Abstract
Chronic inflammation in the terminal ileum (TI) suggests a cause for the patient’s symptoms, especially when the clinical suspicion is Crohn’s disease (CD). Clinic, laboratory, endoscopic, histopathological evaluation of patients is required for the diagnosis of CD. The most frequent localization of CD is the TI. There are many other diseases affecting the TI. Non-steroidal antiinflammatory drug (NSAID) intake as well as other pathological conditions such as lymphoid hyperplasia, intestinal infections, lymphoma, infections and ulcerative colitis (UC) can mimic CD terminal ileitis.
In this article the authors discuss these conditions, firstly in terms of differential diagnosis, and point out the facts that the clinicians must consider when they have a patient with terminal ileitis. Misdiagnosis of CD may be harmful to these patients because of inadequate response to therapy and occasionally an unnecessary operation may be performed. At the same time, the patients require appropriate treatment for their condition.
Keywords: Terminal ileitis, Crohn’s disease, differential diagnosis
Introduction
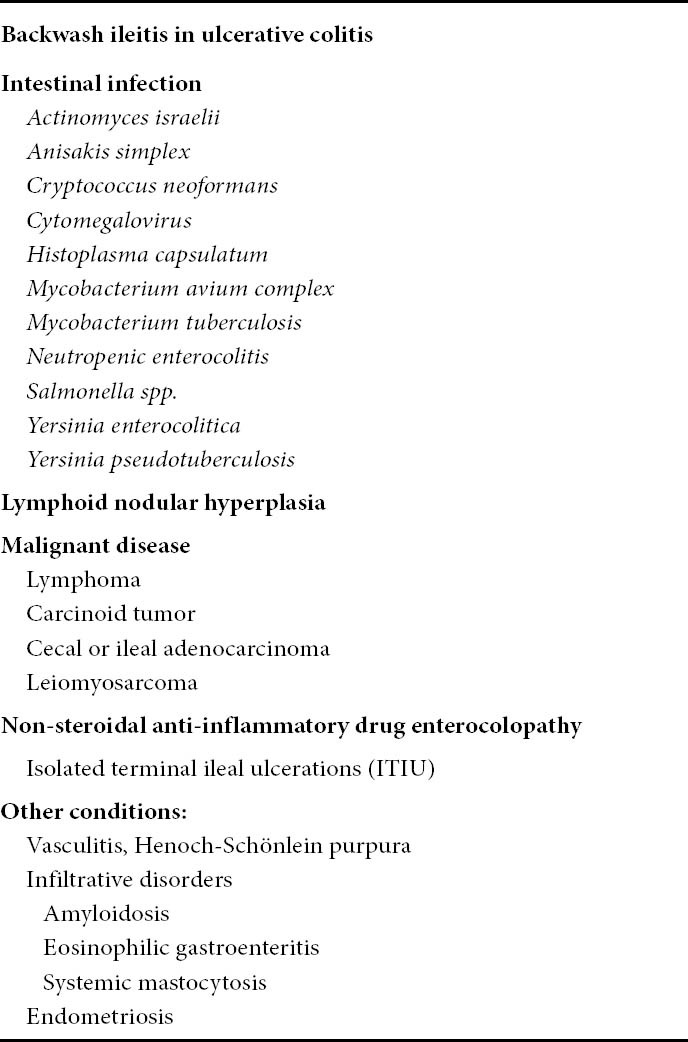
Crohn’s disease (CD) can affect any part of the gastrointestinal (GI) tract, but terminal ileum (TI) is the most frequent localization. Such erosions and ulcers in TI may be the result of non-steroidal anti-inflammatory drug (NSAID) intake and other pathological conditions such as lymphoid hyperplasia, lymphoma, radiation enteritis, infections and ulcerative colitis (UC). These conditions can affect the TI and may mimic CD histologically and endoscopically (Table 1). Intubation and biopsy of the TI during colonoscopy has become a standard procedure in the evaluation and management of patients suspected or known to have inflammatory bowel disease (IBD). Misdiagnosis of CD may be harmful to these patients because of inadequate response to therapy and occasionally unnecessary surgery may be performed.
Table 1.
