glycemic load | 131 | 126 | 124 | 119 | 115 | 111 | 91 | 88 | 88 | 84 | 81 | 79 |
| Folate, μg/d | 506 | 501 | 479 | 450 | 432 | 417 | 387 | 391 | 378 | 358 | 345 | 325 |
| Caffeine, mg/d | 51 | 91 | 194 | 418 | 692 | 885 | 117 | 134 | 218 | 418 | 751 | 881 |
Values are means unless otherwise indicated. Data, except age, were directly standardized to the age distributions of the entire cohorts.
HPFS: Health Professionals Follow-up Study, NHS: Nurses' Health Study, MI: myocardial infarction.
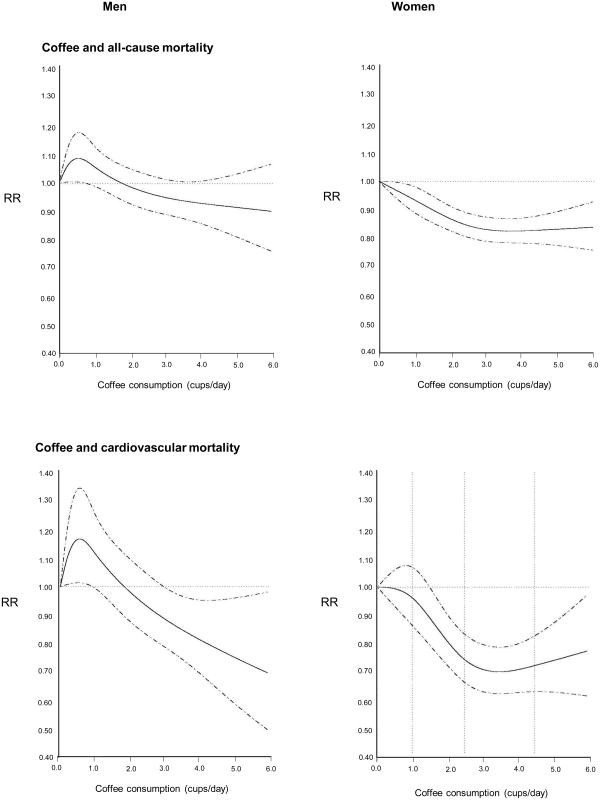
In age-adjusted analyses, we observed that high coffee consumption was associated with a higher risk of all cause mortality in men and women (Table 2). However, after adjusting for confounders especially cigarette smoking, an inverse association between coffee consumption and death from all causes was observed in both men (p for trend =0.008) and women (p for trend <0.001). Among men, the RRs for each category of coffee consumption did not reach the statistical significance. However, among women, the RR of death from all causes in those consuming 5 to 7 cups per week of coffee was 7% lower than in those non-coffee drinkers; the decrease in all cause mortality was 18% in those drinking 2 to 3 cups of coffee per day, 26% in those consuming 4 to 5 cups per day, and finally, 17% in those consuming 6 or more cups/day. This reduction in death from all causes was partly due to the reduction in CVD mortality observed in women who consumed coffee (Table 2, Figure 1). The pooled RRs of all cause mortality for men and women combined across categories of coffee consumption were 1.0, 1.02 (95% CI 0.96 to 1.07), 0.96 (0.92-1.01), 0.86 (0.82-0.91), 0.79 (0.73-0.85), and 0.83 (0.73-0.93).
Table 2.
Relative risks of death from all causes and specific causes by levels of caffeinated coffee consumption in men and women.
| Coffee consumption, cups | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| <1/mo | 1/mo-4/wk | 5-7/wk | 2-3/d | 4-5/d | ≥6/d | P value for trend | |
| Men | |||||||
| Death from all causes | |||||||
| Person-yr | 170,743 | 145,607 | 187,985 | 148,389 | 37,639 | 10,601 | |
| No. of deaths | 1553 | 1570 | 2117 | 1289 | 286 | 73 | |
| Age-adjusted | 1.0 | 0.99 (0.93-1.07) | 0.97 (0.91-1.03) | 0.98 (0.91-1.06) | 1.11 (0.97-1.25) | 1.28 (1.01-1.62) | 0.14 |
| Age and smoking | 1.0 | 1.02 (0.95-1.10) | 1.00 (0.94-1.07) | 0.95 (0.89-1.03) | 0.97 (0.85-1.10) | 0.95 (0.75-1.21) | 0.12 |
| Multivariable * | 1.0 | 1.07 (0.99-1.16) | 1.02 (0.95-1.11) | 0.97 (0.89-1.05) | 0.93 (0.81-1.07) | 0.80 (0.62-1.04) | 0.008 |
| Death from CVD | |||||||
| No. of deaths | 459 | 488 | 664 | 357 | 66 | 15 | |
| Age-adjusted | 1.0 | 1.03 (0.91-1.17) | 1.01 (0.90-1.14) | 0.93 (0.81-1.06) | 0.89 (0.69-1.15) | 0.93 (0.56-1.56) | 0.10 |
| Age and smoking | 1.0 | 1.06 (0.93-1.20) | 1.04 (0.92-1.17) | 0.90 (0.78-1.03) | 0.79 (0.61-1.03) | 0.72 (0.43-1.20) | 0.003 |
| Multivariable | 1.0 | 1.05 (0.90-1.21) | 1.09 (0.95-1.25) | 0.95 (0.81-1.11) | 0.85 (0.65-1.13) | 0.56 (0.31-1.03) | 0.03 |
| Death from Cancer | |||||||
| No. of deaths | 537 | 578 | 729 | 491 | 122 | 34 | |
| Age-adjusted | 1.0 | 1.06 (0.95-1.20) | 0.98 (0.88-1.09) | 1.07 (0.95-1.21) | 1.33 (1.10-1.63) | 1.65 (1.17-2.34) | 0.002 |
| Age and smoking | 1.0 | 1.08 (0.96-1.22) | 0.99 (0.89-1.11) | 1.03 (0.91-1.16) | 1.17 (0.96-1.42) | 1.27 (0.89-1.80) | 0.27 |
| Multivariable | 1.0 | 1.14 (1.00-1.30) | 1.01 (0.89-1.15) | 1.01 (0.88-1.16) | 1.15 (0.93-1.43) | 1.14 (0.79-1.65) | 0.82 |
| Other causes | |||||||
| No. of deaths | 557 | 504 | 724 | 441 | 98 | 24 | |
| Age-adjusted | 1.0 | 0.89 (0.79-1.01) | 0.92 (0.83-1.03) | 0.94 (0.83-1.06) | 1.05 (0.85-1.31) | 1.16 (0.77-1.75) | 0.41 |
| Age and smoking | 1.0 | 0.93 (0.82-1.05) | 0.98 (0.88-1.09) | 0.92 (0.81-1.05) | 0.92 (0.74-1.14) | 0.84 (0.55-1.26) | 0.30 |
| Multivariable | 1.0 | 1.01 (0.88-1.17) | 0.98 (0.85-1.12) | 0.93 (0.80-1.08) | 0.76 (0.59-0.98) | 0.65 (0.11-1.04) | 0.006 |
| Women | |||||||
| Death from all causes | |||||||
