Abstract
In the past three decades, researchers have been attempting to replace the obsolete concept of homogeneity of alcohol dependence, by classifying these patients into specific heterogeneous subtypes. Based on 30 years of experience and research, the Lesch Typology has proved to be very useful in clinical daily routine. The aim of the Lesch Typology is to provide targeted subtype-specific treatments to patients, thereby increasing their probability of long-term abstinence and hence improving their prognosis.
The Lesch Typology is based on data from a longitudinal prospective study (with follow ups even 19 years later) on alcohol dependent patients (n=436). By observing the long term development of these patients, four distinct courses could be identified. In the meantime, a computerized version of the Lesch Typology had been created and translated into many languages, and is currently being employed in numerous psychiatric institutions while assisting clinicians in quickly determining a patient’s subtype (www.lat-online.at).
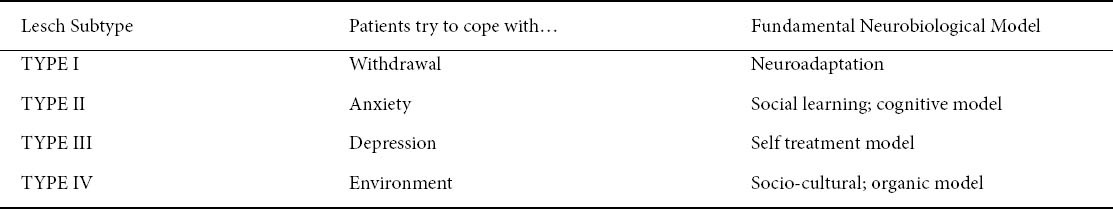
Based on the patients’ drinking patterns and origin of substance craving, hence according to the Lesch Typology, four subtypes of alcohol dependent patients can be distinguished: 1. the “allergy model” (craving caused by alcohol); 2. the “conflict resolution and anxiety model” (craving caused by stress); 3. the “depressive model” (craving caused by mood); and 4. the “conditioning model” (craving caused by compulsion).
Pharmacological treatments are not always the most effective way of preventing relapses in alcohol dependent patients. Many times, a combination with psychosocial as well as psychotherapeutic approaches is necessary and essential for helping patients to stay sober. Depending on the patient’s Lesch Type, certain therapeutic approaches are more appropriate and subsequently lead to better results and higher chances of lasting abstinence.
Keywords: Lesch typology, alcoholism, treatment, psychosocial
Introduction
Alcohol dependence (AD) is a common global disease affecting a large portion of the population worldwide. Demographic data in the United States shows that approximately 8.5% of Americans are alcohol dependent, while in Europe a similar frequency is assumed [1]. Apart from life threatening morbidities associated with chronic alcohol consumption (liver cirrhosis, gastrointestinal neoplasm, esophageal varices), AD also accounts for high social and economic burdens (unemployment, disability, invalidity) [2,3].
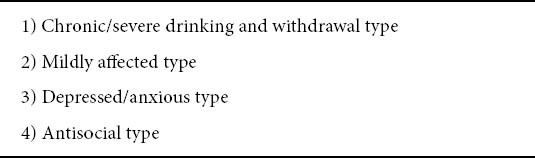
Alcohol dependence represents a chronic brain disease with a relapsing course and is diagnosed based on international criteria for substance addictions (ICD 10, DSM IV) [4, 5], where typical patterns of cognitive, behavioral and physiological symptoms are described (see Table 1 for DSM IV and ICD 10 criteria). For effective treatment results, it is essential to be aware of the core characteristic shared by all substance abusers and addicts, namely, the lack of motivation in changing one’s lifestyle. It would, however, be a mistake to categorize all alcohol dependent patients into a single homogenous group, since the disease’s disposition factors are as diverse as its treatment. Due to the heterogeneity of AD, researchers have attempted to create subtypes with the aim of providing targeted subtype-specific treatments to patients, thereby increasing their probability of long-term abstinence and hence improving prognosis. A relatively recent study from Hesselbrock [6] has shown that a preference towards the categorization of AD patients into four distinct homogenous subgroups is present among experts in the field (see Table 2).
Table 1.