Differential diagnosis of Crohn’s terminal ileitis in clinical practice
In one recent study of 3,921 patients in whom routine colonoscopy was performed with ileoscopy, 125 of them had macroscopic changes in the TI including ulcers, aphthous ulcers or erosions, nodular or erythematous mucosa, and polypoid lesions. In 91.2% of these cases there were non-specific histological findings not thought to be clinically significant, including non-specific inflammation, lymphoid hyperplasia, and low-grade mucosal damage. None of them had chronic or recurrent bowel symptoms for over a month during the follow-up period, and their findings regarding the TI were not considered to be clinically significant. A clinically significant histopathology was present in 11 cases (8.8%). There were 7 cases of CD, 3 cases of intestinal tuberculosis, and 1 case of Adamantiades-Behcet’s disease [1].
Normal-looking ileal mucosa may reveal significant pathological findings in biopsy specimens. Another study reported the diagnostic yield of histopathology examination in normal-appearing ileal mucosa where in a small number of patients with normal-appearing TI, their mucosa was found to have histological findings in accordance with CD [2].
Ulcerative colitis as a cause of chronic inflammation in TI
Involvement of the TI in UC is termed backwash ileitis (BWI). Features that favor a diagnosis of CD rather than chronic UC with BWI, can be extensive length of involved small bowel separated by skip regions of uninvolved cecum or distal ileum, greater inflammatory activity and mucosal injury in the ileum rather than the cecum, transmural ileal inflammation with granulomas and neural hyperplasia, and mucous gland (so-called pyloric gland) metaplasia of the ileal mucosa [3]. An updated and revised definition of BWI in the context of distinguishing BWI from CD in endoscopically procured mucosal biopsy specimens is needed.
Other authors [4] reported that ileal changes in UC are not uncommon (prevalence 17%). BWI is generally mild in nature (villous atrophy, increased inflammation, scattered crypt abscesses), and is not associated with an increased rate of ileo-anal pouch complications, dysplasia, or carcinoma. However, rarely, ileal erosions may occur in patients without cecal involvement, which may indicate that other pathogenetic mechanisms should be considered in the etiology of ileitis in UC patients.
Intestinal infections can mimic CD
The link between CD and infection is complex and can have implications both clinically (problems in diagnosis, differential diagnosis, approach to management and complications) and scientifically (issues in etiology and pathogenesis). Intestinal infections can mimic the classic endoscopic and clinical (abdominal pain, diarrhea, and weight loss) features of IBD, and can present with identical extraintestinal manifestations (e.g., reactive arthritis, erythema nodosum) [5]. Abdominal tuberculosis can be part of a multiorgan disease process or, less commonly, presents as a primary disease. It has been rare in western countries since the introduction of tuberculostatic drugs. Recently, the incidence of this entity has increased due to the HIV epidemic and introduction of biological therapy. GI involvement with mycobacterial infection occurs primarily in the immunosuppressed patient but may occur in patients with normal immunity. Differentiation from CD can be very difficult on clinical and histological grounds if culture is negative. Treatment with steroids or a tumor necrosis factor-alpha inhibitor can lead to exacerbation of tuberculosis. The ileum is the most commonly-affected site, either in isolation or with the involvement of the adjacent bowel segments, especially the cecum. The main reasons for the predilection are due to a high density of lymphoid tissue, neutral pH environment and absorptive transport mechanisms that allow swallowed mycobacterium to be absorbed [6]. Common presentations include abdominal pain and an abdominal mass in the right lower quadrant. Depending on the stage of the disease, findings may range from normal appearance to small polyps or nodules to extensive ulcerations, hypertrophic, ulcerohypertrophic and fibrotic lesions resulting in strictures, causing bowel obstructions and fistulae formations. Both endoscopy and radiological imaging can be used depending on the site affected. Rapid emptying of contrast, known as the “Sterling’s sign”, is commonly seen in TI involvement due to persistent irritability of the mucosa. Bowel wall thickening, mass lesions and regional adenopathy are best seen on CT. Differentiating ileal tuberculosis from CD can be very difficult. Furthermore, these two conditions may coexist. The presence of centrally necrotic regional lymph nodes favors tuberculosis, whereas a cobblestone appearance and skip lesions favor CD. In a recent study, clinical parameters more common in CD were anorectal lesions, longitudinal ulcers, aphthous ulcers, and a cobblestone appearance that involved fewer than four segments; a patulous ileocecal valve, transverse ulcers, and pseudopolyps were observed more frequently in patients with intestinal tuberculosis [7]. The final clinical diagnosis is based on a combination of the clinical history with endoscopic studies, culture and polymerase chain reaction for mycobacterium tuberculosis, biopsy pathology, radiological investigations and response to therapy.
