Abstract
A 23 year old female patient presented with the chief complaint of gummy smile after previously undergoing Orthodontic treatment. Patient had a straight profile with competent lips and during posed and unposed smile the patient exhibited excessive gingival display. Since the patient was unwilling to undergo Orthodontic treatment and apprehensive about surgical procedures, this problem was addressed by injecting Botulinum toxin type-A as an alternative treatment approach. Two weeks post treatment; on follow up examination, improved results were seen without any side effects. As a result, an attractive and confident smile was perceived by the patient.
How to cite the article: Dinker S, Anitha A, Sorake A, Kumar K. Management of gummy smile with Botulinum Toxin Type-A: A case report. J Int Oral Health 2014;6(1):111-5.
Key Words: : Botulinum toxin, excessive gingival display, gummy smile
Introduction
Smile plays a pivotal role in conveying the emotion of a person. In Orthodontics, smile aesthetics is considered to be an important part of any treatment objective. Gummy smile is a term used to describe excessive display of gingival tissue in the maxilla upon smiling. This can cause undue psychological hindrance as the individual with excessive gingival display will be self-conscious and at unease regarding the same and thus seek treatment. 1 Cosmetic surgical procedures like the use of Botulinum toxin type-A, dermal fillers, Orthodontic and Orthognathic procedures, dental bleaching and other dental cosmetic substitutes are widely requested by the adults. 2 The advantages of these procedures are definitive increase in self esteem. However, some of these procedures are more time consuming than the others which can further cause impaired psychological effects especially in adults.
Botulinum toxin has been widely used for the treatment of various conditions associated with pain and excessive muscle contraction since the 1970s. Clostridium botulinum is an anaerobic bacterium responsible for its production. Among the 8 different serotypes of Botulinum toxin that exists, Type A (BTX-A) is the most potent and the most commonly used clinically. Fermentation of Clostridium botulinum leads to a formation of purified BTX-A which is a stable, sterile, vacuum-dried powder that is diluted with saline solution without preservatives. 3 This favours the weakening of skeletal muscles by cleaving the synaptosomal-associated protein SNAP-25, thus inhibiting the release of acetylcholine from the motor-neuron and enabling the repolarization of the postsynaptic term. 4
The purpose of this case report was to show case the use of Botulinum toxin type – A for the treatment of gummy smile as an alternative treatment approach. The patient had previously undergone Orthodontic treatment and was unwilling for Orthognathic surgery. On clinical examination, hyperactive upper lip elevator muscles were seen which was the primary cause for excessive gingival
display. Botulinum toxin type – A has been used previously for the treatment of gummy smile with the same etiology. 5 , 6 This is a case report were the gummy smile was treated by similar means.
Diagnosis and Etiology
A 23 year old female patient presented to the clinic with the chief complaint of excessive gingival display. Pretreatment photographs showed a straight profile with competent lips ( Figure 1 ). On smiling, both posed and unposed, clearly indicated that the patient had excessive show of gingiva and the patient was very conscience of the same (Figure 2a , 2b ) Close-up photographs were taken with a metallic scale placed vertically, such that it coincided
Figure 1: Pre treatment photo – Profile view.
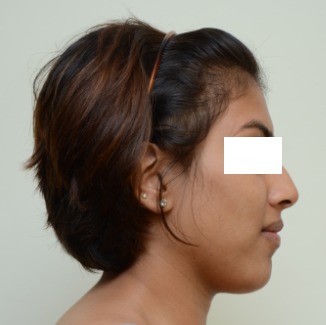
Figure 2a: Pre-treatment - Posed smile.

Figure 2b: Pre-treatment - Unposed smile.

with the facial midline during posed and unposed smile. 4-5mm of gingival exposure was seen in the incisor region during posed smile ( Figure 3a ). With spontaneous, unposed smile, as detected by the expression of the eyes, patient showed a gingival display of 8-10mm ( Figure 3b ). On further examination, hyperactive upper lip elevator muscles were seen.
Figure 3a: Pre-treatment – Close-up Posed smile.
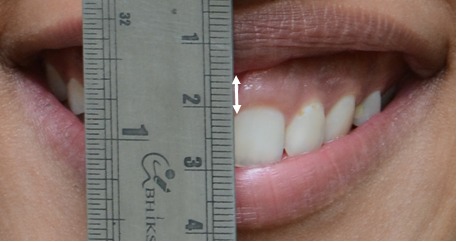
Figure 3b: Pre-treatment – Close-up Posed smile.

