Abstract
This review evaluates the outcomes of intrastromal corneal ring segment (ICRS) implantation for the treatment of keratoconus considering a new grading system based on the preoperative visual impairment of the patient. Additionally, a five-year follow-up analysis of patients with stable and progressive keratoconus is performed in order to assess the long term stability of the surgical procedure. Corrected distance visual acuity decreased statistically significantly in patients with mild keratoconus (P < 0.01) but statistically significantly increased in all other grades (P < 0.05). The improvement in visual acuity and the decrease of keratometric and aberrometric values were stable throughout a long period of time in patients with stable keratoconus. In patients with progressive form keratoconus, a significant improvement was found immediately after the procedure, however clinically relevant regression greater than 3 D was observed at the end of the follow up period.
Keywords: Intracorneal Ring Segments, Keratoconus, Keratoconus Treatment
INTRODUCTION
Keratoconus is an ectasic corneal disorder characterized by a progressive corneal thinning that causes irregular astigmatism and decreased visual acuity. The prevalence varies depending on location and race, affecting 57 in 100 000 Caucasian patients and 229 in 100 000 Asian patients.1 The onset is during puberty and progresses until the third decade of the life when it usually becomes stable.2 There are variety of options for management of this pathological condition including, spectacles,2 rigid gas permeable, soft or hybrid contact lenses,3 intracorneal ring segments (ICRS),4,5,6,8 collagen crosslinking (CXL)9 and lamellar or penetrating keratoplasty.10
The progression of this pathological condition is not completely understood and has not been described consistently in the literature. Over the last decade some studies reported several factors are associated with the progression of keratoconus taking account clinical signs such as visual acuity,11,12,13 refractive status,14,15 topographic12,13,14,15,16,17 and aberrometric14,15,18,19,20,21 data and objective signs assessed by Fourier series harmonic analysis.22 It is a multifactorial process, but clinically factors such as a loss in uncorrected and best corrected visual acuity, an increase in manifest refraction (sphere and cylinder)11,13,14,15,23 and an increase in internal astigmatism (IA)14,21 has been described.
Several classifications of the disease have been made taking into account different parameters, such as keratometry, topography, and aberrometry to define the grade of severity of keratoconus. However, to date, there is no grading system that integrates morphological parameters mentioned above and other factors closely related with visual function such as visual acuity.
The aim of ICRS surgery is to induce a geometric change in the central corneal curvature, thus, reducing the refractive error and the mean keratometry and improving the visual acuity. Additionally, corneal remodelling results in an improvement in the optical quality of the cornea and a reduction in optical aberrations can also be expected.4,5,6,8,24,25,26 Some long term studies27,28,29 have reported that this surgical technique may be a potential therapeutic option to halt the progression of keratoconus, but an independent analysis between stable and progressive cases has not been performed in previous studies. Furthermore, there is not enough clinical evidence published that supports this hypothesis.
The study evaluates the outcome of patients who underwent ICRS implantation by incorporating a new grading system based on modern diagnostic parameters and the limitation of the visual function of the patient. Additionally, the stability of the outcomes was assessed after long term postoperative follow up. We summarize our experience of 5 years of studies in keratoconus from diagnostic and surgical perspectives.
PATIENTS AND METHODS
Patients: The RETICS database
The current study is comprised of a review of three scientific investigations performed by our research group. The first investigation described the outcomes of ICRS implantation considering the results from a different perspective and a grading system that takes into account the visual limitations of the patients. The purpose of the other two investitagations was to analyze the results after long term follow up period in keratoconic eyes that underwent ICRS implantation. Currently, we maintain an ongoing multicentre database comprised of almost 1000 cases of keratoconus patients who have undergone ICRS implantation.
For all procedures performed in the different studies that comprise this review, every patient underwent a thorough discussion of the surgical procedure, its risk and its benefits, and patients signed an informed consent in accordance with the Helsinki Declaration where they agreed that their clinical data may be included in scientific studies. Ethical board committee approval from the institution was obtained for all three studies.
Grading system according to the level of visual limitation
In order to analyse the outcomes of ICRS implantation based on preoperative visual impairment, a multicenter, longitudinal retrospective and non-randomized analysis was performed of 661 eyes of 357 patients who underwent ICRS implantation. All patients were included after a retrospective review of all cases with the diagnosis of keratoconus in six different ophthalmologic centers that belong to the Spanish Network of Research in Ophthalmology (RETICS).
Patients were divided into five different groups according to the grading system based on the limitations of preoperative visual acuity.30 Grade I includes patients with spectacle-corrected distance visual acuity (CDVA) in decimal notation of 0.90 or better; grade II include patients with CDVA equal to or better than 0.60 and worse than 0.90; grade III includes patients with CDVA equal to or better than 0.40 and worse than 0.20; grade IV, patients with CDVA equal to or better than 0.20 and worse than 0.40; and grade plus, patients with CDVA worse than 0.20.