DSM-IV-TR and ICD 10 criteria for Alcohol Dependence
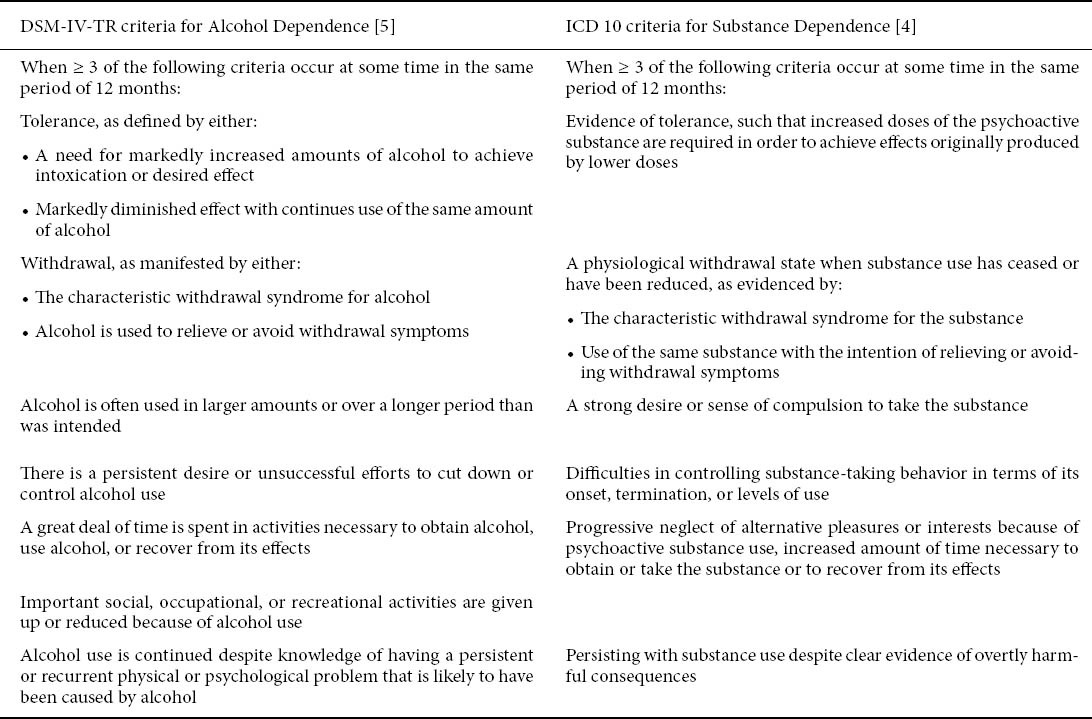
Table 2.
Empirically supported and clinically useful characteristics found to be most accurate in describing distinctive subtypes of alcohol dependent patients [6, 9]
Depending on the patients’ drinking patterns and the origin of their substance-craving, relapses, being more common in some than in others, occur frequently in alcohol dependent patients. Physicians struggle with the challenge of preventing such relapses, however, pharmacological treatments are not always the most effective way of preventing them. Psychosocial as well as psychotherapeutic approaches are often essential for motivating patients to stay sober. In the following article, the four subtypes of the “Lesch Alcoholism Typology” (LAT) will be introduced and the symptoms and treatment methods associated with each subtype will be described in detail.
Treatment Goals
While treating alcoholics, two basic principles should be considered: the principle of reality and the principle of mutuality. Treatment goals should be realistic and reachable and both patient andtherapist should mutually agree upon them. Total abstinence is not always the desired outcome. Some patients wish to simply reduce the amounts of alcohol they drink, while others merely want to relieve the symptoms (co-morbidities, vitamin deficiencies, etc.) associated with chronic alcohol consumption. After the Lesch typology has been determined and the treatment goals have been set, it is the therapist’s duty to present strategies, that could most effectively help the patient accomplish his/her goals.
Methodology – Development of the Lesch Typology
The Lesch Typology is based on data derived from a longitudinal prospective study on alcohol dependent patients (based on ICD-9 criteria) in a catchment area of 210,000 in-habitants [7]. Between 1976 and 1979, all patients diagnosed with AD and admitted to a psychiatric department were included. Patients were assessed during their hospital stay, while simultaneously their families were also evaluated. Over a follow-up period ranging from 4 to 7 years, these patients were explored every 2nd month. After 12 years, the patients were yet again examined in their family environment by two independent psychiatrists. Particular emphasis was placed on the stability of the previously assigned subgroups.
By observing the long term development of 436 alcohol dependent patients, four subgroup specific disease courses could be determined. These subgroups were then correlated with 136 items taken from the patients’ psychosocial and medical records. As a result, 11 items showed statistical significance in predicting the subgroup the patient belongs to. These 11 items were then used to establish an instrument acting as a decision tree [8], which, in the meantime, has been validated through basic and neurophysiologic research studies as well as in many treatment trials [9], and has additionally been translated into many European languages (English, Spanish, French, Polish, Greek, etc.). A computerized version of the LAT decision tree had been created and is being used on a daily basis in hospitals in many European countries. After completing the survey, the computer program determines the patient’s typology, and additionally provides information about treatment goals and methods most appropriate for the patient’s subtype.
The multidimensional diagnostic process involved in determining the Lesch subtype is demonstrated in Figure 1. If a symptom specific to Type IV can be assessed, then the patient instantly falls into the category of Type IV. If there are no symptoms of Type IV, but the patient has an affective disorder or presents suicidal behavior unrelated to alcohol consumption, Type III is diagnosed. If neither symptoms of Type IV or Type III are present, but severe withdrawal symptoms or seizures have occurred, then Type I is diagnosed. Type II patients, consuming alcohol to cope with states of anxiety, do not show any symptoms of Type IV, III or I. In Table 3, the different craving symptoms and fundamental neurobiological models associated with each Lesch subtype are summarized.
Figure 1.
