Abstract
A 50-year-old male was referred with a previous history of conjunctival flap (CF) for a nonhealing fungal corneal ulcer with extreme corneal thinning in the right eye. The peritomy for the CF extended from 6:30 to 9:30 clock h on the cornea. The CF was disengaged, peritomy area deepithelialized, and CF was repositioned. He later underwent penetrating keratoplasty and achieved 20/40 best corrected visual acuity. The authors present a new concept for surgically repositioning CF s to the original site immediately after healing of the corneal ulcer.
Keywords: Limbal Stem Cell Deficiency, Conjunctival Flap, Cornea, Corneal Perforation, Corneal Ulcer
INTRODUCTION
Conjunctival flaps (CFs) have been used to treat recalcitrant corneal ulcers.1 Currently with introduction of newer therapeutic options such as cyanoacrylate tissue adhesive,2 amniotic membrane transplants3 therapeutic deep anterior lamellar keratoplasty (DALK)4 and penetrating keratoplasty (PKP),5 CFs are rarely used. However, in an emergency situation, CFs may be used as a temporary measure. Conventionally, CFs can remain on for few months and are excised before attempting DALK or PKP. Associated deep corneal vascularization predisposes these patients to allograft rejection. We present a new concept for surgical repositioning of the CFs to the original site.
CASE REPORT
A 50-year-old male had complaints of pain, redness, watering, and diminution of vision in the right eye for 4 weeks. The patient had a previous history of a 5.0 × 4.5 mm corneal ulcer and marked corneal thinning in the right eye. He did not show any improvement after 2 weeks of topical and systemic antifungal treatment. The referring ophthalmologist performed a CF in the right eye. After 2 weeks, patient did not show any improvement in symptoms and was referred to us for further treatment.
On examination, the patient's visual acuity was count fingers in the right eye and 20/20 in the left eye. Slit-lamp biomicroscopy revealed a thick CF including Tenon's capsule, extending 6.5 mm on the right cornea. The limbal conjunctiva had been removed from 6:30 to 9:30 clock h [Figure 1a]. The projecting 10-0 nylon sutures were removed. Left eye on examination was normal. We elected to reposit the CF with the method described below.
Figure 1.
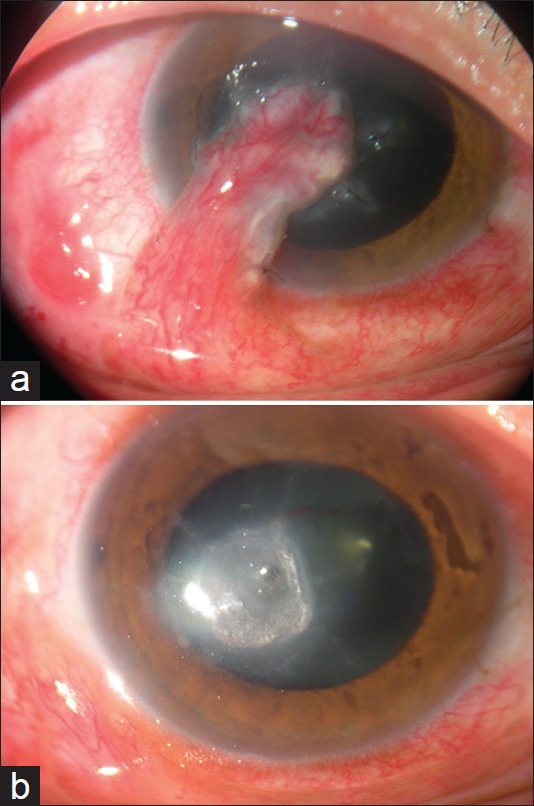
(a) Conjunctival flap done for nonhealing fungal corneal ulcer (right eye). (b) Healthy limbus and leukomatous corneal opacity (right eye)
Repositioning of the CF
A low-dose peribulbar anesthesia (5 mL) was delivered containing 2.5 mL each, of xylocaine (2%) and bupivacaine (1%). The eye was prepared in a sterile fashion and draped. A Barraquer wire eyelid speculum was inserted for adequate globe exposure. First, the wound was evaluated. The peritomy area was deepithelialized. The CF was disengaged, fibrous tissue was excised and the CF was resutured to the original position with interrupted 8-0 vicryl sutures. The excision of the CF left behind a corneal epithelial defect, corneal opacity, and corneal thinning. A bandage contact lens (BCL) was applied. The patient was placed on moxifloxacin 0.3%, natamycin suspension 5%, and cyclopentolate hydrochloride 1% three times daily. The epithelial defect healed within a week and the BCL was removed. The corneal ulcer healed resulting in avascular corneal opacity [Figure 1b].
