Abstract
Choledochal cysts are uncommon congenital anomalies of the biliary tree. We report a 25-year-old female who presented with palpable abdominal lump, jaundice and fever. She was diagnosed with a huge, type IVA choledochal cyst with enormous asymmetric cystic dilatation of extrahepatic segment of left hepatic duct with the help of ultrasound and magnetic resonance cholangiopancreatography (MRCP). The patient experienced complete recovery after total resection of the entire extrahepatic cyst and Roux-en-Y hepaticojejunostomy at the level of the hilum. We discuss the clinical features, imaging characteristics and treatment of this giant Todani’s type IVA choledochal cyst.
Keywords: choledochal cyst, hepaticojejunostomy, magnetic resonance cholangiopancreticography, cholangitis
Introduction
Choledochal cysts are congenital anomalies of the bile ducts and are defined as abnormal, disproportionate, cystic dilatations of the biliary duct. The incidence of bile duct cysts ranges between 1 in 13,000 to 1 in 2 million births, and are encountered more frequently in females [1]. More than 60% present during the first year of life. About 20% present in adulthood [1]. The exact etiology remains unknown, but it is believed to be congenital in origin. The most widely accepted theory for the formation of choledochal cysts is related to an anomalous connection between the biliary and pancreatic ductal systems [2]. Type IVA choledochal cyst is the second most common after type I, characterized by multiple cystic dilatations of the intra and extrahepatic biliary channels [1]. We describe a case of an unusual variety of adult type IVA choledochal cyst which showed massive cystic dilatation of the common bile duct (CBD) and the extrahepatic portion of the left hepatic duct.
Case report
A 25-year-old female was referred to our GI Surgery Unit for unexplained fever, jaundice, and right upper quadrant abdominal pain for the last 10 days. There was a past history of similar episodes over the last year. At presentation, she had jaundice, fever and large soft cystic swelling occupying the entire upper abdomen. Laboratory investigations revealed total bilirubin 8 mg/dL, alkaline phosphatase 1230 U/L, ALT 200 U/L and AST 93 U/L. The ultrasonographic examination demonstrated a huge thick walled cystic lesion with internal echogenic particles and septations that extended from the subhepatic area to the left hypochondrium, separate from liver. There were cystic dilatations of intrahepatic ducts. An MRCP examination disclosed a huge cystic dilatation of the common bile duct measuring 12 cm in diameter (Fig. 1a). Another separate, large-septated cystic lesion with homogenous fluid signal intensity, measuring 12 cm×10 cm×9 cm (Fig. 1b), was seen at porta hepatis contiguous with an extrahepatic segment of left hepatic duct extending to the left hypochondrium. With these findings, the provisional diagnosis of a huge type, IVA choledochal cyst with enormous tortuous dilatation of the extrahepatic segment of the left hepatic duct was considered.
Figure 1.
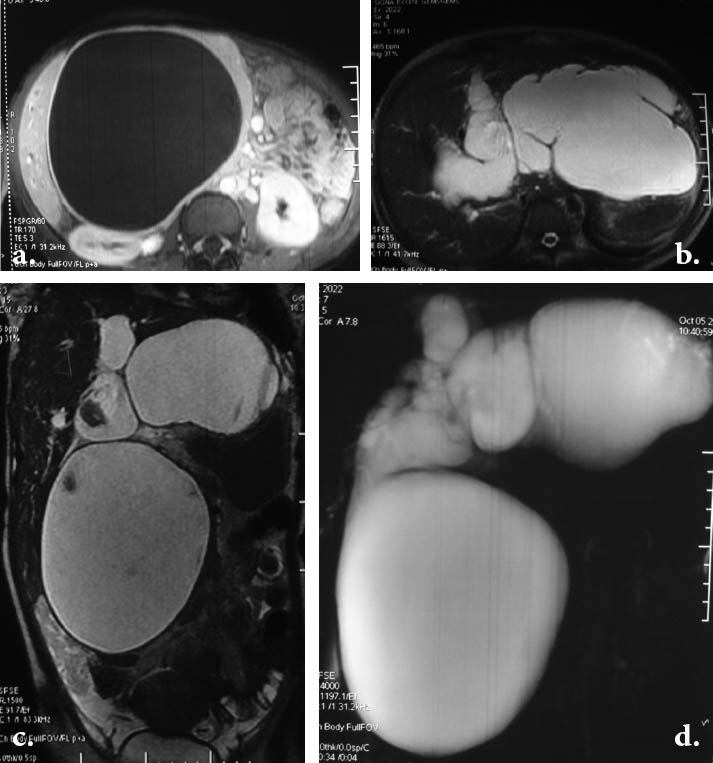
a. Post-gadolinium axial T1W FSPGR image shows large cystic mass at the porta hepatis compressing the right kidney and other adjacent structures. b. Axial T2-weighted image above the level of confluence shows dilated left and right intrahepatic ducts with massive cystic dilatation of extrahepatic segment of the left hepatic duct extending to the left hypochondrium. The peripheral portions of intrahepatic ducts are not involved. c. Coronal T2-weighted image showing a huge cystic dilatation of the common bile duct extending to subhepatic area and another cyst in the epigastrium contiguous with the left hepatic duct. d. Projective MR image showing the bizarre cystic dilatation of the entire biliary tree.
