Summary
Background
Body-mass index (BMI) and diabetes have increased worldwide, whereas global average blood pressure and cholesterol have decreased or remained unchanged in the past three decades. We quantified how much of the effects of BMI on coronary heart disease and stroke are mediated through blood pressure, cholesterol, and glucose, and how much is independent of these factors.
Methods
We pooled data from 97 prospective cohort studies that collectively enrolled 1·8 million participants between 1948 and 2005, and that included 57 161 coronary heart disease and 31 093 stroke events. For each cohort we excluded participants who were younger than 18 years, had a BMI of lower than 20 kg/m2, or who had a history of coronary heart disease or stroke. We estimated the hazard ratio (HR) of BMI on coronary heart disease and stroke with and without adjustment for all possible combinations of blood pressure, cholesterol, and glucose. We pooled HRs with a random-effects model and calculated the attenuation of excess risk after adjustment for mediators.
Findings
The HR for each 5 kg/m2 higher BMI was 1·27 (95% CI 1·23–1·31) for coronary heart disease and 1·18 (1·14–1·22) for stroke after adjustment for confounders. Additional adjustment for the three metabolic risk factors reduced the HRs to 1·15 (1·12–1·18) for coronary heart disease and 1·04 (1·01–1·08) for stroke, suggesting that 46% (95% CI 42–50) of the excess risk of BMI for coronary heart disease and 76% (65–91) for stroke is mediated by these factors. Blood pressure was the most important mediator, accounting for 31% (28–35) of the excess risk for coronary heart disease and 65% (56–75) for stroke. The percentage excess risks mediated by these three mediators did not differ significantly between Asian and western cohorts (North America, western Europe, Australia, and New Zealand). Both overweight (BMI ≥25 to <30 kg/m2) and obesity (BMI ≥30 kg/m2) were associated with a significantly increased risk of coronary heart disease and stroke, compared with normal weight (BMI ≥20 to <25 kg/m2), with 50% (44–58) of the excess risk of overweight and 44% (41–48) of the excess risk of obesity for coronary heart disease mediated by the selected three mediators. The percentages for stroke were 98% (69–155) for overweight and 69% (64–77) for obesity.
Interpretation
Interventions that reduce high blood pressure, cholesterol, and glucose might address about half of excess risk of coronary heart disease and three-quarters of excess risk of stroke associated with high BMI. Maintenance of optimum bodyweight is needed for the full benefits.
Funding
US National Institute of Health, UK Medical Research Council, National Institute for Health Research Comprehensive Biomedical Research Centre at Imperial College Healthcare NHS Trust, Lown Scholars in Residence Program on cardiovascular disease prevention, and Harvard Global Health Institute Doctoral Research Grant.
Introduction
Cardiovascular diseases, especially coronary heart disease and stroke, are the leading causes of death worldwide.1 High body-mass index (BMI) is an important cardiovascular disease risk factor,2–4 and raised blood pressure, cholesterol, and glucose partly mediate its effects.5,6 Present behavioural interventions for weight management are only effective in the short term,7,8 most weight-loss drugs lack either sustained efficacy or an acceptable safety profile,9,10 and surgical methods are recommended only for very obese individuals.11,12 This situation has created concerns about a potentially massive worldwide increase in cardiovascular diseases as a result of increased BMI and prevalence of overweight and obesity in most countries.13–15 By contrast, effective clinical and public health interventions for blood pressure and cholesterol are available, as evidenced by large decreases in these measures in some countries despite rises in obesity.14,16,17 Therefore, an important clinical and public health question is: to what extent can the adverse effects of high BMI be mitigated by targeting its metabolic mediators?
To answer this question we need a detailed understanding of how much of the effect of excess weight on cardiovascular disease is mediated by these metabolic factors, separately and in combinations, which are relevant for individual patients or populations. Whether the extent of mediation differs by population characteristics is also important to understand—eg, Asian versus western populations (North America, western Europe, Australia, and New Zealand)—because of physiological differences in how BMI affects intermediate metabolic risks or differences in the extent to which health-care systems have addressed the mediating metabolic risks.
Some researchers have investigated the mediated effects of BMI on coronary heart disease through blood pressure, cholesterol, and diabetes together;3,18–21 fewer studies have been done for stroke,3,19,22,23 which is the largest cause of death in Asian populations.1 However, these studies did not assess whether characteristics of study populations affect the extent of mediation because the number of events was insufficient or data were comprised of participants from one or two regions. Importantly, these studies did not quantify the role of individual mediators or all possible combinations of two mediators that are needed to select clinical and public health interventions.
We quantified how much of the effects of high BMI, overweight, and obesity, on coronary heart disease and stroke are mediated through blood pressure, serum cholesterol, and glucose, individually and in all possible combinations by analysing data from 97 prospective cohort studies. We also assessed whether the extent of mediation was modified by geographical region, study period, and other characteristics of study populations.
Methods
Cohort identification and selection
We identified cohorts through a review of published articles and through the National Heart, Lung, and Blood Institute (NHLBI, Bethesda, MD, USA), and through personal communication with researchers.
Two reviewers independently assessed the studies and deemed them eligible if they met the following criteria: prospective design with at least 1 year of follow-up; participants were not selected based on previous history of coronary heart disease or stroke; height and weight were measured at baseline; at least one of the mediators (blood pressure, serum cholesterol, and blood glucose, or diabetes) was also measured at baseline; fatal or non-fatal coronary heart disease or both, or stroke were ascertained during follow-up.
We contacted investigators from 126 eligible cohorts, of which 68 (54%) agreed to participate. Seven of these cohorts were subsequently excluded because the participants all had previous cardiovascular disease (three studies), the reported outcome was only total cardiovascular disease (three studies), or the analysis could not adjust for smoking (one study). Collaborating Group members of the other 61 cohorts reanalysed their data with a consistent protocol. We obtained additional data from nine cohorts through a special request to the NHLBI and from 27 cohorts in the Asia Pacific Cohort Studies Collaboration (APCSC) through its participation in the Global Burden of Metabolic Risk Factors for Chronic Diseases Study.14–17
We analysed data from 97 prospective cohort studies. Of these, nine studies were not included in the coronary heart disease analysis and 11 in the stroke analysis because they did not report the corresponding disease outcome or had fewer than five events. All data were de-identified, and the study protocol was approved by the institutional review board at the Harvard School of Public Health (Boston, MA, USA).
Eligibility, exposure definition, mediators, and potential confounders
In each cohort, we excluded participants who were younger than 18 years; had a BMI of lower than 20 kg/m2; had a history of coronary heart disease or stroke before enrolment; were missing data for age, sex, smoking status, height, or weight; or did not have data for mediators at baseline. We used BMI as the main measure of adiposity because it was measured in every cohort; data for waist circumference or waist-to-hip ratio were available in 17 cohorts and were analysed in sensitivity analyses. In the primary analysis, we accepted different metrics for mediators, including systolic blood pressure or hypertension status for blood pressure; total, HDL and LDL cholesterol concentrations, or hypercholesterolaemia for serum cholesterol; and fasting and postprandial glucose, haemoglobin A1c, or diabetes status for blood glucose. Table 1 shows the number of cohorts providing each measure and the appendix (pp 8–14) provides cohort details. We adjusted for age, sex, and smoking status as the minimum set of potential confounders, and for additional variables in individual cohorts as available (appendix, pp 8–14). We obtained data for BMI, mediators, and potential confounder from baseline examinations.
Table 1.
Mediators analysed by participating cohorts in the main analysis
| Number of cohorts | |
|---|---|
| Blood pressure | |
| Systolic blood pressure | 95 |
| Hypertension | 2 |
| Cholesterol | |
| Total serum cholesterol | 86 |
| HDL cholesterol | 1 |
| Hypercholesterolaemia | 1 |
| Blood glucose | |
| Fasting glucose | 39 |
| Postprandial glucose* | 18 |
| Haemoglobin A1c | 1 |
| Diabetes | 19 |
One cohort reported casual (or random) glucose. For each cohort, only one metric was extracted for each mediator in the main analysis.
Follow-up and outcome definitions
Our primary outcomes were the first occurrence of coronary heart disease or stroke event. Coronary heart disease included fatal or non-fatal ischaemic heart disease, including acute myocardial infarction and angina pectoris; stroke included fatal or non-fatal cerebral infarction, and intracerebral or subarachnoid haemorrhage. We followed up each participant until the first occurrence of the corresponding outcome, death, or loss to follow-up, whichever occurred first.
Statistical analysis
We used Cox proportional hazards regression to estimate the hazard ratios (HRs) in each cohort. We analysed BMI as a continuous variable in relation to risk of coronary heart disease and stroke after excluding participants with a BMI of less than 20 kg/m2 at baseline because the associations of BMI with the risks of death from coronary heart disease and stroke are continuous and roughly log-linear except at low BMIs.2,3,24 We first estimated the effect of 5 kg/m2 higher baseline BMI on coronary heart disease or stroke with adjustment for confounders. We then added the mediators to the model, separately, in all combinations of two, and all three together. We did not incorporate interaction between BMI and mediators in the continuous analysis. We also analysed categories of overweight (BMI ≥25–<30 kg/m2) and obesity (BMI ≥30 kg/m2) as compared with normal weight (BMI ≥20–<25 kg/m2) with the same methods as continuous analysis. We pooled HRs across cohorts with a random-effects model with inverse variance weights.25 We assessed heterogeneity with Cochran Q test and I2 statistic.26
We estimated the percentage of excess risk mediated (PERM)27 with pooled HRs as:
PERM is not additive across multiple mediators. To calculate the uncertainty of PERM, we randomly drew 5000 pairs of HR(confounder adjusted) and HR(confounder and mediator adjusted) from their corresponding uncertainty distributions while accounting for their correlations; estimated PERM for each pair of HRs and quantified its variability across all 5000 estimates (appendix pp 5–7). We used the median of these 5000 estimates as the point estimate of PERM, and its 2·5th and 97·5th percentiles as the 95% CI.