Treatment Objective
The photographs clearly showed the presence of excessive gingival display with hyperactive upper lip elevator muscles. As the patient was unwilling to undergo Orthodontic or Orthognathic surgery, the treatment objective was to treat the gummy smile with Botulinum toxin type- A.
Treatment Progress
During the initial visit, all forms and consents were explained to the patient and signed accordingly. Patient’s
medical history was reviewed as well. Before injecting the solution, patient underwent a standardised photographic session. Photographs were taken using Nikon D7000 camera. The procedure was performed by a Dermatologist who was also a Botox certified physician. 7 Botulinum toxin type-A was diluted according to manufacturer’s recommendations to provide 2.5 units per 0.1ml by adding 4.0 ml normal saline solution to 100 units of vacuum-dried Clostridium botulinum toxin type-A. Under sterile conditions, 2.5 units were then injected at 2 sites per side in both overlapping points of the right and left levator labii superioris alaeque nasi, levator labii superioris and zygomaticus minor and levator labii superioris muscle sites ( Figure 4 ). 8 The sites for injection were determined to
Figure 4: Musculature of the face: Pinpointing sites for injection.
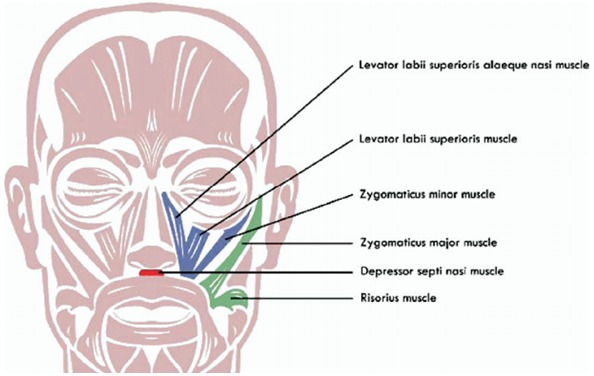
ensure accurate locations of the muscle. This was carried out by asking the patient to smile and simultaneously palpate the muscles on contraction. No local anaesthesia was administered and no electromyographic guidance was used.
Treatment Results
Facial photographs were recorded after two week post
treatment using the same equipment. Extreme effort was placed on obtaining standardised, unposed, spontaneous smiles (Figure 5a , 5b , 5c ). Remarkable improvement in the lip profile was seen and gummy smile reduced to a normal range.
Figure 5a: Post-treatment - Posed smile.

Figure 5b: Post-treatment - Unposed smile.

Figure 5c: Post-treatment - Unposed smile.

