Abstract
Background:
With Sri Lanka aiming towards malaria elimination by 2015, the National Anti Malaria Campaign has stressed on the importance of identification of the species of Plasmodium either by examination of stained blood smears for malaria parasites or by Rapid Diagnostic Tests for malaria antigens before the initiation of treatment. This study aims at confirmation of the accuracy of clinical and/or microscopical malaria diagnosis using serology.
Materials and Methods:
Study population comprised 51 individuals diagnosed with malaria either microscopically or clinically during the first half of 2011. ELISA for detection of the two significant blood antigens (AMA-1 and MSP1-19) was carried out in these individuals, 14-28 days after being diagnosed as being positive for malaria microscopically.
Results:
ELISA confirmed the microscopic diagnosis in all 47 of the patients including two mixed infections which flagged positive for both parasite antigens. However, four individuals diagnosed clinically as being positive for P. vivax by Health Care Providers were negative for malaria antibodies by ELISA.
Conclusions:
With 175 cases of malaria reported in 2011, a formidable challenge exists to diagnose malaria positive blood smears due to the large number of negative blood smears being seen daily. After routine cross checking of positive slides, it is heartening to note that there were no false positives detected through serological assays amongst patients who were diagnosed as malaria positive by microscopy. Presumptive treatment of febrile patients with anti-malarials can lead to waste of resources and adversely impact the condition of the patient if the fever is not due to malaria.
Keywords: Clinical diagnosis, Diagnosis, Elimination, Malaria, Microscopy, Serology
INTRODUCTION
The National Malaria Elimination Program in Sri Lanka is targeting malaria elimination by the end of 2014, due to an annual parasite incidence (API) of <0.01 and a decline in the number of indigenous malaria cases since 2007. Therefore, diagnostic confirmation in every patient suspected of having malaria is critical, prior to the initiation of treatment. The National Anti malaria Campaign (AMC) has stressed on the importance of identification of the species of Plasmodium either by examination of Giemsa stained blood smears or by rapid diagnostic tests (RDT) (Carestart® Pf Combo kits) for antigens before treating patients with the relevant treatment suited for their specific infection. Thus those with Plasmodium falciparum malaria are treated with artemisinin combination therapy under a DOTS strategy and P. vivax malaria infection with chloroquine and primaquine at the recommended dose.
Antimalaria treatment may be delivered by both the public and private sectors in Sri Lanka. State sector curative services are provided through a series of healthcare institutions ranging from basic central dispensaries to teaching hospitals. Administration of antimalaria treatment on clinical suspicion is discouraged by the national guidelines for malaria treatment issued to all healthcare providers (HCPs), including those in the private sector.[1,2] The HCPs can opt to operate exclusively in the public or private sector or to work in the public sector from 8.00 am-4.00 pm and from then on see patients privately. Currently, Public Health Laboratory Technicians (PHLTs) based in government hospitals and Medical Laboratory Technologists working in private hospitals provide malaria diagnostic services within the country. RDTs can be requested from the Regional Malaria Officer (RMO) of each district for confirmation of diagnosis. This study aims to confirm the accuracy of clinical and laboratory malaria diagnosis by estimating the antibody titers against two key malaria antigens of P. falciparum and P. vivax, apical membrane antigen (AMA)-1 and merozoite surface protein (MSP) 1-19 which are present during the blood stage in the human host.
