Abstract
Background
Although the bidirectional association between depressive symptoms and adiposity has been recognized, the contribution of neighborhood factors to this relationship has not been assessed. This study evaluates whether physical and social neighborhood environment modify the bidirectional relationship between depressive symptoms and adiposity (measured by waist circumference and BMI).
Methods
Using data on 5,122 men and women (age 45-84 years) from the Multi-Ethnic Study of Atherosclerosis (MESA) we investigated whether neighborhood physical (i.e. walking environment, availability of healthy food) and social (i.e. safety, aesthetics, social coherence) environments modified the association between: (1) baseline elevated depressive symptoms (EDS, Center for Epidemiologic Study Depression Scale score ≥ 16) and change in adiposity (as measured by waist circumference [WC] and body mass index [BMI]); and (2) baseline overweight/obesity (WC > 102 cm for men and > 88 cm for women, or BMI ≥ 25 kg/m2) and change in depressive symptoms using multilevel models. Neighborhood-level factors were obtained from the MESA Neighborhood Study.
Results
A greater increase in WC in participants with versus without EDS was observed in those living in poorly-rated physical environment, but not in those living in better-rated environments (interaction p-value=0.045). No associations were observed with BMI. Baseline overweight/obesity was not associated with change in depressive symptoms and there was no modification by neighborhood-level factors.
Conclusions
EDS were associated with greater increase in WC among individuals living in poor than in better-rated physical environments. No association was found between overweight/obesity and change in depressive symptoms.
Keywords: Depressive Symptoms, Depression, Overweight/Obesity, Adiposity, Neighborhood, Physical/Social Environment
INTRODUCTION
Previous work have reported bidirectional relations between depressive symptoms and adiposity. A recent meta-analysis showed that baseline depression is associated with higher odds of becoming overweight/obese, and that overweight/obese individuals at baseline have greater odds of becoming depressed compared to those of normal weight,1 suggesting a bidirectional relationship. Some bidirectional studies, nevertheless, have presented mixed results, possibly owing to differences in anthropometry assessment and the racial profile of the study population.2-6
Proposed pathophysiologic pathways between depression and adiposity include dysfunction in the hypothalamus-pituitary-adrenal (HPA) axis and exaggerated inflammatory response. The association of depression with HPA axis hyperactivity, marked by prolonged heightened cortisol levels, may contribute to the accumulation of visceral adiposity due to the high density of glucocorticoid receptors in visceral adipose tissue (VAT).7 In addition, depression is associated with elevated inflammatory markers which might alter eating behavior and/or promote weight gain.8 Conversely, increased adiposity also results in elevated inflammatory markers and immune activation which have been found to induce depression.9
Overweight/obesity may also lead to elevated depressive symptoms (EDS) by the proposed health and appearance concern pathway. In the health concern pathway, obese individuals report functional impairment and poor self-rated health, which can contribute to EDS.10 In the appearance concern pathway, obese individuals experience more body image dissatisfaction, distress regarding repeated diet failures, and actual or perceived stigma related to obesity.10 This can lead to low self-esteem, contributing to EDS, and may also explain why the obesity-EDS association is stronger in women than men.10
In parallel to investigations on depression and adiposity/body mass index (BMI), a growing body of work links neighborhood physical and social environments to these factors. Although results are not consistent, observational studies report associations of neighborhood accessibility to healthy foods with diet and associations of aesthetically pleasant environments and physical activity resources with walkability, physical activity and BMI.11-13 Lower social cohesion, poor aesthetic quality and greater violence within neighborhoods are also related to EDS.14 The availability of healthy food is associated with diet11, 15 and possibly decreased prevalence of depression.16 Thus, increasing healthy food options within neighborhoods may also inadvertently help decrease risk for EDS. Recently, a randomized trial, Moving to Opportunity for Fair Housing,17 demonstrates that low income persons (predominantly women) randomized to receive vouchers to move to low poverty neighborhoods experienced reductions in extreme obesity and HbA1c levels and improvements in mental health.17, 18
There is reason to think that the environment may modify the bidirectional relation between depression and adiposity. For example, depressed persons living in unfavorable (compared to favorable) food environments may more likely engage in unhealthy eating patterns as a consequence of their depression or may exercise less, especially if they live in neighborhoods with poor walking conditions. Conversely, environments that facilitate healthy behaviors may buffer the adverse effects of depression on adiposity. This would result in stronger associations of depression with subsequent development of adiposity in unfavorable environments. It is also possible that the link between adiposity and depression development is strengthened by living in unsafe or less cohesive environments, if for example the psychological or behavioral consequences of adiposity are magnified in stressful neighborhoods.
Using unique longitudinal data from a large population sample including repeat measures of depressive symptoms and adiposity, as well as measures of neighborhood, we investigated whether neighborhood factors modify the bidirectional association between depressive symptoms and adiposity. We hypothesized that EDS would be associated with increases in adiposity measurements and that this relationship would be greater among residents of poor versus better physical and/or social environments. We also hypothesized that overweight/obesity at baseline would be associated with increases in depressive symptoms, and that this association would also be stronger among residents of neighborhoods with poor versus better physical and/or social environments.
