Abstract
This study presents a case report of the clinical presentation and management of a 47-year-old male myope who underwent photorefractive keratectomy (PRK) and developed bilateral sterile corneal infiltrates at 1 day post-operatively. The patient was successfully treated with aggressive topical antibiotic and topical steroid therapy. The final corrected distance visual acuity (CDVA) was 20/25 with faint corneal scarring. Peripheral sterile corneal infiltrate can occur after PRK with excellent prognosis. Infectious causes should be suspected in all cases of corneal infiltrate. The most likely cause of peripheral sterile corneal infiltrate in this case was pooling of the tear film containing antigens under the bandage contact lens.
Keywords: Corneal Scarring, Photorefractive Keratectomy, Post-operative Sterile Keratitis
INTRODUCTION
The peripheral cornea is pre-disposed to inflammatory reactions due to the rich vascular and lymphatic supply to the limbus and the presence of antigen presenting cells. Peripheral corneal infiltrates can occur due to different pathology including staphylococcal toxins from the lids, Terrien's marginal degeneration or ulcers associated with autoimmune or collagen vascular diseases.1,2
Photorefractive keratectomy (PRK) is common surgical procedure for the treatment of mild to moderate refractive error. Complications of this procedure include infectious and sterile keratitis. The pathogenesis of post-operative sterile keratitis remains unknown.3,4 However, some have postulated topical medications as a factor.5
In this report, we present a case of a patient who developed bilateral sterile infiltrates soon after PRK.
CASE REPORT
A 47-year-old male patient underwent bilateral PRK for myopic astigmatism. The patient was in good health, did not take any systemic medications and the ocular history was unremarkable. The pre-operative manifest refractions were −1.25 −1.00 × 110 right eye and −1.75 −0.50 × 70 left eye.
Bilateral PRK was performed on the same day. Two drops of topical anesthetic were instilled in the eye undergoing surgery. The eyes were draped with a plastic sheet. A lid speculum was inserted for maximum globe exposure. The corneal epithelium was removed by mechanical debridgement using a sponge soaked in topical oxybuprocaine hydrochloride 0.4% (benoxinate) and a surgical blade. The surgical procedure was uneventful and a bandage contact lens was placed at the end of surgery. The patient was discharged with instructions to instill topical ofloxacin 4 times a day and diclofenac sodium (Voltaren; Novartis AG, Basel, Switzerland) 6 times a day for pain. No topical steroids were prescribed.
One day post-operatively, the visual acuity was 20/25. Slit lamp examination revealed bilateral corneal infiltrates outside the treatment zone with intact epithelium and clean central epithelial defects and quiet anterior chambers [Figure 1].
Figure 1.
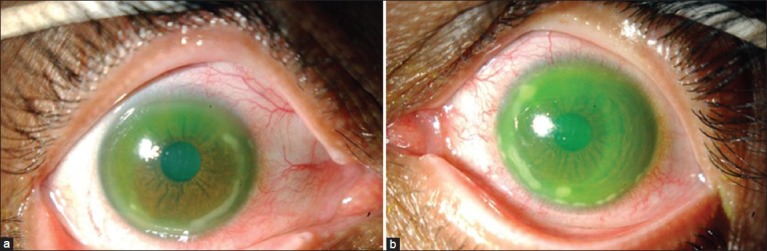
(a) Right eye and (b) left eye of a patient who underwent photorefractive keratectomy and presented with bilateral paralimbal infiltrates outside the optical zone at day one post-operatively
The contact lenses were removed and corneal scrapings were sent for microbial studies. The patient was placed on topical steroid 4 times a day and topical ofloxacin hourly and the voltaren was stopped.
Microbiology studies were negative for any microorganisms. Two days post-operatively, the corneal infiltrates were less prominent than at original presentation. By the sixth post-operative day, the epithelium had completely healed bilaterally. The patient improved on topical steroid and antibiotics within 2 weeks. The central corneas remained clear throughout follow-up. Steroids were tapered over a month and the infiltrates resolved with faint peripheral corneal scarring and final CDVA of 20/25 [Figure 2].
Figure 2.