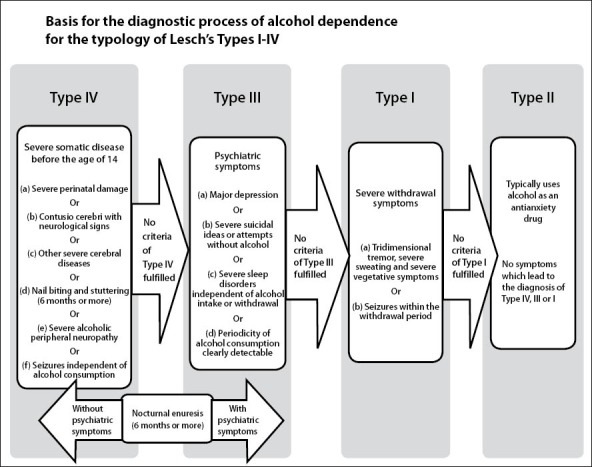
An overview of the decision tree, including the key factors determining each Lesch subtype [27]
Table 3.
Depending on the Lesch subtype, different craving symptoms and neurobiological models may be observed [9, 28]
The Four Lesch Subtypes – Clinical importance in diagnostic and therapeutic approaches
Lesch Type I (Allergy Model)
Symptoms
A biological vulnerability accounts for the symptoms associated with this subtype (high levels of acetaldehyde are also found during abstinent phases). These patients tend to use alcohol to reduce their withdrawal symptoms, which can be seen as a sort of rebound phenomenon (GABA hyper-sensitivity; glutamate-GABA imbalance). If Type I patients abruptly decrease or end their usual alcohol intake, severe withdrawal symptoms, such as three-dimensional tremors, profuse sweating (“wet withdrawal”), restlessness and/or epileptic seizures arise (tonic-clonic seizures may occur on the first or second day after sudden quantity changes). The withdrawal symptoms develop rapidly (often within hours) and disappear within a few days. Without instant medical attention these withdrawal symptoms may increase and lead to a life-threatening delirium tremens. During withdrawal, basic vital functions, such as blood pressure or heart rate, are often irregular; however, these disturbances need no special drug treatment. Type I patients can almost always accurately describe the amount of alcohol necessary each morning to put an end to their withdrawal symptoms. In this subgroup, total abstinence is a realistic goal, however, it is also an absolute necessity.
Treatment of Withdrawal
Benzodiazepines should be applied as early as possible, preferably before withdrawal symptoms begin. The dosage may be determined by several factors: either by the quantity of alcohol needed to end withdrawal symptoms in the morning, or by the severity of the immediate (and/or past) withdrawal symptoms and also by the present alcohol blood level. Since benzodiazepines may prevent life-threatening epileptic seizures, it is important to apply a sufficient dosage early during therapy (see Table 4 for standard dosage according to Lejoyeux et al.[10]). Additionally, adequate hydration should also be ensured.
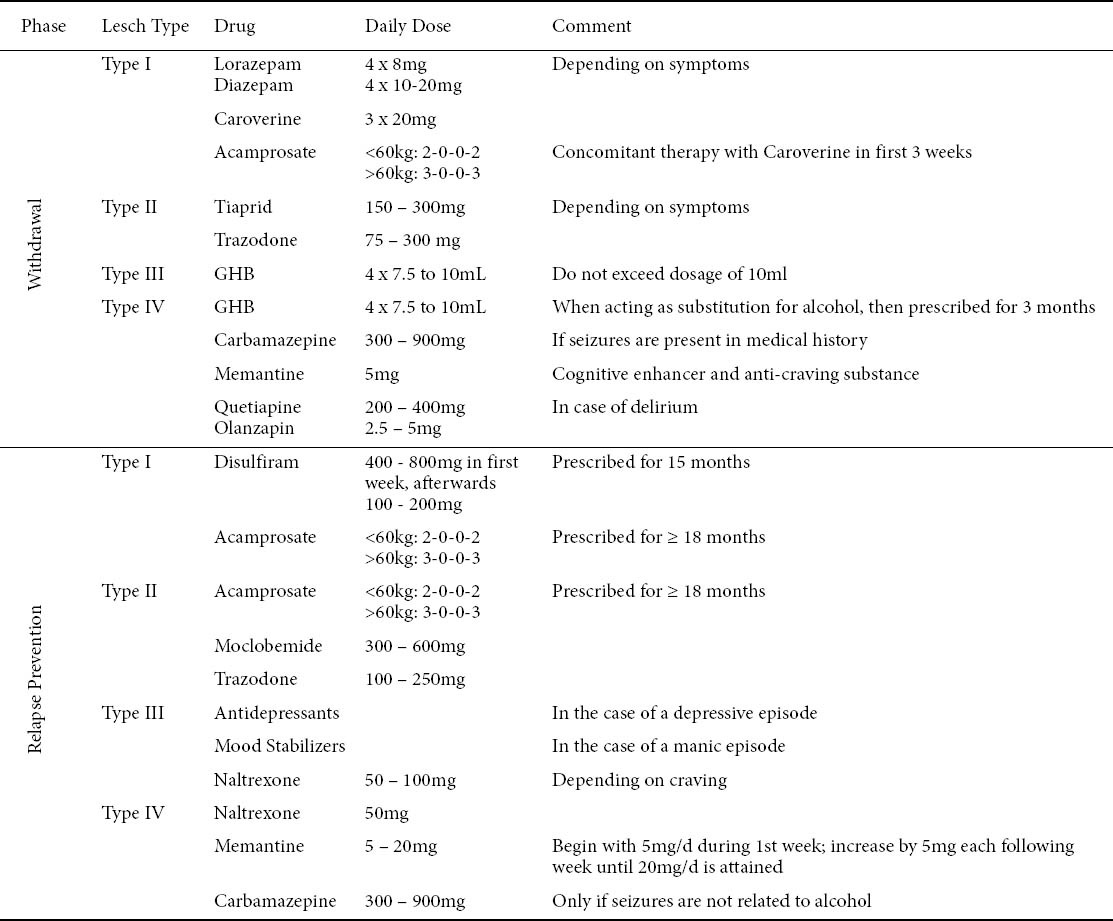
Table 4.