Yersinia enterocolitica infection occurs mainly in the TI and causes mucosal ulceration, neutrophil invasion, and thickening of the ileal wall. Distal ileal and cecal involvement predominates, and patients present with symptoms of small-bowel obstruction and a tender abdominal mass. The diagnosis is made most directly by colonoscopy with biopsy and culture. Endoscopic features of Yersinia include aphthoid lesions of the cecum and TI with round or oval elevations with ulcerations. The ulcers are mostly uniform in size and shape, in contrast to CD [8]. Mycobacterium avium-intracellulare complex infection occurs in advanced stages of HIV infection and in other immunocompromized states; it usually manifests as a systemic infection with diarrhea, abdominal pain, weight loss, fever, and malabsorption. Diagnosis is established by culture of mucosal biopsies. Disseminated histoplasmosis can also involve the ileocecal area. TI can be affected in other intestinal infections caused by Salmonella spp., cytomegalovirus. Ileitis was described in infection with Clostridium difficile (BI/NAP1/027 strains [9]), typical pseudomembranes were seen on ileal mucosa.
Lymphoid hyperplasia
Focal lymphoid hyperplasia of the TI is a rare cause of terminal ileitis. In 1996 the case of a 13-year-old boy was described with a stricture of the TI that was diagnosed as CD on barium follow through. This patient had no response to steroid therapy and the boy required resection of TI. Histology findings of TI showed focal lymphoid hyperplasia and not CD [10].
Lymphoid hyperplasia of the intestine is a benign reactive process also known as pseudolymphoma, lymphonodular hyperplasia, or terminal lymphoid ileitis. It occurs in all age groups, but is best described in children. There are no definitions or valid criteria for transition of normal hyperplasia to a pathologic state. The dividing line between physiologic nodules and hyperplasia is not precisely defined. Lymphoid hyperplasia may be discovered incidentally, at colonoscopy, or in patients undergoing colectomy, especially in the last few centimeters of the TI. Several causes of lymphoid hyperplasia have been postulated. Giardia lamblia is often present. In a small minority, immunodeficiencies underlie the hyperplastic state. Some patients have low or absent levels of IgA and IgM, decreased IgG levels, susceptibility to infection, and diarrhea with or without steatorrhea. In children, lymphoid hyperplasia is often associated with viral infection. The pathology of lymphoid hyperplasia is quite characteristic, consisting of prominent lymphoid follicles with active germinal centers located in the mucosa and submucosa [11].
Malignant disease
Primary malignant tumors of the small intestine are easy to be misdiagnosed because of nonspecific symptoms and signs and the limited examination methods. In the ileum, malignant lymphoma constitutes about half of all malignancies (48.3% in this group), followed by adenocarcinoma, leiomyosarcoma and carcinoid tumors.
Small bowel lymphoma originates in the lymphoid follicle of the submucosa and may be solitary or diffuse. The solitary form tends to encircle the bowel, narrow the lumen and mimic CD clinically, radiologicaly and endoscopicaly. The diffuse form shows multisegment involvement with Terminal numerous polypoidal excrescences. Enlarged nodes in the mesentery adjacent to the lesion are common in primary lymphoma of the small bowel. Lymphoma most commonly manifests as single or multiple segmental areas of markedly thickened (1.5–7 cm) circumferential thickening, or may ulcerate with formation of a fistulous tract to adjacent bowel loops, mimicking CD [12].
90% of carcinoid tumors originate from the distal ileum or appendix (the embryologic midgut). Small-bowel adenocarcinoma, like other small bowel tumors, has a non-specific clinical manifestation. Since most of these lesions occur within 25 cm of the duodenojejunal junction, patients with pain, vomiting, and anemia should have assessment of the proximal jejunum as part of an extended upper-GI investigation. Most (70%) duodenal carcinomas are polypoid, larger lesions tend to ulcerate, and infiltrative duodenal carcinomas are relatively rare. Depending on their location, these may be identified by upper-GI endoscopy or barium studies. Carcinomas of the mesenteric small bowel are commonly constricting “apple core” lesions at the time of diagnosis. These display the typical features of GI malignancies on barium studies: shouldering; mucosal destruction; irregular luminal narrowing; and rigidity of a short segment, with variable degrees of intestinal obstruction. The main differential diagnoses for these appearances are CD, lymphoma, and leiomyosarcoma of the small bowel. CD usually involves longer segments than carcinoma, and the mucosa has a “cobblestone” appearance; lymphoma and leiomyosarcoma tend to be larger and softer tumors [13].
