Abstract
Context:
Early intervention in specific learning disability (SpLD) results in better outcome and prevents comorbidity. Understanding the pathways is therefore important.
Aims:
To study and compare the pathways to care for children with SpLD and mental retardation (MR) before reaching a tertiary care center.
Settings and Design, Material and Methods:
A cross-sectional study was conducted for pathways to care of two groups: SpLD and MR with 50 children in each group from 8 to 16 years. MINI-KID for comorbidity and Goldberg's pathway to care instrument was used. The groups were divided into early contact (up to three carers) and late contact (more than three carers) and compared.
Statistical Analysis:
Data were analyzed using Statistical Packages for Social Sciences (SPSS) version 10.0 software.
Results:
Majority (n = 24 or 48%) of SpLD children visited “others” (teachers, neighbors, relatives, and guardians of fellow classmates) as first carer. Allopathic practitioners were the first choice for MR children (n = 31 or 62%). Six children (12%) in SpLD group and 10 of MR (20%) group have seen either traditional practitioner or healer as first carer. Maximum referral to the tertiary center in both groups was done by others (62% in SpLD and 56% in MR group). Early contacts in SpLD group belonged to younger age group (P = 0.01). While comparing both groups on the basis of early and late contact, mother's education was found to be significant in early contact group (P = 0.036) and having comorbidity was significant among late contacts (P = 0.038).
Conclusions:
The pathways to care for SpLD children are more or less similar to MR children whose parents recognize MR late. Both the groups visit multiple carers including traditional healers substantiating the strong belief for supernatural causation of developmental disorders in India.
Keywords: Care, mental retardation, pathways, specific learning disability
INTRODUCTION
Specific learning disability (SpLD) is a hidden disability. Untreated SpLD can lead to school refusal, conduct, and substance abuse disorder.[1] The earlier the children with SpLD were identified and intervened, the less severe their problems are likely to be.[2] Phonologically mediated reading intervention has shown improvement in reading fluency.[3] Mental retardation (MR) is usually recognized by delaying development milestones or abnormal facial features.[4] However, mild MR may go unnoticed.[5]
The present study was undertaken to understand the pathways and barriers. Taking minimum age criteria of 8 years, it also attempted to identify sources of delay for children with MR who fail to seek early care. We compared the two pathways to detect any significant difference between the two.
MATERIALS AND METHODS
The study was conducted in a tertiary care hospital for mental health and neurological ailments in India. The subjects for the study were selected by purposive sampling method. The children who were worked up in detail for SpLD and MR and then referred to Clinical Psychology Department for LD and intelligent quotient (IQ) assessment and those who fulfilled the selection criteria formed the subject group. National Institute of Mental Health and Neuro Sciences (NIMHANS) index of SpLDs was used for LD assessment, while IQ was measured using various standard scales. The study was approved by the ethical committee of the institute. Informed consent and assent (wherever possible) was taken.
Two groups were created for the purpose of study: 1) SpLD Group and 2) MR Group. Each group consists of 50 subjects of both sexes with chronological age from 8 to 16 years. We took minimum age criteria as 8 years because SpLD cannot be conclusively diagnosed before 8.[6] Children with at least one reliable guardian were selected, as our study was based on history taken from the past. Children with overt neurological illness were excluded as this might contribute to bring them early for tertiary care. For MR group, children with IQ less than 70 were included as per International Classification of Diseases (ICD)-10 criteria.[7] Comorbid autism was excluded. A detailed history and sociodemographic data were taken. The children were then interviewed using MINI-KID for presence of any comorbid axis I disorder.[8] To understand the pathways, we have used Pathways to Care Instrument devised by Goldberg and Huxley.[9] For our study, we have modified and excluded certain questionnaires which were not relevant in developmental disorders. The data were analyzed using the Statistical Packages for Social Sciences (SPSS) version 10.0 software.[10] A P-value of <0.05 was considered statistically significant.
