Abstract
Background
Older patients in particular are vulnerable to memory disturbances and other types of cognitive impairment after surgical operations. In one study, roughly 12% of patients over age 60 had postoperative cognitive dysfunction (POCD) three months after surgery. This is an important issue in perioperative care as extensive surgery on older patients becomes more common.
Methods
Selective review of the literature.
Results
POCD is usually transient. It is diagnosed by comparing pre- and postoperative findings on psychometric tests. Its pathogenesis is multifactorial, with the immune response to surgery probably acting as a trigger. Factors that elevate the risk of POCD include old age, pre-existing cerebral, cardiac, and vascular disease, alcohol abuse, low educational level, and intra- and postoperative complications. The findings of multiple randomized controlled trials indicate that the method of anesthesia does not play a causal role for prolonged cognitive impairment. POCD is associated with poorer recovery and increased utilization of social financial assistance. It is also associated with higher mortality (hazard ratio 1.63, 95% confidence interval 1.11–2.38). Persistent POCD enters into the differential diagnosis of dementia.
Conclusion
POCD can markedly impair postoperative recovery. The findings of pertinent studies performed to date are difficult to generalize because of heterogeneous patient groups and different measuring techniques and study designs. Further investigation is needed to determine which test instruments are best for clinical use and which preventive strategies might lessen the incidence of POCD.
Cognitive impairment after anesthesia and surgery (postoperative cognitive dysfunction, [POCD]) is a recognized clinical phenomenon. As early as 1955, it was described by Bedford in the Lancet under the designation “adverse cerebral effects of anaesthesia on old people” (1).
POCD is a transient disturbance that can affect patients of any age but is more common in older people. Its relevance in the immediate postoperative phase was made clear in a recent article by Chung and Assmann, in which two different cases were described of young patients who caused serious traffic accidents shortly after undergoing ambulatory surgery (2). According to a recent study, about 40% of all persons over age 60 who are hospitalized for surgery have POCD on discharge, and about 10% have POCD three months later.
The aging of the population and new developments in medicine both imply that the number of older patients undergoing extensive surgery will keep rising. All persons caring for patients intra- and postoperatively should know about the risk of POCD after anesthesia and surgery. The aim of this review article is to present the current understanding of POCD in order to foster interdisciplinary dialogue.
Methods
This article is a selective review of pertinent literature retrieved by a search in the Medline, PubMed, and Cochrane Library databases, using the following key words: “cognitive (dys)function AND an(a)esthesia”; “cognitive (dys)function AND surgery”; “postoperative cognitive (dys)function”; “measurement AND cognitive function”; “an(a)esthesia AND dementia (postoperative).” The search yielded several thousand publications. The ones cited here are those that, in the author’s view, make a substantial contribution to the interdisciplinary management of POCD.
Definition and differential diagnosis
Postoperative cognitive dysfunction is defined as a new cognitive impairment arising after a surgical procedure. Its diagnosis requires both pre- and postoperative psychometric testing. Its manifestations are subtle and manifold, depending on the particular cognitive domains that are affected. The most commonly seen problems are memory impairment and impaired performance on intellectual tasks. Common differential diagnoses are listed in Table 1 (3, 4).
Table 1. The differential diagnosis of postoperative neurological disturbances with impaired cognitive performance.
| Manifestations | Diagnostic methods | Timing | Prognosis | |
|---|---|---|---|---|
| Postoperative cognitive dysfunction (POCD) | new cognitive deficits that appear postoperatively (impairment of: memory, ability to combine tasks, psychomotor dexterity, etc.) | pre- and postoperative psychometric testing | arises immediately after surgery, may last up to 6 months | reversible in days to months |
| Delirium | cognitive deficits, hallucinations, fluctuating state of consciousness, and other manifestations | various delirium scales, e.g., Nu-DESC, Cam-ICU | days to weeks, depending on cause (e.g., withdrawal phenomenon, complicating infection) | reversible if the underlying condition is treatable |
| Central anticholinergic syndrome | agitated type or somnolent/comatose type | reversal of manifestations on administration of physostigmine | arises immediatelyafter surgery | reversible with medication |
| Dementia | impaired memory, impairment of abstract thinking and judgment, central impairment of tool manipulation (aphasia, apraxia, agnosia, and/or executive dysfunction), personality changes | various dementia tests, e.g., Mini-Mental Status Examination, Short Syndrome Test, Dementia Detection Test | develops progressively over months to years | poor prognosis, no cure available |
| Akinetic crisis | worsening of parkinsonismwith marked akinesia and inability to verbalize | history: interruption of anti-parkinsonian medications around the time of surgery | immediately after surgery or within hours | reversible with antiparkinsonian medication |
Incidence and importance
The reported incidence figures for postoperative cognitive dysfunction vary depending on the group of patients studied, the definition of POCD used, the tests used to establish the diagnosis and their statistical evaluation, the timing of testing, and the choice of control group (5– 7). Krenk et al. point out in their review that POCD can arise at any age, but tends to last longer and to affect everyday life and the return to work more severely in patients over age 60 (8). Monk et al. documented the presence of POCD on discharge from the hospital (9) in:
36.6% of surgical patients aged 18–39,
30.4% of those aged 40–59, and
41.4% of those aged 60 and up.
