Abstract
Background
The changing epidemiology of a disease often provides valuable insight into possible etiopathogenic mechanisms. There have been significant changes over the last several decades in disease manifestations of the foregut in Western Europe, North America and Asia. This time trend analysis was carried out to determine if any changes have occurred in the prevalence of diseases of the upper gastrointestinal tract in Nigeria.
Method
Records of patients who underwent upper gastrointestinal endoscopy during two time periods (1995 to 1999 and 2006 to 2010) in Enugu, South-East Nigeria were analyzed with regard to biodata of patients, indications for upper gastrointestinal endoscopy and endoscopic findings.
Results
During the two time periods, 1,365 patients had upper gastrointestinal endoscopy (575 patients in the period 1995-1999 and 790 in the period 2006-2010). Dyspepsia was the commonest indication for upper gastrointestinal endoscopy for both periods (81.9% and 72.9%, respectively; p= 0.9052). Heartburn and dysphagia were more frequent during the second time period (p<0.0001). Duodenal ulcer was more common in the first time period (p<0.0001), while esophagitis, gastric ulcer and bile reflux were significantly more common in the second period (p<0.0001, p=0.0007 and p=0.0019, respectively).
Conclusion
Over the 15-year period, the prevalence of duodenal ulcer has declined while that of gastric ulcer has increased. There has also been an increase in the prevalence of gastroesophageal reflux disease. Putative explanations for this trend may include widespread availability and use of very potent acid suppressant drugs, increasing use of non steroidal anti-inflammatory drugs, change towards western diet and increasing obesity.
Keywords: Trends, gastrointestinal diseases, GERD, Nigeria
Introduction
Epidemiology of disease changes over time with changes in socio-economic status, culture and health care systems. The changing epidemiology of a disease often provides valuable insight as to possible etiopathogenic mechanisms. When such changes take place over a relatively short interval of time, they point to the influence of exogenous factors. The past four decades have witnessed significant changes in the epidemiology of diseases of the foregut across the world.
In the adult Caucasian population of North America and Europe, a decreasing prevalence of duodenal ulcer (DU) has been noted during the last 4 decades [1]. Similar observations have been made in the Asia-Pacific region of the world [2]. At the same time, gastroesophageal reflux disease (GERD) has been reported to be increasing in Western countries [3,4] as well as in the Asia-Pacific region [5,6].
Upper gastrointestinal endoscopy is an accurate and safe method of diagnosing diseases of the esophagus, stomach and duodenum. It was introduced in a few centers in Nigeria in the 1980s and with the passage of time more health institutions have acquired the facility. There is a scarcity of published data on time trends of gastrointestinal disease in Africa. In Nigeria, no such study has been conducted. The objective of this study was to determine whether there have been any temporal changes in disease manifestations in the upper gastrointestinal (UGI) tract in Nigeria during a 15-year period.
Materials and Methods
The study was carried out at the gastrointestinal endoscopy unit of the University of Nigeria Teaching Hospital Ituku/Ozalla, Annunciation Specialist Hospital Emene and Uzoma Specialist Hospital Trans Ekulu Enugu. The endoscopy records of patients who underwent first UGI endoscopy during 2 time periods (1995 to 1999 and 2006 to 2010) were examined. For the first time period only records from the University of Nigeria Teaching Hospital were analyzed because it was the only center that provided endoscopy services during the period. For the second time period records from the three centers were analyzed.
Information extracted from the records included patients’ biodata, indications for UGI endoscopy and endoscopic findings. The results are expressed as mean and proportions. Differences between means were determined using Students’ t-test. The χ2 test was used to compare proportion. P value of less than 0.05 was considered statistically significant.
