Abstract
Objective The present study examined the effect of child gender and maternal depressive symptoms on routine supervisory practices of mothers longitudinally. Method Self-report supervision practices were obtained at various time points from 3 months through 3 years of age. Results From 3 to 36 months, the quantity of time mothers reported supervising decreased from 7.1 to 6.3 hours, and the proportion of time spent in an intense style decreased from 63 to 46%, whereas that spent in a peripheral style increased from 14 to 32%. Mothers reported more time supervising girls and a greater proportion of this was in an intense style. Mothers with elevated depressive symptoms reported more time supervising but a lower proportion in an intense style. Conclusion Over the first 36 months of life, routine patterns of supervision change and these vary as a function of maternal depression symptoms and child gender. Implications for child injury risk are discussed.
Keywords: child development, child gender, maternal depression, supervision
Unintentional injury is a leading cause of child mortality in most developed nations, including the United States (Morrongiello, Midgett, & Stanton, 2000; World Health Organization [WHO], 2008). For children <6 years of age, the home is the primary location of injury, accounting for >13 million visits to physician offices and >4 million emergency visits annually in the United States (Phelan, Khoury, Kalkwarf, & Lanphear, 2005). Residential injuries are the result of a complex interplay of physical hazards, child behavior and developmental status, and parental characteristics and safety practices (see Morrongiello, 2005; Schwebel & Gaines, 2007 for extensive discussion). Preventing injury to young children requires eliminating exposure to hazardous objects or situations, until they learn how to interact safely with their environment. Past research has shown that parents teach, and children typically begin to learn, simple home safety rules by 3 years of age (Garling & Garling, 1995; Gralinski & Kopp, 1993). Before 3 years, parental supervision and the physical environment of the home can have profound effects on a child’s risk of injury (Morrongiello, Midgett, & Shields, 2001; Morrongiello, Ondejko, & Littlejohn, 2004a,b; van Aken, Junger, Verhoeven, van Aken, & Dkovic, 2007).
Young children, who are developmentally unable to recognize and negotiate residential hazards, must be provided appropriate and effective supervision by an able caregiver to prevent injury (Peterson, Ewigman, & Kivlahan, 1993). Supervision, potentially one of the most powerful ways to reduce childhood injury, has only recently been studied in a systematic way (Morrongiello, 2005; Petrass, Blitvich, & Finch, 2009). Wills and colleagues were among the first researchers to define supervision and they did so via a taxonomy that mentioned a caregiver who was older than the child and had some responsibility for and ability to interact with the child in a timely manner (Wills et al., 1997). Building on these ideas, Saluja et al. (2004) proposed a theoretical model that identified three relevant dimensions to supervision: attention, proximity, and continuity. Attention is defined based on the extent of engaged interaction and includes listening and watching behaviors; proximity is defined based on the distance between parent and child and is typically divided based on readiness to intervene into “within reach” (i.e., able to intervene in seconds) or “beyond reach” (e.g., different part of home) categories; and continuity is judged as continuous, intermittent, or absent and is applied to describe attention and proximity. According to this model, then, caregivers who are within reach and watching their child continuously are providing a greater level of supervision than those beyond reach and watching only intermittently.
Not surprisingly, level of supervision has been shown to relate to children’s likelihood of experiencing injury. For example, in one study examining injury mortality for children in two U.S. states, inadequate or absent supervision was implicated in more than 40% of death certificates (Landen, Bauer, & Kohn, 2003). In a matched case–control design, Morrongiello, Corbett, and Brison (2009) showed that parents of injured children presenting to emergency departments reported significantly lower levels of supervision (e.g., not watching as often, greater distance from child) than parents of uninjured children of the same age and sex who were engaging in the same activity that had led to the injury. Interestingly, although the pattern of these findings suggests that lapses in caregiver supervision contribute to elevate children’s risk of injury, it is interesting to note that studies of routine levels of supervision suggest that it is not uncommon for young children to be out of view of their caregivers when at home. In fact, during the course of a typical day at home 2–3-year-olds have been found to be out of view of caregivers about 20% of their awake time (Morrongiello, Corbett, McCourt, & Johnston, 2006a,b). Moreover, it seems that supervision becomes less intense as children age, with 4–5-year-olds out of view of caregivers significantly more often than are 2–3-year-olds.