Subgroup and sensitivity analyses
We tested whether the extent of mediation differed by selected cohort characteristics including event types (fatal vs fatal and non-fatal combined), median age of participants at baseline, baseline study year, region of the study, and follow-up duration. In sensitivity analyses, we examined whether the results depended on how the mediators were measured, with use of total versus LDL cholesterol or glucose versus diabetes as the metric of mediator. In sensitivity analyses, we also estimated PERM for waist circumference and waist-to-hip ratio in 17 cohorts that had measured either of them in addition to BMI. We compared PERM per 10 cm waist circumference and 0·1 waist-to-hip ratio (roughly equivalent to 1 standard deviation increment of these metrics in a pooled sample of 58 prospective cohorts)3 with that for 5 kg/m2 BMI in the same cohorts. For simplicity of presentation, we report results of these secondary analyses only for all three mediators together; results for one or two mediators are available from the authors by request. All statistical analyses were done with Stata 11·0 and R 2·11. All reported p values were two-sided and were deemed significant if less than 0·05.
Role of the funding source
The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The members of the Cohort Collaborating Group had access to the original data, which were re-analysed for this report. The corresponding author had final responsibility for the decision to submit.
Results
We included 97 prospective cohorts in the analysis. These studies collectively enrolled 1·8 million participants between 1948 and 2005. During follow-ups that ranged between 2·7 and 57·5 years (median time across all cohorts was 13·3 years), 57 161 coronary heart disease and 31 093 stroke events were reported (appendix pp 8–14). Western European cohorts (32 cohorts) had the largest number of coronary heart disease and stroke events, contributing 31 289 (55%) of coronary heart disease and 13 591 (44%) of stroke events. Cohorts from east and southeast Asia (33 cohorts) contributed 10 163 (33%) of stroke but only 3763 (7%) of coronary heart disease events, showing the importance of stroke in Asia compared with coronary heart disease (table 2). 72 cohorts measured all three mediators and 21 measured two mediators.
Table 2.
Number of analysed cohorts, participants, and events by region
| Number of cohorts (%) | Number of participants (%) | Number of CHD events (%) | Number of stroke events (%) | |
|---|---|---|---|---|
| East and southeast Asia | 33 (34·0%) | 479 736 (26·7%) | 3763 (6·6%) | 10 163 (32·7%) |
| Western Europe | 32 (33·0%) | 1 055 454 (58·7%) | 31 289 (54·7%) | 13 591 (43·7%) |
| North America | 15 (15·5%) | 157 136 (8·7%) | 16 183 (28·3%) | 5485 (17·7%) |
| Australia or New Zealand | 10 (10·3%) | 84 632 (4·7%) | 3207 (5·6%) | 1067 (3·4%) |
| Latin America, central and eastern Europe, North Africa, and Middle East | 7 (7·2%) | 21 110 (1·2%) | 2719 (4·8%) | 787 (2·5%) |
| Total | 97 (100%) | 1 798 068 (100%) | 57 161 (100%) | 31 093 (100%) |
CHD=coronary heart disease.
After we adjusted for confounders, each 5 kg/m2 higher BMI was associated with a HR of 1·27 (95% CI 1·23–1·31) for coronary heart disease and 1·18 (1·14–1·22) for stroke (figure 1; appendix pp 19–36 shows cohort-specific HRs). Blood pressure was the most important mediator for the effects of BMI on both coronary heart disease and stroke; the HR for coronary heart disease fell to 1·19 (1·16–1·22) and for stroke to 1·06 (1·03–1·09) after we adjusted for blood pressure. The second most important mediator was glucose, adjustment for which lowered HRs to 1·23 (1·19–1·27) for coronary heart disease and 1·13 (1·09–1·18) for stroke. Adjustment for any combinations of two or three mediators further reduced HRs of coronary heart disease and stroke compared with adjustment for one mediator (figure 1). When we adjusted for all three mediators, the HR for coronary heart disease decreased to a significantly lower value of 1·15 (1·12–1·18), and for stroke to 1·04 (1·01–1·08; figure 1).
Figure 1.
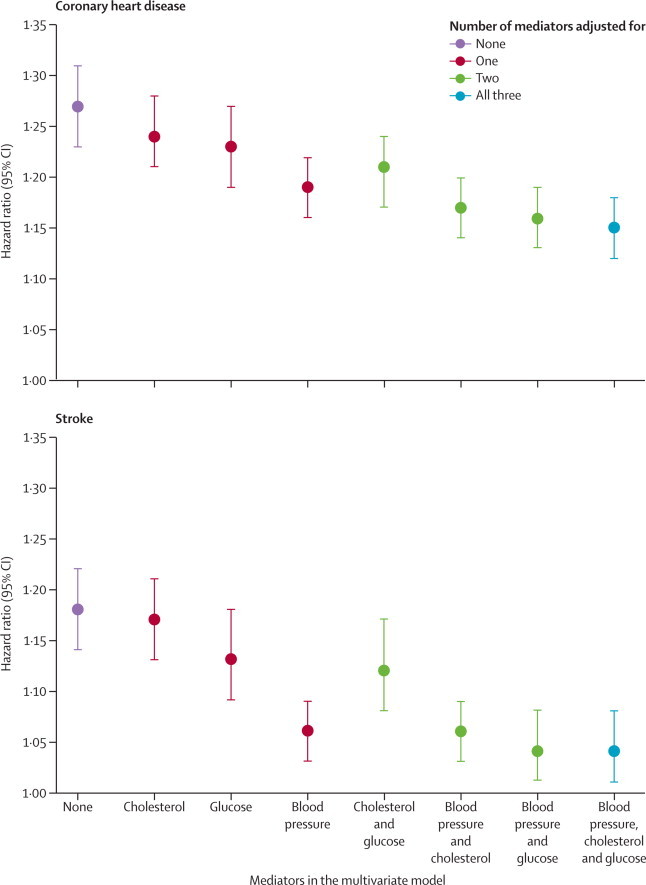
Hazard ratios per 5 kg/m2 higher body-mass index adjusted for different combinations of mediators in coronary heart disease and stroke
All hazard ratios were also adjusted for confounders as described in Methods. The appendix (pp 19–36) shows cohort-specific hazard ratios.
Being overweight, compared with normal weight, was associated with an HR of 1·26 (1·22–1·30) for coronary heart disease and 1·13 (1·08–1·18) for stroke after adjustment for confounders (table 3; appendix pp 37–72 shows cohort-specific HRs). Obesity had a significantly larger association with both coronary heart disease and stroke than did overweight: the confounder-adjusted HR of obesity versus normal weight was 1·69 (1·58–1·81) for coronary heart disease and 1·47 (1·36–1·59) for stroke. We noted associations between both overweight and obesity and the risk of CHD and stroke in both Asian and western cohorts, and in both older (enrolment before 1990) and more recent cohorts (enrolment in or after 1990; appendix pp 15–16).
Table 3.
HRs and excess risk of overweight and obesity mediated through different combinations of metabolic risk factors
|
Overweight |
Obesity |
|||
|---|---|---|---|---|
| HR (95% CI) | Excess risk mediated (%, 95% CI) | HR (95% CI) | Excess risk mediated (%, 95% CI) | |
| Coronary heart disease | ||||
| None | 1·26 (1·22 to 1·30) | .. | 1·69 (1·58 to 1·81) | .. |
| Blood pressure | 1·18 (1·14 to 1·22) | 31% (26 to 36) | 1·48 (1·39 to 1·57) | 31% (27 to 35) |
| Cholesterol | 1·21 (1·18 to 1·25) | 18% (13 to 22) | 1·64 (1·54 to 1·75) | 8% (2 to 12) |
| Blood glucose | 1·23 (1·18 to 1·27) | 12% (6 to 18) | 1·60 (1·49 to 1·72) | 14% (8 to 20) |
| Blood pressure and cholesterol | 1·14 (1·11 to 1·18) | 45% (40 to 52) | 1·44 (1·36 to 1·53) | 36% (33 to 40) |
| Blood pressure and blood glucose | 1·16 (1·12 to 1·20) | 38% (32 to 45) | 1·42 (1·34 to 1·51) | 39% (35 to 44) |
| Cholesterol and blood glucose | 1·19 (1·15 to 1·23) | 27% (22 to 33) | 1·55 (1·46 to 1·64) | 21% (17 to 25) |
| Blood pressure, cholesterol, and blood glucose | 1·13 (1·09 to 1·16) | 50% (44 to 58) | 1·39 (1·32 to 1·47) | 44% (41 to 48) |
| Stroke | ||||
| None | 1·13 (1·08 to 1·18) | .. | 1·47 (1·36 to 1·59) | .. |
| Blood pressure | 1·03 (0·99 to 1·07) | 76% (61 to 104) | 1·21 (1·13 to 1·28) | 56% (50 to 64) |
| Cholesterol | 1·11 (1·06 to 1·16) | 17% (5 to 30) | 1·44 (1·33 to 1·56) | 7% (−1 to 14) |
| Blood glucose | 1·09 (1·04 to 1·15) | 29% (13 to 55) | 1·35 (1·24 to 1·47) | 25% (18 to 34) |
| Blood pressure and cholesterol | 1·04 (0·99 to 1·08) | 74% (54 to 112) | 1·19 (1·12 to 1·27) | 59% (52 to 70) |
| Blood pressure and blood glucose | 1·01 (0·96 to 1·06) | 93% (67 to 147) | 1·15 (1·08 to 1·22) | 68% (62 to 76) |
| Cholesterol and blood glucose | 1·09 (1·04 to 1·15) | 31% (16 to 56) | 1·34 (1·24 to 1·45) | 28% (20 to 36) |
| Blood pressure, cholesterol, and blood glucose | 1·00 (0·96 to 1·05) | 98% (69 to 155) | 1·14 (1·08 to 1·21) | 69% (64 to 77) |
All HRs are relative to normal weight (BMI ≥20–<25 kg/m2), and were adjusted for confounders. HR=hazard ratio. BMI=body-mass index.