RESULTS
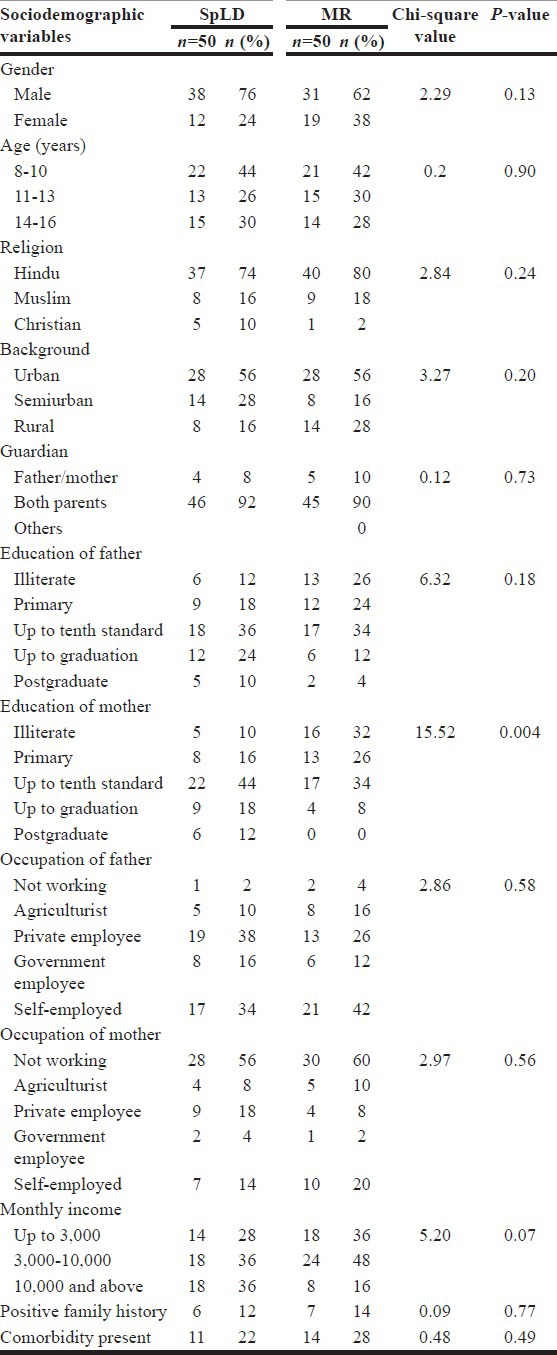
Table 1 shows the sociodemographic pattern of both SpLD and MR groups. Both the groups did not differ significantly except mother's education which was less in MR group (P = 0.004).
Table 1.
Sociodemographic characteristics
The pathways followed by the SpLD and MR children have been depicted in Figures 1 and 2, respectively. Most of SpLD children's parents (n= 24 or 48%) consulted “others” (which include teachers, neighbors, relatives, and guardians of fellow classmates) as first contact and this group referred the maximum cases to our tertiary center (n = 31 or 62%). Next source of referral were the allopathic practitioners whom 20 (40%) children contacted first. Traditional healers (religious and faith healers) were favorites for four (8%) children and nine (18%) children consulted them after seeing others. For two children (4%), traditional practitioners (which include homeopathic, ayurvedic or unani practitioner) were the first carer. Fourteen children (28%) sought consultation from others after visiting allopathic practitioners while nine (18%) did the opposite [Figure 1].
Figure 1.
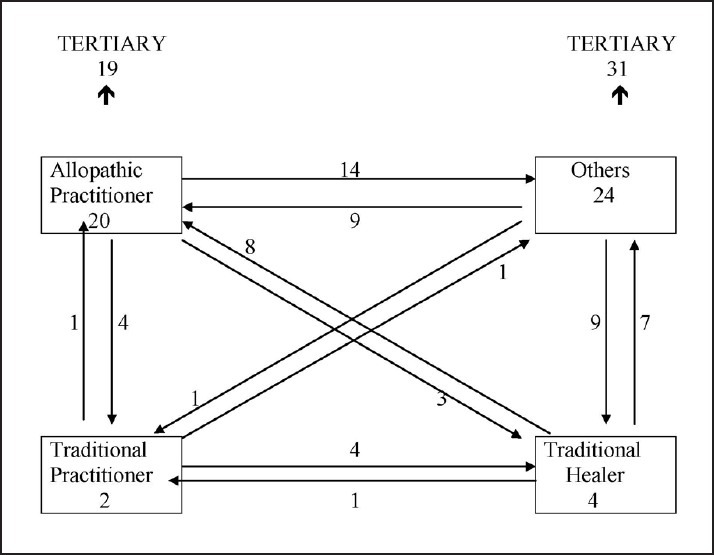
Specific learning disability (SpLD) pathways
Figure 2.
