Abstract
Objective:
Factitious disorder is amongst the more intriguing but less-studied psychological disorders. Studies from different parts of the world have reported of varying prevalence rates. Here, we try to study the prevalence of factitious disorder in a specific sample of patients attending a neuropsychiatric center in India.
Materials and Methods:
We did a retrospective review of our institute's database for cases with a diagnosis of factitious disorder in the 10-year duration from 2001 to 2010. We reviewed the available clinical and socio-demographic data.
Results:
Of the 81,176 patients seen in the 10-year duration, only 8 patients had been assigned the diagnosis of factitious disorder, leading to a prevalence rate of 0.985 per 10,000 patients in this sample. Most of the patients were lost to follow-up; hence.
Conclusion:
Factitious disorder remains highly underdiagnosed in developing countries like India. Mental health professionals need to be more aware and inquisitive about this particular disorder, so that they do not miss the diagnosis.
Keywords: Factitious disorder, India, psychological symptoms
INTRODUCTION
Factitious disorder (FD; pathomimia), which has been described as both disease and deception, presents to the clinician as one of the most challenging conditions in medical experience.[1] Patients who present with the symptoms of this disorder are considered to have a “sick role” seeking as the motivation for feigning the illness. FD is distinguished from malingering by this “sick role” seeking in contrast to external incentives acting as the motivating factor in the latter.
Nosology
Categorized as an Axis I DSM IV condition, it is diagnosed when there is an intentional production or feigning of physical or psychological signs or symptoms where the incentive is to assume the sick role and external incentives for the behavior are absent.[2] In DSM IV, four subtypes of FD are mentioned – FD with predominantly psychological signs and symptoms, FD with primarily physical signs and symptoms, FD with combined physical and psychological signs and symptoms, and FD not otherwise specified. In the expanded International Statistical Classification of Diseases and Related Health Problems, Revision 10 (ICD-10), FD (F68.1) is defined as repeated and consistent feigning of symptoms with obscure motivation for the behavior and is best interpreted as a disorder of illness behavior and the sick role.[3] Another related condition is “FD by proxy,” which was described initially by Meadow as “the deliberate production or feigning of physical or psychological symptoms or signs in another person who is under that individual's care,” and is commonly perpetrated by mothers against infants or young children.[4]
Literature regarding FD is limited to a few case reports or small case series. Interestingly, there has also been a case report on concurrent presence of FD and FD by proxy.[5] Another newer concept or problem in this field is “Munchausen by Internet,” where a person may post false stories of his illness on internet forums to gain attention.[6]
Epidemiology
The diagnosis of FD has controversies regarding the criteria and its empirical content.[7] Patients with FD have an unusually long, rich, and changing historical and clinical profile. So also, FD has high chances of occurrence of medico-legal issues. FD appears to be relatively common in specialty medical settings rather than psychiatric setting – yet, it often goes unrecognized and undiagnosed. Since FD can be difficult to detect, its prevalence may be underestimated.
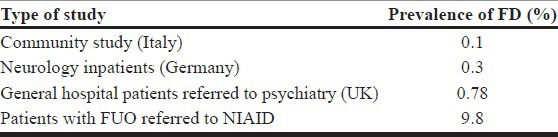
Prevalence of FD varies depending on the type of the patient population studied, study setting, and even clinician's index of suspicion. A community study from Italy reported the prevalence to be 0.1%,[8] whereas it was 9.3% in referrals to the National Institute for Allergy and Infectious Disease with fever of unknown origin (FUO) lasting over 1 year.[9] Prevalence of FD in neurology inpatients was reported to be 0.3% in a German study.[10] Prevalence in psychiatry inpatients also varies from 0.5 to 8%.[11,12] Among psychiatry referrals in a general hospital, one study found 10 patients to be diagnosed with FD among 1288 referrals, making the prevalence 0.78% [Table 1].[13] There are very few reports of FD from developing countries, such as the study regarding FUO in Argentina that reported four cases of FD amongst 113 cases of FUO[14] and the case reports from other countries.
Table 1.
Prevalence of factitious disorder
After a thorough search in Medline, PubMed, Embase, Medknow databases, we came across a few case reports from India of varied presentations like factitious schizophrenia,[15] multiple physical and sexual complaints,[16] and oliguria,[17] whereas detailed case series and long-term studies are yet to be reported.