| Person-yr | 319,326 | 247,470 | 609,374 | 563,666 | 172,583 | 60,180 | |
| No. of deaths | 1665 | 1610 | 3946 | 2876 | 738 | 260 | |
| Age-adjusted | 1.0 | 0.90 (0.84-0.96) | 0.86 (0.81-0.91) | 0.90 (0.84-0.95) | 1.01 (0.93-1.10) | 1.39 (1.22-1.59) | 0.001 |
| Age and smoking | 1.0 | 0.89 (0.83-0.95) | 0.82 (0.77-0.87) | 0.77 (0.73-0.82) | 0.76 (0.70-0.83) | 0.92 (0.80-1.05) | <0.001 |
| Multivariable | 1.0 | 0.98 (0.91-1.05) | 0.93 (0.87-0.98) | 0.82 (0.77-0.87) | 0.74 (0.68-0.81) | 0.83 (0.73-0.95) | <0.001 |
| Death from CVD | |||||||
| No. of deaths | 362 | 362 | 868 | 563 | 151 | 62 | |
| Age-adjusted | 1.0 | 0.91 (0.79-1.06) | 0.86 (0.76-0.97) | 0.80 (0.70-0.91) | 0.95 (0.79-1.15) | 1.53 (1.16-2.00) | 0.78 |
| Age and smoking | 1.0 | 0.91 (0.79-1.05) | 0.82 (0.72-0.92) | 0.67 (0.58-0.76) | 0.67 (0.55-0.81) | 0.91 (0.69-1.19) | <0.001 |
| Multivariable | 1.0 | 1.06 (0.91-1.22) | 0.99 (0.87-1.12) | 0.75 (0.66-0.86) | 0.66 (0.54-0.80) | 0.81 (0.61-1.06) | <0.001 |
| Death from Cancer | |||||||
| No. of deaths | 679 | 691 | 1722 | 1409 | 378 | 132 | |
| Age-adjusted | 1.0 | 0.98 (0.88-1.09) | 0.96 (0.88-1.05) | 1.08 (0.98-1.18) | 1.22 (1.08-1.39) | 1.60 (1.32-1.93) | <0.001 |
| Age and smoking | 1.0 | 0.96 (0.87-1.07) | 0.91 (0.83-0.99) | 0.94 (0.86-1.04) | 0.97 (0.85-1.10) | 1.15 (0.95-1.39) | 0.45 |
| Multivariable | 1.0 | 1.01 (0.91-1.12) | 0.95 (0.87-1.04) | 0.94 (0.86-1.04) | 0.91 (0.80-1.03) | 1.05 (0.87-1.28) | 0.26 |
| Other causes | |||||||
| No. of deaths | 624 | 557 | 1356 | 904 | 209 | 66 | |
| Age-adjusted | 1.0 | 0.80 (0.71-0.89) | 0.75 (0.69-0.83) | 0.75 (0.68-0.84) | 0.81 (0.69-0.95) | 1.06 (0.82-1.37) | 0.12 |
| Age and smoking | 1.0 | 0.79 (0.70-0.88) | 0.72 (0.65-0.79) | 0.65 (0.59-0.72) | 0.60 (0.51-0.70) | 0.66 (0.51-0.85) | <0.001 |
| Multivariable | 1.0 | 0.89 (0.78-1.00) | 0.86 (0.77-0.95) | 0.70 (0.63-0.78) | 0.59 (0.50-0.70) | 0.60 (0.46-0.77) | <0.001 |
Values are relative risks and 95% confidence intervals. CVD: cardiovascular disease.
Adjusted for: age (5-year categories), smoking status (never, past, and current 1-14, 15-24, and ≥25 cigarettes/day), body mass index (<23.0, 23.0-24.9, 25.0-27.9, 28.0-29.9, ≥30.0 kg/m2), physical activity (quintiles of metabolic equivalent tasks hours/week for men, and <1.0, 1.0-1.9, 2.0-3.9, 4.0-6.9, ≥7.0 hours/week for women), alcohol intake (never, 0.1-4.9, 5.0-9.9, 10.0-14.9, 15.0-29.9, ≥30.0 g/d), parental history with respect to myocardial infarction, menopausal status and use of hormone therapy for women (premenopausal women, post without hormone therapy, post with past hormone therapy, post with current hormone therapy), multivitamin use, vitamin E supplement use, total caloric intake, and quintiles of polyunsaturated, saturated, fish n-3, and trans fat intake, glycemic load, and folate intake.
Figure 1.
Non-linear relation between coffee consumption and total and cardiovascular mortality. Data were adjusted for variables in Table 2.
Coffee consumption was not significantly associated with risk of cancer death after adjustment for potential confounders in either cohort (Table 2). In addition, regular coffee consumption was associated with lower risk of mortality from ‘other causes’, mainly in women. In particular, we observed inverse associations between coffee consumption and death from chronic liver disease and cirrhosis (n cases=135, multivariate RRs were 1.0, 0.91, 0.81, 0.41, and 0.35, p for trend<0.001) and diabetes mortality (n cases=152, RRs were 1.0, 0.80, 0.65, 0.49, and 0.57, p for trend=0.02).
The inverse association between coffee consumption and death from all causes remained significant in non-smokers, alcohol drinkers, and non-obese men (Table 3). Among women, we did not find substantial differences in the association between coffee consumption and all cause mortality across all categories of smoking status, alcohol consumption, and BMI.
Table 3.
Caffeinated coffee consumption and relative risks of all cause mortality in men and women, by the stratification variables.