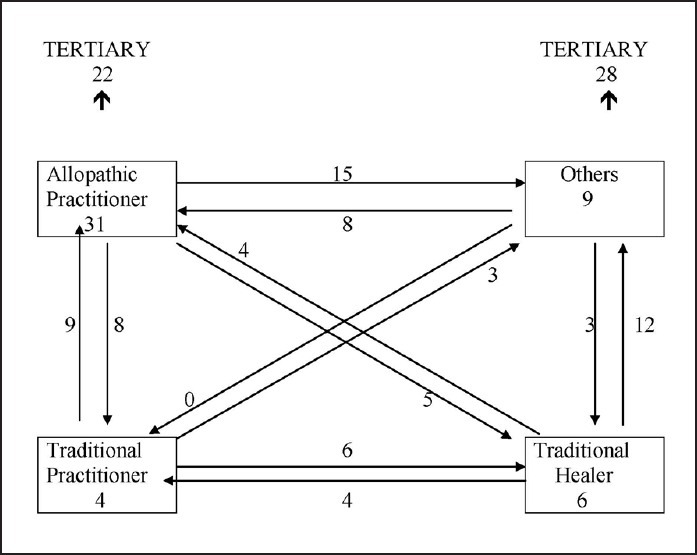
Mental retardation (MR) pathways
For MR children, allopathic practitioners were the first choice for 31(62%). However, they constitute 44% (n = 22) of source of referral as 56% (n = 28) were referred by others. Fifteen children (30%) went to “others” from allopathic doctors, while eight children (16%) did the opposite. Parents of six children (12%) favored traditional healer, while four children (8%) preferred traditional practitioner as primary carer [Figure 2].
Table 2 shows the comparison between early and late contact to the tertiary center for SpLD group. Early contact was defined as those who came to our tertiary care center after visiting less than or equal to three carers. For more than three carers, it is late contact. This cut-off point of three carers was decided taking the median value. Twenty-six (52%) SpLD children contacted early, while 24 (48%) came late. Children in the age group of 8-10 years were brought to the center early, while those belonging to 14-16 