Abstract
Purpose
Recent studies have shown that individuals with schizophrenia and their family members are interested in genetic counseling, but few have received this service. We conducted an exploratory, retrospective study to describe (a) the population of individuals who were referred to the provincial program for genetic counseling for a primary indication of schizophrenia, and (b) trends in number of referrals between 1968 and 2007.
Methods
Referrals for a primary indication of schizophrenia were identified through the provincial program database. Charts were reviewed and the following information was recorded: discipline of referring physician, demographics, psychiatric diagnosis, referred individual’s and partner’s (if applicable) family history, and any current pregnancy history. Data were characterized using descriptive statistics.
Results
Between 1968 and 2007, 288 referrals were made for a primary indication of schizophrenia. Most referrals were made: (a) for individuals who had a first-degree family member with schizophrenia, rather than for affected individuals, (b) for preconception counseling, and (c) by family physicians (69%), with only 2% by psychiatrists.
Conclusions
In British Columbia, individuals affected with schizophrenia and their family members are rarely referred for psychiatric genetic counseling. There is a need to identify barriers to psychiatric genetic counseling and develop strategies to improve access.
Keywords: Family History, Genetic Counseling, Psychiatric, Referrals, Schizophrenia
INTRODUCTION
Schizophrenia is a common, complex disorder affecting ~1% of the population worldwide. Twin and family studies have demonstrated that schizophrenia has a significant genetic component1, and that although environmental factors play an important role in its etiology2, the single greatest risk factor for developing schizophrenia is having a positive family history 3.
Genetic counseling for psychiatric disorders is similar to that provided for other complex disorders. It can provide affected individuals and their family members with information regarding the etiology of illness, recurrence risks, family planning and use of medications during pregnancy1. As with other disorders, genetic counseling in the context of psychiatric illness provides a forum for exploring and promoting understanding of the illness, facilitating decision-making and adaptation to the illness1, and may help decrease stigma4. As compared to other genetic counseling specialties (such as for hereditary cancer syndromes), psychiatric genetic counseling as a specialist discipline is nascent. However; psychiatric genetic counseling was perceived to be an area of growth by 96% of the responding members of the National Society of Genetic Counselors, in a 1995 survey by Turlington and Moldin5.
Recent studies have shown that there is a great deal of interest in the concept of genetic counseling amongst individuals with schizophrenia and their family members. In one study of 48 family members of individuals with schizophrenia, 70.9% indicated that they would attend a genetic counseling appointment6. In another study7, 74% of relatives of people with schizophrenia and 62% of affected individuals indicated they would like to see a genetic counselor; however, 94% of relatives, and 94% of affected individuals had never been offered genetic counseling7.
Although genetic counselors perceive psychiatric disorders to represent an area of service growth, and affected families report having interest in genetic counseling for psychiatric disorders, little is known about the current environment with regards to psychiatric genetic counseling services from the clinical perspective. In order to meet any potential increase in demand and to develop strategies to better serve this population, it is important to develop an understanding of the existing landscape, including characteristics of who has received psychiatric genetic counseling, and how referral patterns may have changed over time.
Since 1968, in the Canadian province of British Columbia, all psychiatric genetic counseling services are provided through the British Columbia Provincial Medical Genetics (BCPMG) program, which provides service for a wide array of conditions. The BCPMG program maintains an extensive database of information about referrals and thus, is ideally suited for the exploration of such issues. We conducted an exploratory study to describe a) the population of individuals who were referred to the BCPMG program for a primary indication of schizophrenia between 1968 and 2007, and b) trends in annual number of referrals for a primary indication of schizophrenia over time.
MATERIALS AND METHODS
The BCPMG program database includes demographic and diagnosis information (manually entered by staff) about each patient referred since the program’s inception in 1968. We performed a search of the “diagnosis” field of the BCPMG program database using the term schizophrenia, as well as wildcard search for schiz, and possible spelling mistakes. There were three main reasons for which schizophrenia could appear in the diagnosis field of the BCPMG program database:
Schizophrenia was the primary reason for referral,
Schizophrenia was an incidental finding that was identified during the personal or family medical history documentation component of the genetic counseling session,
Schizophrenia was one of the phenotypic features listed in a referral for an individual to be evaluated by a Clinical Geneticist to rule out a genetic syndrome.