Similar to analysis using continuous BMI, blood pressure was the most important mediator for the association of overweight and obesity with both coronary heart disease and stroke (table 3). After adjustment for all three mediators, the HR of overweight versus normal weight for coronary heart disease decreased to 1·13 (1·09–1·16) and its association with stroke became null with an HR of 1·00 (0·96–1·05). The HR of obesity versus normal weight for coronary heart disease decreased to 1·39 (1·32–1·47) and that of stroke to 1·14 (1·08–1·21).
We recorded higher HRs per 5 kg/m2 BMI for both coronary heart disease and stroke in east and southeast Asia than HRs in western cohorts (North America, western Europe, Australia, and New Zealand; figure 2, appendix pp 73–90). Asian cohorts had an HR of 1·40 (1·29–1·52) for coronary heart disease versus 1·24 (1·20–1·28) in western cohorts (p value for comparison of the two HRs=0·01), and 1·29 (1·20–1·38) for stroke versus 1·14 (1·09–1·18) in western cohorts (p=0·002). After we adjusted for all three mediators, the HRs for coronary heart disease were 1·23 (1·12–1·36) in Asian cohorts and 1·13 (1·10–1·16) in western cohorts (p=0·10); the HRs for stroke became almost identical between regions (figure 2). The HRs for both coronary heart disease and stroke were larger in cohorts that enrolled younger participants (median age at baseline <55 years compared with ≥55 years), both before and after adjustment for mediators (figure 2).
Figure 2.
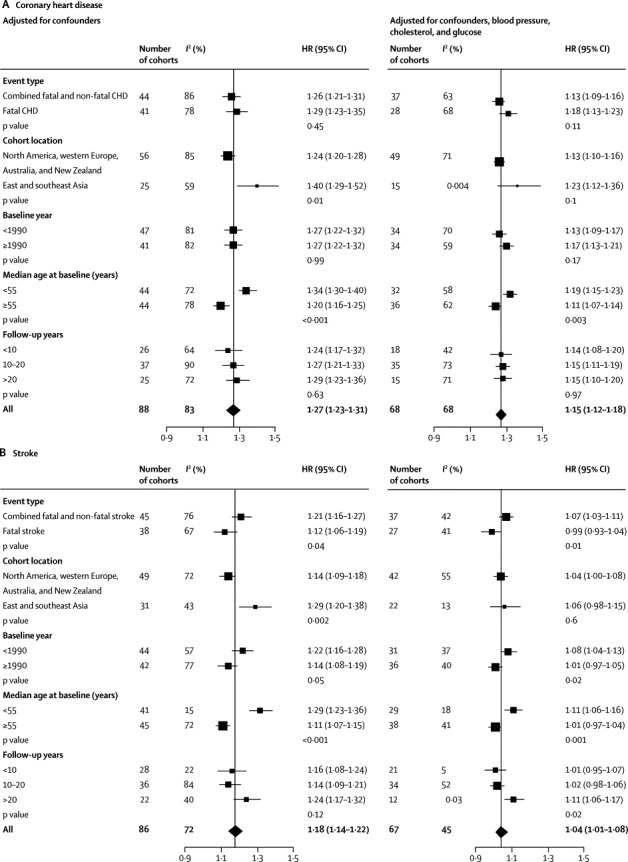
Stratified analyses of HRs per 5 kg/m2 higher body-mass index, with and without adjustment for mediators in CHD (A) and stroke (B)
p values were meta-regression p values between groups. Results are presented for all three mediators combined. The appendix (pp 73–90) shows HRs with adjustment for combinations of one and two mediators. CHD=coronary heart disease. HR=hazard ratio
After we adjusted for blood pressure, the excess risk of coronary heart disease associated with 5 kg/m2 higher BMI decreased by 31% (95% CI 28–35) (figure 3). This figure was three times larger than the proportion mediated by serum cholesterol (10%, 5–15), and more than twice that of glucose (15%, 10–21). Blood pressure alone accounted for a higher percentage of excess risk of BMI than did cholesterol and glucose together (23%, 19–28). The three mediators collectively explained 46% (42–50) of excess risk for coronary heart disease. Blood pressure was a stronger mediator for stroke risk than for coronary heart disease. Adjustment for blood pressure lowered the excess risk of stroke by 65% (56–75). The corresponding percentages were only 24% (15–36) for glucose and 4% (−3 to 12) for cholesterol; we noted this non-significant mediation of stroke risk by cholesterol in both Asian and western cohorts. When we adjusted for all three mediators, the excess risk of stroke was attenuated by 76% (65–91).
Figure 3.
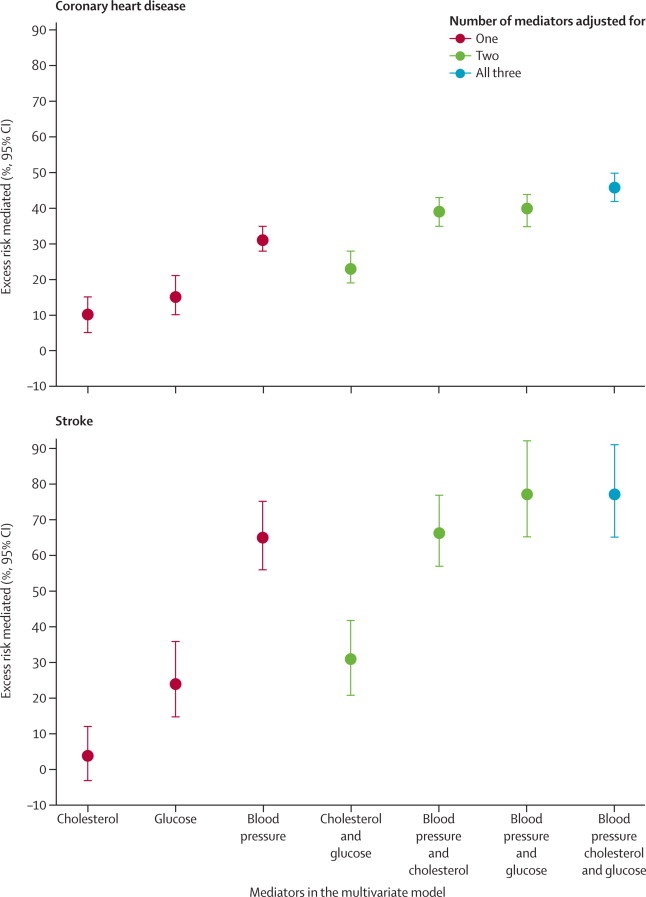
Percentage of excess risk per 5 kg/m2 higher body-mass index mediated through different combinations of metabolic risk factors in coronary heart disease and stroke
The HRs of coronary heart disease decreased by 31% for both overweight and obesity after adjustment for blood pressure (table 3). PERM for the association of overweight with coronary heart disease was larger than that of obesity for most combinations of mediators, but the CIs overlapped (table 3). All three mediators together accounted for 50% (44–58) of the excess risk of overweight on coronary heart disease, and 44% (41–48) of the excess risk of obesity. The metabolic factors also mediated more excess risk of overweight on stroke than of obesity, although the CIs overlapped (table 3). 76% of the excess risk of overweight (61–104) and 56% of that of obesity (50–64) on stroke were mediated through blood pressure alone (table 3). When we adjusted for all three mediators, excess risk of stroke decreased by 98% (69–155) for overweight and by 69% (64–77) for obesity.
In subgroup analyses, PERM for all three mediators combined did not differ significantly by most cohort characteristics (ie, 95% CIs overlapped; table 4). The only significant difference in PERM was for coronary heart disease and baseline year of study, for which a larger percentage of excess risk was mediated by the three mediators in cohorts that had enrolled participants before 1990 versus in 1990 or later. Among individual mediators, blood pressure mediated 69% (57–91) of the excess risk of stroke in Asian cohorts versus 60% (48–78) in western cohorts. The role of blood pressure as a mediator for excess risk of coronary heart disease was similar in Asian and western cohorts (32%, 22–44 vs 30%, 26–34).
Table 4.
Stratified analyses of percentage of excess risk (95% CI) per 5 kg/m2 higher BMI mediated through the combination of blood pressure, cholesterol, and blood glucose
| CHD | Stroke | |
|---|---|---|
| Event type* | ||
| Combined fatal and non-fatal event | 50% (46–55) | 69% (60–81) |
| Fatal event | 39% (31–49) | 115%‡ (78–234‡) |
| Cohort location† | ||
| North America, western Europe, Australia and New Zealand | 44% (40–50) | 73% (57–96) |
| East and southeast Asia | 39% (31–49) | 79% (59–108‡) |
| Baseline year | ||
| <1990 | 53% (46–62) | 62% (51–78) |
| ≥1990 | 38% (34–44) | 93% (74–141‡) |
| Median age at baseline (years) | ||
| <55 | 45% (41–50) | 63% (53–74) |
| ≥55 | 46% (39–56) | 95% (73–149‡) |
| Follow-up years | ||
| <10 | 43% (35–52) | 89% (67–132‡) |
| 10 to 20 | 45% (40–52) | 84% (68–134‡) |
| >20 | 49% (40–59) | 52% (44–62) |
BMI=body-mass index.
Three cohorts reported their results for non-fatal coronary heart disease and non-fatal stroke.
Seven cohorts from other regions reported results for coronary heart disease, and six cohorts from other regions reported results for stroke.
Hazard ratios of BMI were less than 1·0 after adjustment for mediators. Therefore, the numerator of percentage of excess risk mediated was greater than the denominator. This possible overadjustment itself could be due to residual and unmeasured confounding.
In sensitivity analyses, PERMs were 1 to 8 percentage points higher for waist circumference than for BMI in 16 studies that had measured both, but were 4 to 15 percentage points lower for waist-to-hip ratio than for BMI; these differences were not significant (ie, 95% CIs overlapped). LDL cholesterol was a stronger mediator than was total cholesterol, but the difference in PERM was less than 5 percentage points for both coronary heart disease and stroke (results not shown), possibly because of the high correlation between total cholesterol and LDL cholesterol in these cohorts (Pearson correlation coefficient >0·8). PERM for coronary heart disease by all three mediators was only slightly (3 percentage points) and non-significantly higher in cohorts that used measurements for diabetes (25% of cohorts) compared with continuous glucose (results not shown).
