Abstract
Aneurysm of the cystic artery is not common, and it is a rare cause of hemobilia. Most of reported cases are pseudoaneurysms resulting from either an inflammatory process in the abdomen or abdominal trauma. We report a healthy individual who developed hemobilia associated with cystic artery aneurysm. The patient was managed with cholecystectomy and concomitant aneurysm repair. Visceral artery aneurysms are rare and can rupture with potentially grave outcome due to excessive bleeding. Angiographic embolization is a common method of treatment for visceral artery aneurysms. Open cholecystectomy and aneurysm repair was performed in our patient due to radiological evidence of associated cholecystitis.
Keywords: Aneurysm, embolization, cholecystectomy
Introduction
Aneurysmal disease of visceral arteries is uncommon, and it usually involves branches of the hepatic and gastro-duodenal arteries [1]. We report a patient with severe hematemesis and abdominal pain due to hemobilia, caused by cystic artery aneurysm.
Case report
A 35-year-old male patient presented with severe hematemesis and upper right quadrant abdominal pain. He had a history of recurrent vague abdominal pain and melena for the last 3 months and was treated symptomatically at a local hospital. He did not undergo any surgeries or diagnostic
procedures. He had a known history of hypertension, a family history of hypertension, and was under amlodipine. He had no history of smoking, alcohol consumption, or drug abuse. On admission, the patient was afebrile and non-icteric. His blood pressure was 110/60 mmHg, respiratory rate was 20/min, and pulse rate was 100 bpm. Physical examination revealed a well-nourished and oriented young man. The upper right quadrant appeared full and tender to palpation but without rebound tenderness. Rectal examination showed fresh blood. The remainder of the physical examination was normal. Laboratory investigation revealed an elevated white blood cell count of 20×103/μL, hemoglobin of 8.5 g/dL and platelet count of 22 7×103/μL. Blood chemistry showed SGOT:149 U/L (0-37), SGPT:203U/L (0-40), Bilirubin total/conjugated:1.27/0.52 (units?), GGT:872 U/L, total protein/albumin:5.70/3.10 g/dL. Upper GI endoscopy revealed blood was likely to be coming out from pylorus. CT scan revealed markedly distended gallbladder lumen filled with high Hounsfield Unit (H.U.) (60-70) content suggestive of blood along with a 20 mm x 16 mm in size, well-defined, intensely enhanced lesion arising from the wall of the body of the gallbladder and very likely representing vascular pathology [Fig. 1]. MR angiography revealed a 21×17 mm sized aneurysm arising from the terminal end of the cystic artery with a secondary bleeding within gallbladder lumen [Fig. 2,3].
Figure 1.

CT Scan: Demonstration of gallbladder filled with blood and aneurysm
Figure 2.
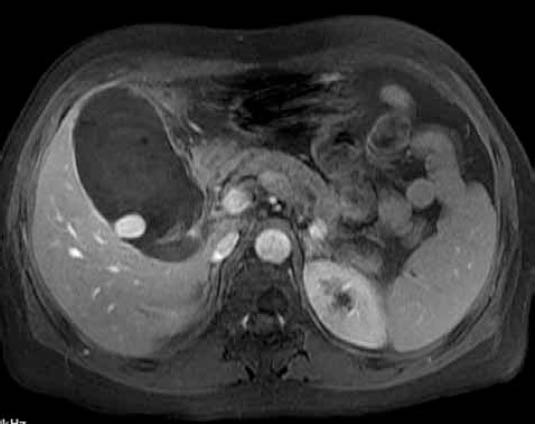
Contrast enhanced MRI: Demonstration of features of cholecystitis with aneurysm
Figure 3.

MR Angiography: Demonstration of aneurysm arising from cystic artery
The patient was referred for surgery due to radiological findings of associated cholecystitis. He underwent open cholecystectomy and aneurysm repair. Intraoperatively the gallbladder was hugely distended and there was dense adhesion surrounding the gallbladder and the Callot’s triangle anatomy was distorted. Gallbladder was opened on fundus and blood clots were drained [Fig. 4]. There was active spurt from the body of the gallbladder following removal of clot-like material which was controlled using 4’0 synthetic, monofilament, nonabsorbable polypropylene suture. Cholecystectomy was then performed following dissection of Callot’s triangle and individually ligating the cystic artery and duct. The condition of the patient remained clinically stable and subsequent follow-up showed normal hemoglobin levels. Histopathological examination revealed chronic cholecystitits. The patient was discharged after 7 days with a plan for outpatient follow-up.
Figure 4.
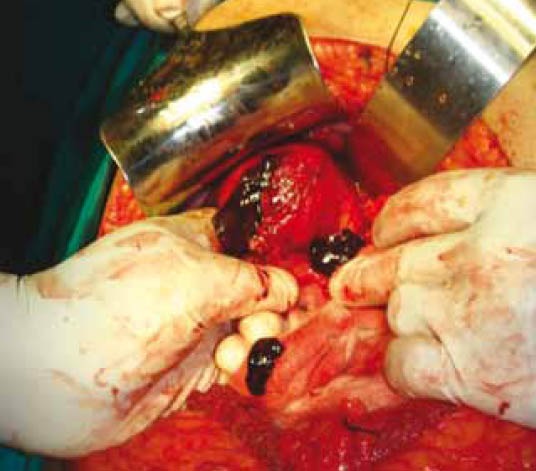
Surgical photographs: Demonstration of blood clots coming out after opening fundus of the gallbladder
Discussion
Cystic artery aneurysm is a rare disease, such that an extensive search identified only 27 published cases. Most of these cases are pseudoaneurysms. Pseudoaneurysms are differentiated from true aneurysms by the presence of a known cause such as trauma or inflammation, and by radiologic findings of aneurysmal dilatation in the setting of otherwise normal artery. Causes of cystic artery aneurysms include abdominal trauma and intra-abdominal inflammatory processes such as cholecystitis or pancreatitis [1]. The etiology of aneurysm in our patient is unknown. There was no history of trauma or any invasive procedures performed. Radiological evaluation revealed no evidence of pancreatitis and gallstones.