| Coffee consumption, cups | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| <1/mo | 1/mo-4/wk | 5-7/wk | 2-3/d | ≥4/d | P value for trend | P value for interaction | |
| Men | |||||||
| Smoking status | |||||||
| Never | 1.0 | 1.01 (0.85-1.18) | 0.95 (0.80-1.12) | 0.79 (0.64-0.97) | 0.63 (0.40-0.99) | 0.003 | |
| Past | 1.0 | 1.15 (0.99-1.33) | 1.06 (0.93-1.22) | 1.02 (0.88-1.18) | 0.86 (0.68-1.10) | 0.06 | |
| Current * | 1.0 | 1.16 (0.78-1.71) | 1.12 (0.79-1.60) | 0.94 (0.66-1.33) | 0.92 (0.62-1.37) | 0.18 | 0.62 |
| Alcohol | |||||||
| Abstainer | 1.0 | 0.99 (0.84-1.16) | 1.04 (0.89-1.22) | 1.06 (0.89-1.27) | 0.76 (0.57-1.01) | 0.34 | |
| Drinker | 1.0 | 1.08 (0.98-1.19) | 1.01 (0.92-1.10) | 0.94 (0.85-1.04) | 0.92 (0.80-1.07) | 0.01 | 0.36 |
| BMI | |||||||
| <30 kg/m2 | 1.0 | 1.05 (0.96-1.14) | 1.02 (0.94-1.10) | 0.95 (0.87-1.04) | 0.86 (0.75-0.99) | 0.005 | |
| ≥30 kg/m2 | 1.0 | 1.19 (0.92-1.55) | 0.99 (0.78-1.27) | 0.95 (0.73-1.23) | 1.17 (0.82-1.66) | 0.79 | 0.57 |
| Women | |||||||
| Smoking status | |||||||
| Never | 1.0 | 1.01 (0.91-1.12) | 0.93 (0.85-1.03) | 0.70 (0.63-0.79) | 0.68 (0.55-0.82) | <0.001 | |
| Past | 1.0 | 0.97 (0.87-1.08) | 0.92 (0.84-1.01) | 0.89 (0.81-0.98) | 0.89 (0.78-1.01) | 0.03 | |
| Current * | 1.0 | 1.00 (0.81-1.24) | 1.00 (0.84-1.19) | 0.82 (0.69-0.96) | 0.72 (0.60-0.86) | <0.001 | 0.36 |
| Alcohol | |||||||
| Abstainer | 1.0 | 1.05 (0.93-1.18) | 0.94 (0.85-1.04) | 0.83 (0.74-0.93) | 0.76 (0.65-0.88) | <0.001 | |
| Drinker | 1.0 | 0.94 (0.86-1.02) | 0.91 (0.85-0.98) | 0.80 (0.74-0.87) | 0.75 (0.68-0.83) | <0.001 | 0.47 |
| BMI | |||||||
| <30 kg/m2 | 1.0 | 0.93 (0.86-1.01) | 0.88 (0.82-0.93) | 0.81 (0.76-0.87) | 0.78 (0.71-0.85) | <0.001 | |
| ≥30 kg/m2 | 1.0 | 1.02 (0.86-1.19) | 0.93 (0.81-1.07) | 0.78 (0.66-0.90) | 0.77 (0.61-0.96) | <0.001 | 0.37 |
Models adjusted for the same covariates as in Table 2, except for the stratification variable. Values are relative risks and 95% confidence intervals. BMI: body mass index.
Additional adjustment for No. of cigarettes/d.
We attempted to separate the effects of coffee (including decaffeinated coffee) from caffeine intake on all cause mortality (Table 4). In the cross-classification analyses, no clear pattern was observed among men, but for women who drank 2 or more cups of coffee per day, the inverse association between coffee and death from all causes was independent of the amount of caffeine ingested. Because these analyses suggested that components in coffee other than caffeine could explain the association observed, we next examined whether decaffeinated coffee was associated with mortality. We found that higher decaffeinated coffee consumption was also associated with a slightly lower risk of total and CVD death, especially in women (Table 5).
Table 4.
RRs of death from all causes by combinations of coffee consumption (including decaffeinated coffee) and caffeine intake.
| Quintiles of caffeine intake | |||
|---|---|---|---|
|
| |||
| Q1-Q2 | Q3 | Q4-Q5 | |
| Men | |||
| Total coffee, <1/mo to 4/wk, cups | |||
| Median caffeine intake (mg/d) | 33 | 164 | 338 |
| Person-yr | 175,021 | 28,477 | 11,715 |
| No. of deaths | 1602 | 237 | 99 |
| Multivariable | 1.0 | 0.97 (0.83-1.12) | 0.91 (0.73-1.13) |
| Total coffee, 5 to 7/wk, cups | |||
| Median caffeine intake (mg/d) | 71 | 179 | 307 |
| Person-yr | 71,136 | 85,037 | 54,586 |
| No. of deaths | 923 | 959 | 596 |
| Multivariable | 1.00 (0.91-1.10) | 0.96 (0.88-1.06) | 1.00 (0.90-1.12) |
| Total coffee, ≥2/day, cups | |||
| Median caffeine intake (mg/d) | 46 | 192 | 451 |
| Person-yr | 33,971 | 26,837 | 214,186 |
| No. of deaths | 351 | 316 | 1805 |
| Multivariable | 0.92 (0.80-1.05) | 1.09 (0.94-1.25) | 0.91 (0.84-0.98) |
| Women* | |||
| Total coffee, <1/mo to 4/wk, cups | |||
| Median caffeine intake (mg/d) | 98 | 302 | 511 |
| Person-yr | 313,837 | 62,955 | 143,116 |
| No. of deaths | 2022 | 415 | 962 |
| Multivariable | 1.0 | 0.90 (0.81-1.00) | 0.79 (0.73-0.86) |
| Total coffee, 5 to 7/wk, cups | |||
| Median caffeine intake (mg/d) | 161 | 292 | 397 |
| Person-yr | 234,597 | 126,844 | 41,575 |
| No. of deaths | 1570 | 859 | 314 |
| Multivariable | 0.98 (0.92-1.05) | 1.01 (0.93-1.10) | 1.04 (0.92-1.17) |
| Total coffee, ≥2/day, cups | |||
| Median caffeine intake (mg/d) | 175 | 314 | 506 |
| Person-yr | 83,305 | 126,042 | 446,278 |
| No. of deaths | 456 | 662 | 2481 |
| Multivariable | 0.84 (0.76-0.93) | 0.80 (0.73-0.88) | 0.84 (0.78-0.89) |
Follow-up since 1984. The person-years and cases are different for women from previous tables because of the different years of follow-up. Models included the same covariates as in Table 2. Values are relative risks and 95% confidence intervals.
Table 5.
Decaffeinated coffee consumption and RRs of death from all causes and specific causes in men and women.