Notably lacking in previous research on supervision is information on the nature and extent of supervision provided to children <2 years of age. Moreover, most studies are cross-sectional in design. The lack of any longitudinal research on routine levels of supervision limits our understanding of how this important parent safety practice changes as children develop. The current study was implemented to address these substantive research gaps and involved tracking the level of supervision parents provided to children from 3 through 36 months of age. Additionally, two factors that have been shown to influence children’s risk of injury and received limited attention in the supervision literature were considered, namely, maternal depression and child gender. Children living with parents experiencing heightened symptoms of depression have been shown to experience more injuries; however, how it is that depression elevates children’s risk of injury has not been determined (Phelan, Khoury, Atherton, & Kahn, 2007; Schwebel & Brezausek, 2008). In the current study, relations between depressive symptoms and supervision patterns were examined. Whether supervision varies for boys and girls as they develop also was assessed in the current study. The few studies that have examined parental supervision of young boys and girls were cross-sectional and limited in scope, although in both, the pattern of results suggested that when there is a difference, it is that girls receive more active supervision than boys (Morrongiello & Dawber, 1998; Morrongiello et al., 2006a). The use of a longitudinal design in this study provided a unique opportunity to more fully examine if boys and girls are differentially supervised by parents as they develop during the first few years of life.
Present Study Overview
The purpose of this study was to examine maternal self-reported supervisory behaviors as a function of child gender and maternal depressive symptoms, with the focus limited to the first 3 years of life, when the rate of childhood injury is highest and before children adopt many parental safety messages (Morrongiello et al., 2001). The sample was participating in the Health Outcomes and Measure of the Environment (HOME) study (Phelan et al., 2011), which was designed as a randomized trial to assess the efficacy of the installation of passive devices (e.g., smoke detectors) in households with young children from birth to 36 months of age (described further under Participants). Mothers completed quarterly phone surveys that included questions about the child’s time of exposure to the indoor environment and maternal supervisory behavior, in the first year of the study and then bi-annually thereafter. Specifically, the 15-min survey progresses through questions on exposure to the indoor environment (total time indoor awake and asleep) and the quantity (hours awake and in home with the child) and quality (i.e., attention, proximity, continuity) of maternal supervisory behavior. Mothers also completed the Beck Depression Inventory (BDI) at baseline and at annual visits. At baseline, the HOME study cohort consisted of 389 women who consented and gave birth to live singleton infants. The current analyses are based on data from 330 (83% of original cohort) women who completed two or more telephone interviews and the BDI measures (at home visits) during the 36-month follow-up period.
Method
Participants
Study details and recruitment have been described in detail previously (Phelan et al., 2011). Briefly, expectant mothers who attended seven participating obstetrical practices were screened for eligibility; mothers had to be at least 18 years of age and at no more than 19 weeks’ gestation. They had to live in a home built before 1978, but not live in public housing or a shelter, and have no plans for relocation within the next 12 months. There were 1,263 eligible of 8,878 new obstetrical patients at participating centers over the 3 years of recruitment.
Of the 468 women enrolled in the HOME study, 389 delivered live singleton babies; 330 mothers completed at least two phone surveys and at least two home visits during the 36-month follow-up period. About one-quarter of these families had public or Medicaid insurance; the majority had private insurance (Table I). The mean (standard deviation) age of the mothers at study entry was 30 (5.7) years. The median income for the cohort was $70,000 annually; about a quarter of families made <$30,000. Thus, this sample comprised a good mix of low-, middle-, and upper-income families.
Table I.
Demographic Characteristics of Mother–Child Participants (N = 330) in the HOME Study.
| Frequency (n) | Percent | |
|---|---|---|
| Child gender | ||
| M | 148 | 44.8 |
| F | 182 | 55.2 |
| Maternal race | ||
| White, non-Hispanic | 218 | 66.1 |
| Black, non-Hispanic | 91 | 27.6 |
| Other | 21 | 6.4 |
| Number of siblings | ||
| 0 | 180 | 54.5 |
| 1 | 117 | 35.5 |
| ≥2 | 33 | 10 |
| Total household income | ||
| <$30,000 | 89 | 27 |
| $30,000–49,999 | 56 | 17 |
| $50,000–69,999 | 54 | 16.4 |
| $70,000-89,999 | 72 | 21.8 |
| $90,000–119,999 | 27 | 8.2 |
| ≥$120,000 | 32 | 9.7 |
| Insurance status | ||
| Private | 249 | 75.5 |
| Medicaid | 81 | 24.5 |
| Maternal education | ||
| ≤High school | 69 | 20.9 |
| <College | 81 | 24.5 |
| College graduate/postgraduate | 180 | 54.5 |
| Maternal depression (BDI >13) | ||
| Baseline | 64 | 19 |
| 12-month | 42 | 13 |
| 24-month | 34 | 13 |
| 36-month | 33 | 13 |
Maternal Supervisory Behaviors
Quantity
During the telephone interview, the research assistants worked through a computerized script with direct data entry. The questions progressed through ones about the time spent in the indoor environment, maternal supervisory behavior (quantity and quality), and, finally, any injury events. The script prompted the research assistants to ask mothers to recall the total time (asleep and awake) spent in the indoor environment and the amount of time awake and indoor with their child for one typical weekday and one typical weekend day during the previous week. A mother who spent more than 3 weekdays away from home during a typical week was asked to recall the quantity and quality of supervisory behavior in the home on the last typical weekday when she worked or attended school. Similarly, for a weekend day, a mother who worked or attended school for more than 1 weekend day was asked to recall how her time was spent supervising her child on the last typical weekend day. If an enrolled mother spent less than half her time working or attending school for a weekend or weekday, then she was asked to recall the last typical day in which she did not work or attend school. The total quantity of hours spent in the home and the total hours awake and supervising the child were calculated, recorded, and confirmed with the mother during the interview. The weighted daily (24-hr period) average hours spent in supervision were calculated; weekday was 5 of 7 and weekend day 2 of 7 of the average.