years age group came late. The difference is statistically significant (P = 0.01). There is no significant difference between the two groups on background, education and occupation of parents, monthly income, positive family history, or comorbidity (P > 0.05).
Table 2.
SpLD correlation between sociodemographic data and pathways to care
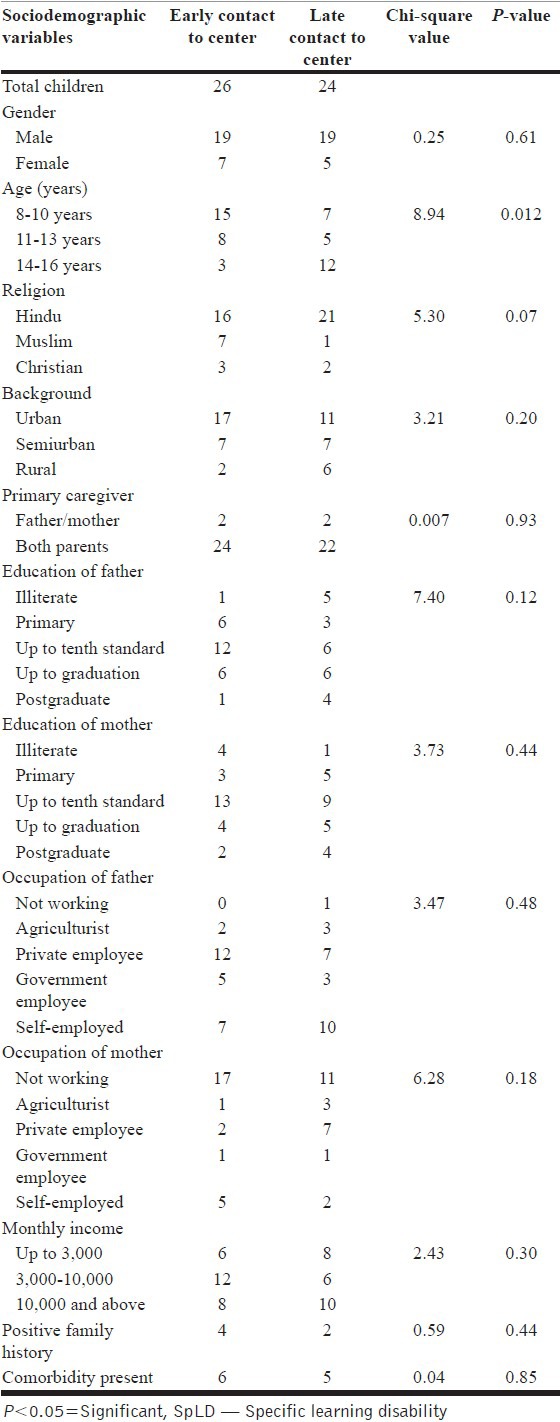
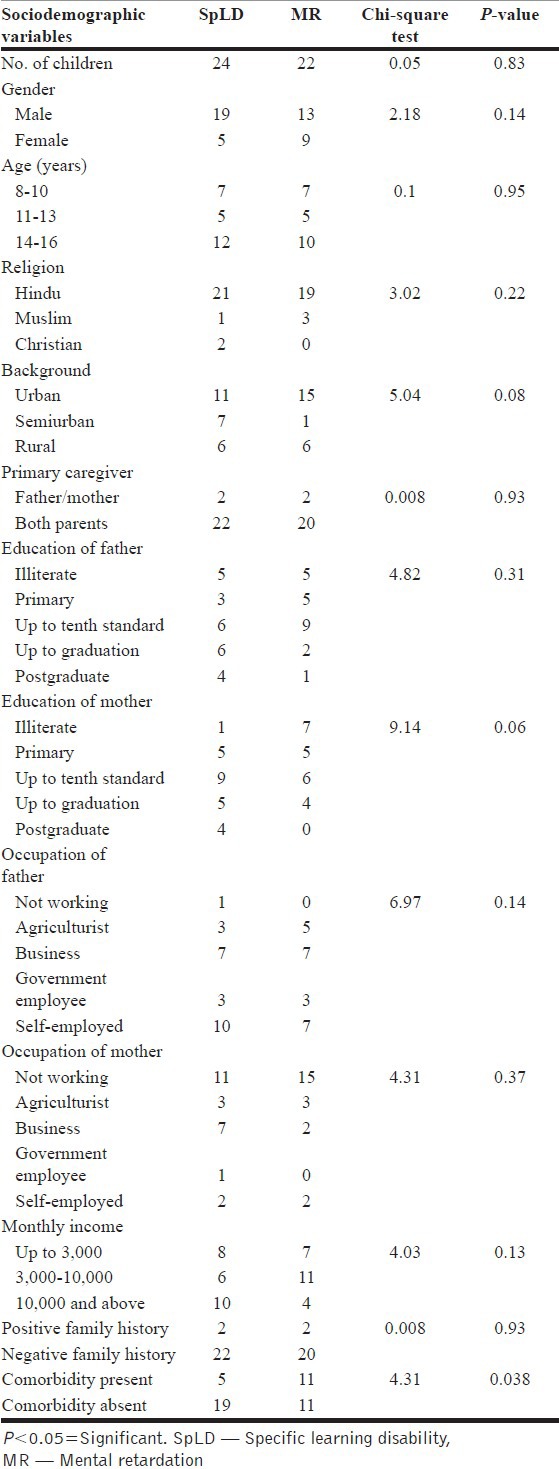
Tables 3 and 4 shows the comparison between SpLD and MR group on the basis of early and late contact. Twenty-six children in SpLD group and 28 in MR group had early contact, while 24 SpLD children and 22 MR children came late. The early contact group differed significantly on education of mother, where six out of 26 mothers in SpLD group had minimal graduate qualification and none had such in MR group (P = 0.036). The late contact group had statistically significant difference on psychiatric comorbidity as 11 out of 22 in MR group had a psychiatric comorbidity compared to five out of 24 in SpLD (P = 0.038).