These were patients who had undergone major surgery other than cardiac surgery. Three months later, 12.7% of the patients over age 60 still had POCD. According to descriptive studies, the likelihood of POCD is higher in special patient groups, e.g., those with coronary atherosclerosis or pre-existing subclinical dementia (10– 12).
Controlled longitudinal studies have shown that POCD is transient (13). Selnes et al. showed that patients with coronary heart disease have similar cognitive deficits regardless of whether they underwent heart surgery on or off pump, or were treated conservatively (11). All three patient groups had significant cognitive impairment over six years of follow-up compared to a healthy control group.
The patients’ own subjective assessment, as documented, for example, with the Critical Failure Questionnaire, only partially reflects the cognitive deficits that are revealed by psychometric testing (14, 15). The case report of Chung and Assmann clearly shows that patients’ misperceptions in the immediate postoperative period can have very serious consequences (2). The critical question must, therefore, be asked whether the test instruments customarily used are themselves adequate to detect relevant changes in cognitive function.
In a longitudinal study with 8.5 years of follow-up performed in the aftermath of the ISPOCD study, Steinmetz et al. found POCD to be associated with higher mortality (Cox proportional hazard ratio 1.63, 95% confidence interval 1.11–2.38; p = 0.01), earlier retirement, and greater utilization of social financial assistance (16). Monk et al. found that the risk of death within one year was greater among patients who had POCD when they were discharged from the hospital (9).
Measuring instruments
The diagnosis of POCD is verified by psychometric testing performed pre- and postoperatively to assess cognitive performance. The following were named as core tests in a consensus recommendation on POCD issued in 1995 (Figures 1 and 2) (17):
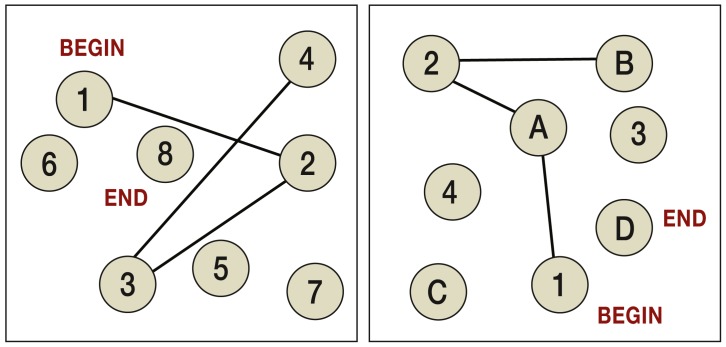
Figure 1.
Left: the Trail Making Test, Part A—connect the numbers, in ascending order, with a line.
Right: the Trail Making Test, Part B—connect the numbers in ascending order and the letters in alphabetical order with a line. The time needed to do each part is measured in seconds. This is a test of dexterity and of the ability to combine tasks.
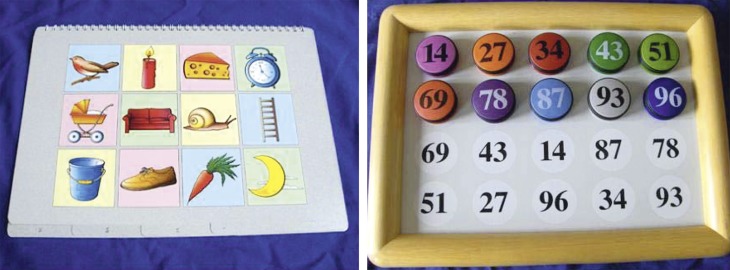
Figure 2.