Pharmacological treatment of alcohol dependent patients according to Lesch Typology
As for soothing craving symptoms during withdrawal, Caroverine [11] and Acamprosate are recommended for this subtype. Since the full satiety of Acamprosate is only reached after 2 or 3 weeks, concomitant therapy with Caroverine is advised during the first 3 weeks of treatment.
Contraindications: Both Antipsychotics (e.g. Flupentixol) and Anti-parkinson drugs (e.g. Lisuride, Tiaprid) may increase the likelihood of seizures (and also of relapses).
Treatment of Relapse
In case of a brief lapse, a syrup containing Gamma-Hydroxybutrate (GHB) is given to the patient for only several days, so that a full relapse can be prevented. During the occurrence of a full relapse after a prolonged period of abstinence, Type I patients are advised to take Naltrexone, which helps diminish the magnitude and length of a relapse. As soon as abstinence is restored, the drug may be discontinued. Should the relapse be severe, Naltrexone may be combined with GHB in order to achieve an optimal effect.
Relapse Prevention – Medical Treatment
Disulfiram should only be prescribed to highly motivated patients, who are exposed to a high pressure of consuming alcohol (e.g. barkeepers). It is recommended to combine Disulfiram [12, 13] with the anti-craving substance Acamprosate [14], which should be prescribed for a period of 18 months or longer, usually starting at the onset of withdrawal treatment. However, the prolonged use of Disulfiram should be avoided in alcoholics with liver disease, since liver function may worsen during therapy.
Relapse Prevention – Psychosocial Treatment
Lesch Type I alcohol dependent patients usually do not exhibit any signs of a primary personality disorder. It is rather a physical or biological disease that affects these patients. For this reason, brief behaviorally-oriented treatment interventions (e.g. role-playing) has been thought to help these patients in overcoming the pressure of drinking they are regularly exposed to. Self-help groups (e.g. Alcoholics Anonymous) have also shown to be very valuable in supporting this group of patients. Sometimes systemic approaches may also be helpful, especially when patients are dealing with issues of power or helplessness in their social circles or family. Also, checkups (alcohol breath and blood level) on a regular basis have shown to significantly increase sobriety rates. Through thorough support, absolute abstinence is a reachable goal, as demonstrated in a prospective trial, which has shown that 85% of Lesch Type I patients have proven to be totally abstinent for a period of 2 years, when treated according to the recommendation previously described [15].
Lesch Type II (Conflict Resolution and Anxiety Model)
Symptoms
When conflicts arise in the lives of Lesch Type II patients they develop strong feelings of anxiety, where instead of dealing with their problems directly (“harm avoidance”), these patients rather turn to alcohol for its anxiolytic and calming effects. In such situations, alcohol is often abused as a conflict resolution strategy. Very often, a primary personality disorder with features of an “ego-weakness” (dependent or anxious (avoidant) personality disorders) may be observed in these patients. In their abstinent phases, Lesch Type II patients often demonstrate a very low self esteem. These patients are frequently found to be (or have been) in a relationship with a dominant partner. Under the influence of alcohol, personality changes may occur with signs of affect instability or reduced impulse-control.
Withdrawals in Type II patients include transitory anxiety/depressive symptoms, signs of physical tension (with increased blood pressure and heart rate), sweating of the hands and a subtle two-dimensional tremor. No signs of epileptic seizures or polyneuropathy should be present in the patient’s medical history. The duration of withdrawal is about two weeks. Long-term abstinence with minor slips, however, without loss of control, is a realistic treatment goal. Minor slips should also be accepted by the therapist, for they do not negatively influence the long-term prognosis.
Treatment of Withdrawal
Well suited for these patients is treatment with Tiaprid, which has very effective anxiolytic properties. The dosage depends on the patient’s symptoms (severity of anxiety) and difficulties falling asleep. Sedating antidepressants may also be used if symptoms are mild.
Contraindications: Due to the risk of shifting their addiction to another substance, Benzodiazepines are no recommended in Type II patients. Many Type II patients learn that benzodiazepines are also effective against feelings of anxiety, and after successful withdrawal, patients may begin abusing benzodiazepines instead.