Table 3.
Comparative chart of children who get early contact: SpLD vs MR
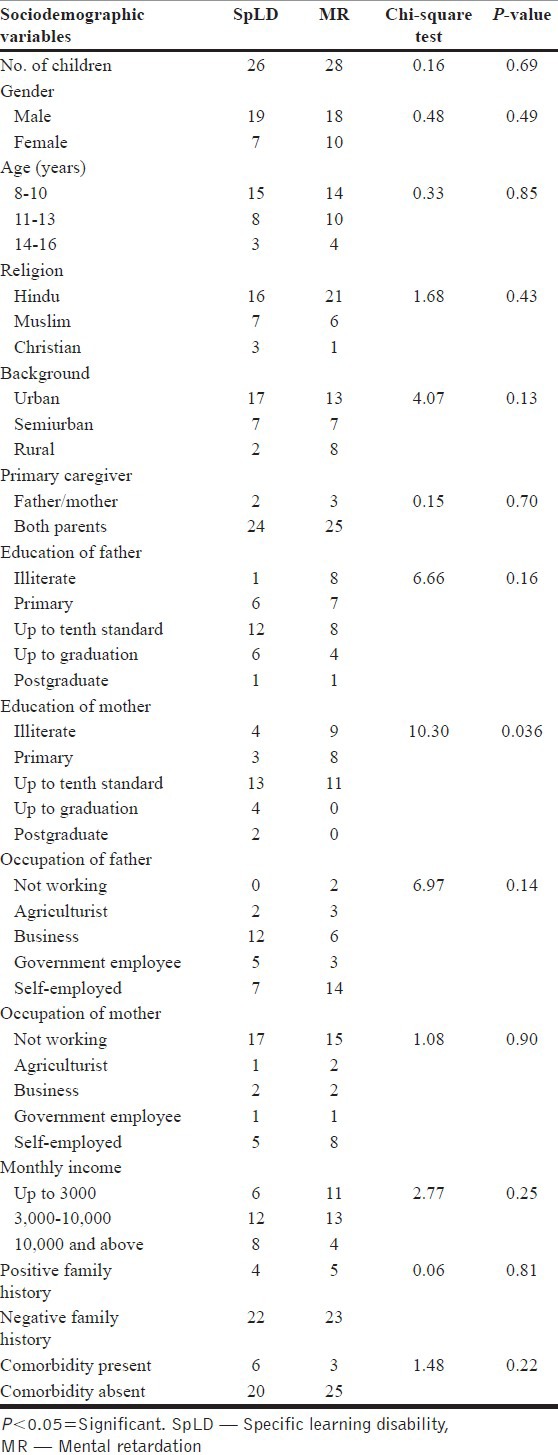
Table 4.
Comparative chart of children who get late contact: SpLD vs MR
We also observed other interesting findings (not shown in the tables). Majority of the SpLD children were in fourth standard (24%) followed by ninth standard (18%) when they contacted us. The mean time to see the first carer and tertiary carer was 1.08 and 3.39 years, respectively. For majority (74%), curriculum was state syllabus and medium of instruction was English. Majority (64%) of SpLD children presented with poor academics, while 14% with symptoms of comorbidity. Parents of 23 (46%) children were not aware of the facility available in this tertiary care hospital, 15 (30%) were hoping for spontaneous resolution, eight (16%) had lack of faith in allopathic system, and four (8%) mentioned stigma as the reason for coming late. In the MR group, 43(86%) had mild MR and main presenting feature was poor intelligence (32%) followed by symptoms of comorbidity (22%).
DISCUSSION
The pathways followed by SpLD children matches with mentally retarded children of older age group. Both visit multiple carers which include traditional practitioner, healers, and allopathic practitioner. Teachers, friends, neighbors, relatives, and guardians of other children (included under “others”) play a crucial role in guiding to the right center. Role of teachers assumes significance as they form the majority of the “others” group. SpLD children who come early for care are of younger age group. Having a positive family history or comorbidity does not bring them early to the proper carer. SpLD children seek help early when their mothers are well-educated. Older children with MR seek help when comorbid symptoms start appearing.