Results
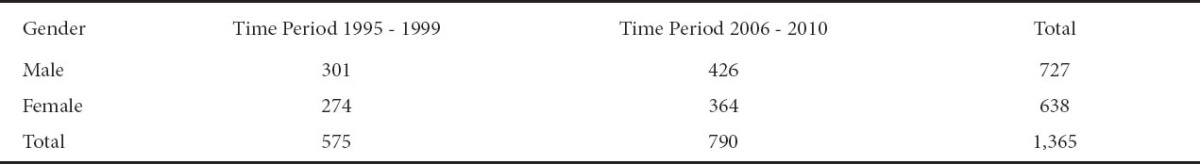
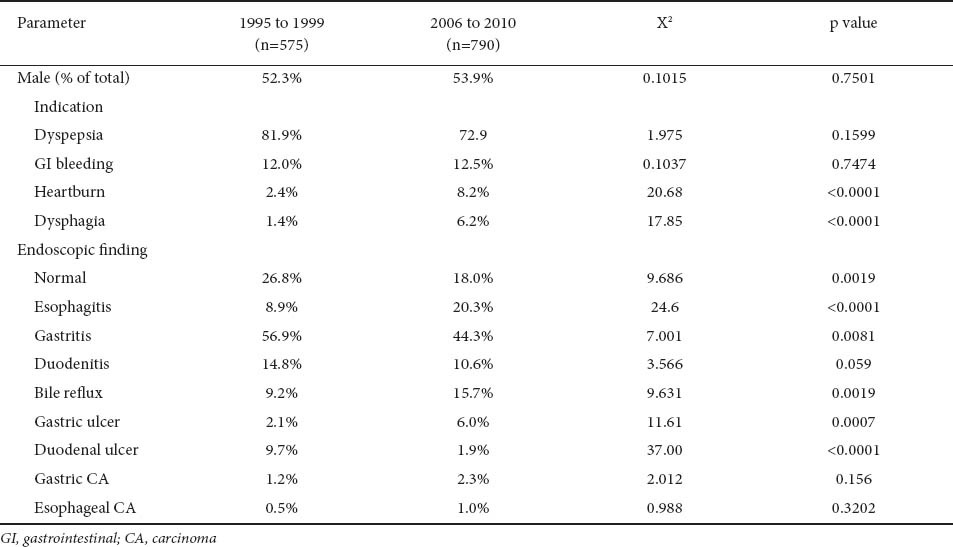
One thousand, three hundred and sixty five patients had UGI endoscopy during the two periods (575 for the period 1995 to 1999, and 790 for the period 2006 to 2010). Table 1 shows the gender distribution of the patients. The mean age of patients in the first time period was 43.3±13.3 years while the mean age of patients in the second time period was 47.2±15.3 years. The difference between the means was not statistically significant (t=0.1347, p=0.9052). Dyspepsia accounted for 81.9% and 72.9% of indications for UGI endoscopy in the two periods. The difference between the proportions was not statistically significant (χ2=1.975, p=0.1599). Heartburn and dysphagia were significantly more frequent as indications for UGI endoscopy in the second time period compared to the first period (p<0.0001 in each case).
Table 1.
Gender distribution of patients in the 2 time periods, 1995-1999 and 2006-2010
Regarding endoscopic findings, only normal endoscopic findings, gastritis and duodenal ulcer were more frequent in the first time period compared with the second period (p=0.0019, 0.0081 and <0.0001, respectively). The endoscopic findings that were significantly more frequent in the second time period were esophagitis (p<0.0001), bile reflux (p=0.0019) and gastric ulcer (p=0.0007). Table 2 illustrates a comparison of selected parameters in the 2 time periods.
Table 2.
Comparisons between the two time periods, 1995-1999 and 2006-2010
Discussion
For the 2 time periods, the dominant indication for UGI endoscopy remained dyspepsia. However, heartburn and dysphagia were significantly more frequent during the second time period (2006 to 2010). This is an important observation with a suggestion that diseases of the esophagus assumed greater prominence during the period. The same trend has since been reported in the western world and Asia [3-6]. Similarly, with regard to endoscopic findings, the prevalence of esophagitis increased from 8.9% in the first time period to 20.3% in the second period (P<0.0001). GERD was previously uncommon in Asia, but has recently increased to attract public health attention [7]. Similar reasons have been advanced for this observation in the two regions. These are aging population, the obesity epidemic and associated changes in diet and physical activity [8].
The effect of Helicobacter pylori (H. pylori) infection of the stomach on the prevalence of GERD remains an unresolved issue. Despite the negative association observed in cross-sectional studies, the results are less consistent in longitudinal studies of H. pylori eradication. The conflicting observations have been linked to differences in anatomical location of gastric inflammation [9], virulence of the organism [10,11], and genetic characteristics of the host [12]. In a meta-analysis of pooled data from 7 randomized controlled trials and 5 cohort studies comparing the prevalence of GERD among patients free from GERD at baseline with H. pylori eradication vs. those with persistent infection, there was no significant difference in either the risk of developing erosive or symptomatic GERD between the two groups of patients. There was no significant heterogeneity among the studies and the results were consistent in various subgroup and sensitivity analyses, suggesting high quality and consistency. Interestingly, there was a two-fold higher risk for development of erosive GERD in a subgroup of patients with peptic ulcer disease in cohort studies (odds ratio: 2.04, 95% C.I.: 1.08-3.85; p=0.03) [13].