| Decaffeinated coffee consumption, cups | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| <1/mo | 1/mo-4/wk | 5-7/wk | 2-3/d | ≥4/d | P value for trend | |
| Men | ||||||
| Death from all causes | ||||||
| Person-yr | 294,554 | 213,006 | 131,207 | 50,843 | 11,355 | |
| No. of deaths | 2783 | 2059 | 1479 | 481 | 86 | |
| Age-adjusted | 1.0 | 0.85 (0.81-0.90) | 0.85 (0.80-0.90) | 0.92 (0.84-1.01) | 1.00 (0.81-1.24) | 0.20 |
| Multivariable | 1.0 | 0.96 (0.90-1.03) | 0.93 (0.86-1.01) | 0.91 (0.82-1.01) | 0.81 (0.64-1.03) | 0.02 |
| Death from CVD | ||||||
| No. of deaths | 777 | 668 | 439 | 146 | 19 | |
| Age-adjusted | 1.0 | 0.98 (0.89-1.09) | 0.88 (0.78-0.99) | 0.99 (0.84-1.19) | 0.81 (0.51-1.28) | 0.23 |
| Multivariable | 1.0 | 1.10 (0.97-1.24) | 0.97 (0.85-1.12) | 0.95 (0.78-1.17) | 0.83 (0.52-1.31) | 0.16 |
| Death from Cancer | ||||||
| No. of deaths | 979 | 746 | 540 | 180 | 46 | |
| Age-adjusted | 1.0 | 0.89 (0.81-0.98) | 0.90 (0.81-1.00) | 0.97 (0.83-1.14) | 1.49 (1.11-2.00) | 0.20 |
| Multivariable | 1.0 | 0.96 (0.86-1.07) | 0.95 (0.84-1.07) | 0.95 (0.80-1.13) | 1.20 (0.87-1.66) | 0.81 |
| Women * | ||||||
| Death from all causes | ||||||
| Person-yr | 760,095 | 387,614 | 314,893 | 99,778 | 16,169 | |
| No. of deaths | 5023 | 2252 | 1921 | 486 | 59 | |
| Age-adjusted | 1.0 | 0.73 (0.69-0.76) | 0.72 (0.68-0.75) | 0.74 (0.67-0.81) | 0.76 (0.59-0.99) | <0.001 |
| Multivariable | 1.0 | 0.92 (0.87-0.97) | 0.89 (0.84-0.94) | 0.85 (0.77-0.94) | 0.78 (0.61-1.00) | <0.001 |
| Death from CVD | ||||||
| No. of deaths | 1096 | 441 | 401 | 114 | 10 | |
| Age-adjusted | 1.0 | 0.66 (0.59-0.73) | 0.68 (0.61-0.76) | 0.78 (0.64-0.94) | 0.58 (0.31-1.08) | <0.001 |
| Multivariable | 1.0 | 0.84 (0.75-0.95) | 0.85 (0.75-0.95) | 0.89 (0.73-1.09) | 0.55 (0.30-1.04) | 0.04 |
| Death from Cancer | ||||||
| No. of deaths | 2126 | 1021 | 852 | 233 | 30 | |
| Age-adjusted | 1.0 | 0.81 (0.75-0.87) | 0.78 (0.72-0.84) | 0.83 (0.72-0.95) | 0.87 (0.60-1.24) | <0.001 |
| Multivariable | 1.0 | 0.97 (0.90-1.05) | 0.93 (0.85-1.01) | 0.94 (0.82-1.08) | 0.86 (0.60-1.23) | 0.14 |
Follow-up since 1984. The person-years and cases are different for women from previous tables because of the different years of follow-up. Models included the same covariates as in Table 2, plus caffeinated coffee consumption. Values are relative risks and 95% confidence interval.
We conducted various sensitivity analyses to evaluate the robustness of our results. First, we performed analyses excluding individuals in the lowest category of coffee consumption (<1 cup per month) to test whether specific characteristics of this group confounded the association and obtained similar results. We also conducted analyses excluding participants who reduced their coffee consumption in the 10 years preceding the study, excluding the first 4 years of follow-up (when participants could suffer from undiagnosed diseases), using only the most recent coffee consumption (to assess short-term effects), and adjusting the models for high blood pressure, hypercholesterolemia, or type 2 diabetes, perceived health, and pack-years of smoking, but the estimates remained similar to those in the main analyses. Finally, after correcting for measurement error, the relative risk for the association between baseline coffee consumption (as a continuous variable) and risk of all cause mortality for men was 1.01 (95% CI 0.99 to 1.04), which was the same as the uncorrected value 1.01 (1.00-1.03). For women, the validation dataset necessary to conduct the correction was unavailable.
Discussion
In these two large cohort studies, we did not find a detrimental effect of coffee consumption on mortality. By contrast, our results showed a modest inverse association between coffee and all cause mortality in both men and women. This association was mainly explained by a reduction in CVD mortality. Our data also suggest that this association was due to other components in coffee rather than caffeine.
Previous studies examined the effect of coffee on all cause mortality in different populations. Legrady et al (25) followed a cohort of 2000 men during 19 years and found that those who drank 6 or more cups of coffee per day had 1.7 times (95% CI 1.27-2.30) higher risk of death from coronary heart disease compared with those consuming l cup per day or less. In addition, a Norwegian study (26) found an increased risk of mortality from coronary heart disease after a follow-up of 6 years, but later, they found that the association was weakened with longer follow-up.(27) In contrast, other studies observed that coffee consumption was inversely associated with mortality. (1-5) For example, Kleemola et al, (2) after 10-year follow-up of a large middle age population, found that men who consumed 7 or more cups of coffee per day had a RR of 1.01 (95% CI 0.84-1.22), but women who consumed that amount of coffee had a significantly decreased risk of all cause mortality (RR=0.62, 95% CI 0.44-0.84). These authors attributed their findings to possible subclinical diseases that led to a reduction in coffee consumption. However, Andersen et al, (6) after analyzing a cohort of postmenopausal women followed during 15 years, concluded that consumption of coffee was inversely associated with all cause mortality (RR=0.87, 95% CI 0.76-1.00 for those drinking 6 or more cups per day in comparison with non- drinkers) and CVD mortality (RR=0.87, 95% CI 0.69-1.09), and attributed the results to the effect of coffee on reducing chronic inflammation.
Our findings are consistent with the possible beneficial effects of coffee on inflammation, endothelial function, and risk of type 2 diabetes. We previously reported an inverse association of caffeinated coffee consumption with surface leukocyte adhesion molecules (E-selectin) and with C-reactive protein (a monocyte activator in the endothelial wall) in diabetic women, and an inverse association of decaffeinated coffee consumption with C-reactive protein in healthy women. (7) In addition, Yukawa et al (28) found that regular coffee ingestion reduced low-density lipoprotein oxidation susceptibility. Coffee may favorably affect endothelial atherosclerotic plaques through this pathway because oxidized low-density lipoprotein is present in atherosclerotic lesions. (29) Also, the phenolic compounds of coffee (chlorogenic acid, ferulic acid, and p-coumaric acid) have a strong antioxidant capacity. (30) Chlorogenic acid might also improve glucose tolerance. (31) In addition, coffee contains many other substances including magnesium, trigonelline, and quinides that have been associated with improved insulin sensitivity.(32) All these mechanisms can counterbalance some of the potential harmful effects of caffeine, for example, the acute stimulation of the release of epinephrine, a potent inhibitor of insulin activity, and the acute increase in blood pressure and homocysteine levels. (33-35) Thus, the above mechanisms also support our finding of an inverse association of coffee and all cause mortality independent of caffeine intake. Finally, in our analysis, coffee consumption was associated with a slight reduction in mortality due to chronic liver disease and cirrhosis in women. Previous studies have shown that coffee consumption may have a protective effect on hepatic cancer (36) and various components of coffee have been associated with this favorable effect, including caffeine, coffee oils kahweol and cafestol, and phenolic components. (37, 38)
We have extended the previous analyses using larger cohorts of men and women, and assessing the cumulative coffee consumption instead of the consumption only at the start of follow-up. The cumulative consumption reflects long-term exposure to coffee, and may therefore be more appropriate for the study of all cause mortality and death from chronic diseases. In addition, we have been able to better control for potential confounders because information about incident diseases and risk factors has been updated every 2 years. We believe that our results were not confounded by morbidity because we performed several additional analyses to address this problem. In particular, we controlled our models for hypertension, hypercholesterolemia, and type 2 diabetes. In addition, we excluded the first 4 years of follow-up to avoid subclinical morbidity, and we adjusted the association for perceived health. On the other hand, some measurement error in the assessment of coffee consumption is inevitable because we estimated the consumption from self-reports; however, the dietary questionnaire has been shown to reflect long-term intake, (39) the validation data showed that coffee was among the most accurately reported items in the food frequency questionnaire, (14) and the relative risk for the association between continuous baseline coffee consumption and all cause mortality corrected for measurement error was very similar to the uncorrected one. In addition, in our analyses, the inverse association between coffee and mortality was stronger in women. Possible reasons include a shorter follow-up in men, different distribution of causes of mortality for men and women, and different age ranges. However, formal tests for heterogeneity in the associations between the two cohorts were not statistically significant. Finally, because our study was conducted among health care professionals, extrapolation of results to the general population should be made with caution.
