Abstract
Background
Bile leak is a common and serious complication of cholecystectomy with endotherapy being an established method of treatment. This retrospective study presents the 11-year experience of a referral center in endoscopic management of post-cholecystectomy bile leaks.
Methods
During the period between January 2000 and December 2010, records of patients who had undergone endoscopic retrograde cholangiopancreatography (ERCP) for suspected post-cholecystectomy bile leaks were reviewed for evidence of clinical presentation of bile leaks, cholangiographic findings, type of endoscopic intervention, procedural complications and post-procedure follow-up.
Results
Seventy-one patients with suspected post-cholecystectomy bile leak were referred for ERCP. Common bile duct (CBD) cannulation was successful in 70 patients (98.59%). Complete transection of CBD was diagnosed in 4 patients; they were treated with surgery. A leak from the cystic duct stump was demonstrated in 49 patients (74.24%), from the ducts of Luschka in 4 (6.06%), from the gallbladder bed in 2 (3.03%), from the CBD in 7 (10.61%) and from the common hepatic duct (CHD) in 4 patients (6.06%). Endoscopic sphincterotomy (ES) plus endoprosthesis was performed in 64 patients (96.97%). A 12-year-old girl with a leak from cystic duct stump was successfully treated with stenting without ES and one patient with leak from gallbladder bed underwent only ES. Endoscopic intervention failed to treat a leak from CHD in one patient. During the follow-up, three patients developed bile duct stricture. Two were treated endoscopically and one with hepaticojejunostomy.
Conclusions
ES plus large-bore straight plastic biliary stent placement is a safe and effective intervention in post-cholecystectomy bile leaks.
Keywords: ERCP, cholecystectomy, endoscopic sphincterotomy, complications, bile leak, endoscopic stenting
Introduction
Bile leaks are broadly reported complications of cholecystectomy, with endoscopic management being an effective therapeutic intervention in most of them [1]. Specifically, these complications occur most frequently after laparoscopic surgeries; despite the increased experience with laparoscopy, a review [2] of 1.6 million laparoscopic cholecystectomies showed an unchanged 0.5% incidence of bile duct injury, and only 30% of injuries are recognized at the time of operation [3]. Bile leaks are usually the result of inadvertent surgical damage to the common and hepatic ducts and associated right hepatic artery injury; misidentification of common duct for the cystic duct; failure to completely clip off the cystic duct; clip ligation of the distal common duct resulting in biliary obstruction and leak; leak from the gallbladder bed, accessory hepatic ducts or from the T-tube tract; and excessive use of cautery or laser in the region of the common bile duct (CBD), resulting in bile leak and strictures [4,5]. The clinical picture of a postoperative bile leak includes an external biliary drainage or an internal biliary-peritoneal leak resulting in biloma, and peritonitis or abscess formation [6,7].
This retrospective study presents the 11-year experience of our Department in endoscopic management of postoperative bile leaks.
Patients - Methods
The endoscopy database of the Department of Endoscopy and Motility Unit, a tertiary referral University-affiliated center specialized in endoscopic management of digestive diseases, was reviewed to identify all patients referred for endoscopic retrograde cholangiopancreatography (ERCP) because of suspected post-cholecystectomy bile leak. Data collected included clinical presentation, time between surgical intervention and ERCP, pre-endoscopic work-up [clinical presentation, biochemical and complete blood count profile, ultrasound (US), computed tomography (CT), magnetic resonance cholangiopancreatography (MRCP)], while ERCP imaging results were reviewed to determine the type of injury, type of therapeutic endoscopic intervention and patients’ follow-up. Antibiotics were given before the endoscopic procedure in all patients (ciprofloxacin 800 mg/day). All endoscopic procedures were performed by an experienced pancreatobiliary endoscopist (PK), with the patients under midazolam (5-10 mg) plus pethidine (50-100 mg) or propofol (0.5-1 mg/kg) sedation by using a duodenoscope with a large (4.2 mm) accessory channel. The patients were given continuous nasal oxygen and their hemoglobin saturation and pulse rate were monitored with pulse oximetry.