Relapse Prevention – Medical Treatment
The anti-craving drug Acamprosate [14,16-18] in combination with psychotherapy has shown to be quite effective in this group of patients. Antidepressants with anxiolytic properties (e.g. Moclobemide or Trazodone) are also beneficial in preventing relapses in Type II patients.
Relapse Prevention – Psychosocial Treatment
As mentioned before, Lesch Type II alcoholics exhibit symptoms of “ego-weakness”, where the main goal of treatment should be the strengthening of the patient’s weak personality, and not necessarily the alcohol addiction. Psychotherapeutic methods specializing in the treatment of dependent or anxious personality disorders should be recommended. During these treatments, patients are made aware of their harmful interactions with others and learn to avoid dependent relationships by identifying early warning signs. Emphasis should also be placed on coping techniques during stress and crisis situations. Also, mental strategies helping to reduce anxieties should also be learned (e.g. Hypnotherapy). The patient’s social environment should also be taken into consideration. Often systemic therapy is quite helpful, especially if the patient’s partner suffers from a certain psychiatric or psychosomatic disease. Occasionally, it may also be of advantage to include the patient’s children into the systemic therapeutic process. Self-help groups focusing on anxiety or ego-strengthening and leadership seminars should also be recommended. Alcohol centered groups, such as Alcoholics Anonymous, have shown to be of no use in Type II patients [19].
Lesch Type III (Depressive Model)
Symptoms
Lesch Type III patients abuse alcohol for its mood enhancing and sleep inducing properties. However, although alcohol seems to act soporifically, it actually destroys the sleep architecture, adding further to the patients’ sleeping problems. Epileptic seizures in the patient’s medical history are very rare, but should be considered. However, mood disorders are often found in the patients’ family history.
Lesch Type III patients are often associated with a “Tellenbach-personality” (melancholic personality). Patients often have inflexible, rigid values and high expectations concerning themselves. These high standard demands are often not met, leading to feelings of dissatisfaction and frustration. Type III patients tend not to experience much psychological enjoyment, hence only under the influence of alcohol do they permit themselves to experience emotions. Optimal functioning in one’s profession, family and society in general are so prioritized that little room is left for one’s emotional and physical (e.g. relaxation, leisure activities) wellbeing.
During withdrawal, similar to Type II patients, Type III patients also show a subtle two-dimensional tremor, light sweating of the hands, and a tense, but stable, cardiovascular circulation (increased blood pressure and heart rate). Sleep disturbances (problems falling asleep or sleeping through the night) are also quite common during withdrawal, as is the development of depressive symptoms and feelings of guilt. After several months of abstinence, a depressive episode may recur, often accompanied by a severe relapse, possibly lasting months (episodic drinking style). Patients judge their relapses as severe failures and strong feelings of guilt redevelop.
It is essential not to interrupt the treatment chain in Type III patients, since suicidal thoughts and tendencies may transpire during the anxious-depressive states occurring during withdrawal (and also during relapses). In order to guarantee a continuous treatment, regular outpatient appointments should take place after the patient is discharged from the hospital (a precondition is a well structured network between inpatient and outpatient care) [20]. The therapeutic aim in Type III patients is to reduce the frequency of depressive episodes, and consequently minimizing the frequency and duration of heavy drinking periods. However, the occurrence of a severe relapse, which may follow months of total abstinence, should be accepted by both the therapist and patient.
Treatment of Withdrawal
Depending on the patients’ psychopathological disturbances (suicidal tendencies or depressive episodes), Lesch Type III patients often need short term admissions to inpatient treatments. Type III alcoholics are given GHB during withdrawal. Already after the first dose the efficacy of the GHB treatment can be assessed. If the desired effect is not achieved, a coexistent benzodiazepine abuse should be considered. In such case, treatment with GHB would be inadequate and therapy must be continued with benzodiazepines. The dosage for benzodiazepines is determined by the patient’s withdrawal symptoms, which over the following several weeks should be reduced and the patient should slowly be weaned off the drug. While reducing the dose of benzodiazepines, overlapping therapy with antidepressants should be started. The anti-craving drug Naltrexone should be given early during withdrawal treatment with the intention of decreasing early relapses.
Contraindications: Due to increased relapse and suicidal rates caused by dopamine antagonists, such as anti-psychotic drugs, these medications are not recommended in Type III patients.
Treatment of Relapse
Naltrexone may be given to reduce the duration and severity of a relapse [14], however, in many cases Naltrexone does not prevent the patient from relapsing when taken during abstinent periods [21,22]. If a severe relapse occurs, GHB should be given to the patient for several days.
Relapse Prevention – Medical Treatment
In their long-term course, many Lesch Type III alcohol dependent patients are diagnosed with a bipolar disorder. For this reason, relapse prevention with appropriate antidepressants (e.g. Trazodone, Sertralin[23]) and mood stabilizers (e.g. Lithium, Valproic-acid, Carbamazepine) is essential. Medications are prescribed depending on the patients’ comorbidities and chronobiological disturbances. In case of mild depressions “bright light” therapy may also be beneficial.