Criteria to define success or failure of surgery
With the aim of analyzing the efficacy of the surgical procedure the following criteria were defined. Successful surgery was defined as one of the following characteristics at 6 months postoperatively: 1) an improvement in one or more lines of uncorrected distance visual acuity (UDVA) or CDVA; 2) a decrease in two or more D of spherical equivalent; 3) a decrease of at least 1 μm of the root mean square (RMS) corneal high-order aberrations or coma-like aberrations.
Failure was defined as one of the following characteristics at 6 months postoperatively: 1) a loss in one or more lines of UDVA or CDVA; 2) an increase in two or more D of spherical equivalent; 3) an increase in 1 μm or more in the RMS corneal high-order or coma-like aberrations.
Stability analysis after long term follow-up
To assess the stability of the outcomes after ICRS implantation over the long term, we selected cases from the database with at least 5 years follow up. “Stable cases” were defined as cases without significant changes in corneal topography (<1 D in the mean keratometry [mean K]) over 12 months preoperatively. To evaluate the capability of the surgical procedure to halt keratoconus progression over the long term we analyzed patients that met any of the following conditions at 6 months preoperatively (“Progressive cases”): 1) Increase in the mean K or in the steepest keratometry (K2) of 3 mm central cornea ≥ 0.75 D; 2) increase in cylinder ≥ 1.0 D; 3) increase in sphere ≥ 1.0 D; 4) decrease of 2 lines in CDVA. In the cases with progression of keratoconus all patients ranged in age from 19 years to 30 years (mean age: 25.75 ± 3.59 years).
Once the criteria of patient selection were established, a longitudinal retrospective and non-randomized analysis was performed. The stable cases comprised 51 keratoconic eyes of 35 patients, and the progressive cases comprised a total of 18 keratoconic eyes of 15 patients. In both, stable and progressive cases the follow up period was 5 years.
Examination protocol
A comprehensive examination was performed in all cases. The tests included were the same for each study that included measurement of uncorrected visual acuity, corrected visual acuity, manifest refraction (sphere and refraction), Goldman tonometry, ultrasonic pachymetry, fundus evaluation, slit-lamp biomicroscopy, and corneal topographic analysis including anterior corneal higher order aberrations measured with a pupil size of 6 mm. As the studies were retrospective and were performed over different time periods and at different centers, there were slight differences in the instrumentation used to obtain data. All the instrumentations in the studies have been validated in order to assert their clinical precision.
Surgical technique
Surgical procedures were performed by different surgeons, depending on each participating center in the study. In all cases antibiotic prophylaxis consisting of topical ciprofloxacin was prescribed every 8 h for 2 days before surgery. All procedures were performed under topical anesthesia.
Surgical procedures were performed using either femtosecond laser technology or mechanical corneal dissection. The mechanical surgical procedure was initiated marking a reference point for centration (pupil centre) and performing a radial incision of approximately 1.8 mm in length. Subsequently, a calibrated diamond knife was set at approximately 70% of the mean corneal thickness determined by ultrasonic pachymetry. From the base of the incision, pocketing hooks were used to create corneal pockets on each side of the incision, ensuring a uniform depth. A device containing a semi-automated suction ring was placed around the limbus, guided by the previously marked reference point on the cornea. Two semicircular dissectors were then placed sequentially into the lamellar pocket to be steadily advanced by a rotational movement (counter-clockwise and clockwise dissectors).
For femtosecond laser-assisted surgery, the suction ring was applied, and then the disposable glass lens of the laser system was applied first to applanate the cornea, fixate the eye and help maintain a precise distance from the laser head to the focal point. Then, a continuous circular stromal tunnel was created at approximately 80% of corneal depth. The 60 kHz IntraLase femtosecond system (IntraLase Corp., Irvine, California, USA) was used for all procedures.
Only keratoconus cases that underwent ICRS implantation (Keraring, Mediphacos Ltd. and Intacs, Addition Technology Inc) were included in this investigation. The selection of the number (1 or 2), arc-length and thickness of ICRS was performed following the nomogram defined by the manufacturer.
Postoperatively, topical tobramycin and dexamethasone eye drops (TobraDex; Alcon Laboratories, Inc., Fort Worth, Texas, USA) were used every 6 h for 1 week and then stopped. Topical lubricants were also prescribed every 6 h for 1 month (Systane, Alcon Laboratories, Inc., Fort Worth, Texas, USA).