Discussion
In this pooled analysis of 97 prospective cohort studies, we estimated that nearly half of excess risk for coronary heart disease and three-quarters of excess risk for stroke due to high BMI were mediated through three metabolic risk factors: blood pressure, cholesterol, and glucose. The most important mediator was blood pressure, especially for stroke, accounting for two-thirds of the excess risk. Compared with having healthy weight, being overweight or obese was associated with an increased risk of coronary heart disease and stroke, with obesity having a larger effect than overweight.
Our results for the overall association between BMI and coronary heart disease or stroke are consistent with those of other large pooled analyses of prospective cohorts.2,3,24 Previous studies mostly analysed all mediators combined, and did not assess the role of other combinations of mediators. A meta-analysis18 of 21 cohorts (including 16 analysed here) reported that 45% of excess risk of coronary heart disease was mediated through blood pressure and total cholesterol, compared with 39% in our analysis (both effects reported for 5 kg/m2 higher BMI). Results of another pooled analysis3 of 58 cohorts (including 15 analysed here) showed that roughly 60% of the excess risk of coronary heart disease and 70% of ischaemic stroke were due to the same three mediators, compared with 46% for coronary heart disease and 76% for stroke in our analysis.
Our lower estimates for coronary heart disease might be the result of a larger number of cohorts that included only fatal coronary heart disease (almost half of our cohorts used only fatal coronary heart disease compared with 9% in the study by Wormser and colleagues3) because PERM tended to be lower when fatal events were analysed (table 4). Our lower estimates for coronary heart disease could also be explained by the use of blood glucose measurements versus diabetes as the metric of mediator. The slightly higher estimates for stroke might be due to the larger number of Asian cohorts in our analysis (34% of our cohorts were from Asia compared with 7% in the study by Wormser and colleagues3), or the stroke subtypes analysed (we used total stroke whereas Wormser and colleagues3 used ischaemic stroke).
Our finding that both overweight and obesity were associated with increased risk of coronary heart disease and stroke differed from reports by Flegal and colleagues,28 who recorded no effects for overweight on either cardiovascular disease mortality in one cohort, or on all-cause mortality in a meta-analysis.29 Flegal and colleagues' findings for cardiovascular disease28 might have differed from ours because of inadequate adjustment for pre-existing diseases and their inadequate control of confounding.30,31 Our results are not directly comparable with those for all-cause mortality.
We noted that metabolic factors mediate a larger proportion of the excess risk for overweight individuals than do those for obese individuals (although the 95% CIs overlapped). This finding suggests that clinical and public health interventions that control blood pressure, cholesterol, and glucose can largely (in coronary heart disease) or fully (in stroke) address the excess risk of coronary heart disease and stroke in overweight individuals. Obese individuals also benefit from interventions on mediators but will continue to have significantly raised risk.
Several pathways link adiposity and excess weight to cardiovascular disease via the mediators analysed in this study. Adiposity can raise blood pressure through increased peripheral vascular resistance and renal salt retention, the latter itself due to higher activity of sympathetic nervous system, leptin concentrations, angiotensin-aldosterone activity, and hyperinsulinaemia.5,32 Adiposity is also associated with dyslipidaemia, and systemic inflammatory state, which could contribute to the development of insulin resistance and diabetes.6 Our results also suggest that the association between adiposity and cardiovascular disease is not completely explained by the three mediators in our analysis. The unexplained risk might be caused by other pathways such as endothelial dysfunction, increase in thrombogenic factors, and the remaining effect of increased sympathetic activity and systemic inflammation not related to risk factors analysed here.6 These other pathways might play a more important part in obese individuals than in overweight individuals. It would be interesting to probe and quantify the role of these other pathways in subsequent studies, including in relation to overweight versus obese status, although fewer cohorts collect comparable data for these other variables compared with the well known metabolic mediators that we analysed.
Panel. Research in context.
Systematic Review
We did a systematic review by searching PubMed and Embase from their inception up to March 23, 2010, using search terms listed in the appendix (pp 2–4). We invited the corresponding authors of eligible cohorts to join the Collaborating Group.
We analysed data from 97 prospective cohort studies to estimate the effects of high body-mass index (BMI) on coronary heart disease and stroke, with and without adjustment for selected metabolic factors (blood pressure, serum cholesterol, and glucose). We pooled hazard ratios (HRs) across cohorts and quantified how much of the excess risk of BMI is mediated through any combination of three metabolic factors.
Interpretation
We found that about half of the excess risk of BMI on coronary heart disease and three-quarters of the excess risk of BMI on stroke was mediated by blood pressure, glucose, and cholesterol collectively. The most important mediator was blood pressure, which mediated a third of the excess risk of BMI on coronary heart disease and two-thirds for stroke. A larger proportion of risk might be mediated for overweight compared with obesity. Interventions that reduce high blood pressure, cholesterol, and glucose might address a substantial proportion of the effect of high BMI on cardiovascular disease. Maintenance of optimum bodyweight is needed to achieve the full benefits.
Our study is the largest pooling analysis of multiple cardiovascular disease risk factors, with 1·8 million participants, and 57 161 coronary heart disease and 31 093 stroke events. This large sample size allowed us to study the extent of mediation, and how it varies by cohort characteristics. The cohorts covered Asian and western populations, and therefore, showed the role of BMI and the mediators of its effects in these diverse populations. The consistent stratified analysis suggested the important role of blood pressure as a mediator in the effect of BMI on stroke in Asian populations, in whom high blood pressure and large stroke burden have made this risk factor the leading cause of disease burden.16,33
Our study has some limitations. First, although we consistently adjusted for age, sex, and smoking as the minimum set of confounders, our results might still be affected by unmeasured and residual confounding. For instance, only a few cohorts were adjusted for diet and physical activity, which are risk factors for coronary heart disease and stroke and are associated with increased BMI. Confounders might have been measured with error, which leads to residual confounding (eg, smoking and socioeconomic status). When we restricted the pooling to cohorts that had adjusted for additional confounders, PERM for the three mediators did not change significantly: it was 6 percentage points higher for coronary heart disease and 1 percentage point lower for stroke than for cohorts with minimum set of confounders, and 95% CIs overlapped. Our analysis did not allow for interactions between BMI and mediators, which might exist.34 The mediators were not measured consistently across cohorts because of variability in laboratory methods or metrics of mediators. Sensitivity analyses showed that our results were robust to the choice of metrics used for mediators. Additionally, we could not analyse stroke subtypes separately because most cohorts had not reported the stroke outcome by subtype. Finally, despite the large number of cohorts included in the analysis, we could not access data from all eligible cohorts, especially some with enrolment decades ago.
Our findings have implications for clinical prevention of cardiovascular disease as well as for public health programmes. As a clinical example, consider a 70-year-old non-smoking man who does not have diabetes, is 174 cm tall and weighs 100 kg (ie, has a BMI of 33 kg/m2), with a systolic blood pressure of 147 mm Hg, total cholesterol of 5·05 mmol/L, and HDL cholesterol of 0·93 mmol/L. This person represents roughly the 80th percentile of age, BMI, and cholesterol of adult men, and 90th percentile of blood pressure among adult men with BMI of 30 kg/m2 or more in the US National Health and Nutrition Examination Survey in 2007–08. According to the Framingham risk score, this man's predicted 10-year risk of coronary heart disease is 25%.35 With the assumption that the results of our observational analysis are indicative of the true benefits of losing excess weight, if this patient lost 15 kg of weight through a hypothetical intervention (ie, 5 kg/m2 lower BMI), his new estimated 10 year coronary heart disease risk would be 19·7% (25% minus [25% divided by 1·27], because the HR for coronary heart disease per 5 kg/m2 BMI is 1·27), which is 5 percentage points lower. Alternatively, if he receives drugs to lower his blood pressure and cholesterol to levels that are expected based on a 15 kg weight loss, his 10 year risk of coronary heart disease would only decrease by 2 percentage points (5% times 39%, because the estimated PERM by blood pressure and cholesterol for coronary heart disease is 39% per 5 kg/m2 higher BMI), as he only receives the benefits of reductions in these two risk factors.
Despite the potentially large benefits of weight loss, interventions have had small long-term success, especially at the population level,7,8 leading to a worldwide rise in overweight and obesity.14 By contrast, effective clinical and lifestyle interventions are available to control blood pressure and serum cholesterol,36–39 with evidence that these risk factors have been successfully reduced, in individual patients and whole populations.16,17,40,41 For example, blood pressure, the most important mediator of the association between BMI and cardiovascular disease, has fallen substantially in high-income countries, central Europe, and parts of Latin America.16 Serum cholesterol has also fallen in western countries, but has increased in east and southeast Asia.17 In the USA, decreases in blood pressure and cholesterol have been even larger in overweight and obese individuals, possibly because of more aggressive management.42 Therefore, control of blood pressure and cholesterol might help to lessen the cardiovascular effects of the global obesity epidemic.
The most important step to leverage this potential is to continue past efforts for the reduction of blood pressure and cholesterol, and to try to replicate these efforts in Asia where blood pressure remains high,16 serum cholesterol has increased,17 and stroke is a common cause of death. Despite this potential, and some past successes, further reduction of blood pressure and cholesterol needs major improvements in both primary care and public health programmes.43 The coverage of blood pressure and lipid-lowering drugs is low in most low-income and middle-income countries, even in patients with cardiovascular disease, and social inequalities in coverage exist.44,45 To increase diagnosis and treatment will need well developed national guidelines that include these activities in the primary care system, with emphasis on improvement of access in disadvantaged social and economic groups.44–46 Interventions related to diet that lower the intake of salt, saturated and trans fats, and processed carbohydrates, and increase the consumption of fruits, vegetables, unsaturated fats, and whole grains, can improve the metabolic risk profile even when total calories remain unchanged,47–50 but access to these interventions needs to be improved worldwide.43,51 Additionally, adiposity increases the risk of diabetes, and prevalence of blood glucose and diabetes has increased worldwide.52 Clinical interventions for glycaemic management are not as effective as those for blood pressure and cholesterol.53 Therefore, reliance on control of the metabolic mediators might be only a partial and temporary response to the obesity epidemic. Rather, creative and bold strategies are needed that can curb and reverse rising adiposity so that the full benefits for cardiovascular disease and diabetes reduction can be achieved.