Left: the Digit Span Test measures how many digits presented in sequence the subject can remember (short-term memory).
Right: in the Stroop Test, the printed words must be read out loud and the color they are printed in must be named. If the word is a color word that is printed in a different color, the reaction time and error rate are higer. This is a test of attention and concentration in the presence of distractors.
the Rey Auditory Verbal Learning Test (a word learning test),
the Trail Making Test, Parts A and B (ability to perform combined tasks),
the Grooved Pegboard Test (manual dexterity),
and the Digit Span Test (ability to remember a sequence of numbers).
Longitudinal studies of POCD additionally employed the Stroop Test (Figure 2), the Paper and Pencil Memory Test (a test of sensorimotor speed and of the speed of recall), the Letter–Number Replacement Test (a test of the speed of general information processing), and the Four-Field Test (a test of psychomotor reaction time) (14).
A comprehensive clinical neuropsychological examination takes about two and a half hours. Erzigkeit’s Short Cognitive Performance Test (SKT) is a shorter alternative consisting of nine subtests (Figure 3) (18). The entire test can be administered in about 15 minutes and is thus suitable for perioperative use (19). Chung et al. tested cognitive performance after general anesthesia with a driving simulator (20).
Figure 3.
Erzigkeit’s Short Cognitive Performance Test (18)
Pictures for Subtests 1 and 2 (left): the pictures shown are to be named (time measured in seconds). After a brief pause, it is then determined how many of these pictures the subject can remember (short-term memory). Board for Subtests 3, 4, and 5 (right): the numbers are to be read out loud, sorted in ascending order, and then re-sorted in the area below. The time needed for this is measured. The purpose of the subtests is to assess information processing and motor skills.
The Mini-Mental Status Examination (MMSE) is intended as a screening test for dementia. It contains questions relating to temporal and spatial orientation, tasks relating to retentiveness, recollection, attention and correctness, and an assessment of language and the ability to write and draw. It takes about five minutes to administer. The MMSE is sometimes used to quantify POCD, but it is not suitable for this purpose because of a marked learning effect (21).
The Cognitive Failure Questionnaire (CFQ) is a patient questionnaire for self-assessment (22). It employs 25 different items to assess the frequency of cognitive errors in everyday life (relating to conceptualization, memory, and motor performance) on a verbal scale.
The MMSE can be used in routine clinical practice to identify preoperative subclinical dementia that would put patients at higher than usual risk for developing POCD. It would seem appropriate that, for patients with a pathological MMSE score, the consensus recommendations should be followed; this is, however, not generally done at present (17, 23).
At the same time, there should be an assessment of anxiety and depression, which also affect cognitive performance. The CFQ is a suitable means of documenting the subjective symptoms of patients who are at risk.
Pathogenesis and risk factors
The mechanisms leading to cognitive impairment after anesthesia and surgery are not yet fully clear. The findings of animal experiments suggest an important role for the immune response to surgery. Terrando et al. showed that a peripheral surgical procedure in mice activates the inflammatory TNFα/NF-?B signal cascades, leading to the release of cytokines that impair the integrity of the blood–brain barrier (24). In turn, macrophages can migrate more easily into the hippocampus, with ensuing memory impairment. Cognitive function remains unimpaired if this mechanism is blocked by the activation of anti-inflammatory cholinergic signal cascades to prevent pro-inflammatory cytokine secretion.
Clinical observational studies have revealed that POCD arises more frequently after extensive surgery under general anesthesia, after secondary surgery, and when there are postoperative complications; these findings are consistent with the hypothesis of an inflammatory component of pathogenesis (14). The effect of anesthesia per se on cognitive function depends on the pharmacodynamics and -kinetics of the particular agents used. As a rule, the shorter the duration of action of the anesthetic agent, the shorter the duration of cognitive impairment in the immediate postoperative period. No definitive evidence has been found to date for the hypothesis that anesthesia itself causes prolonged POCD. The putative neurotoxicity of anesthetic drugs in children has been studied in order to determine whether anesthesia in childhood might lead to behavioral abnormalities, learning disorders, and cognitive impairment in later years. The meaning of the findings that have been obtained is currently debated; in any case, twin studies have failed to yield any definitive evidence that anesthetic drugs are neurotoxic (25). Nor has it been shown that POCD arises any less commonly, or with lesser severity, after regional than after general anesthesia.