In recent years it has been recognized that H. pylori eradication may affect gastric secretory function other than acid secretion. The plasma level of ghrelin (an appetite stimulant produced by the gastric body) is lower in H. pylori-infected patients compared to healthy controls. H. pylori eradication leads to recovery of ghrelin secreting cells and increase in ghrelin levels [14-16]. This might increase the calorie intake and lead to weight gain, a recognized risk factor for GERD [17,18].
In the case of Nigeria, there appears to be an increase in the prevalence of GERD in line with the global trend, but the explanations may not be exactly the same as in the developed world. Life expectancy cannot be said to have improved but the drift towards western diet, increasing body mass index (BMI) and obesity may explain this trend. The prevalence of obesity and obesity-related morbidities in developing countries is relatively low, but is changing rapidly [19-23].
A reduction in the prevalence of duodenal ulcer (DU) was clearly demonstrated in this study. The same trend has since been reported across the world in the last 4 decades [1,2]. In the Western world and Asia the explanations that have been put forward for this trend are decreasing prevalence of H. pylori infection occasioned by improved hygiene and eradication of the organism from infected persons. In this study, H. pylori status was not part of the analysis because it was not consistently determined in the patients, and, where it was determined, various methods were used resulting in non-comparable data. However, in Nigeria, the use of proton pump inhibitors (PPIs) is indiscriminate. There are also no guidelines in place and eradication treatments are subject to abuse. Most patients would have used these drugs before presenting to the gastroenterologist. The result is that the prevalence of H. pylori cannot be said to be decreasing. However, the indiscriminate use of PPIs may have reduced the prevalence of DUs albeit unaltered tendency for recurrence. The status of H. pylori infection in Nigerian patients requires further studies.
In conjunction with the drop in the prevalence of DU over time, an increase in the prevalence of gastric ulcer (GU) is also noticed. The explanation for this may be the increasing use of non steroidal anti-inflammatory drugs (NSAIDs) for various inflammatory and painful conditions [24]. Another possible explanation is the fact that the same period witnessed a rise in the prevalence of bile reflux. It is possible that patients who previously had DUs which healed as a result of the use of potent acid suppressant drugs are now left with deformities of the pylorus and duodenal cap with resultant secondary duodenogastric reflux. When bile gets into the stomach, it excites a nonspecific response which may eventuate in gastric ulcer. Similarly, gastric cancer prevalence increased from 1.2% to 2.3%. The difference was not statistically significant but may be related to several factors including duodenogastric reflux.
Esophageal cancer showed an increase in prevalence from 0.5% to 1.0% over the period under review. The increase, though not statistically significant, is a very important observation. It is possible that with time passing, the rising prevalence of GERD, the westernization of diet and ensuing obesity may lead to more cases of esophageal adenocarcinoma.
Normal endoscopic findings were more frequent in the first time period compared with the second period (p=0.0019). The reason for this may be related to the fact that current endoscopes are able to distinguish subtle mucosal abnormalities. It is also possible that the endoscopists making the assessments might have acquired more competence and experience over time.
The limitations of this study include the non inclusion of H. pylori infection in the analysis, the retrospective design and non standardization of the diagnosis of certain endoscopic lesions such as esophagitis. The Los Angeles (LA) classification of esophagitis which utilizes visible mucosal breaks as the minimum evidence of esophagitis is the most widely used system. Other findings such as erythema at the gastroesophageal junction or an irregular Z-line have proven not to be reliable findings for the diagnosis of reflux esophagitis [25,26]. This is the basis for including grade M (minimal esophagitis) in some modified versions of the LA classification [27]. A previous study in Nigeria showed a high prevalence of grade M esophagitis and a relative rarity of severe esophagitis [28]. Another important limitation of this study is the fact that the patients whose records were analyzed might not have been representative of the general population since economic factors influence health-seeking behavior of patients.
In conclusion, over a 15-year period, there has been a noticeable change in disease manifestation in the UGI in Nigeria. A decline in the prevalence of DU and an increase in the prevalence of GU have been observed. There has also been an increase in the prevalence of GERD over the period. This trend may be related to widespread and indiscriminate use of potent acid suppressants, changes in diet, sedentary life style and increasing obesity.