In conclusion, the data from two large cohort studies of men and women suggest that regular coffee consumption is not associated with an increased mortality in either men or women. The possibility of a modest benefit of coffee consumption on all cause and CVD mortality needs to be further investigated.
Appendix 1.
Cohort studies addressing the association between coffee consumption and total and cause-specific mortality.*
| Author | Sex, age (years) | N | Exposure | Outcome | No. of cases | Mean follow-up (years) | Adjustment for confounding | Multivariate-adjusted result | Comments |
|---|---|---|---|---|---|---|---|---|---|
| Iwai et al. (1) | M/F, 40-79 | 2855 | Coffee at baseline | Death from all causes | 361 | 9.9 | Age, physical activity, education, history of chronic diseases.SMK, alcohol (only in M). | For consumption of ≥2 cups/d, the RR was 0.43 (95% CI 0.30-0.63) for M and 0.76 (0.45-1.27) for F. | Inverse association between coffee and total mortality in M. |
|
| |||||||||
| Kleemola et al. (2) | M/F, 30-59 | 20179 | Coffee at baseline | Death from all causes Death from CHD |
1645 975 |
10 | Age, SMK, cholesterol, blood pressure, history of MI | M: for consumption of ≥7 cups/d, the RR of total death was 1.01 (0.84-1.22) and the RR of CHD death was 1.22 (0.90-1.65). F: for consumption of ≥7 cups/d, the RR of total death was 0.62 (0.44-0.87) and the RR of CHD death was 0.57 (0.28-1.16). |
Inverse association between coffee and total mortality in F.No association between coffee and CHD mortality in M/F. |
|
| |||||||||
| Woodward et al. (3) | M/F, 40-59 | 11000 | Coffee at baseline | Death from all causes Death from CHD |
573 357 |
7.7 | Age, housing tenure, activity at work, activity in leisure, SMK, BMI, Bortner score, cotinine, SBP, fibrinogen, total cholesterol, HDL, TG, alcohol, vit.C, tea. | M: for consumption of ≥5 cups/d, the RR of total death was 0.77 and the RR of CHD death was 0.58. F: for consumption of ≥5 cups/d, the RR of total death was 0.79 and the RR of CHD death was 1.18. |
Inverse association between coffee and total mortality in M/F. Inverse association between coffee and CHD mortality in M. |
|
| |||||||||
| Rosengren et al. (4) | M, 51-59 | 6765 | Coffee at baseline | Death from all causes Death from CHD Death from cancer |
478 169 Not available |
7.1 | Age, SBP, BMI, diabetes, alcohol abuse, family history of MI, mental stress, physical activity, occupational class. | For consumption of ≥9 cups/d, the RR of total death was 0.6 (0.3-0.9), the RR of CHD death was 1.4 (0.8-2.4), and the RR of cancer death was 0.9 (0.4-2.1). | Inverse association between coffee and total mortality. No association between coffee and CHD and cancer mortality. |
|
| |||||||||
| Murray et al. (5) | M, ≥35 | 16911 | Coffee at baseline | Death from all causes other than CHD Death from CHD |
985 721 |
11.5 | Age, SMK, urban/rural residence | For consumption of ≥7 cups/d, the RR of total death was 0.86, and the RR of CHD death was 0.91. | Inverse association between coffee and total and CHD mortality. |
|
| |||||||||
| Andersen et a. (6) | F, 55-69 | 41836 | Coffee at baseline | Death from all causes Death from CVD Death from cancer Death from inflammatory diseases |
4265 1411 1733 713 |
15 | Age, SMK, alcohol, BMI, waist-hip ratio, education, physical activity, use of estrogens, MV, energy intake, whole and refined grain, red meat, fish and seafood, total fruit and vegetables. | For consumption of 4-5 cups/d, the RR of total death was 0.81 (0.72-0.91), the RR of CVD death was 0.81 (0.66-0.99), the RR of cancer death was 0.84 (0.70-1.02), and the RR of inflammatory death was 0.67 (0.50-0.90). | U-shape association between coffee and total and CVD mortality; no association with cancer mortality; inverse association with inflammatory mortality. |
|
| |||||||||
| Lopez-Garcia et al. (8) | M/F, 30-55 | 128493 | Cumulative exposure | Death from CHD | 1417 | 14 (M), 20 (F) | Age, SMK, BMI, physical activity, alcohol, parental history of MI, menopausal status, use of hormone therapy, aspirin, MV, vit. E, hypertension, hypercholesterolemia, diabetes mellitus. | M: For consumption of ≥6 cups/d, the RR of CHD death was 0.60 (0.26-1.36). F: For consumption of ≥6 cups/d, the RR of CHD death was 0.61 (0.37-1.02). |
Weak inverse association between coffee and CHD mortality. |
|
| |||||||||
| Legrady et al. (25) | M, 40-56 | 1910 | Coffee at 1 year baseline | Death from all causes Death from CHD Death from all causes other than CHD |
452 220 232 |
19 | Age, DBP, cholesterol, SMK. | For consumption of ≥6 cups/d, the RR of total death was 1.33 (1.07-1.65), the RR of CHD death was 1.71 (1.27-2.30), and the RR of non-CHD death was 1.02 (0.73-1.41). | Direct association between coffee and total and CHD mortality. |
|
| |||||||||
| Tverdal et al. (26) | M/F, 35-54 | 38564 | Coffee at baseline | Death from CHD | 174 | 6.4 | Age, cholesterol, HDL, SBP, SMK | M: For consumption of ≥9 cups/d, the RR of CHD death was 2.2 (1.1-4.5). F: For consumption of ≥9 cups/d, the RR of CHD death was 5.1 (0.4-60.3). |
Direct association between coffee and CHD mortality. |
|
| |||||||||
| Stensvold et al. (27) | M/F, 35-54 | 38564 | Coffee at baseline | Death from CHD | 476 | 12 | Age, cholesterol, HDL, SBP, SMK | For consumption of ≥9 cups/d, the RR of CHD death was 1.3. | No association between coffee and CHD mortality when Tverdal et al. study (25) was continued for 6 more years. |
|
| |||||||||
| Greenberg et al. (40) | M/F, 32-86 | 6594 | Caffeinated beverages at baseline | Death from CVD Death from CHD Death from cerebrovascular disease |