The therapeutic protocol included visualization of the biliary tree. The demonstration of bile leak (Fig. 1) was followed by endoscopic sphincterotomy (ES). If residual stones were seen in the CBD, ES was followed by stone extraction using a balloon or Dormia basket with or without mechanical lithotripsy. A plastic straight stent 10 or 11.5 Fr, of various length (Cotton-Leung or Tannenbaum, Wilson-Cook) was routinely inserted proximally to the site of the bile leak from the cystic stump (Fig. 2), the CBD or the common hepatic duct (CHD). If the bile leak was from the gallbladder bed or was due to inadvertent rupture of an aberrant hepatic duct, a short (5 cm) stent standing the papilla was placed.
Figure 1.

Endoscopic retrograde cholangiogram showing a leak from the cystic duct stump (arrow).
Figure 2.

Radiograph showing a Tannenbaum stent (Wilson-Cook, Athens) inserted proximally to the site of the bile leak.
The clinical healing of the leak was determined by the elimination of the symptoms, by the cessation of the output of the bile from the drain in situ, and by the removal of the drain without any adverse outcome. The failure of the endoscopic treatment was determined by the need for further intervention to control the leak including surgery or percutaneous drainage of the biliary tree.
ERCP complications were classified and graded according to the consensus criteria of Cotton et al [8]. Early post-ERCP complications evaluated were bleeding, submucosal injection or perforation, pancreatitis, cholangitis, and basket impaction [9,10]. The stents were removed after an interval of four to eight weeks. Patients with CBD or CHD leak and associated stenosis were followed for possible development of biliary stricture with liver function tests and US every three months in the first post-procedure year. MRCP or ERCP was performed only in the case of clinical symptoms or abnormal liver function tests or US.
Results
Between January 2000 and December 2010 a total of 71 patients [median age: 59 (range 12-83) years, male: 29] were referred to our Department for suspected post-cholecystectomy bile leak. Only 9/71 patients were referred by the surgical service of our hospital; the remaining 62 were referred for ERCP at our Department from other outside institutions. The time interval between surgery and ERCP ranged between 3 to 22 days with a median of 8 days.
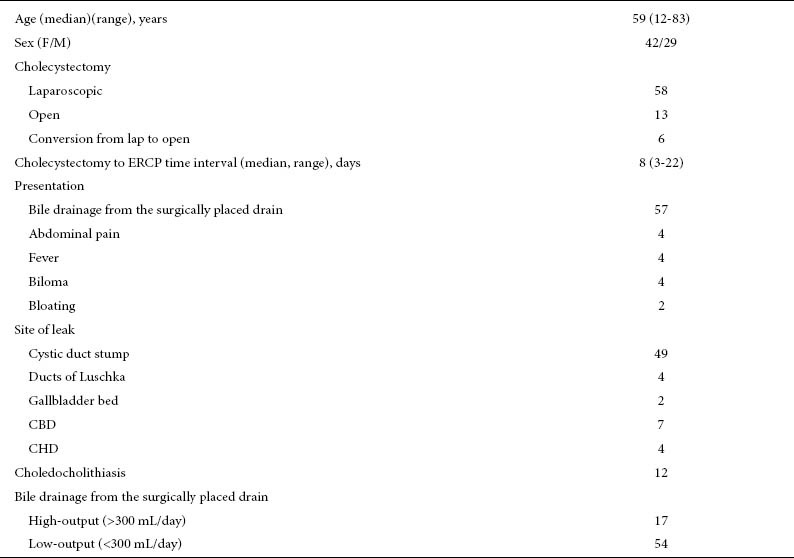
The most common presentation was bile leak from the surgical drain (57/71), followed by abdominal pain (4/71), fever (4/71), biloma (4/71) and bloating (2/71) (Table 1). High-output bile leak was observed in 17 patients (23.94%) and low-output in 54 patients (76.06%) (Table 1).
Table 1.
Demographics, clinical presentation and endoscopic findings of patients undergoing endoscopic retrograde cholangiopancreatography (ERCP) for suspected post-cholecystectomy bile leaks (F, female; M, male; CBD, common bile duct; CHD, common hepatic duct)
Conventional cannulation of CBD via a sphincterotome with or without hydrophilic guide-wire was done in 64 patients (90.14%). In six patients (8.45%) precut technique (needleknife n=3, suprapapillary n=2 and transpancreatic n=1) was needed to achieve CBD cannulation. In one patient (1.41%), despite needle-knife papillotomy, cannulation of CBD was unsuccessful, and the patient underwent surgery with primary closure of the bile leak and T-tube placement.