Relapse Prevention – Psychosocial Treatment
After the symptoms of withdrawal have subsided, therapy relevant personality traits become apparent. The therapist should educate the patient about the relevant factors associated with his/her drinking pattern (it is advisable to first address the cognitive issues, only later on in therapy should the emotional factors be referred to). During psychotherapeutic treatments, with systemic approaches being most appropriate, the therapist should encourage the patient to become aware of his/her position when interacting with others and should aim at stopping the power-struggle in interpersonal relationships (Type III patients are usually perceived as powerful and dominant and tend to quickly overtake control of their partner or of a group). The patients must learn to loosen up and allow for themselves to experience emotions. Hypnotherapeutic approaches have also shown to be quite effective in Type III patients. It is also essential for these patients to become aware of their body and able to identify early signs of onset depressive episodes (e.g. sleeping disturbances, weight loss), and in such cases they should immediately seek the advice of a psychiatrist. By learning and internalizing coping strategies, patients must be prepared to deal with depressive episodes, which should help them stay away from alcohol.
Lesch Type IV (Conditioning Model)
Symptoms
During the phase of brain development (<14 years), and long before developing a drinking career, Lesch Type IV patients are often associated with significant childhood abnormalities. Traumatic brain injuries (with unconsciousness lasting longer than 6 hours) and cerebral diseases (e.g. meningitis) as well as deviant child behaviors (e.g. stuttering, nail-biting and/or bedwetting for a period longer than six months) can often be found in the patient’s history. Tonic-clonic seizures, neither associated with alcohol consumption nor with alcohol withdrawal, are also frequently found in the patients’ medical records. Type IV patients may also display gait disturbances caused by the severe polyneuropathy often seen in these patients.
During withdrawal, patients are often confused and sometimes even completely disoriented. Patients may occasionally be delusional or experience hallucinations and amentia-like states, marked by mood-disturbances and paranoid tendencies. Marked impairments of intellectual capacity and memory (confabulations, perseverations) can also be assessed during withdrawal. Concerning the physical symptoms, a minor twodimensional tremor may be observed. Many Type IV patients don’t show any symptoms of sweating (“dry-deprivation”) and most of the time have stable cardiovascular rates (normal heart rate and blood pressure). It may take up to months before any signs of recovery may be observed.
The symptoms associated with Type IV patients are not primarily caused by the toxicity of alcohol alone, but are also due to the pre-existing organic brain disturbances. Alcohol rather tends to act as a trigger for these symptoms. A thorough differential diagnosis concerning other causes of organic psychoses is imperative (e.g. cerebral tumors, circulatory disturbances (e.g. stroke), inflammations, hypoglycemia etc.).
Type IV alcohol dependent patients have difficulties resisting “societal pressures” to consume alcohol. Their every day environment consists of people who accept alcoholism and consume alcohol on a regular basis. For Type IV patients, the daily consumption of alcohol is perceived as “normal”. Since they are easily influenced by their environment, have weak control over their impulses and barely posses any coping strategies, relapses are often expected after successful withdrawal when and if patients return to their “drinking environment”. Type IV patients tend to be socially deprived, are sometimes unemployed or even homeless. Due to impaired cognitive functioning, patients often have trouble in managing their day-to-day lives (however, this is mainly due to the pre-existing damages and not solely to alcohol). Many times the structure of their daily routine may evolve around the consumption of alcohol, which in many cases is the sole source of social interaction these patients have.
A realistic therapeutic aim is to keep the frequency and severity of relapses low (survival is the key issue) and prolong the length of abstinent periods. It is important to bring structure into the patient’s daily routine and reduce the patient’s physical symptoms to a minimum. The occurrence of relapses must be tolerated by both patient and therapist and must be seen as part of the course of the illness.
Treatment of Withdrawal
GHB is well suited for Type IV patients since it has no sedating side effects (and therefore does not interfere with motivation for further therapy) and significantly reduces the urge to consume alcohol. Also, there are currently no studies that indicate liver toxicity. However, it must be kept in mind, that GHB has no anti-convulsive properties; hence antiepileptic drugs (e.g. Carbamazepine) must additionally be prescribed if the patient is expected to suffer an epileptic seizure. Nootropic medications (cognitive enhancers), such as Memantines, should be prescribed to improve cognitive functioning and simultaneously reduce craving. If patients experience hallucinations or restlessness at night, atypical anti-psychotic medications are recommended (e.g. Quetiapin, Olanzapin).
Contraindications: Tranquilizers (including Benzodiazepines) have adverse effects on cognitive functioning and therefore intensify the patients’ withdrawal symptoms.
Treatment of Relapse
The anti-craving substance Naltrexone [23-26] has shown to be effective in reducing the length of relapses in Type IV patients [14]. Also therapy with GHB has shown to be an effective treatment method during a relapse.