Statistical analysis
The statistical analysis was performed using the SPSS software for Windows (version 15.0; SPSS Inc, Chicago, Illinois, USA). Normal distribution of all data samples were evaluated by means of the Kolmogorov-Smirnov test. When parametric analysis was not possible, the Wilcoxon rank sum test was applied to assess the significance of differences between preoperative and postoperative data. P < 0.05 was considered statistically significant.
For comparisons among groups, the one-way analysis of variance with the Bonferroni post hoc comparison procedure was used when parametric analysis was possible. Variances were checked by the Levene test and when they were not homogeneous, the Tamhane post hoc analysis was used. When parametric analysis was not possible, the Kruskal − Wallis test was used with the same level of statistical significance (P < 0.05). In order to avoid the experimental error rate, the Mann − Whitney test with Bonferroni correction was used for post hoc analysis.
RESULTS
Outcome analysis of ICRS implantation based on the degree of visual limitation
The overall results showed a postoperative clinical improvement of visual outcomes and a reduction in spherical equivalent, keratometry and higher order corneal aberrations.
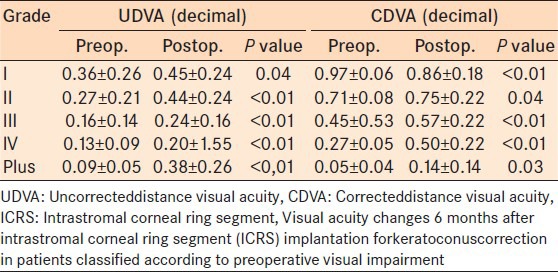
There was a statistically significant increase in the UDVA for all grades of keratoconus compared to preoperative values (P < 0.05, all comparisons). CDVA increased statistically significantly in all grades from preoperative values with the exception of grade I, in which a statistically significantly decreased from preoperative to postoperative values was observed [Table 1].
Table 1.
Visual outcomes 6 months after ICRS implantation
All high-order aberrations (HOA) under study showed a postoperative reduction, however only the RMS coma-like aberrations for grade III keratoconus cases were within the limit of statistical significance (P = 0.05).
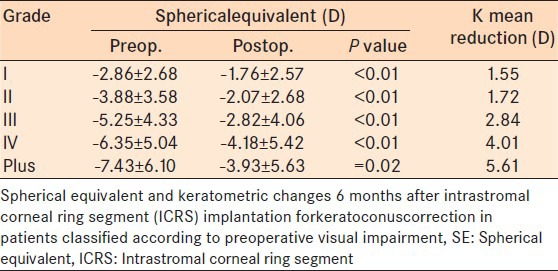
Both spherical equivalent (SE) and keratometry had a statistically significant improvement after ICRS implantation (P < 0.05) [Table 2].
Table 2.
SE and keratometry changes after ICRS implantation
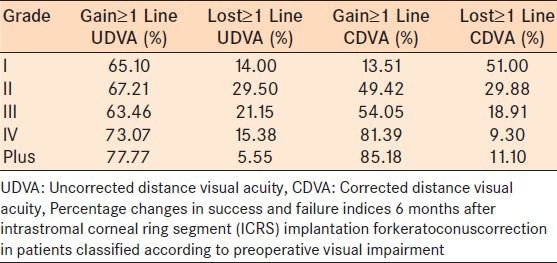
Analysis of results in relation to the success and failure indices showed that eyes with mild keratoconus (grades I and II) experienced the worst outcomes. For example, 37.9% of patients with CDVA 0.6 or better (grades I and II) gained 1 or more lines of CDVA, whereas 82.8% of patients with CDVA 0.4 or worse (grade IV and plus) gained one or more lines of CDVA. Additionally, 36.3% of patients under grade I and II lost 1 or more lines of CDVA, whereas just 10% of patients under grades IV and plus lost 1 or more lines of CDVA. Table 3 shows the distribution of cases according to the success and failure indices.
Table 3.
Success and failure indices
Stability analysis of ICRS implantation: Comparison of “Stable” and “Progressive” cases of keratoconus along 5 years of follow up
The study with stable cases comprised 51 consecutive keratoconic eyes of 35 patients, with a mean age of 29.76 ± 8.84 years (range, 15 years to 56 years), whereas the study with progressive cases comprised 18 consecutive keratoconic eyes of 15 patients ranging in age from 19 years to 30 years (mean age of 25.75 ± 3.59 years).
Visual acuity
No variation in UDVA was recorded in stable cases preoperatively. Preoperative UDVA decreased in progressive cases from the mean value of the first visit (6 months prior to surgery) of 0.24 ± 0.28 to the preoperative value of 0.19 ± 0.15 (P = 0.61).