MATERIALS AND METHODS
The study population comprised patients diagnosed with malaria either microscopically or clinically during the period January-June 2011. In the presence of a PHLT, microscopy was used to confirm diagnosis and antimalarial treatment was initiated by the HCPs based on the results. In instances where microscopic diagnosis of malaria was not feasible, treatment for malaria was initiated based on clinical diagnosis and the RMO notified based on the circular issued by the AMC on the need to report all clinically diagnosed malaria infections.[2]
As part of this study, blood was collected for determining the presence of antimalaria antibodies from individuals who were diagnosed with malaria (microscopically or clinically) within 14-28 days after such diagnosis. Whole blood was stored at 4°C until it could be transported to a central laboratory. After preliminary analysis of the samples, they were stored at –80°C and couriered on dry ice to the National Institute for Biological Standards and Control, UK for estimating the presence of antibodies against P. falciparum and P. vivax AMA-1 and MSP1-19 antigens to determine accuracy of clinical and laboratory diagnosis. The collaborator in the United Kingdom was blinded to the results of the PHLT and HCPs. Enzyme-linked immunosorbent assay (ELISA) was performed by loading all serum samples on to plates in chronological order. Both AMA-1 and MSP1-19 antigens were bound on separate plates before loading of patient samples. Titers were read accordingly.
The past history of malarial infection and sociodemographic data was obtained from each individual.
RESULTS
Results of the tests carried out for malaria diagnosis
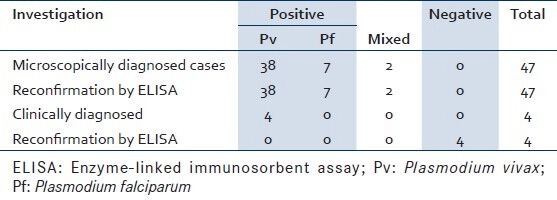
During the study period, 47 individuals were diagnosed as being positive for malaria by microscopy (38 Plasmodium vivax, seven P. falciparum, and two mixed infections). Four individuals were diagnosed as having malaria (P. vivax malaria) by HCPs based on the clinical manifestations at presentation. One of the HCPs was a government employee carrying out private practice after office working hours and the other three were full-time private practitioners. ELISA confirmed the microscopic diagnosis including the two P. vivax, P. falciparum mixed infections by displaying a positive reaction for mixed parasite antigen. However, all four individuals diagnosed clinically as being positive for P. vivax by HCPs were negative for malaria antibodies by ELISA [Table 1].
Table 1.
Results of tests performed for malaria diagnosis
Epidemiological characteristics of the malaria positive patients
Majority of the patients diagnosed with malaria were males (74%). The mean age was 30.15 for males and 27.74 for females. The highest number of cases (27.7%) was reported from the Mannar district in the Northern Province and 25.5% reported from Colombo. Of the 12 cases diagnosed in Colombo, 50% of the infections were acquired abroad as compared to Mannar where of the 13 patients diagnosed with malaria only one had acquired the infection overseas. The district of origin of the malaria positive patients included in this study is given in Table 2.
Table 2.
Characteristics of the population of individuals confirmed as having malaria
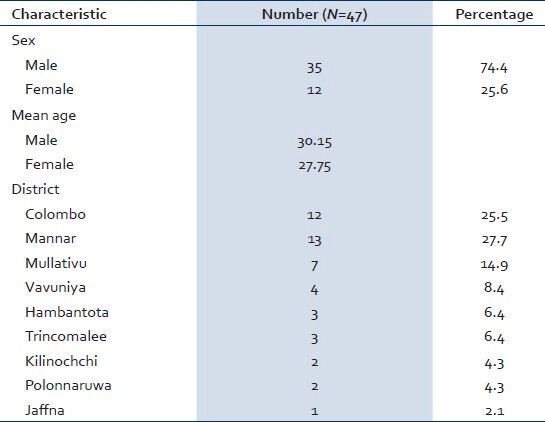
The four clinically diagnosed cases of malaria were male civilians reported from high malaria endemic areas in the Northern Province (one Kilinochchi, one Mannar, and two Mullativu). These individuals were in the age range of 25-45 years.
Treatment of patients with malaria
Patients diagnosed microscopically and clinically were treated with appropriate antimalarials according to the national malaria guidelines.