NSAID enterocolopathy versus CD
The largest number of adverse reactions associated with NSAIDs is related to the GI tract. In addition to the appearance of ulcers in the stomach and duodenum, ulcerations due to NSAID can occur in the small intestine. NSAID enteropathy is usually asymptomatic, although some patients present with iron deficiency anemia, perforation or strictures. Small intestinal injury from NSAIDs runs a spectrum from macroscopically undetectable increased intestinal permeability and mild mucosal inflammation to ulceration and diaphragmatic strictures. Diaphragm strictures are rare but pathognomonic of NSAID use [4,5]. There are often multiple, 2-3 mm thick septae, usually in the small intestine, which can reduce the size of the intestinal lumen to a pinhole. These diaphragm strictures are thin and easily missed on enteroclysis, where they may resemble plicae circularis [14].
German authors [15] recently reported a 39-year-old man who was treated as CD, with corticosteroid therapy firstly and then azathioprine. The patient presented with bloody diarrhea and a stenosis in the transverse colon that was histologically interpreted as “consistent with CD”. After surgical treatment of the stenosis, the episodes of bloody diarrhea persisted, and endoscopy continued to reveal erosions and ulcers in the transverse colon. Subsequent evaluation of the histological specimens by a consultant pathologist pointed to tentative diagnosis of NSAID-induced colonopathy. An analysis of the patient’s medical history revealed that he was suffering from Bechterew’s disease (ankylosing spondylitis), for which he had been taking diclofenac long term. This case history is a good example of the fact that NSAID-induced enterocolopathy is often misinterpreted as CD, and indicates a pathohistological similarity between these two diseases.
Isolated terminal ileal ulcerations
Some asymptomatic individuals may present with aphthous or small ulcerations in the TI, unaccompanied by lesions in the colon or ileocecal valve. Most of the ulcerations were surrounded by normal mucosa, regenerating epithelium, or edematous mucosa and covered by thin or faint exudates. Thus patients with isolated TI ulcerations (ITIU) in most cases do not have CD, and in some cases follow up is needed.
A recent study [16] reported 145 patients with ITIU. All of the patients were asymptomatic healthy individuals who did not take aspirin or NSAIDs and underwent colonoscopy for other indications (mostly surveillance for colorectal carcinoma). In this study [16], ITIU had completely resolved on follow-up colonoscopy in 62 of 93 patients. Only one showed a significant histological abnormality, a granulomatous lesion, and this patient was confirmed as having intestinal tuberculosis. Another patient was later diagnosed with CD, based on follow-up colonoscopic findings of typical longitudinal ulcerations of CD. The time from initial diagnosis of ITIU to confirmation of typical CD was 32 months. During the follow-up period the patients did not have any symptoms nor did they receive any treatment, except for the patient with CD. Aphthous or small ulcerations in the TI may be one of the earliest manifestations of serious diseases, such as CD and intestinal tuberculosis. Some patients with aphthous type CD later develop typical CD. In these patients, progression from aphthous lesions to overt CD requires a relatively long period of time, whereas in other patients, aphthous lesions disappear or remain unchanged on follow up. Another study [17] has reported that CD is unlikely to develop in asymptomatic individuals with isolated ileitis.
Other causes of terminal ileitis
Recent reports [18] indicate that in some patients with collagenous and lymphocytic colitis, there is inflammation in the TI. These changes include surface epithelial lymphocytosis, villous shortening, and subepithelial collagen, but not the distortion, chronic inflammation, or pyloric gland metaplasia that predominate in abnormal TI biopsies. In the few cases of microscopic colitis with TI abnormalities, the diagnosis is based on the colonic biopsies.
GI manifestations of Henoch-Schönlein purpura commonly include abdominal pain and GI bleeding as well as extraintestinal signs and symptoms. In the literature, a case has been reported of a 24-year-old man with endoscopical findings of inflammation with aphthous lesions in the TI, which is a common feature of CD [19]. The observation is that vasculitic disorders such as Henoch-Schönlein purpura can present with inflammatory lesions at TI which are indistinguishable from those of CD.