The age of onset for FD is generally before 30 years.[13] FD is generally seen more commonly among females, especially those who are associated with healthcare field. A retrospective study of 93 patients of FD at the Mayo Clinic showed that 42% patients were female health workers.[18]
Comorbid existence of FD with other psychiatric disorders
Although it is clear that people with FD have a higher rate of comorbid psychiatric disorders, feigning of symptoms itself should be an evidence for psychological distress: “While an act of malingering may be considered adaptive, by definition, a diagnosis of a Factitious Disorder always implies psychopathology…” (APA, 1980: 285). Diagnosis of comorbid problems in people with FD is a contentious issue. DSM Axis I disorders – depression and anxiety disorders have been reported, but the data are scanty.
Practical difficulties in the diagnosis of psychiatric disorders in people with FD include factors such as Varied presentations in different medical specialities, lesser index of suspicion in specialists, presentation in emergency settings where one cannot afford to wait for being investigated extensively to avoid untoward happenings, and lack of thorough knowledge about the symptoms and disease in one who is presenting.
Aim
This study from a neuropsychiatric center aims at reviewing the database for the clinical details of patients with diagnosis of FD from the year 2001 to 2010. It aims to provide information which would be useful in increasing the awareness and understanding about FD at a neuropsychiatric center in a developing country.
MATERIALS AND METHODS
This study describes the nature of psychiatric diagnoses and treatment in patients who were identified to have FD at a neuropsychiatric center in southern India during the 10-year period between 2001 and 2010. The National Institute of Mental Health and Neurosciences (NIMHANS), Bangalore, India is a multidisciplinary institute for patient care and academic pursuit in mental health and neurosciences. The institute is a referral center for patients from all over India. It has a daily psychiatry outpatient turnover of more than 400 patients.
At NIMHANS, an initial screening of the patients is followed by a more detailed evaluation. Postgraduate trainees from the disciplines of psychiatry, psychiatric social work, and psychology do the detailed evaluation and discuss with a consultant psychiatrist. A diagnosis is made if the condition of the patient fulfills the criteria as per ICD-10.[3] The details are entered into computerized database after appropriate coding of each case record. Using this computer database, we identified all individuals with FD between the years 2001 and 2010. Detailed data on clinical characteristics was available for five patients. The hospital records were reviewed by two psychiatrists. The study was a retrospective chart-based review and there were no individual patient identifiers involved in the analysis and reporting. Consent was provided at the time of registration for services by each individual.
RESULTS
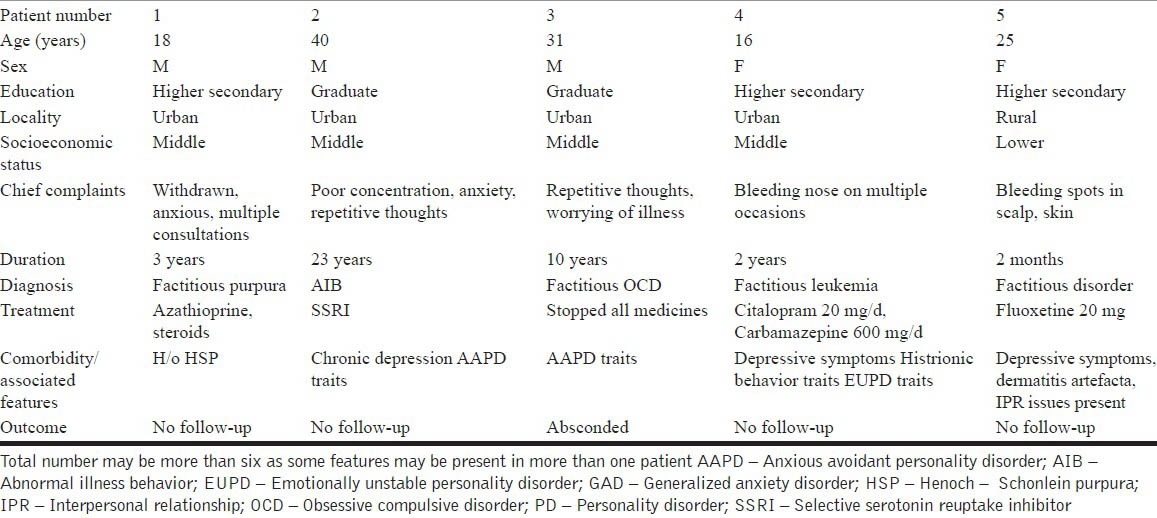
During the above-mentioned period, 81,176 (52,364 men and 28,812 women) patients were assessed. FD was diagnosed in only eight patients. Prevalence of diagnosed FD is, therefore, 0.985 per 10,000 patients in this sample. Detailed data on clinical characteristics was available for five patients. Age of the patients diagnosed with FD ranged from 16 to 40 years. Of all these patients, one had history of chronic depression and two had history suggestive of sub-syndromal depressive symptoms. Personality problems were diagnosed in three patients, of whom two had anxious avoidant personality traits and another patient had histrionic personality disorder. Psychosocial issues like interpersonal problems with in-laws, over-involved parents, and self-medication were present in three patients. Also, one patient had history of dermatitis artefacta and another had history of Henoch – Schonlein purpura. No patient came for even a single follow-up. The socio-demographic and clinical details of the cases are presented in Table 2.