DISCUSSION
Accurate diagnosis of individuals infected with Plasmodium species using microscopy is a challenge to any country which has entered the elimination phase. Fever and parasite surveillance are the key strategies of the elimination program in Sri Lanka. With the official launch of the Malaria Elimination Program on the 3rd of June 2010, the Sri Lankan government has focused heavily on active surveillance and the need to refer any patient with signs and/or symptoms of malaria for confirmation of diagnosis by microscopy. The absolute need for rational therapy during the phase of elimination places increasing importance on the accuracy of malaria diagnosis.[3]
Sri Lanka has a well-developed laboratory network with a PHLT being placed at especially dedicated malaria-only screening laboratories in approximately 350 medical institutions in the country. The PHLTs whose training institute is the National Institute of Health Science are trained on the diagnosis of malaria, filariasis, tuberculosis, leprosy, and sexually transmitted diseases over a period of two years and this training includes a 6 months training on Giemsa stained malaria microscopy at the AMC. Activated passive case detection (APCD) takes place at these malaria only screening laboratories with HCPs referring patients with signs and/or symptoms of malaria for confirmation of diagnosis. APCD capacity increased in the late 1990s by a near doubling of the number of PHLTs in district hospitals.[4]
During the study period, only four clinically diagnosed malaria cases (which accounts for 7.8% of the cases diagnosed during this period) treated with antimalarials were reported to the RMOs of the Northern Province. While this accounts for 7.8% (4/51) of the cases diagnosed, based on the information received it was possible to follow-up the patients and confirm the diagnosis with serology. As vivax malaria was suspected, the patients had only been treated with chloroquine, which should be prevented at all cost as primaquine treatment is essential for a 14-day period to prevent relapses. Following the end of the 30 year civil war in the Northern Province, which led to destruction of hospitals and roads, it is possible that a considerable proportion of patients continue to seek treatment from the private sector and are clinically diagnosed and treated by private HCP. All such cases may not be reported to the respective RMOs, and thereby it is difficult to assess the contribution of the private sector towards malaria diagnosis, treatment, and actual case load of malaria in the country.
Treatment based on clinical manifestations without evidence of malaria parasitemia, results in poor management of patients. Misdiagnosis of malaria also carries the risk of under diagnosis of infections that mimic malaria symptoms, jeopardizing the patient’s health as the actual cause of fever remains untreated. Furthermore, in an era where a dengue epidemic is raging in Sri Lanka with 28,458 cases and 186 deaths reported during this period (January-June 2011),[5] there is a possibility of not subjecting the individual to tests that are confirmatory for dengue resulting in a deterioration of the patient’s condition. Incorrect diagnosis and reporting of clinically diagnosed false positives carry an additional challenge for the surveillance system due to the unnecessary waste of precious resources.
HCPs of both the government and private sector have been informed of the need to diagnose malaria prior to treatment in a circular issued by the Ministry of Health in 2008.[2] Due to the wide publicity given by the AMC with the assistance of Independent Medical Practitioners Association, the largest single association of private HCPs in the country, the number of clinically diagnosed malaria cases remains low in the country. In order to enhance reporting of a malaria case, especially by the private sector, the AMC has embarked on a novel toll free self-reporting system utilizing the high availability of mobile phones. A web-based surveillance mechanism is also in place to report clinically diagnosed cases electronically. However, the facility remains underutilized.
Reemergence of malaria due to imported infections in Sri Lanka is currently a threat to the National Malaria Elimination Program.[6,7] This is evident with the number of indigenous malaria cases declining since 2008 and an increase in the number of imported malaria cases. Imported malaria is defined as a case of malaria which has been acquired in another country and diagnosed in Sri Lanka by a blood smear examination and/or RDT.[6] As a majority of imported infections are being detected outside the traditional malaria zones such as the district of Colombo, a formidable challenge exists for the PHLTs in malaria non-endemic areas to diagnose malaria in spite of the large number of negative blood smears being seen daily as each PHLT is expected to examine approximately 40-50 blood smears for malaria parasites per day.