Relapse Prevention – Medical Treatment
To improve cognitive performance, nootropic drugs (Memantine) may be given for long term therapy. Anticonvulsive drugs, such as Carbamazepin, should only be prescribed if tonic-clonic seizures occur in no connection to alcohol consumption or withdrawal. High dosages of parenterally administered Vitamin B1 (Thiamin) are often necessary to treat polyneuropathy. Physiotherapy should also be considered to alleviate suffering caused by polyneuropathy. GHB may be prescribed as a maintenance drug, acting as a substitute for alcohol during abstinent periods, and hence prolonging periods of sobriety. If GHB is given as a replacement treatment, it should be used for a period of approximately 3 months.
Relapse Prevention – Psychosocial Treatment
An essential focus of withdrawal treatment on Type IV patients is to offer them a secure and abstinent environment (e.g. hospital), where sufficient “activation” (e.g. bright light, physical activities) and supportive measures can be guaranteed. Patients should have a highly structured daily routine, which usually helps them gain stability. Type IV patients should also be encouraged to engage in meaningful activities (e.g. institutions with psychosocial programs). Behavioral therapeutic approaches, where patients are trained to control their impulses in case of a situation where the urge to drink may arise, help broaden their coping resources. Still, for many Type IV patients, socially oriented programs (e.g. social housings with ensured abstinent surroundings)are crucial if they are expected to stay sober and to stay away from their usual “drinking environment”. In some cases, incapacitation and state custodianship may also be necessary.
Many Type IV patients only remain abstinent during their hospital stay. Patients should be able to continue outpatient treatment for at least 1 year, if possible at the same hospital which they had been admitted to as inpatients. Regular visits, starting at a weekly basis (later on at a monthly basis) are essential. Ideally, these appointments should take place with the same therapist at fixed intervals, times and places. During motivational talks, the patient’s poor cognitive capacity (e.g. following complex information may be difficult) should be taken into account, meaning that in the beginning (during withdrawal) motivational content should be repeated several times a day and the patients should gradually be encouraged to set themselves easily achievable goals. Monitoring the drinking habits of patients (e.g. drink-diary and regular checkups) can also be very constructive.
Concluding Remark
Alcohol dependence represents a heterogeneous disease with craving mechanisms being significantly different (e.g. withdrawal, depression, anxiety etc.) in each patient. These craving mechanisms are known to be instigated by diverse biological mechanisms (e.g. NMDA-GABA-, Dopamine-, Opiate-Receptors). The Lesch Typology provides diagnostic procedures helping to define therapy relevant subgroups. The diverse craving mechanisms call for significantly different withdrawal and relapse-prevention medications. By combining these medical treatments with specific psychotherapeutic approaches very good sobriety rates, compared to other chronic conditions, may be achieved.
Biography
Medical University of Vienna
Footnotes
Conflict of Interest: None
References
- 1.Grant BF, Dawson DA, Stinson FS, et al. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States 1991-1992 and 2001-2002. Drug Alcohol Depend. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 2.Mohapatra S, Patra J, Popova S, et al. Social cost of heavy drinking and alcohol dependence in high-income countries. Int J Public Health. 2010;55:149–157. doi: 10.1007/s00038-009-0108-9. [DOI] [PubMed] [Google Scholar]
- 3.Thavorncharoensap M, Teerawattananon Y, Yothasamut J, et al. The economic impact of alcohol consumption: a systematic review. Subst Abuse Treat Prev Policy. 2009;4:20. doi: 10.1186/1747-597X-4-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geneva: WHO; 2000. World Health Organization. International Statistical Classification of Diseases and Related Health Problems (tenth revision) [PubMed] [Google Scholar]
- 5.Washington, DC: American Psychiatric Association. Diagnostic and statistical manual of mental disorders (fourth edition, text rev.); 2000. [Google Scholar]
- 6.Hesselbrock VM, Hesselbrock MN. Are there empirically supported and clinically useful subtypes of alcohol dependence? Addiction. 2006;101(Suppl 1):97–103. doi: 10.1111/j.1360-0443.2006.01596.x. [DOI] [PubMed] [Google Scholar]
- 7.Lesch OM, Dietzel M, Musalek M, Walter H, Zeiler K. The course of alcoholism. Long-term prognosis in different types. Forensic Sci Int. 1988;36:121–138. doi: 10.1016/0379-0738(88)90225-3. [DOI] [PubMed] [Google Scholar]