In stable cases, the mean UDVA value was statistically significantly better postoperatively than preoperatively (P = 0.04). UDVA increased statistically significantly from 0.22 ± 0.19 preoperatively to 0.45 ± 0.26 at 6 months postoperatively (P = 0.04). The improvement in the UDVA remained without statistically significantly changes 5 years after surgery (P = 0.31).
For progressive cases, a significant improvement in UCVA was found 6 months after ICRS implantation (P < 0.05). In contrast to the stable cases a significant reduction of effect was achieved at 6 months was lost during the remaining follow up period in the progressive cases (P < 0.05).
In stable cases CDVA improved statistically significant at 6 months postoperatively compared to preoperatively (P < 0.01). There were no significant changes in postoperative CDVA after 6 months (P = 0.15). In progressive cases, a clinical improvement in CDVA was found 6 months after surgery with no further significant changes. There was a statistically significant reduction at 5 years postoperatively compared to preoperatively (P = 0.04).
Refractive outcomes
Stable cases showed a statistically significant reduction in the SE from preoperatively to 6 months postoperatively of 1.26 D (P =0.04). The SE remained unchanged from 6 months postoperatively onwards in stable cases (P = 0.57). There was a statistically significant reduction of manifest cylinder at 6 months after ICRS implantation (mean reduction of 1.06 D; P < 0.01). There was no significant reduction in manifest cylinder in stable cases after 6 months postoperatively (P =0.38). The change in manifest sphere was not statistically significant at any postoperative visit (P =0.34).
A clinical but not statistical reduction of sphere was observed 6 months after the ICRS implantation in progressive cases (mean improvement of 3.24 D; P =0.10). Manifest cylinder and SE decreased statistically significantly in 1.58 D and 4.11 D respectively (P = 0.05, Wilcoxon test). At 1 year, a slight regression of 1.19 D in the cylinder and 0.77 D in the SE was found in the progressive cases. A regression of 1.40 D in the sphere and 1.29 D in the SE was also found at 3 years. At the end of the follow-up period, no significant changes were found in relation to the sphere, cylinder, and SE (P > 0.05).
Keratometric changes
A statistically significant reduction was observed in all K readings 6 months after surgery in stable cases (K1 3.26 D, P = 0.02; K2 3.01, P ≤ 0.01; mean K 3.24 D, P ≤ 0.01). There was a slight regression of the effect in the mean K value between 6 months and 1 year that was not statistically significant (P = 0.46). An overall regression of 0.97 D occurred between 6 months and the final follow-up examination in the stable cases (P > 0.05)[Figure 1].
Figure 1.
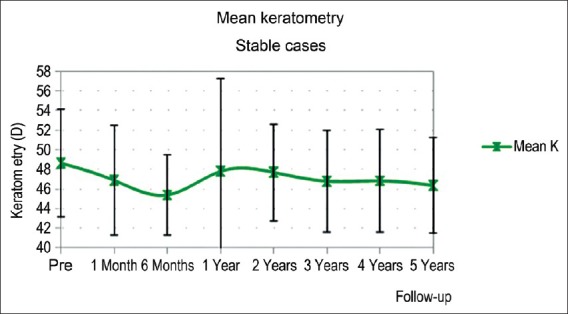
Mean keratometry reading changes five years after intrastromal corneal ring segment (ICRS) implantation in keratoconic patients with the stable form of the disease
In progressive cases there was statistically significant increase in mean keratometry during the preoperative evaluation which confirmed the progressive nature of the cases under analysis. At 6 months postoperatively, there was a statistically significant reduction in mean K (P < 0.05). In the progressive cases, there was a statistically significant reduction immediately after the procedure with regression of 3.36 D between 6 months and 5 years postoperatively (P < 0.05) [Figure 2].
Figure 2.
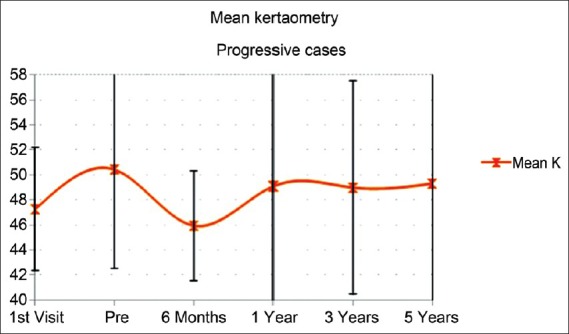
Mean keratometry reading changes five years after intrastromal corneal ring segment (ICRS) implantation in keratoconic patients with the progressive form of the disease
Corneal high-order aberrations
In the stable cases, there was a reduction in all higher order corneal aberrations that were studied at 6 months postoperatively, however none of them reached statistical significance (P > 0.10). There was no statistically significant change in the corneal higher order aberrations during the entire follow up period (P > 0.10).