426 347 79 |
8.8 | Age, SMK, BMI, sex, race, physical activity, alcohol, income, education, American-style diet. | In ≥65 y old, for consumption of ≥4 cups/d the RR of CVD death was 0.53 (0.38-0.75), the RR of CHD death was 0.47 (0.32-0.69), and the RR of cerebrovascular death was 0.88 (0.42-1.83). | Inverse association between caffeinated beverages and CVD and CHD mortality among elderly participants but not among younger participants. |
|
| |||||||||
| Hart et al. (41) | M, 35-64 | 5766 | Coffee at baseline | Death from CHD | 625 | 17 | Age, DBP, cholesterol, SMK, social class, education, BMI, angina. | For consumption of ≥4.5 cups/d, the RR of CHD death was 1.49 (0.89-2.47). | No association between coffee and CHD mortality. |
|
| |||||||||
| Jazbec et al. (42) | M/F, 35-59 | 3364 | Coffee at baseline | Death from all causes Death from CVD |
950 435 |
27 | Age, region, SMK, DBP, feeling of well-being, history of stomach ulcer | M: for consumption of 1-2 cups/d, the RR of total death was 0.78 (0.61-0.98), and the RR of CVD was 0.82 (0.58-1.16). F: for consumption of 1-2 cups/d, the RR of total death was 0.63 (0.46-0.86), and the RR of CVD was 0.67 (0.43-1.05). |
Inverse association between coffee and total mortality. |
|
| |||||||||
| Lindsted et al. (43) | M, ≥30 | 9484 | Coffee at baseline | Death from all causes Death from CVD |
Not available | 25 | Age, BMI, heart disease, hypertension, race, exercise, sleep, marital status, education, SMK, diet history. | For consumption of ≥1-2 cups/d, the RR of total death was 1.15 (1.05-1.26), and the RR of CVD was 1.09 (0.82-1.46). | Weak direct association between coffee and total mortality and CVD mortality. |
|
| |||||||||
| Jacobsen et al. (44) | M/F, not available | 16555 | Coffee at baseline | Death from all causes Death from cancer |
4032 886 |
11.5 | Age, residence, SMK | For consumption of ≥7 cups/d, the RR of total death was 0.95 (p=0.15), and the RR of cancer was 1.14 (p=0.49). | No association between coffee and total and cancer death. |
|
| |||||||||
| Happonen et al. (45) | M, 42-60 | 1971 | Coffee at baseline | Death from CHD | 269 | 14 | Age. SMK, ischemia, diabetes, income, serum insulin, DBP, HDL, LDL, maximal oxygen uptake, WHR. | Heavy drinkers (≥814 mL/d) had a RR of CHD death of 1.43 (1.06-1.94). | Direct association between coffee and CHD mortality. |
|
| |||||||||
| Paganini-Hill et al. (46) | M/F, 44-101 | 13624 | Coffee at baseline | Death from all causes | 11386 | 23 | Age, sex, SMK, physical activity BMI, alcohol, hypertension, angina, heart attack, stroke, diabetes, rheumatoid arthritis, cancer. | For consumption of 2-3 cups/d, the RR of total death was 0.89 (0.85-0.94). | U-shape association between coffee and total and mortality. |
|
| |||||||||
| Dawber et al. (47) | M/F, 30-62 | 5209 | Coffee at baseline | Death from all causes Death from CHD |
321 Not available |
12 | Age, SMK | M: for consumption of ≥6 cups/d, the RR of total death was 1.01 and the RR of CHD death was 0.92. | Direct association between coffee and total mortality in M. No association between coffee and CHD mortality in M/F. |
|
| |||||||||
| Vandenbroucke et al. (48) | M/F, 40-65 | 3091 | Coffee at baseline | Death from all causes | Not available | 25 | Age, SMK, alcohol, BMI, living parents, cholesterol SBP. | M: for consumption of ≥5 cups/d, the RR of total death was 1.42 (0.94-2.15). F: for consumption of ≥5 cups/d, the RR of total death was 0.83 (0.52-1.30). |
Direct association between coffee and total mortality in M. |
|
| |||||||||
| Kurozawa et al. (49) | M/F, 40-79 | 110688 | Coffee at baseline | Death from hepatocellular carcinoma | 258 | 11 | Age, gender, education, history of diabetes and liver diseases, SMK, alcohol. | For consumption of ≥1 cups/d, the RR of cancer death was 0.50 (0.31-0.79). | Inverse association between coffee and risk of death from hepatocellular carcinoma. |
Obtained from a MEDLINE search through February 2008 using the key words coffee and caffeine in combination with mortality and death.
M: men; F: female; SMK: smoking; CHD: coronary heart disease; MI: myocardial infarction; BMI: body mass index; SBP: systolic blood pressure; HDL: high density lipoprotein; TG: tryglicerides; vit.C: vitamin C; MV: multivitamins; vit.E: vitamin E; DBP: diastolic blood pressure; LDL: low density lipoprotein; WHR: waist-hip ratio.
Acknowledgments
Grant Support: Supported by NIH research grants CA87969, CA55075, HL34594, and HL60712. Dr. Lopez-Garcia's research is supported by a ‘Ramón y Cajal’ contract. Dr. Hu's research is partly supported by an American Heart Association Established Investigator Award.
Footnotes
Author Contributions: Study concept and design: Lopez-Garcia, van Dam, Li, Rodriguez-Artalejo, Hu.
Acquisition of data: Hu.
Analysis and interpretation of data: Lopez-Garcia, van Dam, Li, Rodriguez-Artalejo, Hu.
Drafting of the manuscript: Lopez-Garcia.
Critical revision of the manuscript for important intellectual content: Lopez-Garcia, van Dam, Li, Rodriguez-Artalejo, Hu.
Statistical expertise: Lopez-Garcia.
Obtained funding: Hu.
Administrative, technical, or material support: Rodriguez-Artalejo, Hu.
Study supervision: Hu.
Authors who have no conflict of interest: Lopez-Garcia, van Dam, Li, Rodriguez-Artalejo, Hu.
Research Statements: Protocol: available at http://www.hsph.harvard.edu/hpfs/ and http://www.channing.harvard.edu/nhs/
Statistical code: not available
Data: available subject to approval by the Nurses' Health Study and Health Professional Follow-up Study committees.