METHODS
Study Population
The Multi-Ethnic Study of Atherosclerosis (MESA) is a multi-center study to examine the prevalence, correlates and progression of subclinical cardiovascular disease.19 There were 6,814 men and women aged 45-84 years, self-identified as White, Chinese, Black or Hispanic, and free of known clinical cardiovascular disease, recruited from 6 US communities: Baltimore City and Baltimore County, Maryland; Chicago, Illinois; Forsyth County, North Carolina; Los Angeles County, California; Northern Manhattan and the Bronx, New York; and St. Paul, Minnesota. The first exam took place between 2000 and 2002, the second between 2002 and 2004, the third between 2004 and 2005, and the fourth between 2005 and 2007. Written informed consent was obtained from participants, and the study was approved by the Institutional Review Boards of each institution. Additional details regarding MESA's design and objectives have been published.19
Depressive Symptoms Assessment (Exams 1, 3, and 4)
Depressive symptoms were measured using the Center for Epidemiologic Studies Depression (CES-D) Scale, a 20-item questionnaire developed to assess past week's depressive symptoms among community populations,20 administered in English, Spanish, Cantonese, and Mandarin. Although the CES-D is not an assessment for clinical depression, EDS, as defined by a CES-D score 16, are consistent with at least mild-to-moderate depression or dysthymia.21 Using this cut-off, sensitivity and specificity for major depression in the past year has been reported as 70.6% and 88%, respectively.21 The internal consistency reliability of CES-D has been shown to be a coefficient alpha of 0.85 for the general population and 0.90 for a psychiatric patient population,20 and has been found comparable in European-American, African-American, Mexican-American and Chinese-American groups.20, 22, 23 The CES-D has been used widely in cross-cultural epidemiological studies conducted with validated Spanish24 and Chinese versions.23 To account for the contribution of antidepressant use in the relationship between EDS and adiposity, this variable was included in every model.
Adiposity Assessment (Exams 1-4)25
Waist circumference (WC) was measured at the minimum abdominal girth (to the nearest 0.1 cm) using a steel measuring tape of a standard 4-oz tension. Elevated WC corresponding to disease risk among overweight and obese adults was defined as >102 cm for men and >88 cm for women.
Weight and height were measured using a balance beam scale and a stadiometer, respectively, with participants wearing light clothing and no shoes. Height was recorded to the nearest 0.5 cm and weight to the nearest 0.5 kg. BMI was calculated as weight (kg) divided by height squared (m2). Weight categories were defined as normal <25kg/m2 and overweight/obese ≥25kg/m2.
Although central and general adiposity (measured by WC and BMI, respectively) are not synonymous, for simplicity, the terms adiposity and overweight/obese will be used for either measures.
Covariates
Using previously described standard protocols,19 individual-level covariates were assessed fixed at baseline, with the exception of antidepressant use which was time-varying (exams 1-4). Covariates included socio-demographics (age, race/ethnicity, sex, marital status, study site, education, income), use of antidepressants, inflammatory markers (interleukin-6 [IL-6], c-reactive protein [CRP]), health behaviors (current smoking status, number of alcoholic drinks consumed per week, total intentional exercise, daily caloric intake, dietary patterns), social support and comorbidity (type 2 diabetes, cancer, hypertension). IL-6 and CRP were measured using ultra-sensitive ELISA (Quantikine HS Human IL-6 Immunoassay; R&DSystems, Minneapolis, MN) and the BNII nephelometer (N High Sensitivity CRP; Dade Behring Inc., Deerfield, IL), respectively. Total intentional exercise was determined using a 28-item Typical Week Physical Activity Survey.19 Physical activity was summarized as the metabolic equivalent task of minutes per week (met-min/week) spent in moderate/vigorous household, outdoor, sporting, conditioning and volunteer activities. Four dietary patterns were derived from 47 food groups using principal components analysis adapted from previous methodology (using SAS version 9.1, SAS Institute Inc., Cary, NC) and named based on the highest loading food groups: 1) High-fat and Processed Meats, 2) Vegetables and Fish, 3) Beans, Tomatoes and Refined Grains, and 4) Whole Grains and Fruit.26 Each dietary pattern score was calculated as the sum of the daily servings of all food groups multiplied by each food group's respective factor loading. Each participant received a score for each of the four dietary patterns.
A list of items used to assess emotional social support was listed in Table 1.27 Self-reported cancer included a doctor's diagnosis for prostate, breast, lung, colon, blood, nonmelanoma skin cancer, or other cancer. Type 2 diabetes was defined by fasting plasma glucose ≥126 mg/dl and/or use of medications for diabetes.28 Blood pressure was measured in a seated position three times, and the average of the last two measurements was used. Hypertension was defined by a systolic blood pressure ≥140 mmHg, a diastolic blood pressure ≥90 mmHg or use of anti-hypertensive medications.29
Table 1.
Question Items Used To Assess Emotional Social Support
| 1. | Is there someone available to you whom you can count on to listen to you when you need to talk? |
| 2. | Is there someone available to give you good advice about a problem? |
| 3. | Is tehre someone available to you who shows you love and affection? |
| 4. | Is there someone avaialbe to helpyou with daily chores? |
| 5. | Do you have as much contact as you would like with someone you feel close to or someone in whom you can trust and confide? |
| 6. | Can you count on anyone to provide you with emotional support (talking over problems or helping you make a difficult decision)? |
NOTE: Possible answers were scaled from 1to5 which included ‘none of the time’ (scored as 1), ‘a little of the time,’ ‘some of the time,’ ‘most of the time,’ or ‘all of the time’ (scored as 5). A summary score was calculated ranging from 5to30. If any items were missing, a summary score was not provided.
Neighborhood-level data was obtained via telephone interview from the Neighborhood Ancillary Study between January and August of 2004. MESA participants were asked to comment on the area within approximately a mile radius (1.6 km) around their house. Census tracts were used as proxies for neighborhoods and the analytic unit was one standard deviation for each scale.30 Neighborhood measures were created by aggregating all responses of participants within a census tract using conditional empirical Bayes estimates adjusted for age, sex and study site.