All charts identified using this search strategy were reviewed. The purpose of this study was to focus exclusively on schizophrenia referrals that were unrelated to genetic syndromes, so charts were excluded from the study if, upon review, they: a) revealed no mention of schizophrenia, b) were unavailable, or c) were identified as falling into either the second or third categories listed above.
Characterizing the population of individuals referred to the BCPMG Program for a primary indication of schizophrenia
A database was constructed containing demographic information for the individuals whose charts met the criteria outlined above, and who were referred to the BCPMG program between its inception in 1968 and 2007. Data were analyzed using descriptive statistics.
Number of referrals over time for a primary indication of schizophrenia
Number of referrals for a primary indication of schizophrenia over time were described in two ways. First, we studied the raw number of referrals for a primary indication of schizophrenia in 5-year increments. Second, we compared the annual number of referrals for a primary indication of schizophrenia to the total number of referrals to the BCPMG program between the years 1996–2007. Data for the total annual number of referrals to the BCPMG program prior to 1996 were unavailable.
The study was approved by the research ethics boards of the University of British Columbia, and British Columbia’s Children’s and Women’s Hospital.
RESULTS
A search of the BCPMG program database identified 596 charts, of which 308 were excluded: 23 could not be located, 33 revealed no mention of schizophrenia upon review, 82 were referred for evaluation to rule out a genetic syndrome and 170 were referrals in which schizophrenia was an incidental finding (of these, the first were referred between 1978–1982 (n=8) and a peak was found between 1983 and 1992 (89 charts)). The remaining 288 charts were referrals for a primary indication of schizophrenia. Of these, 263 individuals attended and 25 individuals did not attend their appointment.
Characterizing the population of individuals referred to the BCPMG Program for a primary indication of schizophrenia
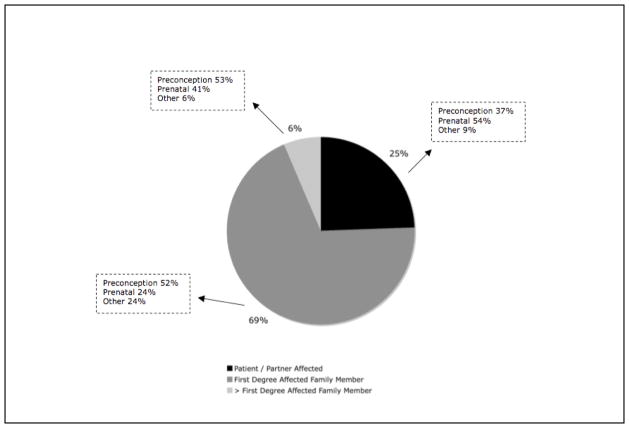
Most individuals referred to the BCPMG program for a primary indication of schizophrenia were Caucasian (61%) and lived within greater Vancouver (81%). The majority of referred individuals were female (86%). Most were not personally affected, but rather had an affected family member. Specifically, only 25% of referrals were for individuals who were personally affected, 69% (n=199) were for individuals who had an affected first-degree relative, and 6% were for individuals with an affected second degree or more distant relative. Proportions of females in the personally affected and unaffected groups were 90% and 87% respectively. The mean age of referred individuals was 31 years, ranging from infants to a 65 year-old individual. The majority of referrals (69%) were from family physicians. Referrals from obstetricians accounted for 9%, while those from psychiatrists accounted for 2%.
Most referrals were made for preconception counseling, rather than prenatal or non-pregnancy related genetic counseling as shown in Figure 1. A total of 32 referrals were made for adoption assessment; this indication accounted for the majority of referrals described as other in each category.
Figure 1.
Description of patients referred to BCPMG program and genetic counseling focus.