Percutaneous transhepatic biliary drainage was done as the patient went into toxic cholangitis and she was not fit for endoscopic retrograde cholangiopancreaticography (ERCP). Subsequently, cholangitis subsided and she was taken up for the surgery after optimization of the coagulation and nutritional status. Intraoperative findings were a large thick walled folded cyst measuring approximately 15 cm arising from the extrahepatic segment of left hepatic duct in continuation with a huge dilatation of CBD confirming the finding of MRCP.
The extrahepatic component of the cyst was excised and biliary-enteric flow was re-established through a wide mucosa to mucosa Roux-en-Y hepaticojejunostomy at the level of the hilum. At 10 months of follow up, the patient was doing well.
Discussion
Alonso-Lej et al published the first systematic description of choledochal cysts in 1959 [3]. He classified choledochal cysts into three types. This classification was further advanced by Todani et al and includes five major types and several subtypes [4]. Type I cysts are a dilatation of the extrahepatic bile duct. These are the most common type and seen in 75% to 85% of cases [5]. Type I cysts may be further classified as cystic (IA), focal (IB), or fusiform (IC). Type II cyst is diverticulum of the CBD. Type III is represented by a cystic dilatation of the intramural portion of the CBD known as choledochoceles. Type IVA lesions involve both the intra and extrahepatic portions of the bile ducts and type IVB are multiple cysts limited to the extrahepatic bile ducts. Type V is synonymous with Caroli disease, which involves abnormalities of the intrahepatic bile ducts resulting in multiple segmental intrahepatic cystic biliary dilatations. Although type I cysts are the most common in patients of all ages, type IVA cysts are more prevalent in adults [1]. The size of choledochal cyst varies, and rarely exceeds 9 cm [6].
Although ultrasound is the best initial method for evaluating the entire intrahepatic and extrahepatic biiary system and gallbladder, it may not always be able to precisely identify that the cyst originates in the bile duct, especially larger cysts as in our case [7]. In this case, the presence of intrahapatic biliary dilatation adds an important clue to the diagnosis of choledochal cyst. MRCP is the current “gold standard” in the imaging of choledochal cysts [8]. The other radiological differential of a huge cyst at porta hepatis includes pseudopancreatic cyst, hepatic cyst, mesenteric and omental cyst [7].
The presentation in adults is often vague and nonspecific. The classic triad of intermittent jaundice, abdominal mass, and pain, rarely seen in adults, was present in our case [9]. The choledochal cyst, particularly the large cyst, can lead to serious complications if left untreated. These include cysto-lithiasis, cholangitis, pancreatitis, cirrhosis, hepatic fibrosis, portal hypertension, and development of cholangiocarcinoma [10]. The incidence of malignant transformation is reported to be 2.5–26% [11]. This risk has been reported to be greatest in patients with intrahepatic biliary involvement [12].