In progressive cases there was a reduction in all corneal higher order aberrations that were studied, however none of them reached statistical significance over the entire duration of follow-up (P > 0.05). At 6 months postoperatively, there was a decrease in mean total, coma, coma-like and spherical-like aberrations, however slight regression was observed over the remaining follow up period for all aberrations.
DISCUSSION
In this review we evaluated the outcomes of ICRS implantation analysing the results based on preoperative visual impairment and the long term outcomes in patients with stable or progressive disease.
Most of the grading system described in the literature has been developed taking into account the keratometric readings, corneal aberrometry and topographic morphology of the disease, without considering other clinical data that are closely related to the visual disability of keratoconus patients. The grading system described in this review takes into account the functional performance of the patient's visual system,21 such as visual acuity, rather than just the geometric assessment of the cornea, which is unpredictable because of the response of keratoconic eyes.31,32,33 Most of the published studies conclude that there is a significant flattening of the central cornea after the procedure.6,7,25,26,34,35,36,37,38 The results in the current study concur with those previously published as we found a significant reduction in keratometry in all grades of keratoconus. Furthermore, the largest reduction in mean K was observed in cases with the most severe disease. In addition, patients classified under this category were those to show the greatest decrease in SE, which correlates well with the amount of flattening in the central cornea. A study by Ertan and Kamburoglu34 with a large keratoconic population showed that patients with severe keratoconus were the ones in whom the largest reduction of keratometry readings was observed, confirming the findings of the current study. Similar results were reported by Boxer-Wachler and associates33 who reported the greatest reduction in SE occurred in advanced keratoconus cases.
Most previous studies that evaluated the impact of ICRS implantation reported a significant improvement in UDVA.24,25,26,33,34,38,39,40,41 The current study found the most significant improvement in UDVA was achieved by the group of patients classified under the category of grade plus. This outcome is consistent with previous studies that have analyzed clinical outcomes according to disease severity that reported a significant improvement in patients who suffered from severe keratoconus.24,33,41
Several publications in the literature note that ICRS implantation results in an improvement of CDVA.6,24,25,26,33,37,42,43,44,45 However, in the current study, patients with a milder form of keratoconus (patients classified as grade I) showed a statistically significant decrease in CDVA. The differences in outcomes may be due to the fact that previous studies analyzed outcomes of the entire population under study without considering the degree of visual impairment independently. When analyzing what the “success index,” we found that patients presenting with worst preoperative best-corrected visual acuity are the ones who gain more lines of CDVA after ICRS implantation. Regarding the “failure index” it was observed that patients who had the greatest levels of CDVA during the preoperative examination were the ones with greater loss of CDVA postoperatively.
Comparison between stable and progressive outcomes
A reduction of keratometric readings was observed 6 months after ICRS implantation in both stable and progressive cases. There were minimal differences in mean K reduction between stable and progressive cases at 6 months postoperatively. These outcomes are consistent with other studies8,25,26,34,46 that also found that ICRS implantation induces a flattering of the cornea, thus inducing a change in the geometry of the tissue. However, in the current study, a statistically significant regression of 3.36 D occurred in progressive cases from 6 months to 5 years postoperatively. The stable cases had lower regression of 1.00 Dover the same postoperative period.
The reduction in keratometry was accompanied with an increase in UDVA and CDVA at 6 months postoperatively. Beyond this period, the progressive cases showed a statistically significant regression in CDVA (P < 0.05). However, the improvement of CDVA remained unchanged in stable cases. Some studies8,26,27,28 that evaluated the long-term stability of this treatment up to 4 years report similar outcomes.
There were no significant changes in anterior corneal aberrations during follow-up. However, there was a trend toward a reduction, even when it was not statistically significant, of the asymmetric aberrations (RMS-coma and coma-like). These findings are valid for both stable and progressive cases. Others studies38,47 that have analyzed corneal HOAs after ICRS implantation also reported no significant changes postoperatively.
In conclusion, analysis of the outcomes after ICRS implantation based on a grading system that takes into account the visual acuity of the patients shows that this surgical procedure will provide better results in patients with severe keratoconus. Alternately, good preoperative visual acuity should be considered a contraindication because these cases are at the highest risk of losing lines of vision. In addition, assessment of the outcomes after a long period of time demonstrate that ICRS implantation is stable after long period of follow up in those keratoconic cases that does not show progression before the surgical procedure. However, in progressive cases it would be prudent to consider other therapeutic options as regression of the effect should be expected after ICRS implantation.