Quality
Drawing on measures developed previously (Morrongiello et al., 2004a, 2006a), mothers were asked during phone interviews to describe the quality of supervisory behavior while in the home with their children. We defined the quality of supervision as intense, intermittent, or peripheral according to the degree of attention and continuity of her time with the infant. Mothers who reported continuous direct interaction, either touching their infant or could easily do so in 1 or 2 s, were categorized as “intense” supervisors. Those who reported either watching or listening for their infant from a close distance in the same or a nearby room but who could easily get to their infant in a matter of seconds or more were classified as “intermittent” supervisors. Finally, those mothers who reported nonvisual auditory or “listening for” noises from their infants in a nonadjacent room or another part of the home and who could not reach the child easily in seconds if needed were classified as “peripheral” supervisors. For analysis, the proportion of the total reported time awake and indoors that was spent supervising a child in a given style was used to model the quality of maternal supervision.
Covariates and Modifiers
Data were also collected on maternal sociodemographics, including age, number and gender of children in household younger than 6 years, the highest level of maternal education, annual income, and type of health insurance. We examined the maternal depressive symptom scores elicited using the BDI (BDI-II) at baseline and at 12-, 24-, and 36-month postpartum home visits. The BDI-II consists of 21 items that assess attitudes and symptoms that are specific to 21 signs of depression. Response options for each item range from 0 to 3, reflecting increasing degrees of severity. The BDI-II required about 10 min to complete during a home visit (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961; Lasa, Ayuso-Mateos, Vazquez-Barquero, Diez-Manrique, & Dowrick, 2000; Richter, Werner, Heerlein, Kraus, & Sauer, 1998). BDI scores greater than 13 are considered clinically significant depressive symptoms (Beck et al., 1961; Kim-Cohen, Moffitt, Taylor, Pawlby, & Caspi, 2005; Lasa et al., 2000). In addition, we analyzed the effect on supervision models of mothers who scored in a clinically significant range at any time point.
Statistical Analytic Approach
The weighted number of hours the mother reported supervising her child while awake and in the indoor environment was calculated. In addition, the number of hours spent in intense, intermittent, or peripheral supervisory styles was calculated in the same way, and from these, the percent of supervisory time spent in each style was also calculated. Measures of maternal supervisory behavior were obtained at four time points in the first year of follow-up and at two time points in each of the second and the third year of follow-up.
In the context of community-based trials, it is not possible to complete home visits and measurements of maternal psychology, child behavior, and the built environment at time points coinciding exactly with 12, 24, and 36 months post enrollment or randomization. Therefore, we completed instruments within approximately a 4-week “window” of these annual time points either 2 weeks before or 2 weeks after a chronologic follow-up time point. As instruments such as the BDI query a subject on feelings up to 2 weeks prior (and others more distant), this did not introduce any appreciable bias into this assessment. Indeed, it is likely that maternal depressive symptoms varied within and between participants over time. Scores on the BDI were analyzed in models as continuous variables. In addition, we examined the effect of groups of participants with clinically significant elevations in depressive symptoms (BDI >13) at any given time point on reported supervisory behavior. In our modeling, generalized linear mixed models were used to account for the accrual of data over time and intermittently missing data points.
A generalized linear mixed model, assuming a first-order autoregressive covariance structure, was used for analysis of supervisory behavior over time. The initial approach was to examine the interaction of either child gender or BDI and visit. If the interaction was not significant, the main effects model was examined to look at the independent effect of child gender or maternal depression. Again the generalized linear mixed model was used. Covariates included maternal sociodemographics: age, number of children in the household younger than 6 years, the highest level of maternal education, annual income, and type of health insurance. The randomized group assignment was included in all models irrespective of statistical significance; it should be noted, however, that inclusion of the group assignment covariate did not significantly affect conclusions drawn from the models and reported in this article, as there was no effect of the child-proofing intervention and presence of safety devices on maternal supervisory behavior.