Emphasis needs to be placed to increase awareness among HCPs (both government doctors, most who engage in private practice after 4 pm and private HCPs) working in malaria endemic and non-endemic areas of the country on the need to test any patient presenting with clinical symptom or signs of malaria by microscopy or RDT at the nearest government hospital/AMC headquarters. This should include those who have a history of travel to a malaria endemic country within the past 1 month. The use of RDTs as a diagnostic tool to confirm malaria in the private sector or in government hospitals where trained PHLT may be unavailable is one of the pillars to attain 100% surveillance and consequently elimination. In keeping with the global guidelines, this will ensure appropriate treatment.[8]
CONCLUSIONS
In a country with a low prevalence of malaria, where microscopy is the main method used for diagnosis, it is heartening to note that there were no false positives diagnosed. The sustainability of the infrastructure available for malaria diagnosis, advocacy, enhanced surveillance, and refresher training of HCPs by the AMC through continuous medical education with the funds received from the Global Fund to fight AIDS, tuberculosis, and malaria must be guaranteed so that the goal of eliminating malaria by the end of 2014 is fulfilled.
Limitations
Due to the low number of positive cases being reported from the country, this study focused on the accuracy of Giemsa stained malaria microscopy available in the country and on the accuracy of clinical diagnosis when used for diagnosing and treating febrile patients in an elimination setting. Excluding one person from the armed forces, the study did not include any of the malaria positive patients diagnosed amongst the military as it was not possible to collect serum for confirmation of diagnosis after 14-28 days.
ACKNOWLEDGEMENTS
The authors would like to thank the Regional Malaria Officers who assisted in collection of blood from patients diagnosed as being positive for malaria for this study.
Footnotes
Source of Support: Grant received from the Global Fund to eliminate AIDS, tuberculosis, and malaria (through Sarvodaya Secretariat, Principal Recipient PR2) is gratefully acknowledged.
Conflict of Interest: None declared.
REFERENCES
- 1.Anti Malaria Campaign Sri Lanka. 2012. [Last accessed on 2012 Nov 11]. Available from: http://www.malariacampaign.gov.lk/Precentation/NewCaseDetection.aspx .
- 2.National guidelines for treatment of malaria. Colombo: Office of the Director General of Health Services; 2008. Ministry of Healthcare and Nutrition. General Circular No 01-14/2008. [Google Scholar]
- 3.Strategic Plan for the Elimination of Malaria 2008-2012. Colombo: Anti-Malaria Campaign, Sri Lanka; 2008. Anti-Malaria-Campaign. [Google Scholar]
- 4.Abeyasinghe RR, Galappaththy GN, Smith Gueye C, Kahn JG, Feachem RG. Malaria control and elimination in Sri Lanka: Documenting progress and success factors in a conflict setting. PLoS One. 2012;7:e43162. doi: 10.1371/journal.pone.0043162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Epidemiological Unit, Ministry of Health. Quarterly Epidemiological Report. 2011. [Last accessed on 2012 Nov 20]. Available from: http://www.epid.gov.lk/web/index.php?option=com_content&view=article&id=164%3Aquarterlyepidemiological-report-2011&catid=50%3Aqeb&lang=en .
- 6.Galappaththy GN, Fernando SD, Abeyasinghe RR. Imported malaria: A possible threat to the elimination of malaria from Sri Lanka? Trop Med Int Health. 2013;18:761–8. doi: 10.1111/tmi.12097. [DOI] [PubMed] [Google Scholar]
- 7.Wickramage K, Galappaththy GN. Malaria burden in irregular migrants returning to Sri Lanka from human smuggling operations in West Africa and implications for a country reaching malaria elimination. Trans R Soc Trop Med Hyg. 2013;107:337–40. doi: 10.1093/trstmh/trt009. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. Guidelines for the treatment of Malaria. 2nd ed. 2010. [Last accessed on 2012 Nov 20]. Available from: http://whqlibdoc.who.int/publications/2010/9789241547925_eng.pdf .