At 3 months follow-up, corneal opacity persisted and best corrected visual acuity was 20/200. The patient underwent an uneventful PKP. Over 4 years of follow-up, the patient achieved a best corrected visual acuity of 20/40 and the graft remained clear.
DISCUSSION
CFs have been used in the treatment of herpetic corneal ulceration, neuroparalytic keratitis, keratitis sicca, severe marginal ulceration, and chemical eye burns.1 Conjunctival flaps may be rarely considered for recalcitrant bacterial or fungal corneal ulcers.1 In our patient, conjunctival flap was performed for resistant fungal corneal ulcer. In general, CFs promote wound healing and improve comfort. CFs promote healing of refractory corneal ulcers through two mechanisms. First, pedicle CFs, rich in blood vessels and lymphatics, transport nutrients including cellular components and growth factors to the corneal surface and increase the resistance to infection. Second, the rich blood supply of CFs also decreases proinflammatory mediators and proteases in the microenvironment. The immune modulator wash out further decreases the inflammation and aiding the healing of refractory corneal ulcers.6
Gunderson's conjunctival flaps are commonly performed. These involve 360° peritomy and mobilization of conjunctiva at the fornix to cover the entire corneal surface.1 Gunderson's conjunctival flap covers the whole cornea making monitoring of the corneal disease difficult. Fornix shortening, ptosis, corneal opacification, conjunctivilization of the cornea, and extensive corneal vascularization are other disadvantages of conjunctival flaps. In a bucket handle type of conjunctival flap, 180° peritomy is performed, the conjunctiva is separated from the underlying Tenon's capsule, an incision parallel to the limbus is given and the conjunctiva is mobilized to cover the corneal ulcer. The microsurgical technique of using a selective pedunculated (pedicle) conjunctival flap provides an alternative method to Gunderson's flaps, in instances when only partial protection and/or additional cure of diseased cornea is required. The pedicle conjunctival flap can be used either as a thin flap (without Tenon's capsule) for superficial corneal ulcer, or as a thick flap (with Tenon's capsule) for deep corneal ulcer. Therefore, the pedicle conjunctival flap can restore ocular surface integrity and provide metabolic and mechanical support for corneal ulcer. A selective pedunculated conjunctival flap as performed in our patient, covering the ulcerated cornea only and avoiding the complications of Gunderson's conjunctival flaps.7 The pedicle conjunctival flaps are favored to cover the peripheral or paracentral corneal ulcer. Thus, the type of conjunctival flap may be selected according to the size and location of the corneal ulcer. CFs are usually not successful in active fungal corneal ulcers resistant to topical and systemic antifungals. The major reason for the failure is incomplete removal of necrotic tissue. In a recent study, anterior segment–optical coherence tomography guided removal of necrotic tissue combined with CFs has been successful in healing resistant fungal corneal ulcers.8
Clinically, limbal stem cell (LSC) deficiency is characterized by conjunctivilization, vascularization, chronic inflammation, poor epithelial integrity, irregular corneal surface, recurrent erosions and persistent epithelial defect.9 LSC deficiency may be categorized as primary or secondary. Secondary LSC deficiency following multiple surgeries involving superior limbus has been termed as iatrogenic LSC deficiency.10 Chronic ocular surface inflammation has also been reported to cause LSC deficiency.10 In application of conjunctival flaps large area of limbal conjunctiva harboring LSC is sacrificed and concomitant chronic ocular surface inflammation may cause iatrogenic LSC damage. The surgical removal of LSC coupled with loss due to chronic inflammation may predispose to LSC deficiency.