- 8.Lesch OM, Kefer J, Lentner S, et al. Diagnosis of chronic alcoholism-classificatory problems. Psychopathology. 1990;23:85–96. doi: 10.1159/000284644. [DOI] [PubMed] [Google Scholar]
- 9.Lesch OM, Walter H, Wetschka C, Hesselbrock MN, Hesselbrock VM. Wien/New York: Springer; 2011. Alcohol and Tobacco: Medical and Sociological Aspects of Use, Abuse and Addiction. [Google Scholar]
- 10.Lejoyeux M, Solomon J, Ades J. Benzodiazepine treatment for alcohol-dependent patients. Alcohol Alcohol. 1998;33:563–575. doi: 10.1093/alcalc/33.6.563. [DOI] [PubMed] [Google Scholar]
- 11.Koppi S, Eberhardt G, Haller R, Konig P. Calcium-channelblocking agent in the treatment of acute alcohol withdrawal-caroverine versus meprobamate in a randomized double-blind study. Neuropsychobiology. 1987;17:49–52. doi: 10.1159/000118340. [DOI] [PubMed] [Google Scholar]
- 12.Carroll KM, Nich C, Ball SA, et al. One-year follow-up of disulfiram and psychotherapy for cocaine-alcohol users: sustained effects of treatment. Addiction. 2000;95:1335–1349. doi: 10.1046/j.1360-0443.2000.95913355.x. [DOI] [PubMed] [Google Scholar]
- 13.Chick J, Gough K, Falkowski W, et al. Disulfiram treatment of alcoholism. Br J Psychiatry. 1992;161:84–89. doi: 10.1192/bjp.161.1.84. [DOI] [PubMed] [Google Scholar]
- 14.Kiefer F, Helwig H, Tarnaske T, et al. Pharmacological relapse prevention of alcoholism: clinical predictors of outcome. Eur Addict Res. 2005;11:83–91. doi: 10.1159/000083037. [DOI] [PubMed] [Google Scholar]
- 15.Resch T. Book Die Stabilität der Typologie nach Lesch im Langzeitverlauf [The long term stability of the Lesch Typology] Medical University of Vienna, City; Die Stabilität der Typologie nach Lesch im Langzeitverlauf [The long term stability of the Lesch Typology] p. 2010. [Google Scholar]
- 16.Whitworth AB, Fischer F, Lesch OM, et al. Comparison of acamprosate and placebo in long-term treatment of alcohol dependence. Lancet. 1996;347:1438–1442. doi: 10.1016/s0140-6736(96)91682-7. [DOI] [PubMed] [Google Scholar]
- 17.Kiefer F, Mann K. Acamprosate: how, where, and for whom does it work? Mechanism of action, treatment targets, and individualized therapy. Curr Pharm Des. 2010;16:2098–2102. doi: 10.2174/138161210791516341. [DOI] [PubMed] [Google Scholar]
- 18.Sass H, Soyka M, Mann K, Zieglgansberger W. Relapse prevention by acamprosate. Results from a placebo-controlled study on alcohol dependence. Arch Gen Psychiatry. 1996;53:673–680. doi: 10.1001/archpsyc.1996.01830080023006. [DOI] [PubMed] [Google Scholar]
- 19.Witkiewitz K, Hartzler B, Donovan D. Matching motivation enhancement treatment to client motivation: re-examining the Project MATCH motivation matching hypothesis. Addiction. 2010;105:1403–1413. doi: 10.1111/j.1360-0443.2010.02954.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sonneck G. [Suicide and suicide prevention in Austria] Wien Klin Wochenschr. 2000;112:943–946. [PubMed] [Google Scholar]
- 21.Krystal JH, Cramer JA, Krol WF, Kirk GF, Rosenheck RA. Naltrexone in the treatment of alcohol dependence. N Engl J Med. 2001;345:1734–1739. doi: 10.1056/NEJMoa011127. [DOI] [PubMed] [Google Scholar]
- 22.Chick J, Anton R, Checinski K, et al. A multicentre, randomized, double-blind, placebo-controlled trial of naltrexone in the treatment of alcohol dependence or abuse. Alcohol Alcohol. 2000;35:587–593. doi: 10.1093/alcalc/35.6.587. [DOI] [PubMed] [Google Scholar]
- 23.Pettinati HM, Oslin DW, Kampman KM, et al. A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occurring depression and alcohol dependence. Am J Psychiatry. 2010;167:668–675. doi: 10.1176/appi.ajp.2009.08060852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Volpicelli JR, Rhines KC, Rhines JS, et al. Naltrexone and alcohol dependence. Role of subject compliance. Arch Gen Psychiatry. 1997;54:737–742. doi: 10.1001/archpsyc.1997.01830200071010. [DOI] [PubMed] [Google Scholar]
- 25.O’Malley SS. Opioid antagonists in the treatment of alcohol dependence: clinical efficacy and prevention of relapse. Alcohol Alcohol. 1996;31(Suppl 1):77–81. [PubMed] [Google Scholar]
- 26.Johnson BA. Medication treatment of different types of alcoholism. Am J Psychiatry. 2010;167:630–639. doi: 10.1176/appi.ajp.2010.08101500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vyssoki B, Munda PS, Ferenci P, et al. Comparison of Alcohol-dependent Patients at a Gastroenterological and a Psychiatric Ward According to the Lesch Alcoholism Typology: Implications for treatment. Alcohol and Alcohol. 2010;45:534–40. doi: 10.1093/alcalc/agq059. [DOI] [PubMed] [Google Scholar]
- 28.Walter H, Ramskogler-Skala K, Dvorak A, et al. Glutamic acid in withdrawal and weaning inpatients classified according to Cloninger`s and Lesch`s typologies. Alcohol Alcohol. 2006;41:505–511. doi: 10.1093/alcalc/agl042. [DOI] [PubMed] [Google Scholar]