Complete transection of CBD was diagnosed in four patients who were referred for hepaticojejunal anastomosis. In the remaining 66 patients, the commonest site of leak was cystic duct stump (49/66). Other sites were CBD (7/66), CHD (4/66), ducts of Luschka (4/66) and gallbladder bed (2/66) (Table 1). In 12 out of 66 patients choledocholithiasis was observed; stones were successfully removed in all cases. Endoscopic interventions for bile leak treatment are demonstrated in Fig. 3. ES plus stent insertion was the main intervention (64/66). A 10 Fr stent was placed in 53 patients and an 11.5 Fr in 11 patients. In a 12-year-old girl a 7 Fr-7 cm straight plastic stent without ES was placed for a cystic duct stump leak, leading to resolution of leak. An 83-year-old man with leak from gallbladder bed and low-output bile leak was successfully treated with ES alone. In one patient with a defect in CHD and a high-output bile leak, despite repeated ERCP, stent insertion failed to control the leak and he underwent hepaticojejunostomy. Biloma, diagnosed before ERCP, was observed in four patients. Percutaneous drainage was achieved in one patient, while the remaining three patients were treated conservatively. Median hospital stay was 12 (range: 6-31) days.
Figure 3.
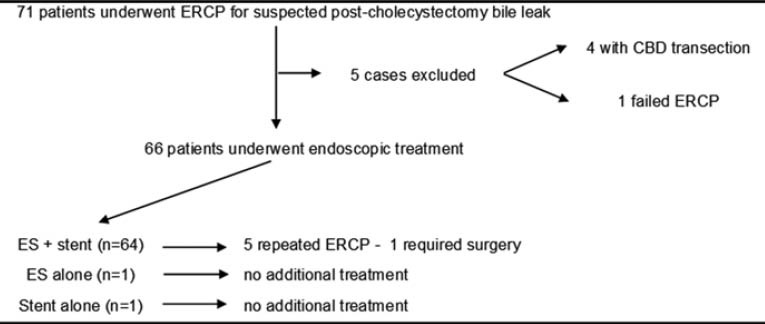
Endoscopic treatment of 71 patients for suspected post-cholecystectomy bile leak
CBD, common bile duct; ERCP, endoscopic retrograde cholangiopancreatography; ES, endoscopic sphincterotomy
All patients underwent a repeat ERCP for stent removal four to six weeks after stent placement. Three patients (4.23%) developed mild post-ERCP pancreatitis, were treated conservatively and all recovered without long-term sequelae. Four patients (5.63%) presented intraprocedural bleeding and were treated with injection of adrenaline and thermocoagulation. None of the patients presented perforation, stent occlusion, basket impaction or cholangitis.
During a median follow-up of 39 months (range 3-132 months), bile duct stricture developed in three patients (4.62%) with leak from CHD (n=2) and CBD (n=1). The stricture was resolved in response to balloon dilation and one year stenting in two patients. In the remaining patient with a high-grade stricture, despite six ERCP procedures with serial balloon dilations and stenting, the stricture did not resolve and he underwent hepaticojejunostomy.
Discussion
The widespread acceptance of laparoscopic cholecystectomy, as the treatment of choice for symptomatic cholelithiasis and even for acute cholecystitis, resulted in the rise of incidence of significant postoperative bile leaks from 0.1-0.3% after open cholecystectomy to 0.15-0.7% after laparoscopic cholecystectomy [11]. Whenever biliary leakage is suspected, close collaboration between endoscopists and surgeons is necessary. Immediate visualization of the biliary tract by ERCP is mandatory to confirm the diagnosis and to locate the precise site of the lesion. This procedure has become the preferred diagnostic and therapeutic modality; its role in the management of bile leaks is well established, and ERCP provides an attractive alternative to both radiological and surgical interventions [12].