Table 2.
Demographic and clinical details of cases
DISCUSSION
Diagnosis of FD seems to be infrequent in the general psychiatric setup in India. Only eight individuals had a diagnosis after screening over 80,000 cases seen in the center over a 10-year period. Prevalence of diagnosed FD is, therefore, 0.985 per 10,000 patients in this sample, which is on lower side when compared to 0.5-8% reported in other studies. Judging by the projected prevalence of FD in the population and the higher prevalence of mental health problems, perhaps this is likely to be the tip of the iceberg. Hence, only those with psychological symptoms would have undergone evaluation here. It is possible that people who attracted the diagnoses of FD are the individuals in whom the presentation was typical and severe. Four of the patients presented with anxiety symptoms, suggesting the need to observe for anxiety symptoms in suspected cases of FD. Three individuals in this sample also had personality disorder or traits. Perhaps, persons with physical symptoms as FD present to medical or surgical settings, whereas those with psychological, emotional, and behavioral factitious symptoms seek psychiatric hospitals.
Thus, it is important for the psychiatrists to take a detailed history of previous admissions and treatment, along with investigation reports while assessing individuals with FD. The second issue is authenticity of the reports as the patients can change the name and claim the report to be theirs. Hence, one has to be careful before making any diagnosis. In this patient subtype, there is, however, a high use of psychotropic medications and this reflects a symptom-focused approach.
Individuals in this sample received counselling with a psycho-educational focus that included information on the nature of FD and its relation to the problems that they had presented with. Most of the patients did not turn up for follow-up after discharge, whereas one patient absconded when doctors tried to confront the patient with the diagnosis and management plan. However, as no clear structured methods are available to diagnose the FD and no clear guidelines are available to confront, precautionary methods need to be taken to avoid untoward outcomes like absconding and denial for follow-up. Perhaps, the improvement in the awareness of the nature of the problem among the patients as well as the relatives may lead to better coping strategies and minimize the reliance on the medications.
There is a need for improving the awareness of FD among mental health professionals as well as general practitioners, as the disorder can be very challenging to the health care professionals. While the assessment and management of FD is integrated in the practice of professionals who specialize in mental health, this is not the case for general practitioners. There is a need to build a multidisciplinary approach in the management of the disorder, as well as for improving the ongoing support with self-support groups, supported employment and carer support.
This study has the limitations of being based on a retrospective approach. However, patients were assessed by a psychiatric trainee and a consultant psychiatrist before the diagnosis was made. Information gathered using a semi-structured interview was recorded in the case notes and diagnoses were made according to the ICD-10 criteria. These measures ameliorated some of the disadvantages of the retrospective design.
CONCLUSION
It can be estimated using prevalence figures available from other countries that India has about 1.3 million people with FD. However, majority of people with this condition unfortunately remain undiagnosed and may be subjected to extensive medical investigations. Although there are some case reports on FD, there is still a paucity of research. This is a retrospective study based on screening of all adults seen in the outpatient clinic of a tertiary institution over a 10-year period. Only eight individuals have been diagnosed as having FD in this time-frame, and a review of their clinical features and management indicates the use of psychotropic medications based approach for comorbidity and symptomatic treatment. The findings from this study point to the need for further research in this area. A prospective design with structured assessment would yield further valuable information.