The extent of the resection in type IV-A cysts is controversial. Clearly, when the intrahepatic cysts are widespread, they cannot be excised; however, when the intrahepatic disease is localized, it would seem reasonable to perform the relevant partial hepatectomy [8]. For the same reason, we excised only the extrahepatic portion of choledochal cyst and biliary-enteric flow was re-established through a wide mucosa to mucosa Roux-en-Y hepaticojejunostomy at the level of the hilum. In older patients with repeated cholangitis and marked pericystic inflammation, this disease may be best managed with resection of the anterolateral part of the cyst followed by an endocystic resection of the lining, leaving the back wall adjacent to the portal vein in place, as reported by Lilly in 1977, but we were able to excise the entire extrahepatic cyst [13].
In conclusion type IVA choledochal cyst may rarely demonstrate atypical features, namely, massive asymmetric cystic dilatation of extrahepatic segment of left hepatic duct and huge size of CBD, posing a diagnostic dilemma. The use of MRCP is highly recommended to reach the definitive diagnosis and plan surgical excision. Due to bilateral intrahepatic ductal dilatation, it is not possible to excise the entire cyst thus extrahepatic excision of the cyst is the treatment of choice.
Biography
Indira Gandhi Institute of Medical Sciences, India
Footnotes
Conflict of Interest: None
References
- 1.Soreide K, Korner H, Havnen J, et al. Bile duct cysts in adults. Br J Surg. 2004;91:1538–1548. doi: 10.1002/bjs.4815. [DOI] [PubMed] [Google Scholar]
- 2.Babbitt DP. Congenital choledochal cysts: new etiological concept based on anomalous relationships of the common bile duct and pancreatic bulb. Ann Radiol (Paris) 1969;12:231–240. [PubMed] [Google Scholar]
- 3.Alonso-Lej F, Rever W, Pessagno D. Congenital choledochal cysts, with report of 2, and an analysis of 94 cases. Int Surg. 1959;108:1–30. [PubMed] [Google Scholar]
- 4.Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263–269. doi: 10.1016/0002-9610(77)90359-2. [DOI] [PubMed] [Google Scholar]
- 5.Yamaguchi M. Congenital choledochal cyst. Analysis of 1433 patients in the Japanese literature. Am J Surg. 1980;140:653–657. doi: 10.1016/0002-9610(80)90051-3. [DOI] [PubMed] [Google Scholar]
- 6.Chokshi NK, Guner YS, Aranda A, Shin CE, Ford HR, Nguyen NX. Laparoscopic choledochal cyst excision: lessons learned in our experience. J Laparoendosc Adv Surg Tech A. 2009;19:87–91. doi: 10.1089/lap.2008.0045. [DOI] [PubMed] [Google Scholar]
- 7.Kim OH, Chung HJ, Choi BG. Imaging of the choledochal cyst. Radiographics. 1995;15:69–88. doi: 10.1148/radiographics.15.1.7899614. [DOI] [PubMed] [Google Scholar]
- 8.Metcalfe MS, Wemyss-Holden SA, Maddern GJ. Management dilemmas with choledochal cysts. Arch Surg. 2003;138:333–339. doi: 10.1001/archsurg.138.3.333. [DOI] [PubMed] [Google Scholar]
- 9.Lipsett PA, Pitt HA, Colombani PM, Boitnott JK, Cameron JL. Choledochal cyst disease. A changing pattern of presentation. Ann Surg. 1994;220:644–652. doi: 10.1097/00000658-199411000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Atkinson H, Fischer C, de Jong C, Madhavan KK, Parks RW, Garden OJ. Choledochal cysts in adults and their complications. HPB Surg. 2003;5:105–110. doi: 10.1080/13651820310001144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fieber SS, Nance FC. Choledochal cyst neoplasm: A comprehensive review of 106 cases and presentation of two original cases. Am Surg. 1997;63:982–987. [PubMed] [Google Scholar]
- 12.Bismuth H, Krissat J. Choledochal cystic malignancies. Ann Oncol. 1999;10:94–98. [PubMed] [Google Scholar]
- 13.Lilly JR. Total excision of choledochal cyst. Surg Gynecol Obstet. 1978;146:254–256. [PubMed] [Google Scholar]