Majority of SpLD children's parents preferred “others” of which teachers were the major constituent. The role of teachers is crucial in pathways to care for child and adolescent psychopathology.[11] Altogether 46 out of 50 children (92%) took other's support before reaching the tertiary center. They referred the maximum children to the center. Several pathways of care studies in adults have reported this group to be major referring agency.[12] We found similar pattern of referral in children also. Many parents revealed about awareness being created by television (TV) programs. The fact that 14 children (28%) came to “others” after seeing allopathic practitioner highlights their significance in help seeking.
In MR group, it is again “others” who did the maximum referral (56%). A similar trend to see “others” after consulting allopathic doctors was seen. This is not an unexpected finding since we included MR children from 8 years onwards and majority (86%) of them were of mild category. Parents seemed to be confused about nature of problem and whom to approach.
Six children in SpLD group and 10 of MR group have seen either traditional practitioner or healer as first carer [Figures 1 and 2]. While 22 SpLD children met them as subsequent carer, 26 did so in MR group. This is an important finding of our study which shows that there is not much difference in pattern of seeking help between the groups. Many parents of SpLD children perceived the problem as poor intelligence and opted for alternative care. Parents of SpLD children took their children to temples where priests touched the tongue with divinely blessed rice grains as a mode of cure. The sprinkling/ingestion of holy water and chanting mantra was also reported. Help seeking pattern in developmental disorders depend on the cultural model of illness prevailing in that region.[13] A belief regarding supernatural causation of illness will promote help seeking from traditional means, and biological causation about psychiatric disorder will favor help seeking behavior from a professional.[14] An earlier Indian study found that parents failed to understand the biological basis of SpLD even after exposure to educational intervention.[15]
The SpLD children who made early contact were of younger age group. Interestingly, we did not find any significant correlation between positive family history, comorbidity, and urgency of seeking care in contrast to other care pathways studies in children.[16]
While comparing the two groups (SpLD and MR) on early and late contact, mother's education was found to be a significant factor in seeking help early. Our finding is in accordance with a 10-year follow-up study of learning disabled students in USA.[17] Also, MR children who came late had more psychological comorbidity. In our study, majority was mild MR and main presenting features were poor intelligence and symptoms of comorbidity. It is apparent that parents sought specialized care only when these children developed behavioral problem and were difficult to manage. This matches the views expressed by authors of an earlier study done in India.[18] Finally, factors like unawareness of facility, hope for spontaneous resolution, stigma of coming to a psychiatric hospital, and more faith in traditional cure methods dithered them from seeking intervention from tertiary care center.
Majority of SpLD children were in fourth and ninth standard at the time of contact. The bimodal peak could be because it is during fourth standard period when children “read to learn” and deficit becomes apparent. The second peak at ninth standard is when pressure to perform in the first board examination makes parents to bring the children for proper care. There was also a considerable time lag between problem perceived by parents and care sought. However, the mean delay in diagnosis in our study (3.39 years) is better than an earlier Indian study which found the delay to be 5.8 years.[19]
To our knowledge, this study is the first of its kind on help seeking pattern of children with SpLD in Indian context. The strength of our study is that it has taken subjects as SpLD or MR diagnosed on standard scales by qualified psychologists. The limitation is that it was conducted in a tertiary level center and the findings may not reflect the attitude of general population.