Correspondence to: Goodarz Danaei, Department of Global Health and Population, Harvard School of Public Health, Boston, MA 02115, USA gdanaei@hsph.harvard.edu
Acknowledgments
Acknowledgments
We thank Zhou Zhou for her help with the systematic reviews and Sanne AE Peters for assistance with the APCSC data. This report was prepared using Atherosclerosis Risk in Communities Study, Cardiovascular Health Study, Framingham Heart Study, Framingham Offspring Study, Honolulu Heart Program, Multi-Ethnic Study of Atherosclerosis, Multiple risk factor intervention trial, Puerto Rico Heart Health Program, Women's Health Initiative: Clinical Trials, Women's Health Initiative: Observational Study research materials obtained from the NHLBI Biological Specimen and Data Repository Information Coordinating Centre. The study was funded by the UK Medical Research Council, National Institute for Health Research Comprehensive Biomedical Research Centre at Imperial College Healthcare NHS Trust, National Institute of Health grant RO1 DK090435, UK Medical Research Council, National Institute for Health Research Comprehensive Biomedical Research Centre at Imperial College Healthcare NHS Trust, Lown Scholars in Residence Program on cardiovascular disease prevention, and Harvard Global Health Institute Doctoral Research Grant. This paper is dedicated to the memory of Gary Whitlock, epidemiologist and scholar.
Contributors
GD and ME developed the study concept and analytical strategy. YL and KH did the systematic review, pooled analysis, and prepared results. YL, KH, and Cohort Collaborating Group analysed cohort data. EBR and MW contributed to the design of the study and interpretation of results. YL, KH, ME, and GD wrote the first draft of the report. All other Collaborating Group members commented on the report draft and have seen and approved of the final text. ME and GD oversaw the research. GD is the study guarantor.
The Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects)
Writing and Pooling Group:
Yuan Lu (Department of Global Health and Population, Harvard School of Public Health, Boston, USA), Kaveh Hajifathalian (Department of Global Health and Population, Harvard School of Public Health, Boston, USA), Majid Ezzati (MRC-PHE Centre for Environment and Health, School of Public Health, Imperial College London, London, UK), Mark Woodward (The George Institute for Global Health, Australia), Eric B Rimm (Channing Division of Network Medicine, Brigham and Women's Hospital, Harvard Medical School, Boston, USA), Goodarz Danaei* (Department of Global Health and Population and Department of Epidemiology, Harvard School of Public Health, Boston, USA).
Cohort Collaborating Group†: †Cohort Collaborating Group members were listed by alphabetical order of last name.
Age 40-programme linked with National Cause of Death Register: Randi Selmer (Norwegian Institute of Public Health, Norway), Bjorn H Strand (Norwegian Institute of Public Health, Norway).
Asia Pacific Cohort Study Collaboration (Data were analysed by the Writing Group on behalf of APCSC for those cohorts that are not separately listed below): Executive Committee: X Fang, D F Gu, R Huxley, Y Imai, H C Kim, T H Lam, W H Pan, A Rodgers, I Suh, H Ueshima, M Woodward Participating Studies and Principal Collaborators: Aito Town Study: H Maegawa, A Okayama, H Ueshima; Akabane Study: N Aoki, M Nakamura; Anzhen 02 Cohort Study: Z S Wu; Beijing Anzhen Cohort Study: Z S Wu, C H Yao; Australian Longitudinal Study of Aging: M Luszcz; Australian National Heart Foundation: T A Welborn; Beijing Aging Study: Z Tang; Beijing Iron and Steel Worker Cohort Study: L S Liu, J X Xie; Blood Donors' Health Study: S Ameratunga, S MacMahon, R Norton, G Whitlock; Busselton Health Study (phase I): M W Knuiman, M L Divitini; Canberra-Queanbeyan Longitudinal Study of the Elderly: H Christensen; Capital Iron and Steel Company Study: X G Wu; Capital Iron and Steel Company Hospital Cohort: X H Yu, J Zhou; Civil Service Workers Study: A Tamakoshi; The CardioVascular Disease risk FACtors Two-township Study: W H Pan; East Beijing Cohort Study: L Q Chen, G L Shan, Z L Wu; Electrical Generating Authority of Thailand Study: P Sritara; Fangshan Cohort Study: X F Duan, D F Gu; Fletcher Challenge Heart and Health Study: R Jackson, S MacMahon, R Norton, G Whitlock; Guangzhou Study: Y H Li; Guangzhou Occupational Cohort Study: C Q Jiang, T H Lam; Hisayama Study (phase I): H Arima, M Iida, Y Kiyohara; Health Risks and Quality of Life in the Hong Kong Elderly: S C Ho, J Woo; Huashan Study: Z Hong, M S Huang, B Zhou; The Kinmen Neurological Disorders Survey: J L Fuh; Konan Health and Nutrition Study: S R Choudhury, Y Kita, H Ueshima; Korean Medical Insurance Corporation Study: S H Jee, I S Kim, I Suh; Melbourne Collaborative Study (MCCS): G G Giles; Miyama Cohort Study: T Hashimoto, K Sakata; Newcastle Study: A Dobson; Ohasama Study: Y Imai, T Ohkubo, A Hozawa; Perth Risk Factors Survey: K Jamrozik, M Hobbs, R Broadhurst; Saitama Cohort Study: K Nakachi; Seven Cities Cohort Study: X H Fang, S C Li, Q D Yang; Shanghai Factory Workers Study: Z M Chen; Shibata Cohort Study: H Tanaka; Shigaraki Town Study: Y Kita, A Nozaki, H Ueshima; Shirakawa Study: H Horibe, Y Matsutani, M Kagaya; Singapore Heart: K Hughes, J Lee; Singapore NHS92: S K Chew, D Heng; Six Chinese Cohorts Study: H Y Zhang, B F Zhou; Tanno - Soubetsu Study: K Shimamoto, S Saitoh; Tianjin Study: Z Z Li, H Y Zhang; Abdominal Aortic Aneurysm Screening Program: K Jamrozik, P Norman; Xi'an Study: Y He, T H Lam; Yunnan Tin Miner Cohort Study: S X Yao.
Atherosclerosis Risk in Communities Study (ARIC): Emily D Parker (HealthPartners Institute for Education and Research, Minneapolis, USA), Mark A Pereira (University of Minnesota, Minneapolis, USA), June Stevens (University of North Carolina at Chapel Hill, USA).
ATTICA Study: Demosthenes B Panagiotakos (Harokopio University of Athens, Greece), Christos Pitsavos (University of Athens, Greece).
Beijing Iron and Steel Worker Cohort Study: John R Attia (School of Medicine and Public Health, University of Newcastle, and Hunter Medical Research Institute, Australia), Catherine A D'Este (School of Medicine and Public Health, University of Newcastle, and Hunter Medical Research Institute, Australia), Xiaofei Zhang (Second Hospital Affiliated Zhejiang University College of Medine, China; Cardiovascular Institute and Fu Wai Hospital, Peking Union Medical College, China).
Belgian Interuniversity Research on Nutrition and Health (BIRNH): Els Clays (Department of Public Health, Ghent University, Ghent, Belgium), Dirk A O De Bacquer (Department of Public Health, Ghent University, Belgium), Koen Van Herck (Department of Public Health, Ghent University, Ghent, Belgium).
Busselton Health Study (BHS): Mark L Divitini (The University of Western Australia, Perth, Australia), Matthew W Knuiman (The University of Western Australia, Perth, Australia).
Canada Nutrition Database: Howard I Morrison (Public Health Agency of Canada, Canada), Feng Wang (Public Health Agency of Canada, Canada).
CardioVascular Disease risk FACtors Two-township Study (CVDFACTS): Shao-Yuan Chuang (Division of Preventive Medicine and Health Services Research, Institute of Population Health Sciences, National Health Research Institutes, Maoli, Taiwan-), Wen-Harn Pan (Institute of Biomedical Sciences, Academia Sinica, Taipei, Taiwan; Division of Preventive Medicine and Health Services Research, Institute of Population Health Sciences, National Health Research Institutes, Maoli, Taiwan), Wen-Ting Yeh (Institute of Biomedical Sciences, Academia Sinica, Taipei, Taiwan).
China Prospective Study (CPS): Zhengming Chen (Clinical Trial Service Unit & Epidemiological Studies Unit (CTSU), University of Oxford, Oxford, UK), Margaret C Smith (Clinical Trial Service Unit & Epidemiological Studies Unit (CTSU), University of Oxford, Oxford, UK), Maigeng Zhou (National Centre for Chronic and Noncommunicable Disease Control and Prevention, Chinese Centre for Disease Control and Prevention, Beijing, China).
Chinese Multi-Provincial Cohort Study (CMCS): Wei Wang (Department of Epidemiology, Capital Medical University Beijing Anzhen Hospital, Beijing Institute of Heart, Lung and Blood Vessel Diseases, Beijing, China), Xiao-ting Zhang (Department of Epidemiology, Capital Medical University Beijing Anzhen Hospital, Beijing Institute of Heart, Lung and Blood Vessel Diseases, Beijing, China), Dong Zhao (Department of Epidemiology, Capital Medical University Beijing Anzhen Hospital, Beijing Institute of Heart, Lung and Blood Vessel Diseases, Beijing, China).