Footnotes
Source of Support: This study has been supported in part by a grant from the Spanish Ministry of Economy and Competitiveness, Instituto Carlos III, Red Temática de Investigación Cooperativa en Salud “Prevención, detección precozy tratamiento de la patología ocular prevalente, degenerativay crónica”, Subprograma “Dioptrio oculary patologías frecuentes” (RD12/0034/0007.)
Conflict of Interest: None declared.
REFERENCES
- 1.Fernández Meijide N. Keratoconus Epidemiology. In: Albertazzi R, editor. Keratoconus: Guidelines for diagnosis and treatment. Buenos Aires, Argentina: Ediciones Científicas Argentinas; 2010. pp. 11–5. [Google Scholar]
- 2.Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 3.Barnett M, Mannis MJ. Contact lenses in the management of keratoconus. Cornea. 2011;30:1510–6. doi: 10.1097/ICO.0b013e318211401f. [DOI] [PubMed] [Google Scholar]
- 4.Ertan A, Colin J. Intracorneal rings for keratoconus and keratectasia. J Cataract Refract Surg. 2007;33:1303–14. doi: 10.1016/j.jcrs.2007.02.048. [DOI] [PubMed] [Google Scholar]
- 5.Pinero DP, Alio JL. Intracorneal ring segments in ectatic corneal disease - A review. Clin Experiment Ophthalmol. 2010;38:154–167. doi: 10.1111/j.1442-9071.2010.02197.x. [DOI] [PubMed] [Google Scholar]
- 6.Zare MA, Hashemi H, Salari MR. Intracorneal ring segment implantation for the management of keratoconus: Safety and efficacy. J Cataract Refract Surg. 2007;33:1886–91. doi: 10.1016/j.jcrs.2007.06.055. [DOI] [PubMed] [Google Scholar]
- 7.Shetty R, Kurian M, Anand D, Mhaske P, Narayana KM, Shetty BK. Intacs in advanced keratoconus. Cornea. 2008;27:1022–9. doi: 10.1097/ICO.0b013e318172fc54. [DOI] [PubMed] [Google Scholar]
- 8.Alio JL, Shabayek MH, Artola A. Intracorneal ring segments for keratoconus correction: Long-term follow-up. J Cataract Refract Surg. 2006;32:978–85. doi: 10.1016/j.jcrs.2006.02.044. [DOI] [PubMed] [Google Scholar]
- 9.Snibson GR. Collagen cross-linking: A new treatment paradigm in corneal disease - A review. Clin Experiment Ophthalmol. 2010;38:141–53. doi: 10.1111/j.1442-9071.2010.02228.x. [DOI] [PubMed] [Google Scholar]
- 10.Busin M, Scorcia V, Zambianchi L, Ponzin D. Outcomes from a modified microkeratome-assisted lamellar keratoplasty for keratoconus. Arch Ophthalmol. 2012;130:776–82. doi: 10.1001/archophthalmol.2011.1546. [DOI] [PubMed] [Google Scholar]
- 11.Davis LJ, Schechtman KB, Wilson BS, Rosenstiel CE, Riley CH, Libassi DP, et al. Longitudinal changes in visual acuity in keratoconus. Invest Ophthalmol Vis Sci. 2006;47:489–500. doi: 10.1167/iovs.05-0381. [DOI] [PubMed] [Google Scholar]
- 12.Li X, Yang H, Rabinowitz YS. Keratoconus: Classification scheme based on videokeratography and clinical signs. J Cataract Refract Surg. 2009;35:1597–603. doi: 10.1016/j.jcrs.2009.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wagner H, Barr JT, Zadnik K. Collaborative longitudinal evaluation of keratoconus (CLEK) study: Methods and findings to date. Cont Lens Anterior Eye. 2007;30:223–32. doi: 10.1016/j.clae.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pinero DP, Alio JL, Tomas J, Maldonado MJ, Teus MA, Barraquer RI. Vector analysis of evolutive corneal astigmatic changes in keratoconus. Invest Ophthalmol Vis Sci. 2011;52:4054–62. doi: 10.1167/iovs.10-6856. [DOI] [PubMed] [Google Scholar]
- 15.Pinero DP, Alio JL, Barraquer RI, Michael R, Jimenez R. Corneal biomechanics, refraction, and corneal aberrometry in keratoconus: An integrated study. Invest Ophthalmol Vis Sci. 2010;51:1948–55. doi: 10.1167/iovs.09-4177. [DOI] [PubMed] [Google Scholar]