The present series of 71 patients with suspected post-cholecystectomy bile leaks who were referred for endoscopic treatment is one of the largest published data. Most patients (64/66) were treated by ES plus a 10 Fr or 11.5 Fr straight plastic polyethylene or Teflon stent and presented favorable outcome (Table 2). Only one patient with a defect in the CHD and high-output leak failed to repeat stenting and underwent surgery. The high rate of endoscopic success is in accordance with the results of other clinical [13-15] and experimental [16] studies which suggest that ES plus stent insertion is more effective to abolish the pressure gradient across the sphincter of Oddi than ES alone, thereby promoting preferential flow of bile into the duodenum and allowing the leak to heal.
Strategies for stent insertion include ‘‘crossing’’ the leak site with the stent vs. elimination of the transpapillary pressure gradient without crossing the leak. These two approaches have not been thoroughly evaluated, but, in general, it seems unlikely that crossing the leak provides any additional therapeutic benefit, such as occlusion of the defect.
It is interesting that a young 12-year-old girl with cystic duct stump leak was successfully treated with a 7 Fr straight plastic stent without ES. The 7 Fr stent was chosen in order to minimize the probability of post-ERCP pancreatitis due to pancreatic orifice occlusion by the stent [17]. It is important to maintain the sphincter of Oddi in young patients because the consequences of chronic duodeno-biliary reflux on biliary epithelium are unknown. There are studies suggesting that the chronic duodeno-biliary reflux predisposes to biliary cancer [18,19]. Alternative treatment strategies to avoid permanent abolishment of basal sphincter of Oddi pressure, especially in young patients, is the topical application of nitroglycerine (which relaxes the sphincter of Oddi) [20], which was used to heal a post-cholecystectomy bile leak or stenting without ES [14]; also, botulinum toxin has been shown in an animal model to heal bile leaks with an efficacy equal to stent insertion [21]. However, at present these strategies are experimental and data from clinical trials are needed before being considered for clinical practice.
In one patient with CHD defect and high-output bile leak, the treatment with a 10 Fr straight plastic stent failed to resolve the bile leak. The surgeon preferred the patient to undergo open surgery after failure of first ERCP to control the leak. It is likely that repeated ERCP with two or three stents insertion might have precluded surgery in this patient. Some authors [13,14] advocated that in major leaks, such as those resulting from damage to CBD or CHD which are often associated with larger defects, plastic stents of large diameter (10 or 11.5 Fr) or multiple stents should be inserted with the intent of filling the bile duct lumen and crossing the site of the leak.
Recently, Wang et al [22] showed the efficacy of endoscopic temporary placement of biliary covered self-expanding metal stents in the treatment of complex bile leaks.
Biliary stricture occurred in only three patients with leak from CHD and CBD and associated stenosis in the cholangiography. Two patients were treated with combination of balloon dilation and stenting and one underwent hepaticojejunal anastomosis. Factors that contribute to stricture formation include local ischemia, electrosurgical injury at surgery and peribiliary inflammation as a result of bile leak [5,23,24]. On the other hand, comparably to our findings, endoscopic stenting helps to avoid surgery in more than 80% of patients bearing postcholecystectomy CBD strictures [25]. Complementary percutaneous drainage of bilomas is useful. In our study, a patient with biloma underwent successful percutaneous drainage and three patients with small collections were treated conservatively.
Importantly, we consider that an ERCP should be performed as soon as a probable biliary problem is suspected, particularly bile from the surgically placed abdominal drain, fever, or abdominal distention. Elevated liver function tests during the first two days after cholecystectomy may have no pathologic significance, but the persistence of abnormal liver function tests for more than 72 hours postoperatively should prompt a retrograde opacification and offer possible treatments. Several authors [5,25,26] have also emphasized the importance of early aggressive investigation in patients with diffuse abdominal pain, fever, malaise, or liver function abnormalities after cholecystectomy. It should be noted that early ERCP decreases the total hospital stay, thereby reducing the total cost for the patient. In our case series the median time interval from cholecystectomy to ERCP was 8 days. These time intervals show that surgeons often underestimate the importance of prompt referral of patients with possible bile leaks to an experienced biliary endoscopist.
In conclusion, despite the retrospective design of the study, our findings suggest that endoscopic intervention should be considered as the preferred treatment strategy in most patients with post-cholecystectomy bile leak.
Summary Box
What is already known:
Endoscopic treatment remains the first-choice treatment of post-cholecystectomy bile leaks.