Results
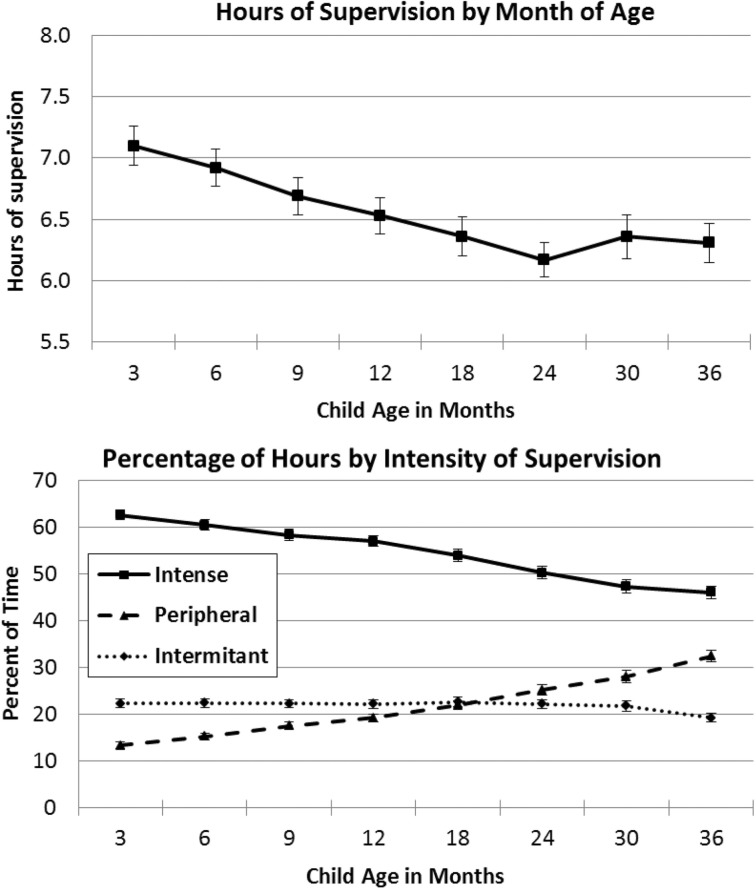
Mothers reported an average of 17.4 (standard deviation = 4.1) hours in the indoor environment (both awake and asleep). Participating mothers reported spending 7.1 (95% confidence interval 6.8–7.4) hours, on average, daily in the home environment, awake and supervising their 3-month-old child. By 36 months, this decreased to 6.3 (95% confidence interval 6.0–6.6) hours daily (p = .006). During this same period, the proportion of time spent in intense supervision decreased from 63% of total supervision time at 3 months to 46% at 36 months (p < .0001). Similarly, as shown in Figure 1, the proportion of time spent in peripheral supervision significantly increased from 14% at 3 months to 32% at 36 months (p < .0001).
Figure 1.
Total hours of self-reported supervision in the home and percent of time in intense, intermittent, or peripheral styles as a function of age of the child (months).
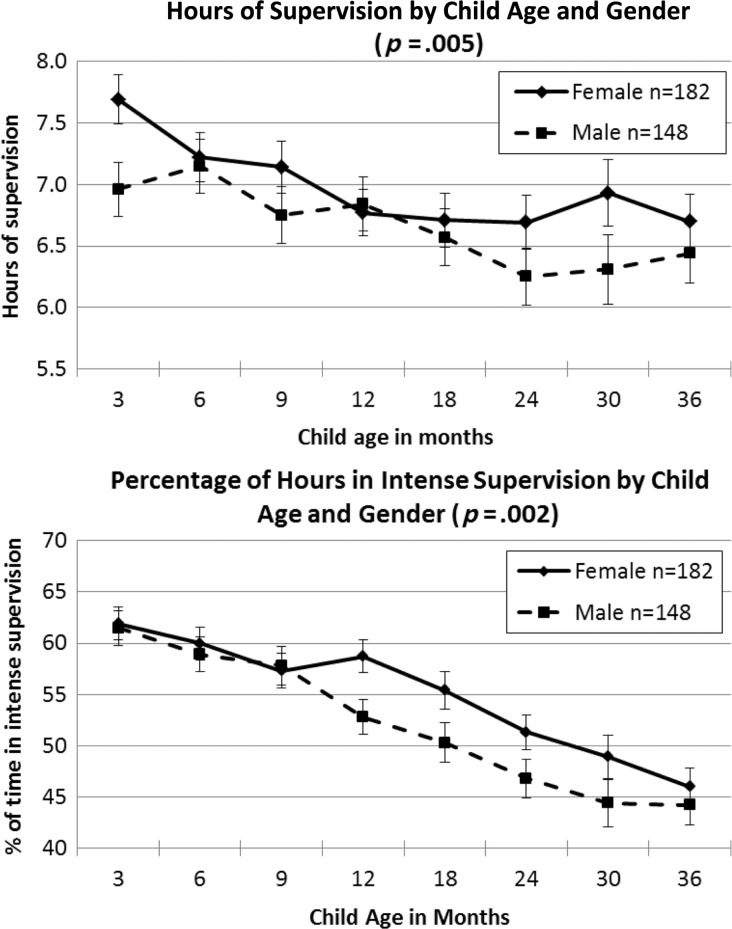
As shown in Figure 2, mothers reported spending significantly greater amounts of time supervising girls (p = .005), and a greater proportion of this time was spent in intense supervision (p = .002), compared with mothers supervising boys. In contrast, the proportion of peripheral supervision time was significantly higher for boys compared with girls (p = .03). Thus, girls generally received more active supervision than boys.