Previous studies have identified seven neighborhood dimensions potentially linked to CVD risk,31 five of which were used in this study (Table 2): walking environment, availability of healthy foods, aesthetic quality, safety and social cohesion. These dimensions were combined into two neighborhood characteristics (physical and social environment) using similar techniques as for dietary patterns.13 Physical environment included walking environment and the availability of healthy foods. Social environment included aesthetic quality, safety and social cohesion. Social cohesion was asked at visit 1 while other scales were asked during visits 2 or 3. Each response was scored on a 5 point Likert scale of 1=strongly agree, 2=agree, 3=neutral, 4=disagree, and 5=strongly disagree. All of the items were reverse coded when appropriate so that higher item responses corresponded to better aesthetic quality and walkability, more availability of healthy foods and increased perceived safety, and less violence in neighborhoods. The median summary score for each construct was used to designate “good” versus “poor” physical or social environment, with higher values indicating “better” environments.
Table 2.
Question Items Used To Assess Neighborhood Physical and Social Environment
| Neighborhood Characteristic | Question Item |
|---|---|
| Physical Environment | |
| Walking Environment | 1. It is pleasant to walk in my neighborhood. |
| 2. In my neighborhood it is easy to walk places. | |
| 3. I often see other people walking in my neighborhood. | |
| 4. I often see other people exercise (for example jog, bicycle, play sports) in my neighborhood. | |
| Aesthetic Quality | 1. There is a lot of trash and litter on the street in my neighborhood. |
| 2. There is a lot of noise in my neighborhood. | |
| 3. My neighborhood is attractive | |
| Social Environment | |
| Availability of Healthy Foods | 1. A large selection of fresh fruits and vegetables is available in my neighborhood. |
| 2. A large selection of low fat products is available in y neighborhood. | |
| Safety | 1. I feel safe walking in my neighborhood day or night. |
| 2. Violence is a problem in my neighborhood. | |
| Social Cohesion | 1. People around heare are willing to help their neighbors. |
| 2. People in my neighborhood generally get along with each other. | |
| 3. People in my neighborhood can be trusted. | |
| 4. People in my neighborhood share the same values. |
Statistical Analyses
Of the 6,814 participants, 652 had no assigned neighborhood and 133 had no observation for physical or social environment or length of residency in assigned neighborhood. Further, 16 had missing CES-D, BMI and WC values at baseline or outlying WC values (>190 cm or <50 cm), and 877 had missing covariate values. Individuals who reported use of weight loss pills were also excluded from the study (n=14), leaving a final study population of 5,122. All participants had at least one follow-up outcome measurement.
We compared the distribution of baseline characteristics by exposure using Student's ‘t’ and chi-square tests for continuous and categorical variables, respectively. Wilcoxon Rank-Sum Test for two-group comparison was used for non-normally distributed continuous variables.
Multivariable linear mixed-effects regression was used to model repeat measures of the outcome (CES-D or WC/BMI) as a function of time since baseline, key exposure, neighborhood factor (physical/social environment), covariates, and interaction terms. The following formula (1) illustrates the general modeling, with β7 serving as the interaction term of interest (i.e. the difference between poor and better neighborhood environment in the difference in change of outcome between exposure groups):1
| (1) |
Likelihood ratio tests were used to determine inclusion of random effects. Main exposures were evaluated fixed at baseline. Exact exam time from baseline was utilized. Neighborhood variables were treated as time-invariant based on baseline addresses.
A sequence of adjustment models was fitted to assess the influence of potential confounders/mediators. First, unadjusted analysis was done to model the outcome (i.e. formula [1] above excluding β8). This was followed by an adjustment for socio-demographics and then including antidepressant use. Subsequent models added inflammatory markers, health behaviors, social support and co-morbidities. The fully-adjusted model included all covariates. Due to minimal changes in estimate after individual covariate adjustments, only models that were unadjusted, adjusted for socio-demographics and antidepressants, and fully-adjusted were reported.
EDS and Change in Adiposity
WC and BMI were analyzed separately as continuous outcomes. To determine if changes in adiposity over time varied by status of depressive symptomatology at baseline, an interaction term between time and EDS status was included. To examine interactions with physical and social environment, interaction terms as shown in formula (1) were also created.
Overweight/Obesity and Change in Depressive Symptomatology
Depressive symptoms were analyzed as a continuous outcome. To determine if changes in depressive symptoms over time varied by baseline overweight/obesity status, an interaction term between time and baseline adiposity status was included. A separate model was done for WC and BMI. As in the previous analysis, interaction terms were created to assess modification by physical and social environment (see formula [1]).
With the exception of generating dietary patterns, all analyses were completed using STATA (StataCorp. 2012. Stata Statistical Software: Release 12. College Station, TX). P-values were considered significant at a two-sided alpha <0.05.
RESULTS
EDS and Change in Adiposity
Table 3 illustrates the population characteristics by depressive symptomatology. Individuals with EDS at baseline were younger, more likely to be female, more likely to be of Hispanic background, less likely to be married and had lower education and income than those without EDS. In addition, EDS were associated with higher level of inflammation, less exercise, higher daily caloric intake, and less perceived social support. Those with EDS were more likely to live in neighborhoods with lower levels of education and median income compared to individuals without EDS. Surprisingly, they were less likely to reside in poorly-rated physical environments; however they were more likely to reside in poorly-rated social environments. Individuals with EDS were more likely to be overweight/obese based on WC and BMI.
TABLE 3.