Cohort of Norway (CONOR) (except Tromso and HUNT studies): Randi Selmer (Norwegian Institute of Public Health, Norway), Bjorn H Strand (Norwegian Institute of Public Health, Norway), Stein Emil Vollset (Norwegian Institute of Public Health and University of Bergen, Norway).
Cohort study from Porto Alegre, southern Brazil: Sandra C Fuchs (Postgraduate Studies Program in Cardiology, Universidade Federal do Rio Grande do Sul, School of Medicine, Porto Alegre, Brazil), Flavio D Fuchs (Hospital de Clinicas de Porto Alegre, Division of Cardiology, and the National Institute for Science and Technology for Health Technology Assessment (IATS), Brazil), Leila B Moreira (Postgraduate Studies Program in Cardiology, Universidade Federal do Rio Grande do Sul, School of Medicine, Porto Alegre, Brazil).
Corfu Cohort, Seven Countries Study: Ismene A Dontas (University of Athens, Greece), Cleo A Dontas (Corfu General Hospital, Greece).
Crete Cohort, Seven Countries Study: Anthony G Kafatos (University of Crete, Greece), Joanna Moschandreas (University of Crete, Greece).
Crevalcore, Montegiorgio and Rome Cohort, Seven Countries Study: Mariapaola Lanti (Association for Cardiac Research, Rome, Italy), Alessandro Menotti (Association for Cardiac Research, Rome, Italy).
Dalmatia and Slavonia Cohort, Seven Countries Study: Daan Kromhout (Division of Human Nutrition, Wageningen University, The Netherlands), Alessandro Menotti (Association for Cardiac Research, Rome, Italy).
Danish Diet, Cancer and Health study: Majken K Jensen (Department of Nutrition, Harvard School of Public Health, Boston), Kim Overvad (Section for Epidemiology, Department of Public Health, Aarhus University, Denmark; Department of Cardiology, Aalborg University Hospital, Aalborg, Denmark), Anne Tjonneland (Danish Cancer Society, Copenhagen, Denmark).
Diabetes Cardiovascular Risk-Evaluation: Targets and Essential Data for Commitment of Treatment (DETECT): Jens Klotsche (Institute of Clinical Psychology and Psychotherapy/Centre of Clinical Epidemiology and Longitudinal Studies (CELOS), Technische Universitaet Dresden, Germany), Hans-Ulrich Wittchen (Institute of Clinical Psychology and Psychotherapy/Centre of Clinical Epidemiology and Longitudinal Studies (CELOS), Technische Universitaet Dresden, Germany)
Diabetes Intervention Study: Sabine Fischer (Medical Clinic III, Technical University Dresden, Germany), Markolf Hanefeld (Centre for Clinical Studies, GWT, Technical University Dresden, Germany), Uta Schwanebeck (Coordination Centre for Clinical Trials, University of Technology, Germany).
Dubbo Study of the Elderly: Leon A Simons (University of NSW and St Vincents Hospital, Sydney, Australia), Judith Simons (St Vincents Hospital, Sydney, Australia).
Duesseldorf Obesity Mortality Study (DOMS): Ralf Bender (IQWiG, Cologne, Germany), Silke Matthies (Department of Mathematics and Technology, RheinAhrCampus, Koblenz University of Applied Sciences, Remagen, Germany).
East and West Finland Cohort, Seven Countries Study, Phase I: Aulikki Nissinen (National Institute for Health and Welfare, Department of Chronic Disease Prevention, Finland), Hanna K Tolonen (National Institute for Health and Welfare, Department of Chronic Disease Prevention, Chronic Disease Epidemiology and Prevention Unit), Jaakko Tuomilehto (Centre for Vascular Prevention, Danube-University Krems, Krems, Austria; Diabetes Prevention Unit, National Institute for Health and Welfare, Helsinki, Finland; Instituto de Investigacion Sanitaria del Hospital Universario La Paz (IdiPAZ), Madrid, Spain; King Abdulaziz University, Jeddah, Saudi Arabia).
East and West Finland Cohort, Seven Countries Study, Phase II: Aulikki Nissinen (National Institute for Health and Welfare, Department of Chronic Disease Prevention, Finland), Jaakko Tuomilehto (Centre for Vascular Prevention, Danube-University Krems, Krems, Austria; Diabetes Prevention Unit, National Institute for Health and Welfare, Helsinki, Finland; Instituto de Investigacion Sanitaria del Hospital Universario La Paz (IdiPAZ), Madrid, Spain; King Abdulaziz University, Jeddah, Saudi Arabia).
EURODIAB Prospective Complications Study: Nish Chaturvedi (National Heart and Lung Institute, Imperial College, London, UK), John H Fuller (Epidemiology and Public Health, Royal Free and University College London Medical School, London, UK), Sabita S Soedamah-Muthu (Division of Human Nutrition, Wageningen University, Wageningen, The Netherlands).
European Action on Secondary Prevention through Intervention to Reduce Events (EUROASPIRE): Dirk AO De Bacquer (Department of Public Health, Ghent University, Ghent, Belgium), Kornelia Kotseva (Department of Cardiovascular Medicine, National Heart and Lung Institute, Imperial College London, UK), David A Wood (Department of Cardiovascular Medicine, National Heart and Lung Institute, Imperial College London, UK).
EUROSTROKE: Michiel L Bots (Julius Centre For Health Sciences and Primary care, UMC Utrecht, The Netherlands), Karel G M Moons (Julius Centre For Health Sciences and Primary care, UMC Utrecht, The Netherlands).
Finnish Mobile Clinic Health Examination Survey (FMC): Markku Heliovaara (National Institute for Health and Welfare, Finland), Paul B Knekt (National Institute for Health and Welfare, Finland), Harri Rissanen (National Institute for Health and Welfare, Finland)
General Post Office Study (GPO): Jane E Ferrie (Department of Epidemiology and Public Health, University College London, UK), Martin J Shipley (Department of Epidemiology and Public Health, University College London, UK), George Davey Smith (School of Social and Community Medicine, University of Bristol, UK).
Goteborg BEDA study: Saga Johansson (AstraZeneca R&D, Molndal, Sweden), Georgios Lappas (Department of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden), Annika Rosengren (Department of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden).
Health Risks and Quality of Life in the Hong Kong Elderly: Aprille Sham (The Chinese University of Hong Kong, Hong Kong), Jean Woo (The Chinese University of Hong Kong, Hong Kong), Ruby HY Yu (The Chinese University of Hong Kong, Hong Kong).
Hisayama Study: Jun Hata (Department of Environmental Medicine, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan), Yutaka Kiyohara (Department of Environmental Medicine, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan), Toshiharu Ninomiya (Department of Medicine and Clinical Science, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan).
Jichi Medical School-Ambulatory blood pressure monitoring (JMS-ABPM), wave 1: Satoshi Hoshide (Department of Cardiology, Jichi Medical University School of Medicine, Tochigi, Japan), Kazuomi Kario (Department of Cardiology, Jichi Medical University School of Medicine, Tochigi, Japan).
Kaunas Rotterdam Intervention Study (KRIS): Daiva Rastenyte (Department of Neurology, Medical Academy of Lithuanian University of Health Sciences, Lithuania), Abdonas Tamosiunas (Department of Population studies of Institute of Cardiology, Medical Academy of Lithuanian University of Health Sciences, Lithuania).
LIFE Study: Giovanni de Simone (Department of Translational Medical Sciences, Federico II University, Naples, Italy), Richard B Devereux (Department of Medicine, The New York Presbyterian Hospital, Weill-Cornell Medical College, New York, USA), Eva Gerdts (Department of Clinical Science, University of Bergen, Bergen, Norway).
Long term Intervention with Pravastatin in Ischaemic Disease (LIPID): David M Colquhoun (University of Queensland, Greenslopes and Wesley Private Hospitals, Australia), Anthony C Keech (NHMRC Clinical Trials Centre, University of Sydney, Australia), Adrienne C Kirby (NHMRC Clinical Trials Centre, University of Sydney, Australia).
Management of Elevated Cholesterol in Primary Prevention Group of Adult Japanese (MEGA): Kyoichi Mizuno (Nippon Medical School of Medicine, Tokyo, Japan), Haruo Nakamura (Mitsukoshi Health and Welfare Foundation, Tokyo, Japan), Shinichiro Uchiyama (Tokyo Women's Medical University, Tokyo, Japan).
Melbourne Collaborative Study (MCCS): Julie K Bassett (Cancer Council Victoria, Cancer Epidemiology Centre, Melbourne, Australia), Graham G Giles (Cancer Council Victoria, Cancer Epidemiology Centre, Melbourne, Australia), Allison M Hodge (Cancer Council Victoria, Cancer Epidemiology Centre, Melbourne, Australia).
Multifactor Primary Prevention Study: Georgios Lappas (Department of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden), Annika Rosengren (Department of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden), Lars Wilhelmsen (Department of Medicine, University of Gothenburg, Sweden).
National Heart Foundation Risk Factor Prevalence Study: Satvinder S Dhaliwal (School of Public Health, Curtin University, Western Australia, Australia), Timothy A Welborn (University of Western Australia, Australia)
NIPPON DATA80: Yasuyuki Nakamura (Kyoto Women's University, Kyoto, Japan), Akira Okayama (The First Institute for Health Promotion and Health Care, Japan Anti-Tuberculosis Association, Tokyo, Japan), Hirotsugu Ueshima (Shiga University of Medical Science, Otsu, Shiga, Japan).
NIPPON DATA90: Aya Kadota (Osaka Kyoiku University, Kashiwara, Osaka, Japan), Tomonori Okamura (Keio University, Tokyo, Tokyo, Japan), Hirotsugu Ueshima (Shiga University of Medical Science, Otsu, Shiga, Japan).
Nord-Trondelag Health Study 1 (HUNT 1): Marie S Sandvei (Department of Neuroscience, Norwegian University of Science and Technology, Trondheim, Norway; Nordland Hospital Bodø, Bodø, Norway), Lars J Vatten (Department of Community Medicine and General Practice, Norwegian University of Science and Technology, Trondheim, Norway), Anne Vik (Department of Neuroscience, Norwegian University of Science and Technology and Department of Neurosurgery, Trondheim University Hospital,, Trondheim, Norway).