Figure 2.
Self-reported hours of supervision and proportion of hours in intense style during the first 36 months of life as a function of child gender.
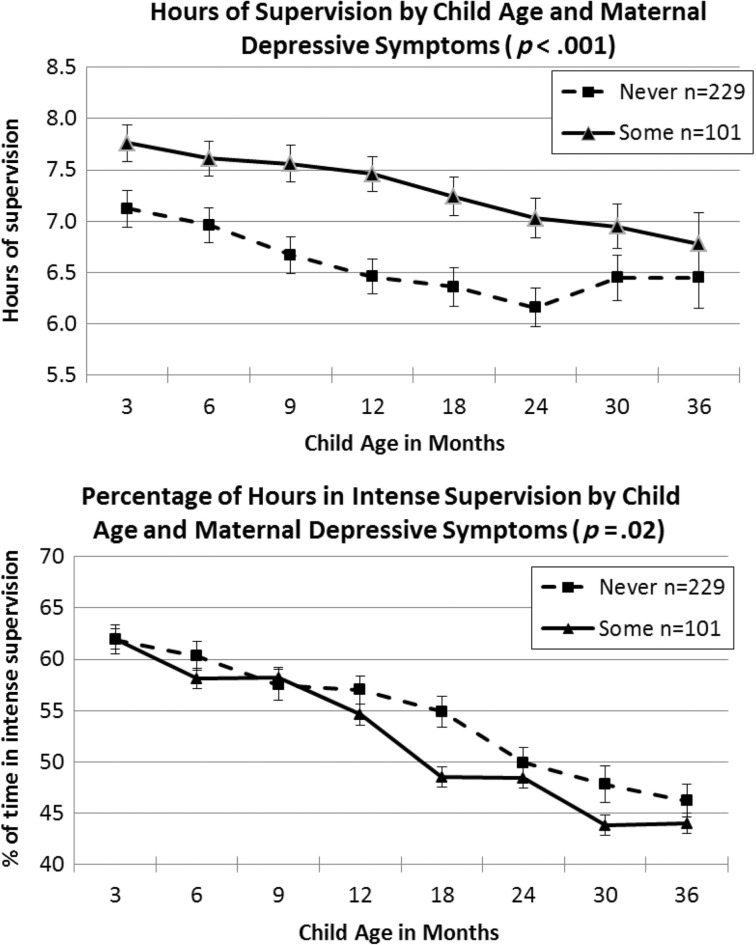
As shown in Figure 3, mothers who scored in the moderate-to-severe range on the BDI, >13 at any time point, reported spending significantly more time supervising their children (p < .0001). However, mothers who had higher depressive symptoms spent a lower proportion of this supervisory time in intense supervision (p = .02) compared with mothers who never had BDI symptom scores >13. Although the proportion of peripheral supervision generally increased significantly from 3 to 36 months (Figure 1), the proportion of time spent in peripheral supervision did not differ statistically significantly between mothers who had ever reported moderate-to-severe depressive symptoms and those who never did (p = .13).
Figure 3.
Self-reported hours of supervision and proportion in intense style during the first 36 months of life as a function of maternal depressive symptoms (BDI >13).
Discussion
Supervision is an important determinant of injury risk for young children, yet little is known about how maternal supervisory practices change as children develop in the first years of life. This longitudinal study of maternal supervisory behavior addresses this gap in knowledge. The results provide important insights into how this behavior changes over the first 36 months of childhood for boys and girls and maternal factors that influence this process.
Parents reported a mean of 7.1 hr of supervision in the first months of life in a typical day, and this decreased as the child aged through 36 months of follow-up. As supervision time decreased, there was also an important change in the pattern of supervision shown. Specifically, the proportion of time spent in an “intense” and active supervisory style decreased, whereas the proportion spent in a “peripheral” style increased. This pattern is surprising, given that infants would be acquiring greater motor skills during this time frame and one might expect, therefore, that caregivers would provide more intense supervision to moderate the child’s increasing ability to reach and interact with more hazards. Past research has found that parents do not routinely think about injury risk and are optimistically biased to assume they can keep young children safe (Morrongiello & Dayler, 1996). Hence, it might be that caregivers do not recognize that increasing mobility equates to greater injury risk. Consistent with this interpretation is evidence of spikes in injury rates when young children first acquire a new motor development milestone that parents have not anticipated (Agran et al., 2003). Alternatively, it might be that caregivers recognize infants are at risk of being injured but they attribute injuries that occur to fate or representative of typical childhood events that cannot be prevented and, therefore, they do not maintain an intense supervisory style as children become more active and mobile (Morrongiello & Kiriakou, 2004; Peterson, Farmer, & Kashani, 1990). Falls, for example, occur often during early childhood and caregivers assume they are normative and not preventable (Morrongiello & Kiriakou, 2004), apparently unaware of the frequency with which these are seriousness health events (Khambalia et al., 2006). Suffice it to say, the current results indicate that not only is supervision declining as children age, but the pattern shifts from comprising watchful/proximal behaviors to more distal/peripheral ones even though children are becoming increasingly mobile and having greater potential to interact with injury hazards.