Baseline Population Characteristics (Analysis 1: Elevated Depressive Symptoms (EDS, CES-D ≥ 16) As a Predictor of Adiposity Change; Analysis 2: Waist Circumference-Defined Overweight/Obesity a As a Predictor of CES-D Score Change), N=5,122
| Analysis 1 | Analysis 2 | |||||
|---|---|---|---|---|---|---|
| Covariates | No EDS (n=4,500) | EDS (n=622) | p-value | Normal Weight (n=2,407) | Overweight / Obese (n=2,715) | p-value |
| Demographics | ||||||
| Age (years] | 62.1 | 60.7 | 0.002* | 61.2 | 62.5 | <0.0001* |
| Female (%) | 50.6 | 68.2 | <0.0001* | 36.8 | 67.0 | <0.0001* |
| Race (%) | <0.0001* | <0.0001* | ||||
| White | 43.1 | 32.0 | 42.0 | 41.5 | ||
| Chinese | 13.5 | 8.8 | 21.0 | 5.8 | ||
| Blacks | 24.2 | 22.5 | 19.6 | 28.0 | ||
| Hispanics | 19.2 | 36.7 | 17.4 | 24.7 | ||
| Marital Status (%) | <0.0001* | <0.0001* | ||||
| Married | 65.2 | 48.2 | 68.9 | 58.0 | ||
| Widowed/Divorced/Separated | 26.9 | 40.0 | 22.7 | 33.6 | ||
| Single | 8.0 | 11.7 | 8.4 | 8.5 | ||
| Education (%) | <0.0001* | <0.0001* | ||||
| Less than High School | 14.7 | 28.0 | 14.3 | 18.1 | ||
| High School | 17.2 | 19.0 | 15.3 | 19.4 | ||
| College or greater | 68.1 | 53.1 | 70.5 | 62.5 | ||
| Income (%) | <0.0001* | <0.0001* | ||||
| <$25,000 | 27.1 | 44.7 | 26.8 | 31.4 | ||
| ≥$25,000 and < $50,000 | 28.8 | 30.2 | 26.6 | 31.2 | ||
| ≥$50,000 and < $75,000 | 17.8 | 13.2 | 17.0 | 17.5 | ||
| <$75,000 | 26.3 | 11.9 | 29.8 | 19.9 | ||
| Inflammatory Markers | ||||||
| Median IL-6 (pg/mL) | 1.14 | 1.29 | 0.0001* | 0.90 | 1.42 | <0.0001* |
| Median CRP (mg/L) | 1.78 | 2.09 | 0.007* | 1.09 | 2.84 | <0.0001* |
| Health Behavior | ||||||
| Number of Alcoholic Drinks/wk | 4.1 | 3.7 | 0.276 | 4.5 | 3.6 | 0.001* |
| Smoking Status | <0.0001* | 0.305 | ||||
| Never | 51.2 | 52.7 | 50.4 | 52.4 | ||
| Former | 37.6 | 31.5 | 37.5 | 36.4 | ||
| Current | 11.1 | 15.8 | 12.1 | 11.2 | ||
| Exercise (met-min/wk) | 896 | 630 | <0.0001* | 1095 | 720 | <0.0001* |
| Daily caloric intake (kcal) | 1,478 | 1,602 | 0.0002* | 1,474 | 1,508 | 0.112 |
| Dietary Patterns (% in 5th score quintile) b | ||||||
| High-fat and Processed food | 19.6 | 22.8 | 0.059 | 16.4 | 23.2 | <0.0001* |
| Vegetables and Fish | 19.9 | 20.6 | 0.696 | 23.2 | 17.2 | <0.0001* |
| Beans, Tomatoes, Refined Grains | 18.4 | 31.2 | <0.0001* | 16.7 | 22.9 | <0.0001* |
| Whole grains and Fruit | 19.8 | 21.7 | 0.255 | 18.5 | 21.3 | 0.014* |
| Social Support | 24.86 | 19.77 | <0.0001* | 24.35 | 24.14 | 0.146 |
| Comorbidities (% Yes) | ||||||
| Diabetes | 11.0 | 14.8 | 0.006* | 7.6 | 14.9 | <0.0001* |
| Cancer | 8.3 | 7.2 | 0.378 | 6.9 | 9.3 | 0.002* |
| Hypertension | 3.1 | 44.1 | 0.642 | 33.8 | 51.5 | <0.0001* |
| Neighborhood Factors | ||||||
| Number of years residence | 18.9 | 18.3 | 0.317 | 17.6 | 20.0 | <0.0001* |
| % with at least a HS diploma | 78.0 | 72.6 | <0.0001* | 78.5 | 76.2 | <0.0001* |
| Median income ($) | 45,974 | 40,615 | <0.0001* | 47,644 | 43,265 | <0.0001* |
| Physical Environment (SD) | ||||||
| Walking environment | 3.93 | 3.93 | 0.978 | 3.95 | 3.91 | <0.0001* |
| Availability of healthy foods | 3.49 | 3.59 | <0.0001* | 3.55 | 3.56 | <0.0001* |
| Below median score (%) | 49.6 | 44.1 | 0.010* | 46.5 | 51.1 | 0.001* |
| Social Environment (SD) | ||||||
| Aesthetic quality | 3.79 | 3.65 | <0.0001* | 3.78 | 3.76 | 0.005* |
| Safety | 3.76 | 3.68 | <0.0001* | 3.77 | 3.74 | 0.0002* |
| Social cohesion | 3.57 | 3.51 | <0.0001* | 3.56 | 3.57 | 0.318 |
| Below median score (%) | 47.9 | 62.5 | <0.0001* | 50.5 | 0.209 | |
| Anthropometry | ||||||
| Waist Circumference, in cm (mean) | 97.5 | 98.9 | 0.023* | 87.5 | 106.7 | <0.0001* |
| Overweight/Obese (%) | 52.0 | 60.1 | <0.0001* | --- | --- | --- |
| BMI, in kg/m2 (mean) | 28.0 | 29.0 | <0.0001* | 24.6 | 31.3 | <0.0001* |
| Overweight/Obese (%) | 70.2 | 74.4 | 0.029* | 45.5 | 93.1 | <0.0001* |
| Weight, in kg (mean) | 173.0 | 170.8 | 0.162 | 1953.9 | 189.4 | <0.0001* |
| CES-D | ||||||
| Mean | 5.2 | 23.0 | <0.0001* | 6.7 | 7.9 | <0.0001* |
| Depressed (%) | --- | --- | --- | 10.3 | 13.8 | <0.0001* |
| Use of Antidepressants | ||||||
| Yes (%) | 7.5 | 16.9 | <0.0001* | 5.1 | 9.5 | <0.0001* |
Overweight/Obese: Waist Circumference > 88 cm for women and > 102 cm for men
The estimates for dietary patterns represent the percentage of the upper 20th percentile of score on each pattern. For example, for Aim 1, the percentage of those with elevated depressive symptoms who scored in the upper 20th percentile on the High-fat and Processed Meats dietary pattern was 23.2% compared to 19.6% of those without elevated depressive symptoms.