Infiltrative causes of ileitis include a number of diseases: eosinophilic gastroenteritis (EG), systemic mastocytosis, sarcoidosis and endometriosis. The endoscopic findings of EG vary from normal mucosa to mild erythema, nodularity and ulceration. Diffuse enteritis with complete loss of villi, submucosal edema, and fibrosis may be present. Multiple biopsies are required because of the patchy nature of the disease, and full-thickness surgical biopsies may be necessary if disease is confined to the muscle layer. CD can usually be differentiated by the typical architectural distortion that is not found in EG. Eosinophilic ileocolitis may be more common than originally thought and the counting of high-power microscopic fields for eosinophils may be a useful way of distinguishing eosinophilic ileocolitis from CD ileocolitis. Rarely, CD is associated with peripheral eosinophilia and/or an eosinophil-rich tissue infiltrate [20,21].
Systemic mastocytosis (SM) is a rare and heterogeneous disease characterized by various biological and clinical features with different prognosis and treatments. GI involvement includes microscopic infiltration of the liver, pancreas, and intestine by mast cells. Abdominal pain has been attributed to peptic ulcer disease, involvement of the GI tract by mast cells, mediators released by mast cells, and motility disorders. Small intestine involvement by SM caused dilatated small bowel, subocclusion and malabsorption. In one study [22] including esophagogastroduodenal and small bowel follow-through in 78 patients with SM, the most frequently observed lesion was 1-3 mm nodules in bowel mucosa, probably related to edema. In a second study regarding 14 patients, 57% displayed thickening of intestinal mucosa, nodular, or polypoid lesions [23]. These results suggest that neoplastic mast cells in patients with SM can infiltrate the mucosa throughout the GI tract and this infiltration can lead to symptoms and findings that can mimic inflammatory bowel disease.
In patients with sarcoidosis and suspected ileitis, ileocolonoscopy with biopsy revealing noncaseating granulomas containing multinucleated giant cells is nearly diagnostic. Precise interpretation of ileal biopsies is crucial because CD, mycobacterial infections, histoplasmosis and lymphoma are granulomatous conditions that mimic sarcoidosis.
Although not very frequent, endometriosis is an important differential diagnosis of CD in young females. It has been reported that endometriosis can cause intestinal obstruction, and the diagnosis is often made postoperatively.
In conclusion, a thorough diagnostic work-up should be performed for every patient with affected TI. Differential diagnosis of terminal ileitis is sometimes extremely difficult, and not every inflammation of TI is CD. Complete colonoscopy with ileoscopy and TI biopsies are of key importance in such cases.
Biography
University of Belgrade, Serbia
Footnotes
Conflict of Interest: None
References
- 1.Jeong SH, Lee KJ, Kim YB, et al. Diagnostic value of terminal ileum intubation during colonoscopy. J Gastroenterol Hepatol. 2008;23:51–55. doi: 10.1111/j.1440-1746.2007.05151.x. [DOI] [PubMed] [Google Scholar]
- 2.Cherian S, Singh P. Is routine ileoscopy useful? An observational study of procedure times, diagnostic yield, and learning curve. Am J Gastroenterol. 2004;99:2324–2329. doi: 10.1111/j.1572-0241.2004.40730.x. [DOI] [PubMed] [Google Scholar]
- 3.Goldstein N, Dulai M. Contemporary morphologic definition of backwash ileitis in ulcerative colitis and features that distinguish it from Crohn disease. Am J Clin Pathol. 2006;126:365–376. doi: 10.1309/UAXMW3428PGN9HJ3. [DOI] [PubMed] [Google Scholar]
- 4.Haskell H, Andrews CW, Reddy SI, et al. Pathologic features and clinical significance of “backwash” ileitis in ulcerative colitis. Am J Surg Pathol. 2005;29:1472–1481. doi: 10.1097/01.pas.0000176435.19197.88. [DOI] [PubMed] [Google Scholar]