- 16.Sahin A, Yildirim N, Basmak H. Two-year interval changes in orbscan II topography in eyes with keratoconus. J Cataract Refract Surg. 2008;34:1295–9. doi: 10.1016/j.jcrs.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 17.Choi JA, Kim MS. Progression of keratoconus by longitudinal assessment with corneal topography. Invest Ophthalmol Vis Sci. 2012;53:927–35. doi: 10.1167/iovs.11-8118. [DOI] [PubMed] [Google Scholar]
- 18.Mihaltz K, Kovacs I, Kranitz K, Erdei G, Nemeth J, Nagy ZZ. Mechanism of aberration balance and the effect on retinal image quality in keratoconus: Optical and visual characteristics of keratoconus. J Cataract Refract Surg. 2011;37:914–22. doi: 10.1016/j.jcrs.2010.12.040. [DOI] [PubMed] [Google Scholar]
- 19.Jinabhai A, Radhakrishnan H, O’Donnell C. Repeatability of ocular aberration measurements in patients with keratoconus. Ophthalmic Physiol Opt. 2011;31:588–94. doi: 10.1111/j.1475-1313.2011.00868.x. [DOI] [PubMed] [Google Scholar]
- 20.Alio JL, Shabayek MH. Corneal higher order aberrations: A method to grade keratoconus. J Refract Surg. 2006;22:539–45. doi: 10.3928/1081-597X-20060601-05. [DOI] [PubMed] [Google Scholar]
- 21.Alió JL, Piñero DP, Alesón A, Teus MA, Barraquer RI, Murta J, et al. Keratoconus-integrated characterization considering anterior corneal aberrations, internal astigmatism, and corneal biomechanics. J Cataract Refract Surg. 2011;37:552–68. doi: 10.1016/j.jcrs.2010.10.046. [DOI] [PubMed] [Google Scholar]
- 22.Oshika T, Tanabe T, Tomidokoro A, Amano S. Progression of keratoconus assessed by fourier analysis of videokeratography data. Ophthalmology. 2002;109:339–42. doi: 10.1016/s0161-6420(01)00903-4. [DOI] [PubMed] [Google Scholar]
- 23.Tuft SJ, Moodaley LC, Gregory WM, Davison CR, Buckley RJ. Prognostic factors for the progression of keratoconus. Ophthalmology. 1994;101:439–47. doi: 10.1016/s0161-6420(94)31313-3. [DOI] [PubMed] [Google Scholar]
- 24.Shetty R, Kurian M, Anand D, Mhaske P, Narayana KM, Shetty BK. Intacs in advanced keratoconus. Cornea. 2008;27:1022–9. doi: 10.1097/ICO.0b013e318172fc54. [DOI] [PubMed] [Google Scholar]
- 25.Coskunseven E, Kymionis GD, Tsiklis NS, Atun S, Arslan E, Jankov MR, et al. One-year results of intrastromal corneal ring segment implantation (KeraRing) using femtosecond laser in patients with keratoconus. Am J Ophthalmol. 2008;145:775–9. doi: 10.1016/j.ajo.2007.12.022. [DOI] [PubMed] [Google Scholar]
- 26.Kymionis GD, Siganos CS, Tsiklis NS, Anastasakis A, Yoo SH, Pallikaris AI, et al. Long-term follow-up of intacs in keratoconus. Am J Ophthalmol. 2007;143:236–44. doi: 10.1016/j.ajo.2006.10.041. [DOI] [PubMed] [Google Scholar]
- 27.Torquetti L, Berbel RF, Ferrara P. Long-term follow-up of intrastromal corneal ring segments in keratoconus. J Cataract Refract Surg. 2009;35:1768–73. doi: 10.1016/j.jcrs.2009.05.036. [DOI] [PubMed] [Google Scholar]
- 28.Pesando PM, Ghiringhello MP, Di Meglio G, Romeo S. Treatment of keratoconus with ferrara ICRS and consideration of the efficacy of the ferrara nomogram in a 5-year follow-up. Eur J Ophthalmol. 2010;20:865–73. doi: 10.1177/112067211002000509. [DOI] [PubMed] [Google Scholar]
- 29.Vega-Estrada A, Alio JL, Brenner LF, Burguera-Gimenez N. Outcomes of intracorneal ring segments for the treatment of keratoconus: Five years follow-up analysis. 2013;39:1234–40. doi: 10.1016/j.jcrs.2013.03.019. [DOI] [PubMed] [Google Scholar]
- 30.Vega-Estrada A, Alio JL, Brenner LF, Javaloy J, Plaza Puche AB, Barraquer RI, et al. Outcome analysis of intracorneal ring segments for the treatment of keratoconus based on visual, refractive, and aberrometric impairment. Am J Ophthalmol. 2013;155:575–84.e1. doi: 10.1016/j.ajo.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 31.Tunc Z, Deveci N, Sener B, Bahcecioglu H. Corneal ring segments (INTACS) for the treatment of asymmetrical astigmatism of the keratoconus, follow-up after 2 years. J Fr Ophtalmol. 2003;26:824–30. [PubMed] [Google Scholar]