Significant level p-value < 0.05
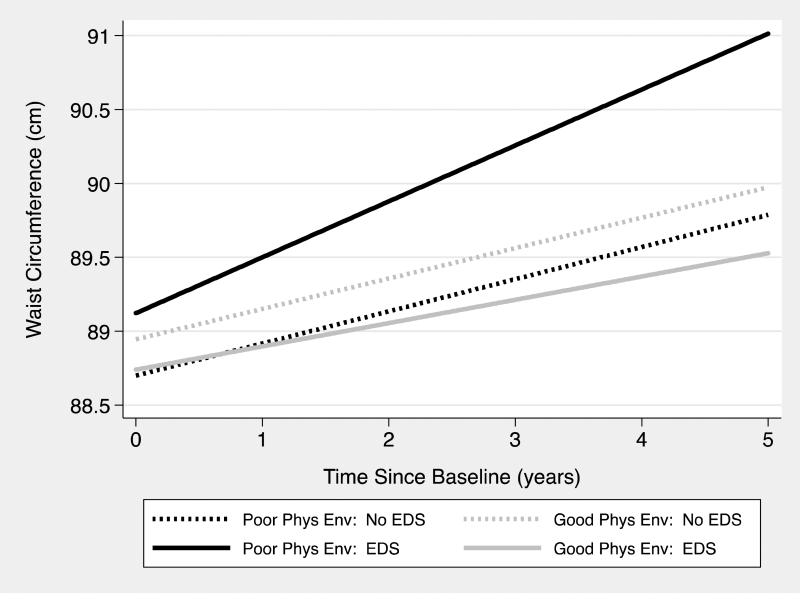
Although the association between baseline EDS and subsequent changes in WC was not modified by social environment, we found statistically significant modification by physical environment (p=0.045). Among participants residing in poorly-rated neighborhoods, those with EDS had a 0.16 cm (95% CI: 0.01 to 0.31 cm) significantly greater increase in WC per year than those without EDS (Table 4 and Figure 1). There was no significant difference in WC change between individuals with and without EDS among those residing in better-rated physical environments.
TABLE 4.
Difference in Annual Change In Waist Circumference (in cm) In Persons With And Without Elevated Depressive Symptoms At Baseline (EDS, CES-D ≥ 16) In The Total Sample And In Physical and Social Environment Strata, N=5,122
| Variable | Strata | Modela | No EDS | EDS | Difference (95% CI) |
|---|---|---|---|---|---|
| All | All | Model 1 | 0.21 | 0.26 | 0.04 (−0.06, 0.14) |
| Model 2 | 0.21 | 0.26 | 0.04 (−0.06, 0.15) | ||
| Model 3 | 0.21 | 0.25 | 0.04 (−0.06, 0.14) | ||
| Physical Environment | Poor Rating | Model 1 | 0.22 | 0.38 | 0.16(0.01, 0.31)* |
| Model 2 | 0.22 | 0.38 | 0.16(0.01, 0.31)* | ||
| Model 3 | 0.22 | 0.38 | 0.16(0.01, 0.31)* | ||
| Good Rating | Model 1 | 0.21 | 0.16 | −0.05 (−0.18, 0.09) | |
| Model 2 | 0.20 | 0.16 | −0.05 (−0.18, 0.09) | ||
| Model 3 | 0.21 | 0.16 | −0.05 (−0.18, 0.09) | ||
| Interaction p-value: Physical Environmentb | 0.045 * | ||||
| Social Environment | Poor Rating | Model 1 | 0.26 | 0.25 | −0.02 (−0.15, 0.11) |
| Model 2 | 0.26 | 0.25 | −0.02 (−0.15, 0.11) | ||
| Model 3 | 0.26 | 0.25 | −0.02 (−0.15, 0.11) | ||
| Good Rating | Model 1 | 0.16 | 0.27 | 0.11 (−0.05, 0.27) | |
| Model 2 | 0.16 | 0.28 | 0.11 (−0.06, 0.27) | ||
| Model 3 | 0.16 | 0.27 | 0.11 (−0.06, 0.27) | ||
| Interaction p-value: Social Environmentb | 0.237 | ||||
Model 1: Unadjusted; Model 2: Adjusted for socio-demographic characteristics (age, sex, race/ethnicity, marital status, study site, education level, income level) and antidepressant use; Model 3 (Fully-adjusted): Socio-demographic characteristics, use of antidepressants, inflammatory markers (IL-6, CRP), health behaviors (smoking status, number of alcoholic drinks/week, total intentional exercise, daily caloric intake, dietary patterns), social support and co-morbidities (type 2 diabetes, cancer, hypertension)
Based on comparing results of fully-adjusted models
Significant level p-value < 0.05
Figure 1.
Difference in the Change in Waist Circumference (in cm) Between Those With and Without Elevated Depressive Symptoms (EDS) By Physical Environment (Phys Env), N=5,122
NOTE: Among those residing in poor physical environment (phys env), the change in average waist circumference per year was 0.16 cm significantly greater (p<0.05) among those with vs. without baseline EDS (black lines). Among those residing in good phys env, there was no significant difference in the change in average waist circumference per year between those with and without EDS at baseline (gray lines). The difference between those with and without baseline EDS in the rate of change in average waist circumference per year is greater in poor phys env than good phys env areas (interaction p-value=0.045).