Age is a major risk factor for POCD (Table 2). Cognitive performance and the ability to compensate for deficits, if present, decline with advancing age. Imaging studies have shown that patients undergoing surgery often have undetected pre-existing brain disease. Ito et al. showed that patients with silent brain ischemia, as detected by MRI, were more likely to have POCD after cardiac bypass surgery (15.2%, versus 4.9% in the control group) (26). The corresponding figure for patients with a prior, clinically manifest cerebral infarction was 18.2%. In a recent review, Julie Ng pointed out the synergistic interaction of inflammatory changes in brain ischemia and surgery (27).
Table 2. Risk factors for postoperative cognitive dysfunction (POCD).
| Risk factors | |
|---|---|
| Patient | advanced age; pre-existing cerebral, cardiac, or vascular disease; preoperative mild cognitive impairment (MCI); low educational level; history of alcohol abuse |
| Operation | extensive surgical procedure, intra- or postoperative complications, secondary surgery |
| Anesthesia | long-acting anesthetic, marked disturbance of homeostasis, organ ischemia due to hypoxia and hypoperfusion, intra- or postoperative anesthesiological complications |
Kline et al. studied POCD in the context of a longitudinal study on the development and course of Alzheimer’s disease (12). They asked whether surgery influences the course of dementia. MRI scans revealed that, 5–9 months after surgery, the volume of the cerebral gray matter was lower, atrophic changes were present in the hippocampus, and the lateral ventricles were larger. Postoperative cognitive function was especially impaired in patients who had already had a mild, subclinical cognitive impairment before surgery. The difference between patients who had and had not undergone surgery disappeared over time as dementia progressed in both groups.
Alcohol abuse and an anxious, depressed basal mood have been identified as further risk factors for POCD. In a randomized trial, Hudetz et al. showed that patients with a history of alcohol abuse had worse cognitive impairment after surgery than patients with no such history, even if they stopped drinking for five weeks preoperatively; these patients also had worse cognitive impairment than patients who did not undergo surgery, whether or not they had a history of alcohol abuse (28). A low educational level is a further risk factor for POCD (14, 29). It is presumed that there are genetic predisposing factors as well (7).
Strategies for prevention and treatment
Indications for surgery
The decision whether to perform an extensive surgical procedure on an elderly, comorbid patient should be based on a critical evaluation of the potential benefit of the operation weighed against its potential harm, including cognitive impairment (even if transient). A neurological examination should be performed; in individual cases, preoperative cognitive testing may be helpful and indicated.
Operative techniques
POCD is more common and more severe after extensive surgery (Table 3). Particular importance is attached to avoiding intra- and postoperative complications. There has been no systematic study of a putative reduction in the incidence and severity of POCD through the use of minimally invasive surgical methods. These methods might be less likely to cause POCD because they involve less tissue trauma and, therefore, elicit a less marked postoperative inflammatory response (9, 30).
Table 3. Overview of randomized controlled trials of postoperative cognitive dysfunction: general anesthesia with xenon.
| Authors | Xenon versus | Patients(number / age) | Time of testing | Number of psychometric tests | Statistical significance of difference between groups |
|---|---|---|---|---|---|
| Rasmussen et al. (32) | Propofol | 39, aged >60 | 3 days –14 weeks | 4 | not significant |
| Coburn et al. (33) | Desflurane | 38, aged 65–75 | 6–72 hours | 4 | not significant |
| Hoecker et al. (34) | Propofol | 101, aged 65–83 | 30 days | 12 | not significant |
| Cremer et al. (35) | Sevoflurane | 40, aged 65–75 | 6–72 hours | 5 | not significant |
Anesthesiological techniques
As a rule, the shorter the duration of action of the anesthetic agent, the shorter the duration of cognitive impairment in the immediate postoperative period. Patients are now often premedicated with a sedative that impairs memory, e.g., midazolam; this practice should be critically reassessed. In a clinical study, the author found measurable memory impairment one day after surgery in patients who had been premedicated with midazolam and had then undergone 1–2 hours of general anesthesia with propofol and remifentanil (19). Cognitive impairment is clearly incompatible with the modern fast-track concepts of perioperative management that are supposed to enable the patient to cooperate actively in the early postoperative period. The incidence of POCD has not been shown to be any less after regional than after general anesthesia (31).