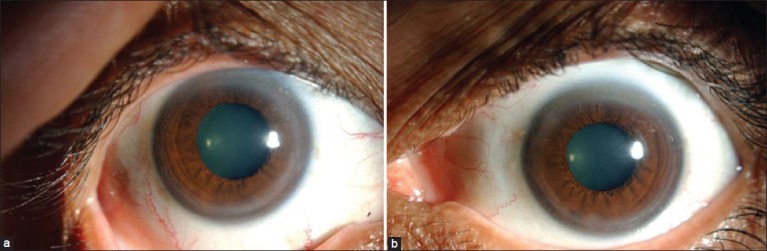
Complete resolution of infiltrates in the (a) right eye and (b) left eye of a patient who developed bilateral paralimbal infiltrates after photorefractive keratectomy
DISCUSSION
In the current case, there were no pre-disposing ocular or systemic factors for peripheral corneal inflammation. Although rare, corneal infiltrates after PRK have been reported.3,4 Some have postulated the use of topical non-steroidal anti-inflammatory agents (NSAIDs) post-operatively can cause corneal infiltrates.3,4 NSAIDs inhibit the cycloxygenase pathway for the metabolism of arachadonic acid. This inhibition causes increased production of leukotrienes and hydroxyeicosatetraenoic acid from the alternate pathway mediated by lipoxygenase. These chemoattractants result in a deposition of inflammatory cells causing infiltrates.1,5 Steroids block leukotrienes and the synthesis of arachidonic acid from the phospholipids.5 In the current case, the patient was instructed to instill topical diclofenac immediately post-operatively every 6 h. No topical steroids were instilled. Although, sterile infiltrates are often multifocal, they are associated with various pathologic conditions and can be caused by an immune etiology. Angunawela et al.6 reported similar findings after corneal cross linking in keratoconus case and they hypothesized the possibility of pooling of the tear film consisting of antigens under the bandage contact lens, possibly staphylococcal. We concur with this tear film/antigen hypothesis rather than the alternate of topical medications (e.g., NSAIDs) as the initiating factor. Until this case, we elected to begin topical steroid on the post-operative day one rather than immediately post-operatively. However, after this case, we prescribe topical steroid immediately post-operatively. Of note, we have never encountered similar findings in our refractive practice, which is mostly (at least 90%) PRK.
Differentiate between infection and inflammation is difficult as infiltrates can occur with both conditions. Hence, we elected to perform corneal scrapings and microbial studies due to the potential of significant complications and visual loss from an infectious etiology. Sterile infiltrates, with sudden onset can be successfully treated with an aggressive steroid therapy to avoid significant corneal scarring.
In conclusion, sterile corneal infiltrate is rare after refractive surgery. The most likely cause of paralimbal sterile corneal infiltrates in this case was antigens contained in the pooled tear film under the bandage contact lens. Treatment is usually successful with excellent prognosis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lahners WJ, Hardten DR, Lindstrom RL. Peripheral keratitis following laser in situ keratomileusis. J Refract Surg. 2003;19:671–5. doi: 10.3928/1081-597X-20031101-10. [DOI] [PubMed] [Google Scholar]
- 2.Lifshitz T, Levy J, Mahler O, Levinger S. Peripheral sterile corneal infiltrates after refractive surgery. J Cataract Refract Surg. 2005;31:1392–5. doi: 10.1016/j.jcrs.2004.12.057. [DOI] [PubMed] [Google Scholar]
- 3.Teal P, Breslin C, Arshinoff S, Edmison D. Corneal subepithelial infiltrates following excimer laser photorefractive keratectomy. J Cataract Refract Surg. 1995;21:516–8. doi: 10.1016/s0886-3350(13)80208-8. [DOI] [PubMed] [Google Scholar]
- 4.Sher NA, Frantz JM, Talley A, Parker P, Lane SS, Ostrov C, et al. Topical diclofenac in the treatment of ocular pain after excimer photorefractive keratectomy. Refract Corneal Surg. 1993;9:425–36. [PubMed] [Google Scholar]
- 5.Ku EC, Lee W, Kothari HV, Scholer DW. Effect of diclofenac sodium on the arachidonic acid cascade. Am J Med. 1986;80:18–23. doi: 10.1016/0002-9343(86)90074-4. [DOI] [PubMed] [Google Scholar]
- 6.Angunawela RI, Arnalich-Montiel F, Allan BD. Peripheral sterile corneal infiltrates and melting after collagen crosslinking for keratoconus. J Cataract Refract Surg. 2009;35:606–7. doi: 10.1016/j.jcrs.2008.11.050. [DOI] [PubMed] [Google Scholar]