There were very small changes in BMI and no significant differences between those with and without EDS, overall and within strata (data not shown). Also, no interaction with neighborhood factors was found.
Overweight/Obesity and Change in Depressive Symptomatology
Table 3 presents the population characteristics by weight status. Compared to normal weight individuals, those who were overweight/obese were older, more likely to be female, less likely to be Chinese and more likely to be Hispanic or Black, less likely to be married and had lower socioeconomic status (SES). In addition, they had greater levels of inflammation, less weekly alcohol consumption, exercised less, and had dietary patterns consisting of more high-fat, processed food, but less vegetables and fish compared to those of normal weight. Overweight/obese individuals were also more likely to have diabetes, hypertension, and cancer, as well as EDS. Compared to normal weight individuals, overweight/obese participants resided in their neighborhoods longer, and lived in lower SES neighborhoods. Overweight/obesity was also associated with more poorly-rated physical environment.
Overall, baseline overweight/obesity (defined using either WC or BMI) was not associated with change in depressive symptoms and there were no interactions by neighborhood factors (data not shown).
In all of the analyses, there were no significant changes in estimates after controlling for socio-demographic characteristics, antidepressant use, inflammatory markers, health behaviors, social support and co-morbidities.
DISCUSSION
Overall, we found EDS at baseline significantly associated with increases in WC over time but only among persons residing in poorly-rated physical environments. The difference in BMI changes by depressive symptoms status was small and no modification by the environment was observed. We did not find any significant change in CES-D scores by baseline weight status using either WC- or BMI-defined overweight/obesity, similar to findings from prior studies,2, 3 and there was no evidence that this was modified by environmental features.
Although results showed that EDS predicted change in WC for those residing in poorly-rated physical environments, we did not find a significant change in WC by EDS status in the overall group. The latter result contrasted with those of Needham et al, although the null findings for change in BMI were similar.3 Most prospective studies that have found a higher weight increase among those with depression or EDS have used BMI as the outcome.6, 32
The negligible difference in the rate of BMI increase by EDS status, compared to WC, might suggest that depressive symptoms are more closely related to visceral adiposity (as estimated by WC) than general adiposity (as measured by BMI). In the assessment of middle-aged women, Everson-Rose et al found that depressive symptoms were associated with VAT, but not subcutaneous tissue.33 This was supported by Lee et al who also found no significant association between BMI and depressive symptoms.34
Among those residing in poor physical environment, EDS were associated with a greater increase in WC, suggesting depression may act synergistically with the physical environment to affect future changes in WC. There are a number of possible explanations for these findings.
Living in an environment with poor physical features (e.g. poor walkability, decreased connectivity, lack of sidewalks), may discourage physical activity,12 leading to increased adiposity. In contrast, the presence of these neighborhood characteristics has been associated with greater physical activity and lower BMI in some studies.35 The availability of healthy food may affect diet.11, 15 It is plausible that individuals with depression are more dependent on local resources or are more sensitive to environmental features.36 Individuals residing in poor physical surroundings will also be less likely to benefit from the positive physiological changes37 and social aspects of exercise shown to alleviate mood.11, 38
Neighborhoods with poor physical environment are likely to have residents of lower socioeconomic status (SES) as in our study population.39 In a meta-analysis of socioeconomic inequalities, individuals residing in neighborhoods of low versus high SES had higher depression prevalence.40 They also exhibited greater stressors, weaker social support and poorer coping styles, escalating their risk for psychiatric disorders.41 The significant increase in adiposity among individuals with EDS residing in poorly-, but not in better-rated, physical environment, may be related to hypercortisolism from increased exposure to chronic stress associated with these neighborhoods.42 It is plausible that the measure of the social environment that we investigated did not fully capture these chronic stressors which could be correlated with the physical environment measure.
Most population-based studies show that individuals with EDS engage in obesity-promoting behaviors, including consumption of higher calorie diets and physical inactivity.43 The use of anti-depressants may also induce weight gain,44 making it a potential mediator in the association between depression and overweight/obesity. Although adjustment for these variables does not affect the estimates, suggesting other mechanisms may be involved, our analyses are limited in their ability to examine the mechanisms that may mediate the relationship. Social support which affects both depression and weight status also does not confound the relationship; however, the possibility of residual confounding remains.
Some limitations should be mentioned. The use of CES-D does not diagnose clinical depression; however, it is a meaningful measure of depressive symptoms shown to have good reliability and validity.20, 21 Time spent in sedentary behaviors was not directly measured, and diet was assessed at only one time point. The diet measures may also not be the most relevant to the development of adiposity or depression. Prior history of depression or depression treatment was also not assessed. In addition, census tract data used to define neighborhoods may only be imperfect proxies for the truly relevant spatial context (e.g. work environment). Further, although 23.5 million people in the US reportedly reside in food deserts,45 summary statistics on the overall walkability of US neighborhoods have yet to be estimated. Although this limits full assessment of the public health impact of poorly-rated physical environment on the depression-obesity relationship, it may be significant given obesity's high prevalence.
This research provided the opportunity to investigate the bidirectional association between adiposity and depressive symptoms. The MESA Neighborhood Study also allowed the evaluation of neighborhood-level factors, which have not, to our knowledge, been previously investigated as a potential modifier of this relationship. Further, MESA is unique in including four race/ethnic groups that provided a more generalizable evaluation of the depression-adiposity association than other prospective studies. WC and BMI were also clinically assessed, and, along with CES-D scores, were measured repeatedly over time. In addition, we examined the contribution of several covariates.
In conclusion, our study identified residents of poorly-rated physical environments as a high risk group for increased adiposity in the presence of EDS. Interventions aimed at improving neighborhood physical environment might assist in stabilizing or reducing obesity prevalence especially in individuals with EDS.