Patients wake up very quickly after general anesthesia with the noble gas xenon. Many animal experiments have shown that xenon has neuroprotective effects in cerebral ischemia. On the other hand, randomized controlled trials have not revealed any difference in the incidence of POCD in patients anesthetized with xenon compared to those anesthetized with propofol, desflurane, or sevoflurane (32– 35) (Table 4). Xenon cannot be used as a single anesthetic agent in humans; this might explain why the encouraging experimental findings have not been reflected in clinical trials. It is not yet clear whether patients at increased risk of POCD, e.g., very old patients with pre-existing brain disease who are going to have extensive surgery, would benefit from xenon-based general anesthesia rather than from an alternative technique.
Table 4. Potential perioperative strategies for the prevention and treatment of POCD.
| Person | Strategies |
|---|---|
| Patient | perioperative cognitive training (?); perioperative geriatric consultation for high-risk patients, e.g., very old patients (?) |
| Surgeon | meticulous surgical technique to prevent complications; minimally invasive technique (?) |
| Anesthesiologist | cautious use of premedicating drugs (sedatives) in elderly patients, short-acting anesthetics during surgery, meticulous anesthetic technique to prevent perioperative disturbances of homeostasis and organ ischemia, tight volumetric balance, EEG monitoring (?) |
Cardiovascular, respiratory, hepatic, and renal insufficiency are all associated with impaired brain performance. Dedicated studies on POCD are currently lacking. It is theoretically obvious that an adequate intraoperative oxygen supply for all vital organs is essential if postoperative cerebral dysfunction is to be avoided.
The same is true of tight intraoperative management of homeostasis to keep the patient in fluid, electrolyte, and glycemic balance. Cognitive impairment is a leading manifestation of disturbed homeostasis. Longitudinal studies have clearly shown that inadequate glycemic control impairs cognitive function (36). In an observational study on patients undergoing coronary surgery, Puskas et al. found that intraoperative hyperglycemia above 200 mg/dL in non-diabetic patients was associated with a significant degree of cognitive impairment six weeks after surgery (37).
There have been clinical studies on the question whether the use in intraoperative electroencephalography (EEG) to control the depth of anesthesia has any effect on POCD. The author carried out a randomized trial that revealed only a short-lasting benefit in the first hour after surgery performed under propofol-remifentanil anesthesia (38). Farag et al. found that information processing was more rapid six weeks after surgery if a deeper level of anesthesia was aimed at intraoperatively, as measured by BIS (bispectral index), a processed EEG index (39). A randomized controlled trial from China showed that POCD and delirium were less common if the BIS indicated a more superficial level of anesthesia (40). The incidence of delirium was between 16% and 24% after a mean anesthesia time of two hours. This report did not contain any information about how many patients received what kind of anesthetic agent, or about the types of surgery performed. It is thus unclear whether anesthesia control with EEG monitoring truly affected the results, or whether other factors were at work. In summary, the available study findings on this issue are inconsistent, and a conclusive assessment is not yet possible.
Overview and future prospects
POCD is a well-recognized clinical phenomenon of multifactorial origin. Advanced age, accompanying cerebrovascular disease, and extensive surgery all increase the risk of POCD. Meticulous surgical and anesthesiological technique are important for preventing complications and keeping the risk of POCD to a minimum. The pertinent studies to date have shown that POCD is generally transient. It is associated with diminished quality of life and increased mortality after surgery.
No measuring instruments for cognitive performance have yet become established as part of routine clinical practice, because such instruments are time- and labor-intensive. A further problem is that POCD is variously defined in the studies that have addressed it. Heterogeneous patient groups, different testing methods, and different study designs make it difficult to generalize from the study findings that are available. Randomized controlled trials on adequately sized groups of patients, employing standardized test instruments, are needed so that we can reliably determine the effect of different surgical techniques, the clinical relevance of psychometric data, and the potential utility of preventive strategies for POCD. It would be desirable for psychometric test batteries to be developed that could be implemented in routine clinical practice. Further research could also determine the extent to which cognitive training might promote cognitive performance, particularly in elderly patients, and thereby enable patients to enjoy a more rapid recovery and a better quality of life after anesthesia and surgery.
