Abstract
Background:
Insomnia is a common sleep disorder, characterized by difficulties in sleep initiation, sleep maintenance or early morning awakening. Although polysomnography (PSG) is a standard method in the evaluation of sleep disorders, it is not recommended for routine use in the clinical assessment of insomnia. Instead, standard questionnaires could be used in the primary evaluation of insomnia.
Objective:
The main object of this study was to compare the type and severity of patients’ subjective complaints of insomnia gathered from insomnia severity index (ISI) questionnaire with the result of their polysomnographic evaluation.
Materials and Methods:
In this cross-sectional study conducted during 2010-2011 in Iran, all patients in one clinic with sleep disorders were evaluated. The study consisted of self-administered questionnaires completed by participants to provide information on demographic characteristics and ISI questionnaire. After completing the questionnaire, all the participants underwent standard overnight PSG.
Results:
Subjects were 151 patients (47.2 ± 10.8 years old). The average ISS was 6.1 ± 4. There was a significant relationship between the subjective complaint of difficulty in sleep initiation and sleep onset latency in PSG (r = 0.5, P < 0.001). Furthermore, there was a correlation between the subjective complaint of difficulty in sleep maintenance and number of awakening in PSG (r = 0.19, P = 0.01). A low patients’ satisfaction from their sleep was associated with lower total sleep time (r = −0.2, P = 0.02) and a lower percentage of rapid eye movement (REM) sleep in their PSG study (r = −0.25, P = 0.002). No relation was found between patients’ satisfaction and sleep efficiency measured with PSG (r = −0.04, P = 0.6).
Conclusions:
Our findings suggest that objective insomnia, measured with ISI, is related with PSG variables and ISI could be a useful tool to quantify perceived insomnia severity. Further studies are needed to determine the sensitivity and specificity of this questionnaire.
Keywords: Insomnia, insomnia severity index, polysomnography
INTRODUCTION
Insomnia is one of the most common sleep disorders world-wide. It is most often defines as the presence of any of following four major criteria: Difficulty in initiating or maintaining sleep, early morning awakening and non-restorative sleep. In order for insomnia to be present, the above difficulties must occur despite adequate opportunity and time for sleep.[1,2]
The reported prevalence of insomnia in the epidemiological studies depends upon the definition used, the populations whose been studied and whether chronic versus intermittent or acute insomnia were assessed. According to a general consensus which has developed from population-based studies in different countries, approximately 30% of adults have one or more of the above mentioned four major insomnia diagnostic criteria.[3,4,5]
Cognitive, physical and psychological consequences of insomnia lead to impaired individual's work performance and quality-of-life and indicate the importance of early recognition and treatment of it.[6]
There are several objective and subjective assessment tools for measuring sleep disorders, among which polysomnography (PSG) is the gold standard.[7,8,9] Considering bothersome and time consuming accomplishment of PSG and poor availability of it to most clinicians, it is not recommended for routine use in assessment of insomnia. Hence, application of a simple, but reliable instrument would be of great importance in the clinical evaluation of insomnia complaints.[10]
The insomnia severity index (ISI) is a short subjective instrument measuring symptoms and consequences of insomnia. The ISI is composed of seven items assessing recent problems with sleep onset, sleep maintenance and early morning awakening, interference of sleep problems with daily functioning and perceived prominence of impairment attributed to the sleep problem, concern about sleep problems and satisfaction with sleep patterns. Perceived severity of each item is rated on a 0-4 scale and a total score, which ranges from 0 to 28 obtains from summing the items ratings.[11,12] The main object of this study was comparing the data from the ISI to those of a standard overnight PSG.
MATERIALS AND METHODS
In this cross-sectional study a total of 151 patients who attended a sleep disorders clinic in Tehran, Iran and diagnosed as chronic insomniacs were consecutively enrolled. After that the goals of the study were fully explained for the participants, an informed consent document was signed by them.