Cystic artery aneurysm usually manifests itself with hemobilia, hematemesis and/or melena [3-5]. First described in 1654 by Francis Glisson, hemobilia commonly presents as an upper gastrointestinal hemorrhage [6,7]. Causes of hemobilia can be traumatic and non-traumatic. The most common traumatic cause in Western countries is liver trauma, followed by iatrogenic injury during diagnostic and therapeutic hepatobiliary procedures [6]. Non-traumatic causes include cholecystitis and pancreatitis [8, 9]. Hemobilia is classically associated with Quincke’s clinical triad of colicky abdominal pain, jaundice and gastrointestinal hemorrhage [5]. Because of the rarity of this disease, there is no consensus on the clinical management or operative treatment of cystic artery aneurysms. While cholecystectomy is considered as the definitive treatment in most cases, arterial embolization has also been used effectively to treat visceral artery aneurysms including cystic artery aneurysms. Cholecystectomy may specifically be considered if (necrotizing) cholecystitis is suspected. In the past there was a concern that embolization of the cystic artery would cause gallbladder necrosis, but recent publications fail to confirm this theory [9]. Arterial embolization has the advantages of reduced surgical morbidity and mortality compared to open or laparoscopic cholecystectomy. The angiographic treatment is not possible in all cases. Many of the reported cases had associated cholecystitis and were surgically managed with cholecystectomy with operative repair of aneurysm.
In conclusion, visceral artery aneurysms are rare and can rupture with potentially grave outcome due to excessive bleeding. Cross-sectional imaging usually demonstrates the pathological changes of the disease. Angiographic embolization is a common method of treatment for visceral artery aneurysms. In our case, surgery was considered as the treatment of choice, due to cholecystitis probably caused by blockage of cystic duct by clots.
Biography
Indira Gandhi Institute of Medical Sciences, Bihar Institute of Gastroenterology, India
Footnotes
Conflict of Interest: None
References
- 1.Baker KS, Tisnado J, Cho SR, Beachley MC. Splanchnic artery aneurysms and pseudoaneurysms: transcatheter embolization. Radiology. 1987;163:135–139. doi: 10.1148/radiology.163.1.3823426. [DOI] [PubMed] [Google Scholar]
- 2.Karazincir S, Ada E, Sarsilmaz A, et al. Frequency of vascular variations and anomalies accompanying intracranial aneurysms. Tani Girisim Radyol. 2004;10:103–109. [PubMed] [Google Scholar]
- 3.Kaman L, Kumar S, Behera A, Katariya RN. Pseudoaneurysm of the cystic artery: a rare cause ofhemobilia. Am J Gastroenterol. 1998;93:1535–1537. doi: 10.1111/j.1572-0241.1998.475_y.x. [DOI] [PubMed] [Google Scholar]
- 4.Gutierrez G, Ramia JM, Villar J, et al. Cystic artery pseudoaneurism from an evolved acute calculous cholecystitis. Am J Surg. 2004;187:519–520. doi: 10.1016/j.amjsurg.2003.12.033. [DOI] [PubMed] [Google Scholar]
- 5.Nakajima M, Hoshino H, Hayashi E, et al. Pseudoaneurysm of the cystic artery associated with upper gastrointestinal bleeding. J Gastroenterol. 1996;31:750–754. doi: 10.1007/BF02347630. [DOI] [PubMed] [Google Scholar]
- 6.Maeda A, Kunou T, Saeki S, et al. Pseudoaneurysm of the cystic artery with hemobilia treated by arterial embolization and elective cholecystectomy. J Hepatobiliary Pancreat Surg. 2002;9:755–758. doi: 10.1007/s005340200105. [DOI] [PubMed] [Google Scholar]
- 7.Green MH, Duell RM, Johnson CD, Jamieson NV. Haemobilia. Br J Surg. 2001;88:773–786. doi: 10.1046/j.1365-2168.2001.01756.x. [DOI] [PubMed] [Google Scholar]
- 8.England RE, Marsh PJ, Ashleigh R, Martin DF. Case report: pseudoaneurysm of the cystic artery: a rare cause of haemobilia. Clin Radiol. 1998;53:72–75. doi: 10.1016/s0009-9260(98)80041-x. [DOI] [PubMed] [Google Scholar]
- 9.Lee MJ, Saini S, Geller SC, Warshaw AL, Mueller PR. Pancreatitis with pseudoaneurysm formation: a pitfall for the interventional radiologist. Am J Roentgenol. 1991;156:97–98. doi: 10.2214/ajr.156.1.1898577. [DOI] [PubMed] [Google Scholar]
- 10.Jornod P, Wiesel PH, Pescatore P, Gonvers JJ. Hemobilia, a rare cause of acute pancreatitis after percutaneous liver biopsy: diagnosis and treatment by endoscopic retrograde cholangiopancreatography. Am J Gastroenterol. 1999;94:3051–3054. doi: 10.1111/j.1572-0241.1999.01460.x. [DOI] [PubMed] [Google Scholar]