ACKNOWLEDGEMENTS
The NIDDK training grant (T32-DK062707) supported this work. MESA was supported by N01-HC-95159 through N01-HC-95169 from NHLBI and UL1-RR-024156 and UL1-RR-025005 from NCRR. The MESA Neighborhood Study was supported by 2R01-HL-071759 from NHLBI. RAR, SHG, MS, RC, JL, and MF were involved in literature review, study design, concept development and analyses. All authors contributed to writing and editing the manuscript. Ms. Kari Moore assisted with the neighborhood data (University of Michigan, Center for Social Epidemiology and Population Health).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
For simplicity, random effect terms were not included in this formula.
DISCLOSURE
The authors report no proprietary or commercial interest in any concept discussed in this article.
REFERENCES
- 1.Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BWJH, et al. Overweight, obesity and depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 2.Hasler G, Lissek S, Ajdacic V, Milos G, Gamma A, Eich D, et al. Major depression predicts and increase in long-term body weight variability in young adults. Obes Res. 2005;13:1991–1998. doi: 10.1038/oby.2005.244. [DOI] [PubMed] [Google Scholar]
- 3.Needham BL, Epel ES, Adler NE, Kiefe C. Trajectories of change in obesity and symptoms of depression: The CARDIA Study. Am J Public Health. 2010;100:1040–1046. doi: 10.2105/AJPH.2009.172809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pan A, Sun Q, Czernichow S, Kivimaki M, Okereke O, Lucas M, et al. Bidirectional association between depression and obesity in middle-aged and older women. International Journal of Obesity. 2011;36:595–602. doi: 10.1038/ijo.2011.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roberts RE, Deleger S, Strawbridge WJ, Kaplan GA. Prospective association between obesity and depression: Evidence from the Alameda County Study. International Journal of Obesity. 2003;27:514–521. doi: 10.1038/sj.ijo.0802204. [DOI] [PubMed] [Google Scholar]
- 6.Forman-Hoffman VL, Yankey JW, Hillis SL, Wallace RB, Wolinsky FD. Weight and depressive symptoms in older adults: Direction of influence? J Gerontol B Psychol Sci Soc Sci. 2007;62:S43–S51. doi: 10.1093/geronb/62.1.s43. [DOI] [PubMed] [Google Scholar]
- 7.Pasquali R, Vicennati V, Cacciari M, Pagotto U. The hypothalamic-pituitary-adrenal axis activity in obesity and the metabolic syndrome. Ann NY Acad Sci. 2006;1083:111–128. doi: 10.1196/annals.1367.009. [DOI] [PubMed] [Google Scholar]
- 8.Capuron L, Poitou C, Machaux-Tholliez D, Frochot V, Bouillot JL, Basdevant A, et al. Relationship between adiposity, emotional status and eating behaviour in obese women: role of inflammation. Psychol Med. 2011;41:1517–1528. doi: 10.1017/S0033291710001984. [DOI] [PubMed] [Google Scholar]
- 9.Currier MB, Nemeroff CB. Inflammation of mood disorders: Proinflammatory cytokines and the pathogenesis of depression. Anti-Inflammatory & Anti-Allergy Agents in Medicinal Chemistry. 2010;9:212–220. [Google Scholar]
- 10.Marokowitz S, Friedman MA, Arent SM. Understanding the relation between obesity and depression: Causal mechanisms and implications for treatment. Clinical Psychology: Science and Practice. 2008;15:1–20. [Google Scholar]
- 11.Franco M, Diez-Roux AV, Nettleton JA, Lazo M, Brancati F, Caballero B, et al. Availability of healthy foods and dietary patterns: the Multi-Ethnic Study of Atherosclerosis. Am J Clin Nutr. 2009;89:897–904. doi: 10.3945/ajcn.2008.26434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saelens BE, Sallis JF, Black JB, Chen D. Neighborhood-based differences in physical activity: An enviroment scale evaluation. Am J Public Health. 2003;93:1552–1558. doi: 10.2105/ajph.93.9.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mujahid MS, Diez Roux AV, Shen M, Gowda D, Sanchez B, Shea S, et al. Relation between neighborhood environments and obesity in the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2008;167:1349–1357. doi: 10.1093/aje/kwn047. [DOI] [PubMed] [Google Scholar]
- 14.Mair C, Diez Roux AV, Shen M, Shea S, Seeman T, Echeverria S, et al. Cross-sectional and longitudinal associations of neighborhood cohesion and stressors with depressive symptoms in the Multiethnic Study of Atherosclerosis (MESA). Ann Epidemiol. 2009;19:49–57. doi: 10.1016/j.annepidem.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moore LV, Diez Roux AV, Nettleton JA, Jacobs DR. Associations of the local food environment with diet quality - A quality comparison of assessments based on surveys and geographic information systems: The Multiethnic Study of Atherosclerosis. Am J Epidemiol. 2008;167:917–924. doi: 10.1093/aje/kwm394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sanchez-Villegas A, Delgado-Rodriguez M, Alonso A, Schlatter J, Lahortiga F, Majem LS, et al. Association of the Mediterranean dietary pattern with the incidence of depression: The Seguimiento Universidad de Navarra/University of Navarra Follow-up (SUN) Cohort. Arch Gen Psychiatry. 2009;66:1090–1098. doi: 10.1001/archgenpsychiatry.2009.129. [DOI] [PubMed] [Google Scholar]
- 17.Ludwig J, Sanbonmatsu L, Gennetian L, Adam E, Duncan GJ, Katz LF, et al. Neighborhood, obesity, and diabetes - A randomized social experiment. N Engl J Med. 2011;365:1509–1519. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sanbonmatsu L, Ludwig J, Katz LF, Gennetian LA, Duncan GJ, Kessler RC, et al. Moving to Opportunity Fair Housing Demonstration Program: Final Impacts Evaluation [WWW document] 2011 http://www.huduser.org/portal/publications/pubasst/MTOFHD.html.