- 32.Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000;26:1117–22. doi: 10.1016/s0886-3350(00)00451-x. [DOI] [PubMed] [Google Scholar]
- 33.Boxer Wachler BS, Christie JP, Chandra NS, Chou B, Korn T, Nepomuceno R. Intacs for keratoconus. Ophthalmology. 2003;110:1031–40. doi: 10.1016/s0161-6420(03)00094-0. [DOI] [PubMed] [Google Scholar]
- 34.Ertan A, Kamburoglu G. Intacs implantation using a femtosecond laser for management of keratoconus: Comparison of 306 cases in different stages. J Cataract Refract Surg. 2008;34:1521–6. doi: 10.1016/j.jcrs.2008.05.028. [DOI] [PubMed] [Google Scholar]
- 35.Shabayek MH, Alio JL. Intrastromal corneal ring segment implantation by femtosecond laser for keratoconus correction. Ophthalmology. 2007;114:1643–52. doi: 10.1016/j.ophtha.2006.11.033. [DOI] [PubMed] [Google Scholar]
- 36.Siganos D, Ferrara P, Chatzinikolas K, Bessis N, Papastergiou G. Ferrara intrastromal corneal rings for the correction of keratoconus. J Cataract Refract Surg. 2002;28:1947–51. doi: 10.1016/s0886-3350(02)01495-5. [DOI] [PubMed] [Google Scholar]
- 37.Kwitko S, Severo NS. Ferrara intracorneal ring segments for keratoconus. J Cataract Refract Surg. 2004;30:812–20. doi: 10.1016/j.jcrs.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 38.Piñero DP, Alio JL, El Kady B, Coskunseven E, Morbelli H, Uceda-Montanes A, et al. Refractive and aberrometric outcomes of intracorneal ring segments for keratoconus: Mechanical versus femtosecond-assisted procedures. Ophthalmology. 2009;116:1675–87. doi: 10.1016/j.ophtha.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 39.Colin J. European clinical evaluation: Use of intacs for the treatment of keratoconus. J Cataract Refract Surg. 2006;32:747–55. doi: 10.1016/j.jcrs.2006.01.064. [DOI] [PubMed] [Google Scholar]
- 40.Kubaloglu A, Sari ES, Cinar Y, Koytak A, Kurnaz E, Ozerturk Y. Intrastromal corneal ring segment implantation for the treatment of keratoconus. Cornea. 2011;30:11–7. doi: 10.1097/ICO.0b013e3181e2cf57. [DOI] [PubMed] [Google Scholar]
- 41.Sansanayudh W, Bahar I, Kumar NL, Shehadeh-Mashour R, Ritenour R, Singal N, et al. Intrastromal corneal ring segment SK implantation for moderate to severe keratoconus. J Cataract Refract Surg. 2010;36:110–3. doi: 10.1016/j.jcrs.2009.07.040. [DOI] [PubMed] [Google Scholar]
- 42.Kanellopoulos AJ, Pe LH, Perry HD, Donnenfeld ED. Modified intracorneal ring segment implantations (INTACS) for the management of moderate to advanced keratoconus: Efficacy and complications. Cornea. 2006;25:29–33. doi: 10.1097/01.ico.0000167883.63266.60. [DOI] [PubMed] [Google Scholar]
- 43.Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000;26:1117–22. doi: 10.1016/s0886-3350(00)00451-x. [DOI] [PubMed] [Google Scholar]
- 44.Siganos D, Ferrara P, Chatzinikolas K, Bessis N, Papastergiou G. Ferrara intrastromal corneal rings for the correction of keratoconus. J Cataract Refract Surg. 2002;28:1947–51. doi: 10.1016/s0886-3350(02)01495-5. [DOI] [PubMed] [Google Scholar]
- 45.Alio JL, Artola A, Hassanein A, Haroun H, Galal A. One or 2 intacs segments for the correction of keratoconus. J Cataract Refract Surg. 2005;31:943–53. doi: 10.1016/j.jcrs.2004.09.050. [DOI] [PubMed] [Google Scholar]
- 46.Shabayek MH, Alio JL. Intrastromal corneal ring segment implantation by femtosecond laser for keratoconus correction. Ophthalmology. 2007;114:1643–52. doi: 10.1016/j.ophtha.2006.11.033. [DOI] [PubMed] [Google Scholar]
- 47.Pinero DP, Alio JL, El Kady B, Pascual I. Corneal aberrometric and refractive performance of 2 intrastromal corneal ring segment models in early and moderate ectatic disease. J Cataract Refract Surg. 2010;36:102–9. doi: 10.1016/j.jcrs.2009.07.030. [DOI] [PubMed] [Google Scholar]