Findings from our study substantiate the role of teachers as gatekeepers. It implicates that teachers should be trained about presenting features of learning disability, when to suspect it. Our second suggestion is to create awareness through electronic and print media. Films like “Tare Zameen Par” were successful in conveying these messages. Topics on SpLD can be discussed during parent-teacher meetings. Finally, strengthening collaboration between traditional practitioners, general practitioners (GPs), pediatricians, neurologists, and mental health professionals would help in removing the unnecessary delay in referral.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Benasich AA, Curtiss S, Tallal P. Language, learning, and behavioural disturbances in childhood: A longitudinal perspective. J Am Acad Child Adolesc Psychiatry. 1993;32:585–94. doi: 10.1097/00004583-199305000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Torgerson CJ, Elbourne D. A systematic review and meta-analysis of the effectiveness of information and communication technology (ICT) on the teaching of spelling. J Res Read. 2002;25:129–43. [Google Scholar]
- 3.Shaywitz BA, Shaywitz SE, Blachman BA, Pugh KR, Fulbright RK, Skudlarski P, et al. Development of left occipitotemporal systems for skilled reading in children after a phonologically-based intervention. Biol Psychiatry. 2004;55:926–33. doi: 10.1016/j.biopsych.2003.12.019. [DOI] [PubMed] [Google Scholar]
- 4.Girimaji SR, Srinath S, Seshadri SP. A clinical study of Infants presenting to a mental retardation clinic. Indian J Pediatr. 1994;61:373–8. doi: 10.1007/BF02751893. [DOI] [PubMed] [Google Scholar]
- 5.Boyle CA, Yeargin-Allsopp M, Doernberg NS, Holmgreen P, Murphy CC, Schendel DE. Prevalence of selected developmental disabilities in children 3-10 years of age: The metropolitan Atlanta developmental disabilities surveillance program. MMWR CDC Surveill Summ. 1996;45:1–14. [PubMed] [Google Scholar]
- 6.Shaywitz SE. Dyslexia. N Engl J Med. 1998;338:307–12. doi: 10.1056/NEJM199801293380507. [DOI] [PubMed] [Google Scholar]
- 7.Geneva: WHO; 1994. World Health Organisation: International classification of diseases and related health problems: ICD-10. [Google Scholar]
- 8.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 9.Goldberg DP, Huxley P. London: Tavistock press; 1980. Mental illness in the community: The pathways to psychiatry care. [Google Scholar]
- 10.USA: SPSS Incorporate; 2007. Statistical Package for Social Sciences. SPSS version 10.0. [Google Scholar]
- 11.Stanger C, Lewis M. Agreement among parents, teachers, and children on internalizing and externalizing behavior problems. J Clin Child Psychol. 1993;22:107–15. [Google Scholar]
- 12.Lahariya C, Singhal S, Gupta S, Mishra A. Pathways of care among psychiatric patients attending a mental health institution in central India. Indian J Psychiatry. 2010;52:333–8. doi: 10.4103/0019-5545.74308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kleinman A. USA: University of California Press; 1980. Patients and healers in the context of culture: An exploration of the borderland between anthropology, medicine and psychiatry. [Google Scholar]
- 14.Jorm AF. Mental health literacy: Public knowledge and beliefs about mental disorders. Br J Psychiatry. 2000;177:396–401. doi: 10.1192/bjp.177.5.396. [DOI] [PubMed] [Google Scholar]
- 15.Karande S, Mehta V, Kulkarni M. Impact of an education program on parental knowledge of specific learning disability. Indian J Med Sci. 2007;61:398–406. [PubMed] [Google Scholar]
- 16.Gasquet I, Ledoux S, Chavance M, Choquet M. Consultation of mental health professionals by French adolescents with probable psychiatric problems. Acta Psychiatr Scand. 1999;99:126–34. doi: 10.1111/j.1600-0447.1999.tb07210.x. [DOI] [PubMed] [Google Scholar]
- 17.Hartzell HE, Compton C. Learning disabilities: 10-years follow-up. Pediatrics. 1984;74:1058–64. [PubMed] [Google Scholar]
- 18.Purakayastha M, Girimaji SR, Srinath S, Seshadri SP. Research endeavours in Child and adolescent psychiatry in India Published by Dr Rajendra Hegde 4th Biennial IACAMH Conference; Clinical profile in mental retardation: NIMHANS Experience. [Google Scholar]
- 19.Karande S, Satam N, Kulkarni M, Sholapurwala R, Chitre A, Shah N. Clinical and psychoeducational profile of children with specific learning disability and co-occurring attention-deficit hyperactivity disorder. Indian J Med Sci. 2007;61:639–47. [PubMed] [Google Scholar]