Number of referrals over time for a primary indication of schizophrenia
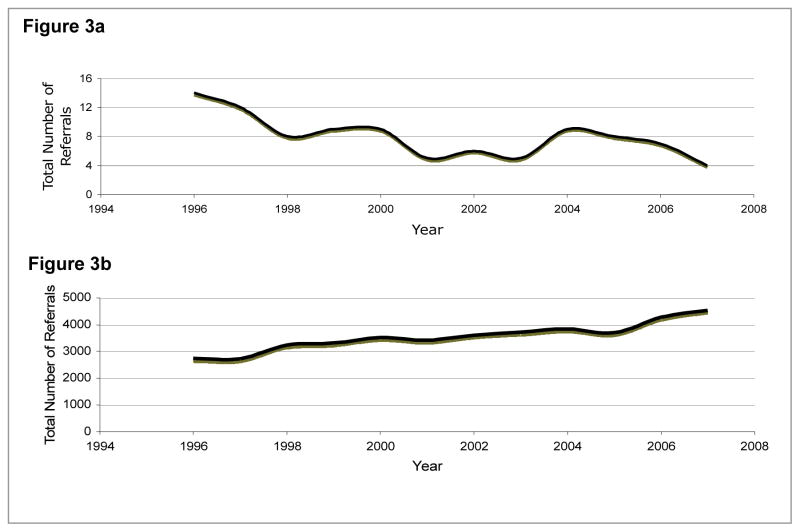
Trends in referrals to the BCPMG program for a primary indication of schizophrenia from 1968 until 2007 are described in 5-year increments in Figure 2. There was a peak in referrals between 1988 and 1992. In the most recent 5-year period studied (2003–2007), the BCPMG program received 33 referrals.
Figure 2.
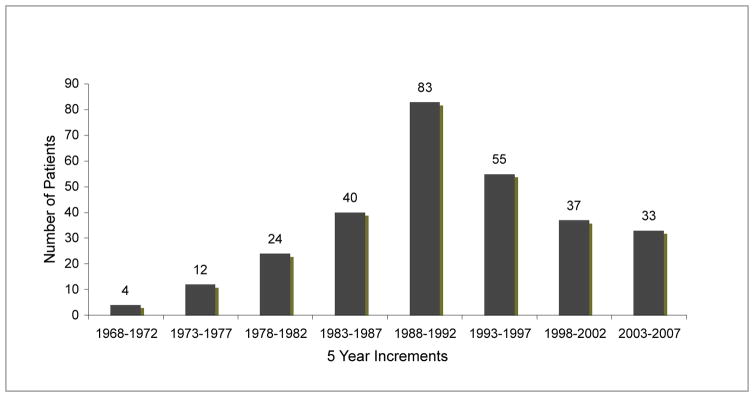
Referrals to the BCPMG program for a primary indication of schizophrenia described in 5-year increments from 1968 to 2007 (N=288).
Trends in number of referrals for a primary indication of schizophrenia compared to the total number of referrals to the BCPMG program over the past 12 years are described in Figure 3, panels (a) and (b), respectively. The annual number of referrals to the BCPMG program for a primary indication of schizophrenia has decreased over the past 12 years, while the total number of referrals has increased. Using the most recent data-point from 2007, referrals for a primary indication of schizophrenia constitute 0.09% of the total referrals to the BCPMG program, or approximately 1 referral per million British Columbia residents.
Figure 3.
Figure 3a Referrals to the BCPMG program for a primary indication of schizophrenia between 1996 and 2007.
Figure 3b Total number of referrals to the PMG program for a between 1996 and 2007.
DISCUSSION
One of the most striking findings of this study was the very small number of referrals for schizophrenia received by this regional genetics program, which serves the entire province of British Columbia. In the last 40 years, the BCPMG program has seen only 288 individuals for a primary indication of schizophrenia. The discrepancy between the number of referrals to the BCPMG program for schizophrenia and the number of affected individuals in the province is more striking in light of the interest in genetic counseling voiced by individuals with schizophrenia and their family members 6, 7. Schizophrenia is a common disorder, affecting ~1% of the population, thus there is an estimated 42,000 affected British Columbians. Each of these affected individuals have unaffected family members who may be interested in receiving genetic counseling too. Further, over the last 12 years (1996–2007), there has been a decrease in the raw annual number of referrals for schizophrenia, while the total number of annual referrals to the BCPMG program has increased. This trend is in direct disagreement with genetic counselor’s reported perception that psychiatric genetic counseling was an area of growth. Thus, although genetic counselors felt that number of referrals for psychiatric conditions would increase over time, it appears that – at least at this centre, until now - they have not. Although we are unable to draw definitive conclusions from these data regarding the mechanisms underlying the very low rate of referrals for this condition, potential explanations may include: lack of awareness (of affected individuals, family members of affected individuals, and health care professionals) about the relevance or availability of genetic counseling for schizophrenia; lack of awareness of mechanisms by which to access the service; stigma associated with psychiatric illness as a barrier to accessing the service; or provision of genetic counseling by other healthcare professionals (e.g. psychiatrists)9. Given that individuals with schizophrenia and their family members have previously reported interest in genetic counseling services, it seems likely that one of the main barriers is lack of awareness about mechanisms by which the service can be accessed, however, this area warrants future research.