In the initial assessment, self-administered questionnaires were completed by the participants to provide information on demographic characteristics and ISI. No specific exclusion criteria were used except incomplete filling the questionnaire. After fill in the questionnaire, all participants spent one night in the sleep laboratory for PSG assessment.
Interpretation of ISI scores was performed according to a commonly using guideline, which classifies scores of 0-7 as no clinically significant insomnia, 8-14 as sub-threshold insomnia, 15-21 as clinical insomnia of moderate severity, 21-28 as severe clinical insomnia.[13] All the scoring and interpretations of polysomnographic results were done by a certified sleep specialist. All analyses were performed using Statistical Package for the Social Sciences Version 15 for Windows. Differences between categorical variables were analyzed with Chi-square test and differences between mean values of continuous variables were tested using t-test. Correlations between ISI scores and PSG results were tested using the two tailed Spearman correlation coefficients. A significance level of 0.05 was used for each hypothesis.
RESULTS
The mean (standard deviation) and range of participants’ ages in years were 47.2 (10.8) and 15-83, respectively. Among the total of 151 participants, 21.2% (n = 32) were male and 78.8% (n = 119) were female. There was not any significant difference between mean ages of male versus female participants (47.25 ± 12.6 and 47.27 ± 10.3, respectively, P = 0.99). The ISI internal consistency was high with a cronbach's alpha of 0.85.
According to the ISI score interpretation guideline, provided in the method section, among the 151 participants, 26.5% (n = 40) indicated no clinically significant insomnia, 31.8% (n = 48) a sub-threshold insomnia, 35.1% (n = 53) a clinical insomnia of moderate severity and 6.6% (n = 10) a severe clinical insomnia. The average ISS score was 6.1 ± 4 in our patients.
According to a cut-off score of 14 in ISI to distinguish subjects with clinical insomnia of at least moderate severity from the others, the participants were divided into two groups. Anthropometric and clinical characteristics as well as polysomnographic results of the 151 patients and comparison of these characteristics between participants with and without insomnia are illustrated in Table 1.
Table 1.
Anthropometric and clinical characteristics of the total study population, as well as comparison of this characteristics between subjects with and without insomnia
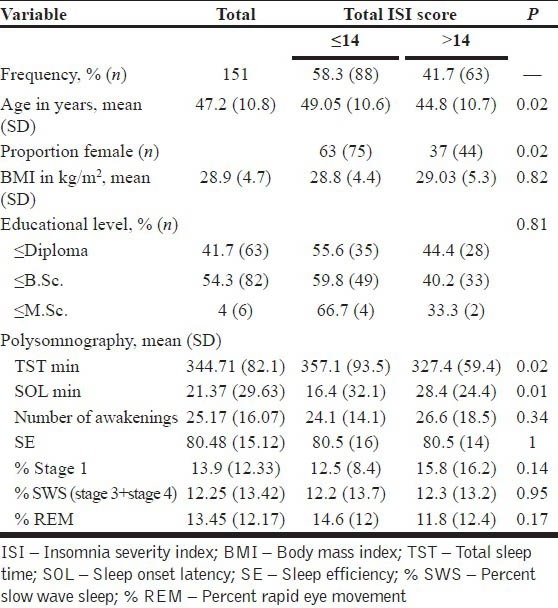
There was a significant difference in the mean age between groups and subjects with ISI ≤14 (n = 88) were significantly older than those with ISI >14 (n = 63) [Table 1] (P = 0.02). The proportion of female subjects was significantly higher in the lower ISI score group than the other one (P = 0.02), but there were no statistically significant difference in body mass index, nor in the educational levels between them [Table 1] (P = 0.82 and 0.81, respectively).