Summary Box
What is already known:
The changing epidemiology of a disease often provides valuable insight as to possible etiopathogenic mechanisms
The past 4 decades have witnessed a decrease in the prevalence of duodenal ulcer (DU) in North America, Western Europe and Asia
There has also been an increase in the prevalence of gastroesophageal reflux disease (GERD) over the same period in the same regions
What the new findings are:
During a fifteen year period in Nigeria, there have been a decrease in the prevalence of DU and an increase in the prevalence of gastric ulcer
There has also been an increase in the prevalence of GERD
Possible explanations for this trend in Nigeria include widespread and indiscriminate use of acid suppressants, changes in diet, sedentary lifestyle and increasing obesity
Biography
Teaching Hospital Ituku, Ozalla, Nigeria
Footnotes
Conflict of Interest: None
References
- 1.El-Serag HB, Sonnenberg A. Opposing time trends of peptic ulcer and reflux disease. Gut. 1998;43:327–333. doi: 10.1136/gut.43.3.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wong SN, Sollano JD, Chan MM, et al. Changing trends in peptic ulcer prevalence in a tertiary care setting in the Philippines: a seven-year study. J Gastroenterol Hepatol. 2005;20:628–632. doi: 10.1111/j.1440-1746.2005.03719.x. [DOI] [PubMed] [Google Scholar]
- 3.Sonnenberg A. Temporal trends and geographical variations of peptic ulcer disease. Aliment Pharmacol Ther. 1995;9(Suppl 2):3–12. [PubMed] [Google Scholar]
- 4.Sharma P, Wani S, Romero Y, Johnson D, Hamilton F. Racial and geographical issues in gastroesophageal reflux disease. Am J Gastroenterol. 2008;103:2669–2680. doi: 10.1111/j.1572-0241.2008.02089.x. [DOI] [PubMed] [Google Scholar]
- 5.Goh KL. Changing trends in gastrointestinal disease in the Asia-Pacific region. J Dig Dis. 2007;8:179–185. doi: 10.1111/j.1751-2980.2007.00304.x. [DOI] [PubMed] [Google Scholar]
- 6.Fujimoto K. Prevalence and epidemiology of gastroesophageal reflux disease in Japan. Aliment Pharmacol Ther. 2004;20(Suppl 8):5–8. doi: 10.1111/j.1365-2036.2004.02220.x. [DOI] [PubMed] [Google Scholar]
- 7.Goh KL. Gastroesophageal reflux disease in Asia. A historical perspective and present challenges. J Gastroenterol Hepatol. 2011;26(Suppl 1):2–10. doi: 10.1111/j.1440-1746.2010.06534.x. [DOI] [PubMed] [Google Scholar]
- 8.Lewis JV. Gastroesophageal reflux disease and obesity. South Med J. 2009;102:995–996. doi: 10.1097/SMJ.0b013e3181b666e5. [DOI] [PubMed] [Google Scholar]
- 9.Kamada T, Haruma K, Kawaguchi H, Yoshihara M, Sumii K, Kajiyama G. The association between antral G and D cells and mucosal inflammation, atrophy and Helicobacter pylori infection in subjects with normal mucosa, chronic gastritis and duodenal ulcer. Am J Gastroenterol. 1998;93:748–752. doi: 10.1111/j.1572-0241.1998.218_a.x. [DOI] [PubMed] [Google Scholar]
- 10.Sharma P, Vakil N. Helicobacter pylori and reflux disease. Aliment Pharmacol Ther. 2003;17:297–305. doi: 10.1046/j.1365-2036.2003.01428.x. [DOI] [PubMed] [Google Scholar]
- 11.Somi MH, Fattahi E, Fouladi RF, Kavimi M, Bonyadi R, Baballou Z. An inverse relation between CagA+ strains of Helicobacter pylori infection and risk of erosive GERD. Saudi Med J. 2008;29:393–396. [PubMed] [Google Scholar]
- 12.Chourasia D, Achyut BR, Tripathi S, Mittal B, Mittal RD, Ghoshal UC. Genotypic and functional roles of IL-1B and IL-1RN on the risk of gastroesophageal reflux disease: the presence of IL-1B511*T/IL-1RN*1(T1) haplotype may protect against the disease. Am J Gastroenterol. 2009;104:2704–2713. doi: 10.1038/ajg.2009.382. [DOI] [PubMed] [Google Scholar]