Key Messages.
POCD is defined as an impairment of cognitive function arising after a surgical procedure. The diagnosis can only be made if the patient’s preoperative cognitive functional status is known.
Advanced age, pre-existing cerebral, cardiac, and vascular disease, low educational level, and extensive surgery elevate the risk of POCD.
POCD is a transient postoperative disturbance associated with poorer recovery after surgery.
Its pathogenesis is multifactorial, with the immune response to surgery probably serving as a trigger.
Meticulous care by the anesthesia and surgical teams to prevent intra- and postoperative complications can reduce the risk of POCD.
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
Dr. Rundshagen has received payment for preparing continuing medical education presentations from Abbott GmbH & Co. KG (now AbbVie Deutschland GmbH & Co. KG).
References
- 1.Bedford PD. Adverse cerebral effects of anaesthesia on old people. Lancet. 1955:259–263. doi: 10.1016/s0140-6736(55)92689-1. [DOI] [PubMed] [Google Scholar]
- 2.Chung F, Assmann N. Car accidents after ambulatory surgery in patients without an escort. Anesth Analg. 2008;106:817–820. doi: 10.1213/ane.0b013e3181609531. [DOI] [PubMed] [Google Scholar]
- 3.Guenther U, Radtke FM. Delirium in the postanaesthesia period. Cur Opin Anesthesiol. 2010;24:670–674. doi: 10.1097/ACO.0b013e32834c7b44. [DOI] [PubMed] [Google Scholar]
- 4.Haase U, Rundshagen I. Pharmacotherapy-physostigmine administered post-operatively. Anästhesiologie Intensivmedizin Notfallmedizin Schmerztherapie. 2007;42:188–189. doi: 10.1055/s-2007-974580. [DOI] [PubMed] [Google Scholar]
- 5.Newman S, Stygall J, Hirani S, Shaefi S, Maze M. Postoperative cognitive dysfunction after noncardiac surgery. Anesthesiology. 2007;106:572–590. doi: 10.1097/00000542-200703000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Avidan MS, Evers AS. Review of clinical evidence for persistent cognitive decline or incident dementia attributable to surgery or general anesthesia. Journal of Alzheimer’s Disease. 2011;24:201–216. doi: 10.3233/JAD-2011-101680. [DOI] [PubMed] [Google Scholar]
- 7.Ghoneim MM, Block RI. Clinical, methodological and theoretical issues in the assessment of cognition after anaesthesia and surgery: a review. Eur J Anaesthesiol. 2012;29:409–422. doi: 10.1097/EJA.0b013e328356bd6e. [DOI] [PubMed] [Google Scholar]
- 8.Krenk L, Rasmussen LS, Kehlet H. New insights into the pathophysiology of postoperative cognitive dysfunction. Acta Anaesthesiol Scand. 2010;54:951–956. doi: 10.1111/j.1399-6576.2010.02268.x. [DOI] [PubMed] [Google Scholar]
- 9.Monk TG, Weldon BC, Garvan CW, et al. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology. 2008;108:18–30. doi: 10.1097/01.anes.0000296071.19434.1e. [DOI] [PubMed] [Google Scholar]
- 10.Müllges W, Berg D, Schmidtke A, Weinacker B, Toyka KV. Early natural course of transient encephalopathy after coronary artery bypass grafting. Crit Care Med. 2000;28:1808–1811. doi: 10.1097/00003246-200006000-00020. [DOI] [PubMed] [Google Scholar]
- 11.Selnes OA, Grega MA, Bailey MM, et al. Cognition 6 years after surgical or medical therapy for coronary artery disease. Ann Neurol. 2008;63:581–590. doi: 10.1002/ana.21382. [DOI] [PubMed] [Google Scholar]