- 19.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, et al. Multi-Ethnic Study of Atherosclerosis: Objectives and Design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 20.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:1385–1401. [Google Scholar]
- 21.Beekman AT, Deeg DJ, Van Limbeek J, Braam AW, De Vries MA, Van Tilburg W. Criterion validity of the Center for Epidemiologic Studies Depression Scale (CES-D): Results from a community-based sample of older subjects in the Netherlands. Psychol Med. 1997;27:231–235. doi: 10.1017/s0033291796003510. [DOI] [PubMed] [Google Scholar]
- 22.Roberts RE. Reliability of the CES-D scale in different ethnic contexts. Psychiatry Res. 1980;2:125–134. doi: 10.1016/0165-1781(80)90069-4. [DOI] [PubMed] [Google Scholar]
- 23.Cheung C, Bagley C. Validating an American scale in Hong Kong: The Center for Epidemiological Studies Depression Scale (CES-D). J Psychol. 1998;132:169–186. doi: 10.1080/00223989809599157. [DOI] [PubMed] [Google Scholar]
- 24.Aneshensel CS, Clark VA, Frerichs RR. Race, ethnicity, and depression: a confirmatory analysis. Journal of Personality and Social Psychology. 1983;44:385–398. doi: 10.1037//0022-3514.44.2.385. [DOI] [PubMed] [Google Scholar]
- 25.National Institute of Health Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults - The Evidence Report. National Institute of Health. Obes Res. 1998;6:51S–209S. [PubMed] [Google Scholar]
- 26.Nettleton JA, Steffen LM, Mayer-Davis EJ, Jenny NS, Kiang R, Herrington DM, et al. Dietary patterns are associated with biochemical markers of inflammation and endothelial activation in the Multi-Ethnic Study of Atherosclersosis (MESA). Am J Clin Nutr. 2006;83:1369–1379. doi: 10.1093/ajcn/83.6.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.ENRICHD Investigators Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD): study design and methods. Am Heart J. 2000;139:1–9. doi: 10.1016/s0002-8703(00)90301-6. [DOI] [PubMed] [Google Scholar]
- 28.Genuth S, Alberti K, Bennett P, Buse J, Defronzo R, Kahn R, et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003;26:3160–3167. doi: 10.2337/diacare.26.11.3160. [DOI] [PubMed] [Google Scholar]
- 29.Joint National Committee on Prevention Detection Evaluation and Treatment of High Blood Pressure The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI). Arch Intern Med. 1997;157:2413–2466. doi: 10.1001/archinte.157.21.2413. [DOI] [PubMed] [Google Scholar]
- 30.Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T. Assessing the measurement properties of neighborhood scales: From psychometrics to ecometrics. Am J Epidemiol. 2007;165:858–867. doi: 10.1093/aje/kwm040. [DOI] [PubMed] [Google Scholar]
- 31.Echeverria SE, Diez-Roux AV, Link BG. Reliability of self-reported neighborhood characteristics. Journal of Urban Health. 2004;81:682–701. doi: 10.1093/jurban/jth151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haukkala A, Uutela A, Salomaa V. Depressive symptoms, cynical hostility, and weight change: A 3-year follow-up among middle-aged men and women. International Journal of Behavioral Medicine. 2001;8:116–133. [Google Scholar]
- 33.Everson-Rose SA, Lewis TT, Karavolos K, Dugan SA, Wesley D, Powell LH. Depressive symptoms and increased visceral fat in middle-aged women. Psychosom Med. 2009;71:410–416. doi: 10.1097/PSY.0b013e3181a20c9c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee ES, Kim YH, Beck S-H, Lee S, Oh SW. Depressive mood and abdominal fat distribution in overweight premenopausal women. Obes Res. 2005;13:320–325. doi: 10.1038/oby.2005.43. [DOI] [PubMed] [Google Scholar]
- 35.Berke E, Koepsell T, Moudon A, Hoskins R, Larson E. Association of the built environment with physical activity and obesity in older persons. Am J Public Health. 2007;97:486–492. doi: 10.2105/AJPH.2006.085837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cutrona CE, Wallace G, Wesner KA. Neighborhood characteristics and depression: an examination of stress processes. Current Directions in Psychological Science. 2008;15:188–192. doi: 10.1111/j.1467-8721.2006.00433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thoren P, Floras JS, Hoffmann P, Seals DR. Endorphins and exercise: Physiological mechanisms and clinical implications. Med Sci Sports Exerc. 1990;22:417–428. [PubMed] [Google Scholar]
- 38.Grant I, Patterson TL, Yager J. Social supports in relation to physical health and symptoms of depression in the elderly. Am J Psychiatry. 1988;145:1254–1258. doi: 10.1176/ajp.145.10.1254. [DOI] [PubMed] [Google Scholar]
- 39.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Affairs. 2002;21:60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- 40.Lorant V, Dellege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: A meta-analysis. Amer J of Epidemiol. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- 41.Turner R, Lloyed D. The stress process and the social distribution of depression. J health Soc Behav. 1999;40:374–404. [PubMed] [Google Scholar]
- 42.Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems, and associations with socioeconomic status and health. Ann Behav Med. 2001;23:177–185. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- 43.Golden SH, Lazo M, Carnethon M, Bertoni AG, Schreiner PJ, Diez Roux AV, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299:2751–2759. doi: 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Serretti A, Mandelli L. Antidepressants and body weight: A comprehensive review and meta-analysis. J Clin Psychiatry. 2010;71:1259–1272. doi: 10.4088/JCP.09r05346blu. [DOI] [PubMed] [Google Scholar]
- 45.Dutko P, Ploeg MV, Farrigan T. U.S. Department of Agriculture, Economic Research Service; Aug, 2012. Characteristics and influential factors of food deserts, ERR-140. [Google Scholar]