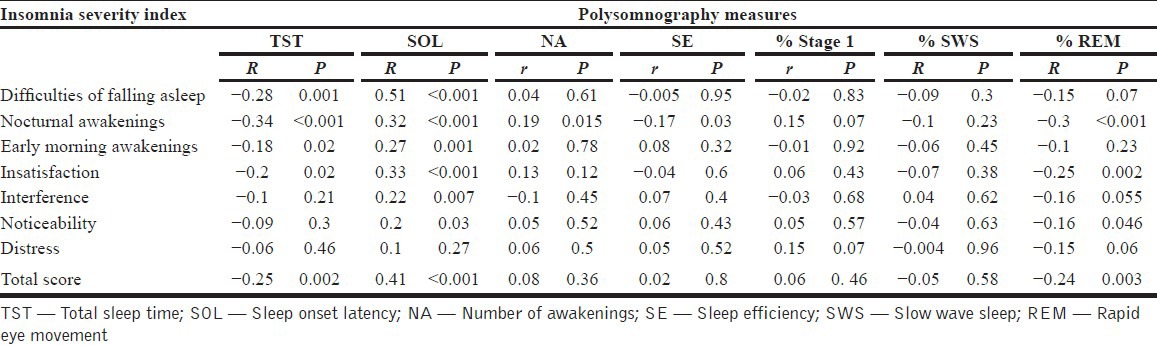
The assessment of correlation between ISI and the polysomnographic evaluation shows the following results: There was a significant correlation between the subjective complaint of difficulty in sleep initiation and sleep onset latency (SOL) in PSG (r = 0.5, P < 0.001). Furthermore, there was a significant correlation between the subjective complaint of difficulty in sleep maintenance and the number of awakening (NA) in PSG (r = 0.19, P = 0.01). A low patients’ satisfaction from sleep was associated with lower total sleep time (TST) (r = −0.2, P = 0.02) and a lower percentage of rapid eye movement (REM) sleep in the polysomnographic evaluation (r = −0.25, P = 0.002). No significant correlation was found between the patients’ satisfaction from sleep and sleep efficiency (SE) in PSG (r = −0.04, P = 0.6) [Table 2].
Table 2.
Correlation between Insomnia severity index and polysomnographic results
DISCUSSION
According to simplicity and short time for application, ISI could be a useful tool to measure the type and severity of insomnia. The ISI is designed to be both a brief screening measure of insomnia severity and an outcome measure, which have significant interaction with each other.[14,15] Since PSG is a gold standard for quantitative and qualitative assessment of insomnia, comparing the results of ISI with PSG could be of great importance in reliability assessment of ISI among Iranian patients suffering from insomnia and was the main goal of this study.
The results of our study indicate that in ISI, questions, which measure difficulties in sleep initiation and maintenance (Questions 1-3), have significant correlations with SOL and TST in PSG, also report of nocturnal awakenings in ISI (Question 2) has significant positive correlation with total NA and negative correlations with SE and percent of REM in PSG [Table 2]. These finding are similar to those of some previous published studies.[11,16]
The report of insatisfaction in ISI had a significant negative correlation with TST and positive correlation with SOL in PSG.
The total score of ISI had significant negative correlations with TST and percent of REM sleep and had significant positive correlation with SOL in PSG. A recent study also surveyed the ISI results in patients with insomnia and was compared with those of polysomnographic findings pre- and post-treatment for insomnia. Their findings shows that the correlation for SOL variable was significant at insomniac patients before treatment, whereas all correlations without one Early Morning Awakening (EMA) were significant at post treatment. Furthermore, there was a stronger relationship between the ISI and polysomnographic variables at patients’ assessment after treatment than before treatment.[11]
In our study, the most association was observed between difficulty in sleep initiation and SOL in PSG. This result is different from another study conducted by Bastien et al. They found the strongest association between NA during the night and Number Of Awakening in PSG. This discrepancy may be due to the difference in the mean age of patients in two studies. Mean age of our patients was 47 years, while the mean age of Bastien's et al. patients was 65 years. Sleep maintenance problems are much more prominent in the older population.[11]
In our study, highest correlation was found between ISI variables and PSG items that indicated in quantity of sleep and did not exists a relationship between any questions from ISI questionnaire indicated that interference with daily functioning and patients concern with PSG variables.
These findings may indicate two issues; the first one, the changes in sleep quantities is better perceived in patients with insomnia and the second is questions from ISI indicated a problem in sleep quantity is more represent of patients discomfort than questions indicated interference of insomnia with daily functioning.