- 12.Kline RP, Pirraglia E, Cheng H, et al. for the Alzheimer’s Disease Neuroimaging Initiative: Surgery and brain atrophy in cognitively normal elderly subjects and subjects diagnosed with mild cognitive impairment. Anesthesiology. 2012;116:603–612. doi: 10.1097/ALN.0b013e318246ec0b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abildstrom H, Rasmussen LS, Rentowl P, et al. Cognitive dysfunction 1-2-years after non-cardiac surgery in the elderly. Acta Anaesthesiol Scand. 2000;44:1246–1251. doi: 10.1034/j.1399-6576.2000.441010.x. [DOI] [PubMed] [Google Scholar]
- 14.Moller JT, Cluitmans P, Rasmussen LS, et al. Long-term postoperative cognitive dysfunction in the elderly: ISPOCD1 study. Lancet. 1998;251:857–861. doi: 10.1016/s0140-6736(97)07382-0. [DOI] [PubMed] [Google Scholar]
- 15.Ward B, Imarengiaye C, Peirovy J, Chung F. Cognitive function is minimally impaired after ambulatory surgery. Can J Anaesth. 2005;52:1017–1021. doi: 10.1007/BF03021598. [DOI] [PubMed] [Google Scholar]
- 16.Steinmetz J, Christensen KB, Lund T, Lohse N, Rasmussen LS ISPOCD Group. Long-term consequences of postoperative cognitive dysfunction. Anesthesiology. 2009;110:548–555. doi: 10.1097/ALN.0b013e318195b569. [DOI] [PubMed] [Google Scholar]
- 17.Murkin JM, Newman SP, Stump DA, Blumenthal JA. Statement of consensus on assessment of neurobehavioral outcomes after cardiac surgery. Ann Thorac Surg. 1995;59:1289–1295. doi: 10.1016/0003-4975(95)00106-u. [DOI] [PubMed] [Google Scholar]
- 18.Erzigkeit H. Weinheim, Germany: Beltz Test GmbH; 1989. SKT Manual. [Google Scholar]
- 19.Dressler I, Fritzsche I, Spies C, Cortina K, Rundshagen I. Psychomotor dysfunction after remifentanil/propofol anaesthesia. Eur J Anaesthesiol. 2007;24:347–354. doi: 10.1017/S0265021506001530. [DOI] [PubMed] [Google Scholar]
- 20.Chung F, Kayumov L, Sinclair DR, Edward R, Moller HJ, Shapiro CM. What is the driving performance of ambulatory surgical patients after general anesthesia? Anesthesiology. 2005;103:951–956. doi: 10.1097/00000542-200511000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Helkala EL, Hallikainen M, Alhainen K, et al. Usefulness of repeated presentation of Mini-Mental State Examination a diagnostic procedure—a population based study. Acta Neurol Scand. 2002;106:341–346. doi: 10.1034/j.1600-0404.2002.01315.x. [DOI] [PubMed] [Google Scholar]
- 22.Broadbent DE, Cooper PF, FitzGerald P, Parkes KR. Cognitive failure questionnaire and its correlates. Br J Clin Psychol. 1982;21:1–16. doi: 10.1111/j.2044-8260.1982.tb01421.x. [DOI] [PubMed] [Google Scholar]
- 23.Rudolph JL, Schreiber KA, Culley DJ, et al. Measurement of postoperative cognitive dysfunction after cardiac surgery: a systematic review. Acta Anaesthesiol Scand. 2010;54:663–677. doi: 10.1111/j.1399-6576.2010.02236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Terrando N, Eriksson LI, Ryu JK, et al. Resolving postoperative neuroinflammation and cognitive decline. Ann Neurol. 2011;70:986–995. doi: 10.1002/ana.22664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stratmann G. Neurotoxicity of anesthetic drugs in the developing brain. Anesth Analg. 2011;113:1170–1179. doi: 10.1213/ANE.0b013e318232066c. [DOI] [PubMed] [Google Scholar]
- 26.Ito A, Goto T, Maekawa K, Baba T, Mishima Y. Postoperative neurological complications and risk factors for pre-existing silent brain infarction in elderly patients undergoing coronary artery bypass grafting. J Anesth. 2012 doi: 10.1007/s00540-012-1327-4. DOI: 10.1007/s00540-012-1327-4. [DOI] [PubMed] [Google Scholar]
- 27.Ng J, Chan MTV, Gelb AW. Perioperative stroke in noncardiac, nonneurosurgical surgery. Anesthesiology. 2011;115:879–890. doi: 10.1097/ALN.0b013e31822e9499. [DOI] [PubMed] [Google Scholar]