ACKNOWLEDGMENTS
The authors would like to thank all the units of the Department of Psychiatry, NIMHANS and the Medical Records Department, NIMHANS for providing case records.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Feldman MD, Eisendrath SJ. Washington (DC): American Psychiatric Press; 1996. The spectrum of factitious disorders. [Google Scholar]
- 2.Washington: American Psychiatric Association; 1994. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 3.Geneva: World Health Organization; 1992. World Health Organization: The ICD-10 Classification of Mental and Behavioral Disorders: Clinical descriptions and diagnostic guidelines. [Google Scholar]
- 4.Meadow R. Munchausen syndrome by proxy. The hinterland of child abuse. Lancet. 1977;2:343–5. doi: 10.1016/s0140-6736(77)91497-0. [DOI] [PubMed] [Google Scholar]
- 5.Feldman MD, Rosenquist PB, Bond JP. Concurrent factitious disorder and factitious disorder by proxy. Double jeopardy. Gen Hosp Psychiatry. 1997;19:24–8. doi: 10.1016/s0163-8343(96)00108-9. [DOI] [PubMed] [Google Scholar]
- 6.Feldman MD. Munchausen by Internet: Detecting factitious illness and crisis on the Internet. South Med J. 2000;93:669–72. [PubMed] [Google Scholar]
- 7.Turner MA. Factitious disorders: Reformulating the DSM-IV criteria. Psychosomatics. 2006;47:23–32. doi: 10.1176/appi.psy.47.1.23. [DOI] [PubMed] [Google Scholar]
- 8.Faravelli C, Abrardi L, Bartolozzi D, Cecchi C, Cosci F, D’Adamo D, et al. The Sesto Fiorentino study: Point and one-year prevalences of psychiatric disorders in an Italian community sample using clinical interviewers. Psychother Psychosom. 2004;73:226–34. doi: 10.1159/000077741. [DOI] [PubMed] [Google Scholar]
- 9.Aduan RP, Fauci AS, Dale DC, Herzberg JH, Wolff SM. Factitious fever and self-induced infection: A report of 32 cases and review of the literature. Ann Intern Med. 1979;90:230–42. doi: 10.7326/0003-4819-90-2-230. [DOI] [PubMed] [Google Scholar]
- 10.Bauer M, Boegner F. Neurological syndromes in factitious disorder. J Nerv Ment Dis. 1996;184:281–8. doi: 10.1097/00005053-199605000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Catalina ML, Gomez Macias V, De Cos A. Prevalence of factitious disorder with psychological symptoms in hospitalized patients. Actas Esp Psiquiatr. 2008;36:345–9. [PubMed] [Google Scholar]
- 12.Bhugra D. Psychiatric Munchausen's syndrome. Literature review with case reports. Acta Psychiatr Scand. 1988;77:497–503. doi: 10.1111/j.1600-0447.1988.tb05160.x. [DOI] [PubMed] [Google Scholar]
- 13.Sutherland AJ, Rodin GM. Factitious disorders in a general hospital setting: Clinical features and a review of the literature. Psychosomatics. 1990;31:392–9. doi: 10.1016/S0033-3182(90)72133-0. [DOI] [PubMed] [Google Scholar]
- 14.Chantada G, Casak S, Plata JD, Pociecha J, Bologna R. Children with fever of unknown origin in Argentina: An analysis of 113 cases. Pediatr Infect Dis J. 1994;13:260–3. doi: 10.1097/00006454-199404000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Grover S, Kumar S, Mattoo SK, Painuly NP, Bhateja G, Kaur R. Factitious schizophrenia. Indian J Psychiatry. 2005;47:169–72. doi: 10.4103/0019-5545.55944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharma I, Ancharaz V, Azmi SA, Chugh S, Ram D. Factitious disorder-a case report. Indian J Psychiatry. 1990;32:285–6. [PMC free article] [PubMed] [Google Scholar]
- 17.Mishra PB, Shyangwa P, Khandelwal SK, Kalra OP. Factitious disorder with oligoanuria: A case report. Indian J Psychiatry. 1999;41:374–6. [PMC free article] [PubMed] [Google Scholar]
- 18.Krahn LE, Li H, O’Connor MK. Patients who strive to be ill: Factitious disorder with physical symptoms. Am J Psychiatry. 2003;160:1163–8. doi: 10.1176/appi.ajp.160.6.1163. [DOI] [PubMed] [Google Scholar]