- 13.Yaghoobi M, Farrokhyar F, Yuan Y, Hunt RH. Is there an increased risk of GERD after Helicobacter pylori eradication? A meta-analysis. Am J Gastroenterol. 2010;105:1007–1013. doi: 10.1038/ajg.2009.734. [DOI] [PubMed] [Google Scholar]
- 14.Isomoto H, Nakazato M, Ueno H, et al. Low plasma ghrelin levels in patients with Helicobacter pylori-associated gastritis. Am J Med. 2004;117:429–432. doi: 10.1016/j.amjmed.2004.01.030. [DOI] [PubMed] [Google Scholar]
- 15.Nwokolo CU, Freshwater DA, O’Hare P, Randeva HS. Plasma ghrelin following cure of Helicobacter pylori. Gut. 2003;52:637–640. doi: 10.1136/gut.52.5.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tatsuguchi A, Miyake K, Gudis K, et al. Effect of Helicobacter pylori infection on ghrelin expression in human gastric mucosa. Am J Gastroenterol. 2004;99:2121–2127. doi: 10.1111/j.1572-0241.2004.30291.x. [DOI] [PubMed] [Google Scholar]
- 17.Moki F, Kusano M, Mizuide M, et al. Association between reflux esophagitis and features of the metabolic syndrome in Japan. Aliment Pharmacol Ther. 2007;26:1069–1075. doi: 10.1111/j.1365-2036.2007.03454.x. [DOI] [PubMed] [Google Scholar]
- 18.Wu JC, Mui LM, Cheung CM, Chan Y, Sung JJ. Obesity is associated with lower esophageal sphincter relaxation. Gastroenterology. 2007;132:883–889. doi: 10.1053/j.gastro.2006.12.032. [DOI] [PubMed] [Google Scholar]
- 19.Akinkugbe OO. Non-communicable diseases in Nigeria, the next epidemics: Nigeria preparedness. Third Biennial Abayomi Bamidele memorial lecture. Niger J Clin Pract. 2000;3:37–42. [Google Scholar]
- 20.Ilo GUP, Amadi AN, Nwankwo BO, Ugwu VC. Obesity in adult Nigerians: a study of its pattern and common primary co-morbidities in a rural mission general hospital in Imo State, South-East Nigeria. Niger J Clin Pract. 2011;14:212–218. doi: 10.4103/1119-3077.84019. [DOI] [PubMed] [Google Scholar]
- 21.Popkin BM. The nutrition transition in low income countries: an emerging crisis. Nutr Rev. 1994;52:285–295. doi: 10.1111/j.1753-4887.1994.tb01460.x. [DOI] [PubMed] [Google Scholar]
- 22.Akpa MR, Mato CN. Obesity in Nigeria: current trends and management. Niger Med Pract. 2008;54:11–15. [Google Scholar]
- 23.Ogunjimi LO, Ikorok MM, Olayinka YO. Prevalence of obesity among Nigerian nurses: the Akwa Ibom State experience. Int NGO J. 2010;5:45–49. [Google Scholar]
- 24.Awofisayo OS, Awofisayo OA, Iferi II, Akpan OE. The pattern of sale and use of non-steroidal anti-inflammatory drugs in rural and urban centres in Nigeria. Trop J Pharma Res. 2008;7:1013–1018. [Google Scholar]
- 25.Vieth M, Haringsma J, Delarive J, et al. Red streaks in the esophagus in patients with reflux disease: Is there a histopathological correlate? Scand J Gastroenterol. 2001;36:1123–1127. doi: 10.1080/00365520152584725. [DOI] [PubMed] [Google Scholar]
- 26.Bytzer P, Haveland T, Hansen JM. Interobserver variation in endoscopic diagnosis of reflux esophagitis. Scand J Gastroenterol. 1993;28:119–125. doi: 10.3109/00365529309096057. [DOI] [PubMed] [Google Scholar]
- 27.Hongo M. Minimal changes in reflux esophagitis: red ones and white ones. J Gastroenterol. 2006;41:95–99. doi: 10.1007/s00535-006-1775-4. [DOI] [PubMed] [Google Scholar]
- 28.Nwokediuko S, Ijoma U, Obienu O, Agunyenwa C. Gastroesophageal reflux disease: a clinical and endoscopic study of Nigerian patients. Internet J Gastroenterol. 2009:8. [Google Scholar]