Interestingly, child gender influenced supervision, with girls receiving closer supervision than boys. Mothers of girls reported not only significantly greater supervision time but that a greater proportion of this time reflected an intense (watchful, proximal) style, whereas boys received more peripheral supervision and less time being supervised. In a previous prospective study of minor home injuries, Morrongiello obtained maternal reports of supervisory patterns at the time of injury and developed a taxonomy of supervisory practices. Results revealed that these various levels of supervision systematically related to frequency of injury differentially for boys and girls. Specifically, watching continuously was associated with the lowest frequency of injury and not supervising was associated with the highest frequency of injuries, and these relations applied for both boys and girls. However, intermittently checking on the child was associated with relatively infrequent injuries for girls but high rates of injuries for boys (Morrongiello et al., 2004a,b) The pattern of findings suggested that boys required more frequent and effortful supervisory strategies than girls to ensure their safety, and other studies using different methods support the same conclusions (Morrongiello & Dawber, 1998, 2000; Morrongiello & Rennie, 1998). The current findings suggest that caregivers are more motivated to closely supervise girls than boys. This mismatch between the level of supervision that boys need to secure their safety and that is provided routinely by caregivers may explain why boys experience more frequent and severe injuries than girls (WHO, 2008). Although the nature of our data does not allow us to definitively explain why caregivers show differential supervision patterns for boys and girls, this finding may relate to the fact that caregivers seem to believe they can have greater impact to change girls’ than boys’ behaviors (Morrongiello & Hogg, 2004; Morrongiello, Zdzieborski, & Normand, 2010). Certainly, exploring the basis for the current gender differences in supervision merits attention in future research so that prevention messaging can address this issue and encourage caregivers to provide the intense level of supervision that boys seem to need to prevent injuries.
Interestingly, mothers with higher maternal depressive symptoms reported significantly greater total amounts of time spent supervising their children, but a smaller proportion of this time was in an “intense” style compared with mothers with lower depressive symptoms. This is an important finding because it suggests one possible explanation for why caregiver depression is associated with greater frequency of child injury (Phelan et al., 2007), namely, if caregivers are not closely supervising, this can create opportunities for children to engage with hazards. To the extent that providing intense supervision taxes attention and can be physically demanding (e.g., staying proximal to child), maintaining this supervision style may be beyond the capabilities of caregivers who are experiencing depression (e.g., tired, not able to sustain focused attention). Nonetheless, these caregivers may believe they are doing all they can to keep their child safe (i.e., spending more time supervising than even nondepressed parents) but may not realize the ineffective nature of their practices (i.e., children need intense supervision for safety). The current findings suggest that interventions aimed at improving supervision by these caregivers will need to target the nature of their supervision practices, more so than the extent to which they supervise.
Conclusions
Not surprisingly, the amount and type of maternal supervision changed over the first 36 months of children’s lives, with “intense” (watchful, proximal) supervision decreasing significantly over the course of early childhood and “peripheral” supervision increasing. Generally, girls received more supervision and greater intense supervision than boys, and mothers who reported high depressive symptoms during this period showed less intense supervision of their children. Extending these findings to determine the implications of these changes in supervision for children’s rate of injury is a necessary next step in this research.
Funding
Canada Research Chair in Child & Youth Injury Prevention (to B.A.M.); 1 R01 HD066115-01A1 from the Eunice Kennedy Shriver National Institute of Child Health and Development (NICHD) and an interagency agreement with the U.S. Department of Housing & Urban Development (to K.J.P.); U.S. Environmental Protection Agency (PO1-ES11261) and the National Institutes for Environmental Health Sciences (R01ES014575) (to B.L.).
Conflicts of interest: None declared.