- 5.De Hertogh G, Geboes K. Crohn's disease and infections: a complex relationship. MedGenMed. 2004;6:14. [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma MP, Bhatia V. Abdominal tuberculosis. Indian J Med Res. 2004;120:305–315. [PubMed] [Google Scholar]
- 7.Lee YJ, Yang SK, Byeon JS, et al. Analysis of colonoscopic findings in the differential diagnosis between intestinal tuberculosis and Crohn's disease. Endoscopy. 2006;38:592–597. doi: 10.1055/s-2006-924996. [DOI] [PubMed] [Google Scholar]
- 8.Matsumoto T, Iida M, Matsui T, et al. Endoscopic findings in Yersinia enterocolitica enterocolitis. Gastrointest Endosc. 1990;36:583–587. doi: 10.1016/s0016-5107(90)71169-8. [DOI] [PubMed] [Google Scholar]
- 9.Lavallee C, Laufer B, Pepin J, et al. Fatal Clostridium difficile enteritis caused by the BI/NAP1/027 strain: a case series of ileal C difficile infections. Clin Microbiol Infect. 2009;15:1093–1099. doi: 10.1111/j.1469-0691.2009.03004.x. [DOI] [PubMed] [Google Scholar]
- 10.Ganly I, Shouler PJ. Focal lymphoid hyperplasia of the terminal ileum mimicking Crohn's disease. Br J Clin Pract. 1996;50:348–349. [PubMed] [Google Scholar]
- 11.Mukhopadhyay S, Harbol T, Floyd FD, et al. Polypoid nodular lymphoid hyperplasia of the terminal ileum. Arch Pathol Lab Med. 2004;128:1186–1187. doi: 10.5858/2004-128-1186-PNLHOT. [DOI] [PubMed] [Google Scholar]
- 12.Hoeffel C, Crema MD, Belkacem A, et al. Multi-detector row CT: spectrum of diseases involving the ileocecal area. Radiographics. 2006;26:1373–1390. doi: 10.1148/rg.265045191. [DOI] [PubMed] [Google Scholar]
- 13.Posner MC, Vokes EE, Weichselbaum RR. Hamilton, London: BC Decker Inc; 2002. American Cancer Society. Atlas of clinical oncology cancer of the upper gastrointestinal tract. [Google Scholar]
- 14.Adebayo D, Bjarnason I. Is nonsteroidal anti-inflammatory drug (NSAID) enteropathy clinically more important than NSAID gastropathy? Postgrad Med J. 2006;82:186–191. doi: 10.1136/pgmj.2005.039586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stolte M, Hartmann FO. Misinterpretation of NSAID-induced colopathy as Crohn's disease. Z Gastroenterol. 2010;48:472–475. doi: 10.1055/s-0028-1109760. [DOI] [PubMed] [Google Scholar]
- 16.Chang HS, Lee D, Kim JC, et al. Isolated terminal ileal ulcerations in asymptomatic individuals: natural course and clinical significance. Gastrointest Endosc. 2010;72:1226–1232. doi: 10.1016/j.gie.2010.08.029. [DOI] [PubMed] [Google Scholar]
- 17.Courville EL, Siegel CA, Vay T, et al. Isolated asymptomatic ileitis does not progress to overt Crohn disease on long term follow-up despite features of chronicity in ileal biopsies. Am J Surg Pathol. 2009;33:1341–1347. doi: 10.1097/PAS.0b013e3181ad25b6. [DOI] [PubMed] [Google Scholar]
- 18.Sapp H, Ithamukkala S, Brien TP, et al. The terminal ileum is affected in patients with lymphocytic or collagenous colitis. Am J Surg Pathol. 2002;26:1484–1492. doi: 10.1097/00000478-200211000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Scherbaum WA, Kaufmann R, Vogel U, et al. Henoch-Schönlein purpura with ileitis terminalis. Clin Investig. 1993;71:564–567. doi: 10.1007/BF00208482. [DOI] [PubMed] [Google Scholar]
- 20.Dilauro S, Crum-Cianflone NF. Ileitis: when it is not Crohn's disease. Curr Gastroenterol Rep. 2010;12:249–258. doi: 10.1007/s11894-010-0112-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daneshjoo R, J Talley N. Eosinophilic gastroenteritis. Curr Gastroenterol Rep. 2002;4:366–372. doi: 10.1007/s11894-002-0006-2. [DOI] [PubMed] [Google Scholar]
- 22.Johnson AC, Johnson S, Lester PD, et al. Systemic mastocytosis and mastocytosis-like syndrome - radiologic features of gastrointestinal manifestations. South Med J. 1988;81:729–733. doi: 10.1097/00007611-198806000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Sokol H, Georgin-Lavialle S, Grandpeix-Guyodo C, et al. Gastrointestinal involvement and manifestations in systemic mastocytosis. Inflamm Bowel Dis. 2010;16:1247–1253. doi: 10.1002/ibd.21218. [DOI] [PubMed] [Google Scholar]