The conjunctival flaps reside on the corneal surface for a considerable time even after healing of the corneal disease. Long-standing conjunctival flaps may enhance conjunctivilization, corneal opacification, and corneal vascularization. Conventionally, conjunctival flaps are excised prior to PKP. With the current understanding of LSC locus and their role in corneal epithelial homeostasis, the excision of CF may cause significant loss of LSC. A more conservative approach, in which LSC are preserved may be more appropriate. In our view, the conjunctival flaps may be disengaged and sutured at the original position to limit LSC damage. Early repositioning of the conjunctival flap immediately after healing of the corneal disease is beneficial as the prolonged presence of conjunctival flap on the cornea enhances ocular surface damage. After removal of the CF, the cornea may be thin and vascularized. We consider amniotic membrane graft in these cases at the time of removal. In case, the cornea is very thin one may consider an application of multilayered amniotic membrane. Amniotic membrane graft increases the corneal thickness and decreases the corneal vascularization, once the corneal ulcer heals.
In our experience repositioning of the CFs to the original site, within few weeks of healing preserves LSCs and provides better cosmesis. Early repositioning also avoids corneal vascularization, which minimizes the risk of allograft rejection. The authors advocate repositioning of CFs to the original position, as it is a simple surgical procedure and does not cause any complications.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Khodadoust A, Quinter AP. Microsurgical approach to the conjunctival flap. Arch Ophthalmol. 2003;121:1189–93. doi: 10.1001/archopht.121.8.1189. [DOI] [PubMed] [Google Scholar]
- 2.Sharma A, Kaur R, Kumar S, Gupta P, Pandav S, Patnaik B, et al. Fibrin glue versus N-butyl-2-cyanoacrylate in corneal perforations. Ophthalmology. 2003;110:291–8. doi: 10.1016/S0161-6420(02)01558-0. [DOI] [PubMed] [Google Scholar]
- 3.Kitagawa K, Yanagisawa S, Watanabe K, Yunoki T, Hayashi A, Okabe M, et al. A hyper dry amniotic membrane patch using a tissue adhesive for corneal perforations and bleb leaks. Am J Ophthalmol. 2009;148:383–9. doi: 10.1016/j.ajo.2009.03.030. [DOI] [PubMed] [Google Scholar]
- 4.Noble BA, Agrawal A, Collins C, Saldana M, Brogden PR, Zuberbuhler B. Deep Anterior Lamellar Keratoplasty (DALK): Visual outcome and complications for a heterogeneous group of corneal pathologies. Cornea. 2007;26:59–64. doi: 10.1097/01.ico.0000240080.99832.f3. [DOI] [PubMed] [Google Scholar]
- 5.Xie L, Zhai H, Shi W. Penetrating keratoplasty for corneal perforations in fungal keratitis. Cornea. 2007;26:158–62. doi: 10.1097/01.ico.0000248381.24519.0d. [DOI] [PubMed] [Google Scholar]
- 6.Zhou Q, Long X, Zhu X. Improved conjunctival transplantation for corneal ulcer. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2010;35:814–8. doi: 10.3969/j.issn.1672-7347.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 7.Sandinha T, Zaher SS, Roberts F, Devlin HC, Dhillon B, Ramaesh K. Superior forniceal conjunctival advancement pedicles (SFCAP) in the management of acute and impending corneal perforations. Eye (Lond) 2006;20:84–9. doi: 10.1038/sj.eye.6701814. [DOI] [PubMed] [Google Scholar]
- 8.Sun GH, Li SX, Gao H, Zhang WB, Zhang MA, Shi WY. Clinical observation of removal of the necrotic corneal tissue combined with conjunctival flap covering surgery under the guidance of the AS-OCT in treatment of fungal keratitis. Int J Ophthalmol. 2012;5:88–91. doi: 10.3980/j.issn.2222-3959.2012.01.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Puangsricharern V, Tseng SC. Cytologic evidence of corneal diseases with limbal stem cell deficiency. Ophthalmology. 1995;102:1476–85. doi: 10.1016/s0161-6420(95)30842-1. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz GS, Holland EJ. Iatrogenic limbal stem cell deficiency. Cornea. 1998;17:31–7. doi: 10.1097/00003226-199801000-00006. [DOI] [PubMed] [Google Scholar]