The data regarding the number of referrals described in 5-year increments showed increasing number of referrals until 1988–1992, after which number declined. Aside from the possibility of stochastic variation, there are a number of potential explanations for the observed 1988–1992 peak in number of referrals. First, it is possible that the launch of the Human Genome Project in 1990 contributed to an increase in knowledge and awareness of genetics in both the medical community and the general public, and resulted in an increase in total referrals to the BCPMG program, including an increase in referrals for schizophrenia. Second, there were well-publicized findings in the late 1980s and early 1990s (including some from research by members of the BCPMG program) that linked a region of chromosome 5 to schizophrenia10, 11, which could have inspired an increase in number of referrals for genetic counseling for schizophrenia. Alternatively, perhaps the data is better conceptualized as a decline in number of referrals for schizophrenia post-1992. Specifically, it is possible that changes to the BCPMG program procedures (introduction of a telephone consultation service in (year) designed to field general genetics questions from the medical community) resulted in questions regarding recurrence risks for schizophrenia being handled by this service, such that physicians felt able to discuss these issues with their patients themselves, and made fewer referrals to the BCPMG program.
Most referrals for genetic counseling for schizophrenia in BC over the last 40 years were for first-degree relatives of individuals with schizophrenia, rather than for affected individuals themselves. Indeed, the number of referrals that were made for affected individuals themselves was very small. Accordingly, the most frequent source of referrals for psychiatric genetic counseling was family physicians, rather than psychiatrists. This suggests that perhaps genetic counseling services are being provided for affected individuals by psychiatrists. Indeed, recent work has shown that psychiatrists feel that addressing these issues falls in the realm of their clinical responsibilities8, 9. Alternatively, perhaps (as the popular conceptualization of genetic counseling is that it is a service primarily concerned with childbearing), few people with schizophrenia have been seen at the BCPMG program because there are few in BC who are having families. Related to this, perhaps the relevance of genetic counseling for individuals with schizophrenia who are not planning families is not clear. In this study, individuals were most frequently referred for preconception counseling rather than for prenatal or non-pregnancy related counseling. Taken together, these findings suggest that first-degree family members of individuals with schizophrenia and/or their physicians are aware that schizophrenia can “run in families”, and wish to learn more about the probability that offspring would be affected prior to embarking on having a family. This explanation for the current data is consistent with previous findings that first-degree family members of individuals with schizophrenia (a) are keen to learn more about genetics6,7, and (b) perceive the risk to their offspring to be a very important consideration, and may indeed make childbearing decisions based on their perceptions of this risk8. As we have already discussed, although most of the referrals for schizophrenia in this study were for first-degree relatives of affected individuals, the number were still very small.
Genetic services are traditionally conceptualized as being most relevant to pregnancy, so the fact that most referrals for a primary indication of schizophrenia were made for females likely reflects the fact that most individuals referred for genetic services in general, are female.
Limitations
Disruptions or alterations to the BCPMG program (e.g. healthcare worker strikes, implementation of the telephone service to answer questions of healthcare providers), may have affected trends in number of referrals. It is important to note that we did not assess all clinical genetics services relating to schizophrenia. For example, it is possible that number of physician-initiated lab consults for 22q11 deletion testing for individuals with schizophrenia changed over time. This question would be interesting to explore in future studies. Also, referrals were only identified for inclusion in this study during our search of the BCPMG program database if the word schizophrenia was included in the “diagnosis” field, and it is possible that some referrals for schizophrenia were not found because of human error in accidental omission of the ”diagnosis” field. Lastly, it may be difficult to extrapolate our findings to other geographical regions, which may have provided genetic counseling services for schizophrenia to populations with different characteristics, and where trends in referral numbers are different. This study paves the way for comparisons to be made between different regional programs.