- 28.Hudetz JA, Iqbal Z, Gandhi SD, et al. Postoperative cognitive dysfunction in older patients with a history of alcohol abuse. Anesthesiology. 2007;106:423–430. doi: 10.1097/00000542-200703000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Ancelin ML, De Roquefeuil G, Ledesert B, Bonnel F, Cheminal JC, Ritchie K. Exposure to anaesthetic agents, cognitive functioning and depressive symptomatology in the elderly. Br J Psychiatry. 2001;178:360–366. doi: 10.1192/bjp.178.4.360. [DOI] [PubMed] [Google Scholar]
- 30.Gameiro M, Eichler W, Schwandner O, et al. Patient mood and neuropsychological outcome after laparoscopic and conventional colectomy. Surgical Innovation. 2008;15:171–178. doi: 10.1177/1553350608320554. [DOI] [PubMed] [Google Scholar]
- 31.Mason SE, Noel-Storr A, Ritchie CA. The impact of general and regional anesthesia on the incidence of postoperative cognitive dysfunction and postoperative delirium: a systematic review with meta-analysis. J Alzheimers Dis. 2010;22:67–79. doi: 10.3233/JAD-2010-101086. [DOI] [PubMed] [Google Scholar]
- 32.Rasmussen LS, Schmehl W, Jakobsson J. Comparison of xenon with propofol for supplementary general anaesthesia for knee replacement: A randomized study. Br J Anaesth. 2006;97:154–159. doi: 10.1093/bja/ael141. [DOI] [PubMed] [Google Scholar]
- 33.Coburn M, Baumert HJ, Roertgen D, et al. Emergence and early cognitive function in the elderly after xenon or desflurane anaesthesia: a double-blinded randomized controlled trial. British Journal of Anaesthesia. 2007;98:756–762. doi: 10.1093/bja/aem103. [DOI] [PubMed] [Google Scholar]
- 34.Hoecker J, Stapelfeldt C, Leiendecker J, et al. Postoperative neurocognitive dysfunction in elderly. patients after xenon versus propofol anesthesia for major noncardiac surgery. Anesthesiology. 2009;110:1068–1076. doi: 10.1097/ALN.0b013e31819dad92. [DOI] [PubMed] [Google Scholar]
- 35.Cremer J, Stoppe C, Fahlenkamp AV, et al. Early cognitive function, recovery and well-being after sevoflurane and xenon anaesthesia in the elderly: a double-blinded randomized controlled trial. Medical Gas Research. 2011 doi: 10.1186/2045-9912-1-9. 1 9. www.medicalgasresearch.com/content/1/1/9) (last accessed on 17th December 2013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Puskas F, Grocott HP, White WD, Mathew JP, Newman MF, Bar-Yosef S. Intraoperative hyperglycemia and cognitive decline after CABG. Ann Thorac Surg. 2007;84:1467–1473. doi: 10.1016/j.athoracsur.2007.06.023. [DOI] [PubMed] [Google Scholar]
- 37.Reijmer YD, van den Berg E, Dekker JM, et al. Development of vascular risk factors over 15 years in relation to cognition: The Hoorn Study. JAGS. 2012;60:1426–1433. doi: 10.1111/j.1532-5415.2012.04081.x. [DOI] [PubMed] [Google Scholar]
- 38.Kretzschmer N. Beeinflusst die Narcotrend gestützte Narkose die psychomotorischen Funktionen in der frühen postoperativen Phase? Dissertation der Medizinischen Fakultät der Humboldt Universität. Charité - Universitätsmedizin Berlin. 2013 [Google Scholar]
- 39.Farag E, Chelune GJ, Schubert A, Mascha EJ. Is depth of anesthesia, as assessed by the bispectral index, related to postoperative cognitive dysfunction and recovery? Anesth Analg. 2006;103:633–640. doi: 10.1213/01.ane.0000228870.48028.b5. [DOI] [PubMed] [Google Scholar]
- 40.Chan MTV, Cheng BCP, Lee TMC, Gin T and the Coda Trial Group. BIS-guided anesthesia decreases postoperative delirium and cognitive decline. J Neurosurg Anesthesiol. 2013;25:33–42. doi: 10.1097/ANA.0b013e3182712fba. [DOI] [PubMed] [Google Scholar]