References
- 1.Iwai N, Ohshiro H, Kurozawa Y, Hosoda T, Morita H, Funakawa K, et al. Relationship between coffee and green tea consumption and all-cause mortality in a cohort of a rural Japanese population. J Epidemiol. 2002;12:191–8. doi: 10.2188/jea.12.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kleemola P, Jousilahti P, Pietinen P, Vartiainen E, Tuomilehto J. Coffee consumption and the risk of coronary heart disease and death. Arch Intern Med. 2000;160:3393–400. doi: 10.1001/archinte.160.22.3393. [DOI] [PubMed] [Google Scholar]
- 3.Woodward M, Tunstall-Pedoe H. Coffee and tea consumption in the Scottish Heart Health Study follow up: conflicting relations with coronary risk factors, coronary disease, and all cause mortality. J Epidemiol Community Health. 1999;53:481–7. doi: 10.1136/jech.53.8.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosengren A, Wilhelmsen L. Coffee, coronary heart disease and mortality in middle-aged Swedish men: findings from the Primary Prevention Study. J Intern Med. 1991;230:67–71. doi: 10.1111/j.1365-2796.1991.tb00407.x. [DOI] [PubMed] [Google Scholar]
- 5.Murray SS, Bjelke E, Gibson RW, Schuman LM. Coffee consumption and mortality from ischemic heart disease and other causes: results from the Lutheran Brotherhood study, 1966-1978. Am J Epidemiol. 1981;113:661–7. doi: 10.1093/oxfordjournals.aje.a113145. [DOI] [PubMed] [Google Scholar]
- 6.Andersen LF, Jacobs DR, Jr, Carlsen MH, Blomhoff R. Consumption of coffee is associated with reduced risk of death attributed to inflammatory and cardiovascular diseases in the Iowa Women's Health Study. Am J Clin Nutr. 2006;83:1039–46. doi: 10.1093/ajcn/83.5.1039. [DOI] [PubMed] [Google Scholar]
- 7.Lopez-Garcia E, van Dam RM, Qi L, Hu FB. Coffee consumption and markers of inflammation and endothelial dysfunction in healthy and diabetic women. Am J Clin Nutr. 2006;84:888–93. doi: 10.1093/ajcn/84.4.888. [DOI] [PubMed] [Google Scholar]
- 8.Lopez-Garcia E, van Dam RM, Willett WC, et al. Coffee consumption and coronary heart disease in men and women: a prospective cohort study. Circulation. 2006;113:2045–53. doi: 10.1161/CIRCULATIONAHA.105.598664. [DOI] [PubMed] [Google Scholar]
- 9.van Dam RM, Hu FB. Coffee consumption and risk of type 2 diabetes: a systematic review. JAMA. 2005;294:97–104. doi: 10.1001/jama.294.1.97. [DOI] [PubMed] [Google Scholar]
- 10.La Vecchia C. Coffee, liver enzymes, cirrhosis and liver cancer. J Hepatol. 2005;42:444–6. doi: 10.1016/j.jhep.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 11.Tavani A, Bertuzzi M, Talamini R, Gallus S, Parpinel M, Franceschi S, et al. Coffee and tea intake and risk of oral, pharyngeal and esophageal cancer. Oral Oncol. 2003;39:695–700. doi: 10.1016/s1368-8375(03)00081-2. [DOI] [PubMed] [Google Scholar]
- 12.Tavani A, La Vecchia C. Coffee, decaffeinated coffee, tea and cancer of the colon and rectum: a review of epidemiological studies, 1990-2003. Cancer Causes Control. 2004;15:743–57. doi: 10.1023/B:CACO.0000043415.28319.c1. [DOI] [PubMed] [Google Scholar]
- 13.Colditz GA, Hankinson SE. The Nurses' Health Study: lifestyle and health among women. Nat Rev Cancer. 2005;5:388–96. doi: 10.1038/nrc1608. [DOI] [PubMed] [Google Scholar]
- 14.Salvini S, Hunter DJ, Sampson L, Stampfer MJ, Colditz GA, Rosner B, et al. Food-based validation of a dietary questionnaire: the effects of week-to-week variation in food consumption. Int J Epidemiol. 1989;18:858–67. doi: 10.1093/ije/18.4.858. [DOI] [PubMed] [Google Scholar]
- 15.Stampfer MJ, Willett WC, Speizer FE, Dysert DC, Lipnick R, Rosner B, et al. Test of the National Death Index. Am J Epidemiol. 1984;119:837–9. doi: 10.1093/oxfordjournals.aje.a113804. [DOI] [PubMed] [Google Scholar]
- 16.Koh-Banerjee P, Chu NF, Spiegelman D, Rosner B, Colditz G, Willett W, et al. Prospective study of the association of changes in dietary intake, physical activity, alcohol consumption, and smoking with 9-y gain in waist circumference among 16 587 US men. Am J Clin Nutr. 2003;78:719–27. doi: 10.1093/ajcn/78.4.719. [DOI] [PubMed] [Google Scholar]
- 17.Rockhill B, Willett WC, Manson JE, Leitzmann MF, Stampfer MJ, Hunter DJ, et al. Physical activity and mortality: a prospective study among women. Am J Public Health. 2001;91:578–83. doi: 10.2105/ajph.91.4.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1:466–73. doi: 10.1097/00001648-199011000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Chasan-Taber S, Rimm EB, Stampfer MJ, Spiegelman D, Colditz GA, Giovannucci E, et al. Reproducibility and validity of a self-administered physical activity questionnaire for male health professionals. Epidemiology. 1996;7:81–6. doi: 10.1097/00001648-199601000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Giovannucci E, Colditz G, Stampfer MJ, Rimm EB, Litin L, Sampson L, et al. The assessment of alcohol consumption by a simple self-administered questionnaire. Am J Epidemiol. 1991;133:810–7. doi: 10.1093/oxfordjournals.aje.a115960. [DOI] [PubMed] [Google Scholar]
- 21.Hu FB, Stampfer MJ, Rimm E, Ascherio A, Rosner BA, Spiegelman D, et al. Dietary fat and coronary heart disease: a comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am J Epidemiol. 1999;149:531–40. doi: 10.1093/oxfordjournals.aje.a009849. [DOI] [PubMed] [Google Scholar]
- 22.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8:551–61. doi: 10.1002/sim.4780080504. [DOI] [PubMed] [Google Scholar]
- 23.Rosner B, Willett WC, Spiegelman D. Correction of logistic regression relative risk estimates and confidence intervals for systematic within-person measurement error. Stat Med. 1989;8:1051–69. doi: 10.1002/sim.4780080905. discussion 1071-3. [DOI] [PubMed] [Google Scholar]
- 24.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–7. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 25.LeGrady D, Dyer AR, Shekelle RB, Stamler J, Liu K, Paul O, et al. Coffee consumption and mortality in the Chicago Western Electric Company Study. Am J Epidemiol. 1987;126:803–12. doi: 10.1093/oxfordjournals.aje.a114717. [DOI] [PubMed] [Google Scholar]