Discussion
The cause for gummy smiles can be of skeletal, dentoalveolar or soft tissue in origin. The skeletal type is caused by excessive growth of the maxilla in vertical direction and is commonly associated with long-face
syndrome. 9 , 10 This condition is often corrected with Orthognathic surgery. Dentoalveolar type could be treated by using micro implants. However, this form of treatment
will require fixed mechanotherapy at the same time. For the patient whose gummy smile was mainly caused due to hyperactive lip muscles, treatment with Botox was considered as an alternative treatment approach. Muscles of facial expression responsible for upper lip elevation and lateral retraction upon smiling are LLSAN, LLS, Zm, zygomaticus major (ZM), risorius, and, to a lesser degree, the depressor septi nasi muscle. All of these muscles interact with the orbicularis oris muscle in the production of a smile. The mechanism involved was well described in 2 cadaver studies, by Rubin et al11 and another by Pessa. 12 Rubin et al concluded that the LLS, the ZM, and the superior fibers of the buccinator muscles under the nasolabial fold helps to produce a full smile. Pessa indicated that the LLSAN was responsible for the formation of the medial portion of the fold and minimally responsible for the elevation of the upper lip and smile formation. He also found that the ZM and the Zm muscles are primarily responsible for the production of the smile.
Botulinum toxin type-A aids to inhibit the release of acetylcholine by blocking the neuromuscular transmission and binding to acceptor sites on motor or sympathetic nerve terminals. This inhibition occurs as the neurotoxin cleaves SNAP- 25, a protein integral to the successful docking and release of acetylcholine from vesicles in nerve endings. 13 , 14 When injected intramuscularly at therapeutic doses, it produces partial chemical denervation of the muscle, resulting in localized reduction in muscle activity. Botox has been approved by the Food and Drug Administration as a safe and effective therapy for blepharospasm, strabismus, cervical dystonia, hemifacial spasm and primary axillary hyperhidrosis. The National Institutes of Health Consensus Conference of 1990 also included it as a safe and effective therapy for other unlabelled uses. The use of Botulinum toxin type-A has been extensively described in literature, especially for various cosmetic procedures. 15 After injecting 1.25U Botulinum toxin on both the side, reduction in excessive gingival display was noticed with maximum effect
following 2 weeks. Gingival display gradually increased, but even at the end of 24 weeks, average gingival exposure was still retained.
Conclusion
The Botulinum toxin type-A injection which was used for the correction of excessive gingival display caused by hyperactive upper lip elevator muscles was seen to be highly effective. The results were extremely satisfactory for both the patient and the orthodontist. Even though Botox has a transitory effect, six months post treatment the gummy smile was still seen to be within the normal range. Hence, depending on the cause and the needs of the patient, this treatment approach could well be used as an alternative procedure for faster and minimally invasive treatment of gummy smile.
Footnotes
Source of Support: Nil
Conflict of Interest: None
Contributor Information
Sudeeptha Dinker, Department Of Orthodontics & Dento-Facial Orthopedics, A J Institute of Dental Sciences, Mangalore, Karnataka, India.
A Anitha, Department Of Orthodontics & Dento-Facial Orthopedics, A J Institute of Dental Sciences, Mangalore, Karnataka, India.
Abhinay Sorake, Department Of Orthodontics & Dento-Facial Orthopedics, A J Institute of Dental Sciences, Mangalore, Karnataka, India.
Kishore Kumar, Department Of Orthodontics & Dento-Facial Orthopedics, A J Institute of Dental Sciences, Mangalore, Karnataka, India.
References
- 1.C Flanary. The psychology of appearance and the psychological impact of surgical alteration of the face. Philadelphia:WB Saunders. 1992:2–21. [Google Scholar]
- 2.EL Gottlieb. By the numbers. J Clin Orthod. 1999;33:278–281. [PubMed] [Google Scholar]
- 3.R Ananthanarayanan, CK Panicker. Textbook of microbiology, 7th ed. Hyderabad, India:Orient Longman. 2005 [Google Scholar]
- 4.GW Jaspers, J Pijpe, J Jansma. The use of botulinum toxin type A in cosmetic facial procedures. Int J Oral Maxillofac Surg. 2011;40:127–133. doi: 10.1016/j.ijom.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 5.WS Hwang, MS Hur, KS Hu, WC Song, KS Koh, HS Baik, ST Kim, HJ Kim, KJ Lee. Surface anatomy of the lip elevator muscles for the treatment of gummy smile using botulinum toxin. Angle Orthod. 2009;79:70–77. doi: 10.2319/091407-437.1. [DOI] [PubMed] [Google Scholar]
- 6.M Polo. Botulinium toxin type A in the treatment of excessive gingival display. Am J Orthod Dentofacial Orthop. 2005;127:214–218. doi: 10.1016/j.ajodo.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 7.JA Neville, TS Housman, JA Letsinger, Jr Fliesher AB, SR Feldman, PM Williford. Increase in procedures performed at dermatology office visits from 1995 to 2001. Dermatol Surg. 2005;31:160–162. doi: 10.1111/j.1524-4725.2005.31037. [DOI] [PubMed] [Google Scholar]
- 8.M Polo. Botulinum toxin type A (Botox) for the neuromuscular correction of excessive gingival display on smiling (gummy smile) Am J Orthod Dentofacial Orthop. 2008;133:195–203. doi: 10.1016/j.ajodo.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 9.WR Proffit, HW Fields, DM Sarver. Contemporary orthodontics. St Louis:Mosby Year Book. 2007 [Google Scholar]
- 10.JW Robbins. Differential diagnosis and treatment of excess gingival display. Pract Periodont Aesthet Dent. 1999;11:265–272. [PubMed] [Google Scholar]
- 11.LR Rubin. The anatomy of a smile: its importance in the treatment of facial paralysis. Plast Reconstr Surg. 1974;53:384–387. doi: 10.1097/00006534-197404000-00002. [DOI] [PubMed] [Google Scholar]
- 12.MF Brin, M Hallett, J Jankovic. Scientific and therapeutic aspects of botulinum toxin. Philadelphia:Lippincott Williams and Wilkins. 2002:v–vi. [Google Scholar]
- 13.AV Benedetto. The cosmetic uses of botulinum toxin type A. Int J Dermatol. 1999;38:641–655. doi: 10.1046/j.1365-4362.1999.00722.x. [DOI] [PubMed] [Google Scholar]
- 14.WJ Binder, A Blitzer, MF Brin. Treatment of hyperfunctional lines of the face with botulinum toxin A. Dermatol Surg. 1998;24:1198–1205. doi: 10.1111/j.1524-4725.1998.tb04098.x. [DOI] [PubMed] [Google Scholar]
- 15.toxin Botulinum. Consens Statement. 1990;8(8):1–20. [PubMed] [Google Scholar]