Nord-Trondelag Health Study 2 (HUNT 2): Bjorn Morkedal (Department of Public Health and General Practice, Norwegian University of Science and Technology, Trondheim, Norway), Pal R Romundstad (Department of Community Medicine and General Practice, Norwegian University of Science and Technology, Trondheim, Norway), Marie S Sandvei (Department of Neuroscience, Norwegian University of Science and Technology, Trondheim, Norway; Nordland Hospital Bodø, Bodø, Norway).
Northern Manhattan Study (NOMAS): Mitchell SV Elkind (Department of Neurology, College of Physicians and Surgeons, and Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, NY, USA), Hannah Gardener (University of Miami Miller School of Medicine, Department of Neurology, Miami, USA), Ralph L Sacco (Departments of Neurology and Public Health Sciences, University of Miami Miller School of Medicine, Miami, USA)
Norwegian Counties Study (NCS): Randi Selmer (Norwegian Institute of Public Health, Norway), Bjorn H Strand (Norwegian Institute of Public Health, Norway).
Prediction of cerebrovascular and cardiovascular events in patients with subclinical carotid atherosclerosis: the role of C-reactive protein: Antonino Mignano (Operative Unit of Cardiology AOUP “Paolo Giaccone” Palermo, Italy), Salvatore Novo (Operative Unit of Cardiology AOUP “Paolo Giaccone” Palermo, Italy), Manfredi Rizzo (Department of Internal Medicine and Clinical Specialties, University of Palermo, Italy).
Prospective Cardiovascular Münster Study (PROCAM): Gerd Assmann (Assmann Foundation for Prevention, Münster, Germany), Helmut Schulte (Assmann Foundation for Prevention, Münster, Germany).
Prospective Study of Women in Gothenburg: Lauren Lissner (Department of Public Health and Community Medicine, University of Gothenburg, Sweden), Ingmar Skoog (Department of Psychiatry and Neurochemistry, University of Gothenburg, Sweden), Valter Sundh (Department of Public Health and Community Medicine, University of Gothenburg, Sweden).
Risk of ischaemic heart disease in Zaragoza (ZACARIS): Alejandro Marin (Centro De Salud Zaragoza Norte Zaragoza, Spain), Maria Jose Medrano (National Centre for Epidemiology, Carlos III Institute of Health (ISCIII), Madrid, Spain).
Rotterdam Study (RS): Albert Hofman (Department of Epidemiology, Erasmus Medical Centre, Rotterdam, The Netherlands), Maris Kuningas (Department of Epidemiology, Erasmus Medical Centre, Rotterdam, The Netherlands), Bruno H Stricker (Department of Epidemiology, Erasmus Medical Centre, Rotterdam, The Netherlands).
Secondary Manifestations of ARTerial Disease (SMART): Yolanda van der Graaf (Julius Centre for Health Sciences and Primary Care, University Medical Centre Utrecht, The Netherlands), Frank LJ Visseren (Vascular Medicine University Medical Centre Utrecht, The Netherlands).
Singapore Cardiovascular Cohort Study: Jeannette JM Lee (Saw Swee Hock School of Public Health, National University of Singapore, Singapore).
Study of Multifactorial Prevention of Ischemic Heart Disease: Daiva Rastenyte (Department of Neurology, Medical Academy of Lithuanian University of Health Sciences, Lithuania), Abdonas Tamosiunas (Department of Population studies of Institute of Cardiology, Medical Academy of Lithuanian University of Health Sciences, Lithuania).
Survey in Europe on Nutrition and the Elderly, a Concerted Action (SENECA): Wanda Bemelmans (National Institute for Public Health and the Environment, Bilthoven, The Netherlands), Lisette C P G M de Groot (Wageningen University, Wageningen, The Netherlands), Ellen L de Hollander (Wageningen University, Wageningen, the Netherlands and National Institute for Public Health and the Environment, Bilthoven, The Netherlands).
Tanushimaru and Ushibuka Cohort, Seven Countries Study: Hisashi Adachi (Department of Community Medicine, Kurume University School of Medicine, Kurume, Japan), Yuji Hirai (Department of Internal Medicine, Division of Cardio-Vascular Medicine, Kurume University School of Medicine, Kurume, Japan).
Tehran Lipid and Glucose Study (TLGS): Fereidoun Azizi (Endocrine Research Centre, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran), Farzad Hadaegh (Prevention of Metabolic Disorders Research Centre, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran), Davood Khalili (Prevention of Metabolic Disorders Research Centre, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran).
Tromso Study: Ellisiv B Mathiesen (Department of Clinical Medicine, University of Tromso, Tromso, Norway), Inger Njolstad (Department of Community Medicine, University of Tromso, Tromso, Norway), Tom Wilsgaard (Department of Community Medicine, University of Tromso, Tromso, Norway).
Turkish Adult Risk Factor Study (TARF): Gunay Can (Department of Public Health, Cerrahpasa Medical Faculty, Istanbul University, Turkey), Altan Onat (Emeritus, Cerrahpasa Medical Faculty, Istanbul University, Turkey).
Uppsala Longitudinal Study of Adult Men (ULSAM): Johan Arnlov (Department of Public Health and Caring Sciences, Uppsala University, Sweden), Johan Sundstrom (Department of Medical Sciences, Uppsala University, Sweden).
US Railroad Cohort, Seven Countries Study: Henry W Blackburn (University of Minnesota School of Public Health, USA), David R Jacobs (University of Minnesota School of Public Health, USA).
Ventimiglia di Sicilia Heart Study: Maurizio R Averna (Department of Biomedicine, Internal Medicine and Medical Specialties, University of Palermo, Italy), Angelo B Cefalu (Department of Biomedicine, Internal Medicine and Medical Specialties, University of Palermo, Italy), Davide Noto (Department of Biomedicine, Internal Medicine and Medical Specialties, University of Palermo, Italy).
Vorarlberg Health Monitoring & Promotion Programme (VHM&PP): Hans Concin (Agency for Preventive and Social Medicine, Bregenz, Austria), Gabriele Nagel (Institute for Epidemiology and medical biometry, University of Ulm, Germany, and Agency for Preventive and Social Medicine, Bregenz, Austria), Hanno Ulmer (Department of Medical Statistics, Informatics and Health Economics, Innsbruck Medical University, Austria).
Western Collaborative Group Study (WCGS): Ruth E Krasnow (Centre for Health Sciences, SRI International, Menlo Park, USA), Gary E Swan (Centre for Health Sciences, SRI International, Menlo Park, USA)
Whitehall II Study: Mika Kivimaki (Department of Epidemiology and Public Health, University College London, UK), Martin J Shipley (Department of Epidemiology and Public Health, University College London, UK).
Whitehall I Study: G David Batty (Department of Epidemiology and Public Health, University College London, UK), Martin J Shipley (Department of Epidemiology and Public Health, University College London, UK).
Zrenjanin, Belgrade and Velika Krsna Cohort, Seven Countries Study: Natasa Milic (School of Medicine, University of Belgrade, Serbia), Miodrag C Ostojic (School of Medicine, University of Belgrade, Serbia), Biljana Parapid (Division of Cardiology, Clinical Centre of Serbia, Belgrade, Serbia).
Zutphen cohort, Seven Countries Study, Phase I: Johanna M Geleijnse (Division of Human Nutrition, Wageningen University, The Netherlands), Daan Kromhout (Division of Human Nutrition, Wageningen University, The Netherlands), Eveline Waterham (Division of Human Nutrition, Wageningen University, The Netherlands).
Zutphen cohort, Seven Countries Study, Phase II: Edith J Feskens (Division of Human Nutrition, Wageningen University, The Netherlands), Daan Kromhout (Division of Human Nutrition, Wageningen University, The Netherlands), Eveline Waterham (Division of Human Nutrition, Wageningen University, The Netherlands).
Conflicts of interest
The members of the Writing and Pooling Group declare that they have no conflicts of interest.
Footnotes
Corresponding author.
Cohort Collaborating Group members were listed by alphabetical order of last name.