- 26.Tverdal A, Stensvold I, Solvoll K, Foss OP, Lund-Larsen P, Bjartveit K. Coffee consumption and death from coronary heart disease in middle aged Norwegian men and women. BMJ. 1990;300:566–9. doi: 10.1136/bmj.300.6724.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stensvold I, Tverdal A, Jacobsen BK. Cohort study of coffee intake and death from coronary heart disease over 12 years. BMJ. 1996;312:544–5. doi: 10.1136/bmj.312.7030.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yukawa GS, Mune M, Otani H, Tone Y, Liang XM, Iwahashi H, et al. Effects of coffee consumption on oxidative susceptibility of low-density lipoproteins and serum lipid levels in humans. Biochemistry (Mosc) 2004;69:70–4. doi: 10.1023/b:biry.0000016354.05438.0f. [DOI] [PubMed] [Google Scholar]
- 29.Meisinger C, Baumert J, Khuseyinova N, Loewel H, Koenig W. Plasma oxidized low-density lipoprotein, a strong predictor for acute coronary heart disease events in apparently healthy, middle-aged men from the general population. Circulation. 2005;112:651–7. doi: 10.1161/CIRCULATIONAHA.104.529297. [DOI] [PubMed] [Google Scholar]
- 30.Gomez-Ruiz JA, Leake DS, Ames JM. In vitro antioxidant activity of coffee compounds and their metabolites. J Agric Food Chem. 2007;55:6962–9. doi: 10.1021/jf0710985. [DOI] [PubMed] [Google Scholar]
- 31.Arnlov J, Vessby B, Riserus U. Coffee consumption and insulin sensitivity. JAMA. 2004;291:1199–201. doi: 10.1001/jama.291.10.1199-b. [DOI] [PubMed] [Google Scholar]
- 32.van Dam RM. Coffee and type 2 diabetes: from beans to beta-cells. Nutr Metab Cardiovasc Dis. 2006;16:69–77. doi: 10.1016/j.numecd.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 33.Thong FS, Graham TE. Caffeine-induced impairment of glucose tolerance is abolished by beta-adrenergic receptor blockade in humans. J Appl Physiol. 2002;92:2347–52. doi: 10.1152/japplphysiol.01229.2001. [DOI] [PubMed] [Google Scholar]
- 34.Hartley TR, Lovallo WR, Whitsett TL. Cardiovascular effects of caffeine in men and women. Am J Cardiol. 2004;93:1022–6. doi: 10.1016/j.amjcard.2003.12.057. [DOI] [PubMed] [Google Scholar]
- 35.Verhoef P, Pasman WJ, Van Vliet T, Urgert R, Katan MB. Contribution of caffeine to the homocysteine-raising effect of coffee: a randomized controlled trial in humans. Am J Clin Nutr. 2002;76:1244–8. doi: 10.1093/ajcn/76.6.1244. [DOI] [PubMed] [Google Scholar]
- 36.Larsson SC, Wolk A. Coffee consumption and risk of liver cancer: a meta-analysis. Gastroenterology. 2007;132:1740–5. doi: 10.1053/j.gastro.2007.03.044. [DOI] [PubMed] [Google Scholar]
- 37.Huber WW, Scharf G, Rossmanith W, Prustomersky S, Grasl-Kraupp B, Peter B, et al. The coffee components kahweol and cafestol induce gamma-glutamylcysteine synthetase, the rate limiting enzyme of chemoprotective glutathione synthesis, in several organs of the rat. Arch Toxicol. 2002;75:685–94. doi: 10.1007/s00204-001-0295-5. [DOI] [PubMed] [Google Scholar]
- 38.Scharf G, Prustomersky S, Huber WW. Elevation of glutathione levels by coffee components and its potential mechanisms. Adv Exp Med Biol. 2001;500:535–9. doi: 10.1007/978-1-4615-0667-6_82. [DOI] [PubMed] [Google Scholar]
- 39.Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;122:51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]
- 40.Greenberg JA, Dunbar CC, Schnoll R, Kokolis R, Kokolis S, Kassotis J. Caffeinated beverage intake and the risk of heart disease mortality in the elderly: a prospective analysis. Am J Clin Nutr. 2007;85:392–8. doi: 10.1093/ajcn/85.2.392. [DOI] [PubMed] [Google Scholar]
- 41.Hart C, Smith GD. Coffee consumption and coronary heart disease mortality in Scottish men: a 21 year follow up study. J Epidemiol Community Health. 1997;51:461–2. doi: 10.1136/jech.51.4.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jazbec A, Simic D, Corovic N, Durakovic Z, Pavlovic M. Impact of coffee and other selected factors on general mortality and mortality due to cardiovascular disease in Croatia. J Health Popul Nutr. 2003;21:332–40. [PubMed] [Google Scholar]
- 43.Lindsted KD, Kuzma JW, Anderson JL. Coffee consumption and cause-specific mortality. Association with age at death and compression of mortality. J Clin Epidemiol. 1992;45:733–42. doi: 10.1016/0895-4356(92)90051-n. [DOI] [PubMed] [Google Scholar]
- 44.Jacobsen BK, Bjelke E, Kvale G, Heuch I. Coffee drinking, mortality, and cancer incidence: results from a Norwegian prospective study. J Natl Cancer Inst. 1986;76:823–31. [PubMed] [Google Scholar]
- 45.Happonen P, Voutilainen S, Salonen JT. Coffee drinking is dose-dependently related to the risk of acute coronary events in middle-aged men. J Nutr. 2004;134:2381–6. doi: 10.1093/jn/134.9.2381. [DOI] [PubMed] [Google Scholar]
- 46.Paganini-Hill A, Kawas CH, Corrada MM. Non-alcoholic beverage and caffeine consumption and mortality: the Leisure World Cohort Study. Prev Med. 2007;44:305–10. doi: 10.1016/j.ypmed.2006.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dawber TR, Kannel WB, Gordon T. Coffee and cardiovascular disease. Observations from the framingham study. N Engl J Med. 1974;291:871–4. doi: 10.1056/NEJM197410242911703. [DOI] [PubMed] [Google Scholar]
- 48.Vandenbroucke JP, Kok FJ, van 't Bosch G, van den Dungen PJ, van der Heide-Wessel C, van der Heide RM. Coffee drinking and mortality in a 25-year follow up. Am J Epidemiol. 1986;123:359–61. doi: 10.1093/oxfordjournals.aje.a114245. [DOI] [PubMed] [Google Scholar]
- 49.Kurozawa Y, Ogimoto I, Shibata A, Nose T, Yoshimura T, Suzuki H, et al. Coffee and risk of death from hepatocellular carcinoma in a large cohort study in Japan. Br J Cancer. 2005;93:607–10. doi: 10.1038/sj.bjc.6602737. [DOI] [PMC free article] [PubMed] [Google Scholar]