References
- Agran P, Anderson C, Winn D, Trent R, Walton-Haynes L, Thayer S. Rates of pediatric injuries by 3-month intervals for children 0 to 3 years of age. Pediatrics. 2003;111:683–692. doi: 10.1542/peds.111.6.e683. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Garling A, Garling T. Mothers’ anticipation and prevention of unintentional injury to young children in the home. Journal of Pediatric Psychology. 1995;20:23–36. doi: 10.1093/jpepsy/20.1.23. [DOI] [PubMed] [Google Scholar]
- Gralinski J H, Kopp C B. Everyday rules for behavior: Mothers’ requests to young children. Developmental Psychology. 1993;29:573–584. [Google Scholar]
- Khambalia A, Joshi P, Brussoni M, Raina P, Morrongiello B, Macarthur C. Risk factors for unintentional injuries due to falls in children aged 0-6 years: A systematic review. Injury Prevention. 2006;12:378–385. doi: 10.1136/ip.2006.012161. doi:10.1136/ip.2006.012161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J, Moffitt T E, Taylor A, Pawlby S J, Caspi A. Maternal depression and children's antisocial behavior. Archives of General Psychiatry. 2005;62:173–181. doi: 10.1001/archpsyc.62.2.173. [DOI] [PubMed] [Google Scholar]
- Landen M G, Bauer U, Kohn M. Inadequate supervision as a cause of injury deaths among young children in Alaska and Louisiana. Pediatrics. 2003;111:328–331. doi: 10.1542/peds.111.2.328. [DOI] [PubMed] [Google Scholar]
- Lasa L, Ayuso-Mateos J L, Vazquez-Barquero J L, Diez-Manrique F J, Dowrick C F. The use of the Beck Depression Inventory to screen for depression in the general population: A preliminary analysis. Journal of Affective Disorders. 2000;57:261–265. doi: 10.1016/s0165-0327(99)00088-9. [DOI] [PubMed] [Google Scholar]
- Morrongiello B A. Caregiver supervision and child-injury risk: I. Issues in defining and measuring supervision; II. Findings and directions for future research. Journal of Pediatric Psychology. 2005;30:536–552. doi: 10.1093/jpepsy/jsi041. doi:jsi041 [pii]10.1093/jpepsy/jsi041. [DOI] [PubMed] [Google Scholar]
- Morrongiello B, Corbett M, Brison R J. Identifying predictors of medically-attended injuries to young children: Do child or parent behavioral attributes matter? Injury Prevention. 2009;15:220–225. doi: 10.1136/ip.2008.019976. [DOI] [PubMed] [Google Scholar]
- Morrongiello B A, Corbett M, McCourt M, Johnston N. Understanding unintentional injury risk in young children I. The nature and scope of caregiver supervision of children at home. Journal of Pediatric Psychology. 2006a;31:529–539. doi: 10.1093/jpepsy/jsj045. doi:jsj073 [pii]10.1093/jpepsy/jsj045. [DOI] [PubMed] [Google Scholar]
- Morrongiello B A, Corbett M, McCourt M, Johnston N. Understanding unintentional injury risk in young children II. The contribution of caregiver supervision, child attributes, and parent attributes. Journal of Pediatric Psychology. 2006b;31:540–551. doi: 10.1093/jpepsy/jsj073. doi:jsj073 [pii]10.1093/jpepsy/jsj073. [DOI] [PubMed] [Google Scholar]
- Morrongiello B A, Dawber T. Toddlers' and mothers' behaviors in an injury-risk situation: Implications for sex differences in childhood injuries. Journal of Applied Developmental Psychology. 1998;19:625–639. [Google Scholar]
- Morrongiello B A, Dawber T. Mothers' responses to sons and daughters engaging in injury-risk behaviors on a playground: implications for sex differences in injury rates. Journal of Experimental Child Psychology. 2000;76:89–103. doi: 10.1006/jecp.2000.2572. doi:10.1006/jecp.2000.2572S0022-0965(00) 92572-4 [pii] [DOI] [PubMed] [Google Scholar]
- Morrongiello B A, Dayler L A. A community-based study of parents’ knowledge, attitudes, and beliefs related to childhood injuries. Canadian Journal of Public Health. 1996;87:383–388. [PubMed] [Google Scholar]
- Morrongiello B A, Hogg K. Mothers' reactions to children misbehaving in ways that can lead to injury: Implications for gender differences in children risk taking and injuries. Sex Roles. 2004;50:103–118. doi:0360-0025/04/0100-0103/0. [Google Scholar]
- Morrongiello B A, Kiriakou S. Mothers’ home safety practices for preventing six types of childhood injuries: What do they do, and why? Journal of Pediatric Psychology. 2004;29:285–297. doi: 10.1093/jpepsy/jsh030. doi:10.1093/jpepsy/jsh030. [DOI] [PubMed] [Google Scholar]
- Morrongiello B A, Midgett C, Shields E. Don't run with scissors: Young children's knowledge of home safety rules. Journal of Pediatric Psychology. 2001;26:105–115. doi: 10.1093/jpepsy/26.2.105. [DOI] [PubMed] [Google Scholar]