Supplementary Material
References
- 1.Lozano R, Naghavi M, Foreman K. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whitlock G, Lewington S, Sherliker P, the Prospective Studies Collaboration Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wormser D, Kaptoge S, Di Angelantonio E, the Emerging Risk Factors Collaboration Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377:1085–1095. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh GM, Danaei G, Farzadfar F, the Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group. Asia-Pacific Cohort Studies Collaboration (APCSC) the Diabetes Epidemiology: Collaborative analysis of Diagnostic criteria in Europe (DECODE) the Emerging Risk Factor Collaboration (ERFC) the Prospective Studies Collaboration (PSC) The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: a pooled analysis. PLoS One. 2013;8:e65174. doi: 10.1371/journal.pone.0065174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poirier P, Giles TD, Bray GA, the American Heart Association. the Obesity Committee of the Council on Nutrition. Physical Activity, and Metabolism Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- 6.Van Gaal LF, Mertens IL, De Block CE. Mechanisms linking obesity with cardiovascular disease. Nature. 2006;444:875–880. doi: 10.1038/nature05487. [DOI] [PubMed] [Google Scholar]
- 7.Franz MJ, VanWormer JJ, Crain AL. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107:1755–1767. doi: 10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 8.Douketis JD, Macie C, Thabane L, Williamson DF. Systematic review of long-term weight loss studies in obese adults: clinical significance and applicability to clinical practice. Int J Obes (Lond) 2005;29:1153–1167. doi: 10.1038/sj.ijo.0802982. [DOI] [PubMed] [Google Scholar]
- 9.Gray LJ, Cooper N, Dunkley A. A systematic review and mixed treatment comparison of pharmacological interventions for the treatment of obesity. Obes Rev. 2012;13:483–498. doi: 10.1111/j.1467-789X.2011.00981.x. [DOI] [PubMed] [Google Scholar]
- 10.Rucker D, Padwal R, Li SK, Curioni C, Lau DC. Long term pharmacotherapy for obesity and overweight: updated meta-analysis. BMJ. 2007;335:1194–1199. doi: 10.1136/bmj.39385.413113.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sjöström L, Narbro K, Sjöström CD, the Swedish Obese Subjects Study Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–752. doi: 10.1056/NEJMoa066254. [DOI] [PubMed] [Google Scholar]
- 12.Buchwald H, Avidor Y, Braunwald E. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–1737. doi: 10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- 13.Anand SS, Yusuf S. Stemming the global tsunami of cardiovascular disease. Lancet. 2011;377:529–532. doi: 10.1016/S0140-6736(10)62346-X. [DOI] [PubMed] [Google Scholar]
- 14.Finucane MM, Stevens GA, Cowan MJ, for the Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Body Mass Index) National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. 2011;377:557–567. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stevens GA, Singh GM, Lu Y, for the Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Body Mass Index) National, regional, and global trends in adult overweight and obesity prevalences. Popul Health Metr. 2012;10:22. doi: 10.1186/1478-7954-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Danaei G, Finucane MM, Lin JK, for the Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Pressure) National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5·4 million participants. Lancet. 2011;377:568–577. doi: 10.1016/S0140-6736(10)62036-3. [DOI] [PubMed] [Google Scholar]
- 17.Farzadfar F, Finucane MM, Danaei G, for the Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Cholesterol) National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3·0 million participants. Lancet. 2011;377:578–586. doi: 10.1016/S0140-6736(10)62038-7. [DOI] [PubMed] [Google Scholar]
- 18.Bogers RP, Bemelmans WJ, Hoogenveen RT, the BMI-CHD Collaboration Investigators Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: a meta-analysis of 21 cohort studies including more than 300 000 persons. Arch Intern Med. 2007;167:1720–1728. doi: 10.1001/archinte.167.16.1720. [DOI] [PubMed] [Google Scholar]
- 19.Wilson PW, Bozeman SR, Burton TM, Hoaglin DC, Ben-Joseph R, Pashos CL. Prediction of first events of coronary heart disease and stroke with consideration of adiposity. Circulation. 2008;118:124–130. doi: 10.1161/CIRCULATIONAHA.108.772962. [DOI] [PubMed] [Google Scholar]
- 20.Jousilahti P, Tuomilehto J, Vartiainen E, Pekkanen J, Puska P. Body weight, cardiovascular risk factors, and coronary mortality. 15-year follow-up of middle-aged men and women in eastern Finland. Circulation. 1996;93:1372–1379. doi: 10.1161/01.cir.93.7.1372. [DOI] [PubMed] [Google Scholar]
- 21.Batty GD, Shipley MJ, Jarrett RJ, Breeze E, Marmot MG, Davey Smith G. Obesity and overweight in relation to disease-specific mortality in men with and without existing coronary heart disease in London: the original Whitehall study. Heart. 2006;92:886–892. doi: 10.1136/hrt.2005.072637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu G, Tuomilehto J, Silventoinen K, Sarti C, Männistö S, Jousilahti P. Body mass index, waist circumference, and waist-hip ratio on the risk of total and type-specific stroke. Arch Intern Med. 2007;167:1420–1427. doi: 10.1001/archinte.167.13.1420. [DOI] [PubMed] [Google Scholar]
- 23.Kurth T, Gaziano JM, Rexrode KM. Prospective study of body mass index and risk of stroke in apparently healthy women. Circulation. 2005;111:1992–1998. doi: 10.1161/01.CIR.0000161822.83163.B6. [DOI] [PubMed] [Google Scholar]
- 24.Ni Mhurchu C, Rodgers A, Pan WH, Gu DF, Woodward M, the Asia Pacific Cohort Studies Collaboration Body mass index and cardiovascular disease in the Asia-Pacific Region: an overview of 33 cohorts involving 310 000 participants. Int J Epidemiol. 2004;33:751–758. doi: 10.1093/ije/dyh163. [DOI] [PubMed] [Google Scholar]
- 25.Brockwell SE, Gordon IR. A comparison of statistical methods for meta-analysis. Stat Med. 2001;20:825–840. doi: 10.1002/sim.650. [DOI] [PubMed] [Google Scholar]
- 26.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin DY, Fleming TR, De Gruttola V. Estimating the proportion of treatment effect explained by a surrogate marker. Stat Med. 1997;16:1515–1527. doi: 10.1002/(sici)1097-0258(19970715)16:13<1515::aid-sim572>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 28.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298:2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 29.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Willett WC, Hu FB, Colditz GA, Manson JE. Underweight, overweight, obesity, and excess deaths. JAMA. 2005;294:551. doi: 10.1001/jama.294.5.551-a. author reply 552–53. [DOI] [PubMed] [Google Scholar]
- 31.Willett WC, Hu FB, Thun M. Overweight, obesity, and all-cause mortality. JAMA. 2013;309:1681. doi: 10.1001/jama.2013.3075. [DOI] [PubMed] [Google Scholar]
- 32.Corden B, Keenan NG, de Marvao AS. Body fat is associated with reduced aortic stiffness until middle age. Hypertension. 2013;61:1322–1327. doi: 10.1161/HYPERTENSIONAHA.113.01177. [DOI] [PubMed] [Google Scholar]
- 33.Lim SS, Vos T, Flaxman AD. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mora S, Yanek LR, Moy TF, Fallin MD, Becker LC, Becker DM. Interaction of body mass index and framingham risk score in predicting incident coronary disease in families. Circulation. 2005;111:1871–1876. doi: 10.1161/01.CIR.0000161956.75255.7B. [DOI] [PubMed] [Google Scholar]
- 35.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 36.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. doi: 10.1136/bmj.b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baigent C, Blackwell L, Emberson J, the Cholesterol Treatment Trialists' (CTT) Collaboration Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170 000 participants in 26 randomised trials. Lancet. 2010;376:1670–1681. doi: 10.1016/S0140-6736(10)61350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sacks FM, Campos H. Dietary therapy in hypertension. N Engl J Med. 2010;362:2102–2112. doi: 10.1056/NEJMct0911013. [DOI] [PubMed] [Google Scholar]
- 39.Sacks FM, Svetkey LP, Vollmer WM, the DASH-Sodium Collaborative Research Group Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 40.Carroll K, Majeed A, Firth C, Gray J. Prevalence and management of coronary heart disease in primary care: population-based cross-sectional study using a disease register. J Public Health Med. 2003;25:29–35. doi: 10.1093/pubmed/fdg007. [DOI] [PubMed] [Google Scholar]
- 41.Laverty AA, Bottle A, Majeed A, Millett C. Blood pressure monitoring and control by cardiovascular disease status in UK primary care: 10 year retrospective cohort study 1998–2007. J Public Health (Oxf) 2011;33:302–309. doi: 10.1093/pubmed/fdq078. [DOI] [PubMed] [Google Scholar]
- 42.Gregg EW, Cheng YJ, Cadwell BL. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005;293:1868–1874. doi: 10.1001/jama.293.15.1868. [DOI] [PubMed] [Google Scholar]
- 43.Ezzati M, Riboli E. Can noncommunicable diseases be prevented? Lessons from studies of populations and individuals. Science. 2012;337:1482–1487. doi: 10.1126/science.1227001. [DOI] [PubMed] [Google Scholar]
- 44.Di Cesare M, Khang YH, Asaria P, the Lancet NCD Action Group Inequalities in non-communicable diseases and effective responses. Lancet. 2013;381:585–597. doi: 10.1016/S0140-6736(12)61851-0. [DOI] [PubMed] [Google Scholar]
- 45.Yusuf S, Islam S, Chow CK, the Prospective Urban Rural Epidemiology (PURE) Study Investigators Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet. 2011;378:1231–1243. doi: 10.1016/S0140-6736(11)61215-4. [DOI] [PubMed] [Google Scholar]
- 46.Farzadfar F, Murray CJ, Gakidou E. Effectiveness of diabetes and hypertension management by rural primary health-care workers (Behvarz workers) in Iran: a nationally representative observational study. Lancet. 2012;379:47–54. doi: 10.1016/S0140-6736(11)61349-4. [DOI] [PubMed] [Google Scholar]
- 47.Pietinen P, Vartiainen E, Seppänen R, Aro A, Puska P. Changes in diet in Finland from 1972 to 1992: impact on coronary heart disease risk. Prev Med. 1996;25:243–250. doi: 10.1006/pmed.1996.0053. [DOI] [PubMed] [Google Scholar]
- 48.Jackson R, Beaglehole R. Trends in dietary fat and cigarette smoking and the decline in coronary heart disease in New Zealand. Int J Epidemiol. 1987;16:377–382. doi: 10.1093/ije/16.3.377. [DOI] [PubMed] [Google Scholar]
- 49.He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009;23:363–384. doi: 10.1038/jhh.2008.144. [DOI] [PubMed] [Google Scholar]
- 50.Ikeda N, Gakidou E, Hasegawa T, Murray CJ. Understanding the decline of mean systolic blood pressure in Japan: an analysis of pooled data from the National Nutrition Survey, 1986–2002. Bull World Health Organ. 2008;86:978–988. doi: 10.2471/BLT.07.050195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mozaffarian D, Afshin A, Benowitz NL, for the American Heart Association Council on Epidemiology and Prevention. Council on Nutrition. Physical Activity and Metabolism. Council on Clinical Cardiology. Council on Cardiovascular Disease in the Young. Council on the Kidney in Cardiovascular Disease. Council on Peripheral Vascular Disease. the Advocacy Coordinating Committee Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126:1514–1563. doi: 10.1161/CIR.0b013e318260a20b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Danaei G, Finucane MM, Lu Y, for the Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose) National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 53.Boussageon R, Bejan-Angoulvant T, Saadatian-Elahi M. Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ. 2011;343:d4169. doi: 10.1136/bmj.d4169. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