These findings support the reliability of ISI in the clinical assessment of insomnia in research and treatment purposes. It is useful to quantify the severity of insomnia and its interference with patients’ performance and concerned experienced by the patients. Since our patients selected from a sleep clinic population, it would be useful to replicate this study with patients in primary care setting and ISI rating and sleep tests was done after treatment of patients.
Finally, it has been suggested that three questions from ISI about wake-related consider for additional survey to enhance its diagnostic specificity.
CONCLUSIONS
The findings of this study suggest that subjective insomnia measured with ISI is correlated with PSG variables. The ISI could be a valuable questionnaire for use at sleep clinic as a severity measure of insomnia. Further research is needed to assess the observed associations in this study.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Dinges DF, Douglas SD, Hamarman S, Zaugg L, Kapoor S. Sleep deprivation and human immune function. Adv Neuroimmunol. 1995;5:97–110. doi: 10.1016/0960-5428(95)00002-j. [DOI] [PubMed] [Google Scholar]
- 2.National Institutes of Health. National Institutes of Health state of the science conference statement on manifestations and management of chronic insomnia in adults, June 13-15, 2005. Sleep. 2005;28:1049–57. doi: 10.1093/sleep/28.9.1049. [DOI] [PubMed] [Google Scholar]
- 3.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–84. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 4.Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment. Prevalence and correlates. Arch Gen Psychiatry. 1985;42:225–32. doi: 10.1001/archpsyc.1985.01790260019002. [DOI] [PubMed] [Google Scholar]
- 5.Estivill E, Bové A, García-Borreguero D, Gibert J, Paniagua J, Pin G, et al. Consensus on drug treatment, definition and diagnosis for insomnia. Clin Drug Investig. 2003;23:351–85. doi: 10.2165/00044011-200323060-00001. [DOI] [PubMed] [Google Scholar]
- 6.Benca RM. Insomnia. In: DeStefano FR, Scheidt S, editors. Handbook of Sleep Medicine. 1st ed. Philadelphia: Lippincott Williams & Wilkins; 2006. pp. 112–9. [Google Scholar]
- 7.Reis MS, Sampaio LM, Lacerda D, De Oliveira LV, Pereira GB, Pantoni CB, et al. Acute effects of different levels of continuous positive airway pressure on cardiac autonomic modulation in chronic heart failure and chronic obstructive pulmonary disease. Arch Med Sci. 2010;6:719–27. doi: 10.5114/aoms.2010.17087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bahammam AS, Sharif M, Gacuan DE, George S. Evaluation of the accuracy of manual and automatic scoring of a single airflow channel in patients with a high probability of obstructive sleep apnea. Med Sci Monit. 2011;17:MT13–9. doi: 10.12659/MSM.881379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patra S, Telles S. Positive impact of cyclic meditation on subsequent sleep. Med Sci Monit. 2009;15:CR375–81. [PubMed] [Google Scholar]
- 10.Yue W, Hao W, Liu P, Liu T, Ni M, Guo Q. A case-control study on psychological symptoms in sleep apnea-hypopnea syndrome. Can J Psychiatry. 2003;48:318–23. doi: 10.1177/070674370304800507. [DOI] [PubMed] [Google Scholar]
- 11.Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 12.Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–8. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith MT, Wegener ST. Measures of sleep. Arthritis Care Res. 2003;49:S184–96. [Google Scholar]
- 14.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 15.Doi Y, Minowa M, Uchiyama M, Okawa M, Kim K, Shibui K, et al. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh sleep quality index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res. 2000;97:165–72. doi: 10.1016/s0165-1781(00)00232-8. [DOI] [PubMed] [Google Scholar]
- 16.Savard MH, Savard J, Simard S, Ivers H. Empirical validation of the insomnia severity index in cancer patients. Psychooncology. 2005;14:429–41. doi: 10.1002/pon.860. [DOI] [PubMed] [Google Scholar]