What the new findings are:
Endoscopic stenting without sphincterotomy appeared to be safe in our pediatric patient with a bile leak, and suggests that sphincterotomy could be avoided in young patients to prevent long-term complications of duodenobiliary reflux.
Biography
aG. Gennimatas General Hospital, Thessaloniki, Greece, bIppokration Hospital, Thessaloniki, Greece
Footnotes
Conflict of Interest: None
References
- 1.Bergmann JJ, van den Brink GR, Rauws EA, et al. Treatment of bile duct lesions after laparoscopic cholecystectomy. Gut. 1996;38:141–147. doi: 10.1136/gut.38.1.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Russell JC, Walsh SJ, Mattie AS, Lynch JT. Bile duct injuries 1989-1993. A statewide experience. Connecticut Laparoscopic Cholecystectomy Registry. Arch Surg. 1996;131:382–388. doi: 10.1001/archsurg.1996.01430160040007. [DOI] [PubMed] [Google Scholar]
- 3.Way LW, Stewart L, Gantert W, et al. Causes and prevention of laparoscopic bile duct injuries: analysis of 252 cases from a human factors and cognitive psychology perspective. Ann Surg. 2003;237:460–469. doi: 10.1097/01.SLA.0000060680.92690.E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deziel DJ, Millikan KW, Economou SG, Doolas A, Ko ST, Airan MC. Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 1993;165:9–14. doi: 10.1016/s0002-9610(05)80397-6. [DOI] [PubMed] [Google Scholar]
- 5.Davidoff AM, Pappas TN, Murray EA, et al. Mechanisms of major biliary injury during laparoscopic cholecystectomy. Ann Surg. 1992;215:196–202. doi: 10.1097/00000658-199203000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barkun AN, Rezieg M, Mehta SN, et al. Postcholecystectomy biliary leaks in the laparoscopic era: risk factors, presentation, and management. McGill Gallstone Treatment Group. Gastrointest Endosc. 1997;45:277–282. doi: 10.1016/s0016-5107(97)70270-0. [DOI] [PubMed] [Google Scholar]
- 7.Katsinelos P, Kountouras J, Paroutoglou G, et al. A comparative study of 10-Fr vs. 7-Fr straight plastic stents in the treatment of postcholecystectomy bile leak. Surg Endosc. 2008;22:101–106. doi: 10.1007/s00464-007-9381-y. [DOI] [PubMed] [Google Scholar]
- 8.Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–393. doi: 10.1016/s0016-5107(91)70740-2. [DOI] [PubMed] [Google Scholar]
- 9.Katsinelos P, Kountouras J, Chatzis J, et al. High-dose allopurinol for prevention of post-ERCP pancreatitis: a prospective randomized double-blind controlled trial. Gastrointest Endosc. 2005;61:407–415. doi: 10.1016/s0016-5107(04)02647-1. [DOI] [PubMed] [Google Scholar]
- 10.Katsinelos P, Kountouras J, Paroutoglou G, Beltsis A, Mimidis K, Zavos C. Intravenous N-acetylcysteine does not prevent post-ERCP pancreatitis. Gastrointest Endosc. 2005;62:105–111. doi: 10.1016/s0016-5107(05)01574-9. [DOI] [PubMed] [Google Scholar]
- 11.Roy PG, Soonawalla ZF, Grant HW. Medicolegal costs of bile duct injuries incurred during laparoscopic cholecystectomy. HPB (Oxford) 2009;11:130–134. doi: 10.1111/j.1477-2574.2008.00023.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donnellan F, Zeb F, Courtney G, Aftab AR. Successful outcome of sphincterotomy and 7 French pigtail stent insertion in the management of post-cholecystectomy bile leaks. Hepatobiliary Pancreat Dis Int. 2009;8:309–311. [PubMed] [Google Scholar]
- 13.Sandha GS, Bourke MJ, Haber GB, Kortan PP. Endoscopic therapy for bile leak based on a new classification: results in 207 patients. Gastrointest Endosc. 2004;60:567–574. doi: 10.1016/s0016-5107(04)01892-9. [DOI] [PubMed] [Google Scholar]