- Morrongiello B A, Midgett C, Stanton K L. Gender biases in children's appraisals of injury risk and other children's risk-taking behaviors. Journal of Experimental Child Psychology. 2000;77:317–336. doi: 10.1006/jecp.2000.2595. doi:10.1006/jecp.2000.2595S0022-0965(00)92595-5 [pii] [DOI] [PubMed] [Google Scholar]
- Morrongiello B A, Ondejko L, Littlejohn A. Understanding toddlers' in-home injuries: I. Context, correlates, and determinants. Journal of Pediatric Psychology. 2004a;29:415–431. doi: 10.1093/jpepsy/jsh046. doi:10.1093/jpepsy/jsh04629/6/415 [pii] [DOI] [PubMed] [Google Scholar]
- Morrongiello B A, Ondejko L, Littlejohn A. Understanding toddlers' in-home injuries: II. Examining parental strategies, and their efficacy, for managing child injury risk. Journal of Pediatric Psychology. 2004b;29:433–446. doi: 10.1093/jpepsy/jsh047. doi:10.1093/jpepsy/jsh04729/6/433 [pii] [DOI] [PubMed] [Google Scholar]
- Morrongiello B A, Rennie H. Why do boys engage in more risk taking than girls? The role of attributions, beliefs, and risk appraisals. Journal of Pediatric Psychology. 1998;23:33–43. doi: 10.1093/jpepsy/23.1.33. [DOI] [PubMed] [Google Scholar]
- Morrongiello B A, Zdzieborski D, Norman J. Understanding gender differences in children’s risk taking and injury: A comparison of mothers’ and fathers’ reactions to sons and daughters misbehaving in ways that lead to injury. Journal of Applied Developmental Psychology. 2010;31:322–329. [Google Scholar]
- Peterson L, Ewigman B, Kivlahan C. Judgments regarding appropriate child supervision to prevent injury: The role of environmental risk and child age. Child Development. 1993;64:934–950. [PubMed] [Google Scholar]
- Peterson L, Farmer J, Kashani J H. Parental injury prevention endeavors: A function of health beliefs? Health Psychology. 1990;9:177–191. doi: 10.1037//0278-6133.9.2.177. doi:10.1037/0278-6133.9.2.177. [DOI] [PubMed] [Google Scholar]
- Petrass L, Blitvich J D, Finch C F. Parent/Caregiver supervision and child injury: A systematic review of critical dimensions for understanding this relationship. Family and Community Health. 2009;32:123–135. doi: 10.1097/FCH.0b013e3181994740. doi:10.1097/FCH.0b013e318199474000003727-200904000-00007 [pii] [DOI] [PubMed] [Google Scholar]
- Phelan K, Khoury J, Atherton H, Kahn R S. Maternal depression, child behavior, and injury. Injury Prevention. 2007;13:403–408. doi: 10.1136/ip.2006.014571. doi:13/6/403[pii]10.1136/ip.2006.014571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan K J, Khoury J, Kalkwarf H, Lanphear B. Residential injuries in U.S. children and adolescents. Public Health Reports. 2005;120:63–70. doi: 10.1177/003335490512000111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan K J, Khoury J, Xu Y, Liddy S, Hornung R, Lanphear B P. A randomized controlled trial of home injury hazard reduction: The HOME injury study. Archives of Pediatrics and Adolescent Medicine. 2011;165:339–345. doi: 10.1001/archpediatrics.2011.29. doi:10.1001/archpediatrics.2011.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter P, Werner J, Heerlein A, Kraus A, Sauer H. On the validity of the Beck Depression Inventory: A review. Psychopathology. 1998;31:160–168. doi: 10.1159/000066239. [DOI] [PubMed] [Google Scholar]
- Saluja G, Brenner R A, Morrongiello B A, Haynie D, Rivera M, Cheng T L. The role of supervision in child injury risk: Definition, conceptual and measurement issues. Injury Control and Safety Promotion. 2004;11:17–22. doi: 10.1076/icsp.11.1.17.26310. [DOI] [PubMed] [Google Scholar]
- Schwebel D C, Brezausek C M. Chronic maternal depression and children's injury risk. Journal of Pediatric Psychology. 2008;33:1108–1116. doi: 10.1093/jpepsy/jsn046. doi:jsn046[pii]10.1093/jpepsy/jsn046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwebel D, Gaines J. Pediatric unintentional injury: Behavioral risk factors and implications for prevention. Journal of Developmental and Behavioral Pediatrics. 2007;28:245–254. doi: 10.1097/01.DBP.0000268561.80204.2a. [DOI] [PubMed] [Google Scholar]
- van Aken C, Junger M, Verhoeven M, van Aken M A G, Dkovic M. Externalizing behaviors and minor unintentional injuries in toddlers: common risk factors? Journal of Pediatric Psychology. 2007;32:230–244. doi: 10.1093/jpepsy/jsj118. [DOI] [PubMed] [Google Scholar]
- Wills K A, Tanz R R, Christoffel K K, Schofer J L, Lavigne J V, Donovan M, Kalangis K. Supervision in childhood injury cases: A reliable taxonomy. Accident Analysis & Prevention. 1997;29:133–137. doi: 10.1016/s0001-4575(96)00057-7. [DOI] [PubMed] [Google Scholar]
- World Health Organization. World Report on Child Injury Prevention. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]