Conclusion
To our knowledge, this exploratory study is the first reported investigation of numbers of referrals for, and characteristics of, individuals who have been referred for genetic counseling for schizophrenia. As such, it provides valuable insight into the actual clinical experience of one provincial medical genetics program’s provision of psychiatric genetic counseling services, and will provide a basis from which further research can be conducted. Specifically, we propose that there is a need for future research which focuses on exploring (a) barriers to psychiatric genetic counseling, (b) strategies to improve access and outreach to this population, and (c) the practices of other healthcare professionals’ (e.g. psychiatrists) relating to the provision of genetic counseling for schizophrenia.
Acknowledgments
The authors would like to thank Emily Morris for her assistance with data entry. Dr. Austin was supported by CIHR, the Michael Smith Foundation for Health Research, and the Provincial Health Services Authority of British Columbia.
Footnotes
Conflict of interest notification page.
The authors declare that they have no conflicts of interest related to this manuscript.
References
- 1.Finn C, Smoller J. Genetic Counseling in Psychiatry. Hav Rev Psychiatry. 2006;14(2):109–121. doi: 10.1080/10673220600655723. [DOI] [PubMed] [Google Scholar]
- 2.Mortensen PB, Pederesn B, Westergaard T, Wohlfahrt J, Ewald H, Mors O, Andersen PK, Melbye M. Effects of family history and place and season on birth on the risk of schizophrenia. N Engl J Med. 1999;340:603–608. doi: 10.1056/NEJM199902253400803. [DOI] [PubMed] [Google Scholar]
- 3.Lauren Tm, Labouriau R, Licht RW, Bertelsen A, Munk-Olsen, Mortensen PB. Family history of psychiatric illness as a risk factor for schizoaffective disorder. Arch Gen Psychiatry. 2005;62:841–848. doi: 10.1001/archpsyc.62.8.841. [DOI] [PubMed] [Google Scholar]
- 4.Austin JC, Honer WG. The potential impact of genetic counseling for mental illness. Clin Genet. 2005;67:134–142. doi: 10.1111/j.1399-0004.2004.00330.x. [DOI] [PubMed] [Google Scholar]
- 5.Turlington L, Moldin SO. Assessing the demand for psychiatric genetic counseling. Am J Hum Genet. 1994;55:A144. [Google Scholar]
- 6.DeLisi LE, Bertisch H. A preliminary comparison of the hopes of researchers, clinicians, and families for the future ethical use of genetic findings on schizophrenia. Am J Med Genet B Neuropsychiatr Genet. 2006 Jan 5;141B(1):110–5. doi: 10.1002/ajmg.b.30249. [DOI] [PubMed] [Google Scholar]
- 7.Lyus V. The importance of genetic counseling for individuals with schizophrenia and their relatives: Potential clients’ opinions and experiences. Am J Med Genet B. 2007 Dec 5;144B(8):1014–21. doi: 10.1002/ajmg.b.30536. [DOI] [PubMed] [Google Scholar]
- 8.Austin JC, Smith GN, Honer WG. The genomic era and perceptions of psychotic disorders: genetic risk estimation, associations with reproductive decisions and views about predictive testing. Am J Med Genet B Neuropsychiatr Genet. 2006 Dec 5;141B(8):926–8. doi: 10.1002/ajmg.b.30372. [DOI] [PubMed] [Google Scholar]
- 8.Finn CT, Wilcox MA, Korf BR, Blacker D, Racette SR, Sklar P, Smoller JW. Psychiatric genetics: a survey of psychiatrists’ knowledge, opinions, and practice patterns. J Clin Psychiatry. 2005 Jul;66(7):821–30. doi: 10.4088/jcp.v66n0703. [DOI] [PubMed] [Google Scholar]
- 9.Hoop JG, Roberts LW, Green Hammond KA, Cox NJ. Psychiatrists’ attitudes, knowledge, and experience regarding genetics: a preliminary study. Genet Med. 2008 May 16; doi: 10.1097/GIM.0b013e318177014b. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 10.McGillivray BC, Bassett AS, Langlois S, Pantzar T, Wood S. Familial 5q11.2----q13.3 segmental duplication cosegregating with multiple anomalies, including schizophrenia. Am J Med Genet. 1990 Jan;35(1):10–3. doi: 10.1002/ajmg.1320350103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bassett AS, McGillivray BC, Jones BD, Pantzar JT. Partial trisomy chromosome 5 cosegregating with schizophrenia. Lancet. 1988 Apr 9;1(8589):799–801. doi: 10.1016/s0140-6736(88)91660-1. [DOI] [PMC free article] [PubMed] [Google Scholar]