- 14.Kaffes AJ, Hourigan L, De Luca N, Byth K, Williams SJ, Bourke MJ. Impact of endoscopic intervention in 100 patients with suspected postcholecystectomy bile leak. Gastrointest Endosc. 2005;61:269–275. doi: 10.1016/s0016-5107(04)02468-x. [DOI] [PubMed] [Google Scholar]
- 15.Katsinelos P, Kountouras J, Paroutoglou G, et al. A comparative study of 10-Fr vs. 7-Fr straight plastic stents in the treatment of postcholecystectomy bile leak. Surg Endosc. 2008;22:101–106. doi: 10.1007/s00464-007-9381-y. [DOI] [PubMed] [Google Scholar]
- 16.Marks JM, Ponsky JL, Shillingstad RB, Singh J. Biliary stenting is more effective than sphincterotomy in the resolution of biliary leaks. Surg Endosc. 1998;12:327–330. doi: 10.1007/s004649900663. [DOI] [PubMed] [Google Scholar]
- 17.Simmons DT, Petersen BT, Gostout CJ, Levy MJ, Topazian MD, Baron TH. Risk of pancreatitis following endoscopically placed large-bore plastic biliary stents with and without biliary sphincterotomy for management of postoperative bile leaks. Surg Endosc. 2008;22:1459–63. doi: 10.1007/s00464-007-9643-8. [DOI] [PubMed] [Google Scholar]
- 18.Hakamada K, Sasaki M, Endoh M, Itoh T, Morita T, Konn M. Late development of bile duct cancer after sphincteroplasty: a ten- to twenty-two-year follow-up study. Surgery. 1997;121:488–492. doi: 10.1016/s0039-6060(97)90101-x. [DOI] [PubMed] [Google Scholar]
- 19.Tocchi A, Mazzoni G, Liotta G, Lepre L, Cassini D, Miccini M. Late development of bile duct cancer in patients who had biliary-enteric drainage for benign disease: a follow-up study of more than 1,000 patients. Ann Surg. 2001;234:210–214. doi: 10.1097/00000658-200108000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feliu Palá X, Encinas Méndez X, Poveda Gómez S, Martí Sintes G. Nitroglicerina topica: una alternativa en el tratamiento conservador de la fistula biliar. Rev Esp Enferm Dig. 1996;88:877–879. [PubMed] [Google Scholar]
- 21.Brodsky JA, Marks JM, Malm JA, Bower A, Ponsky JL. Sphincter of Oddi injection with botulinum toxin is as effective as endobiliary stent in resolving cystic duct leaks in a canine model. Gastrointest Endosc. 2002;56:849–851. doi: 10.1067/mge.2002.129869. [DOI] [PubMed] [Google Scholar]
- 22.Wang AY, Ellen K, Berg CL, Schmitt TM, Kahaleh M. Fully covered self-expandable metallic stents in the management of complex biliary leaks: preliminary data - a case series. Endoscopy. 2009;41:781–786. doi: 10.1055/s-0029-1215050. [DOI] [PubMed] [Google Scholar]
- 23.Rossi RL, Schirmer WJ, Braasch JW, Sanders LB, Munson JL. Laparoscopic bile duct injuries. Risk factors, recognition, and repair. Arch Surg. 1992;127:596–601. doi: 10.1001/archsurg.1992.01420050124016. [DOI] [PubMed] [Google Scholar]
- 24.Hanazaki K, Sodeyama H, Sode Y, et al. Endoscopic nasobiliary drainage for bile duct injury after laparoscopic cholecystectomy. Surg Endosc. 1997;11:1123–1125. doi: 10.1007/s004649900545. [DOI] [PubMed] [Google Scholar]
- 25.Tuvignon N, Liguory C, Ponchon T, et al. Long-term follow-up after biliary stent placement for postcholecystectomy bile duct strictures: a multicenter study. Endoscopy. 2011;43:208–216. doi: 10.1055/s-0030-1256106. [DOI] [PubMed] [Google Scholar]
- 26.Trerotola SO, Savader SJ, Lund GB, et al. Biliary tract complications following laparoscopic cholecystectomy: imaging and intervention. Radiology. 1992;184:195–200. doi: 10.1148/radiology.184.1.1535161. [DOI] [PubMed] [Google Scholar]


