Abstract
Objective
Adult intussusception (AI) is a rare entity and differs from childhood intussusception in its presentation, etiology, and treatment. It accounts for 1/30,000 of all hospital admissions, 1/1300 of all abdominal operations, 1/30-1/100 of all cases operated for intestinal obstruction and one case of AI for every 20 childhood ones. This study was designed to review the mode of presentation, diagnosis and appropriate treatment and finally the etiology of cases presenting in our hospital over a period of 6 years.
Methods
A retrospective review of 15 cases of intussusceptions in individuals older than 18 years presenting to a tertiary referral center of South India during a period of 6 years (2004-2010) was done in respect to mode of presentation, diagnosis, etiology and treatment.
Results
There were 15 cases of AI. Mean age was 45.5 years. Abdominal pain, nausea and vomiting were the commonest symptoms. There were 8 enteric, 6 ileocolic, and 1 colonic intussusceptions. 73% of AIs were associated with a definable lesion. Only 1 case of enteric lesions had malignancy. All ileocolic lesions were malignant. Twelve of 15 patients underwent surgical intervention.
Conclusion
AI is a rare entity and requires a high index of suspicion. Small-bowel intussusception should be reduced before resection whenever possible if the underlying etiology is suspected to be benign or if the resection required without reduction is deemed to be massive. Large bowel should generally be resected without reduction because pathology is mostly malignant.
Keywords: intussusception, benign, malignant, surgery
Introduction
Intussusception was first reported in 1674 by Barbette of Amsterdam [1]. In 1789, John Hunter gave a detailed report about intussusception, or introsusception as it was called then [2]. Sir Jonathan Hutchinson was the first to successfully operate a child with intussusception in 1871 [3]. Intussusception is defined as the telescoping of a segment of the gastrointestinal tract into an adjacent one. It is the leading cause of intestinal obstruction in children and ranks second only to appendicitis as the most common cause of acute abdominal emergency in children [4]. The exact mechanism that precipitates intussusceptions is still unknown, but it is generally believed that any lesion in the bowel wall or irritant within the bowel lumen may alter the normal peristaltic pattern and is capable of starting an invagination leading to intussusceptions [5]. The optimal surgical approach in AI has been controversial in the past. More recently, manual reduction of the intussusception followed by definitive surgical resection has been advocated. Way back in the 1950’s Sanders and colleagues [6] and Brayton and Norris [7] recommended primary resection without attempting reduction in all adult patients with intussusception, regardless of anatomic site, because of significant risk of associated malignancy, which approaches 65%. Thus, a controversy continues to focus on whether AI should be surgically resected without an attempt at reduction for fear that undue operative manipulation of a malignant lesion may result in tumor dissemination [8,9].
Patients and Methods
The records of all patients aged 18 years or older admitted to a tertiary referral hospital of South India from 2004 to 2010 were studied retrospectively. A total of 15 patients were identified and were classified into four categories on the basis of the location of the lead point of the intussusception: 1) enteric, in which the intussusception is confined to the small bowel; 2) ileocolic, ileum invaginates through ileocecal valve; 3) colocolic, in which the intussusception is confined to the colon; 4) colorectal, colon invaginates through rectal ampulla. There were 5 cases of jejunogastric intussusception which were excluded from the study. For each group age, gender, clinical features and diagnostic procedures were studied. Operative and histopathology reports were reviewed to determine the location and etiology of the disease and method of surgical management and outcome.
Results
Age and gender data: There was equal gender distribution in our study: 8 females (53.3%) and 7 males (46.7%). The youngest patient in this series was aged 18 years and the oldest was aged 65 years with a mean of 44.5 years.
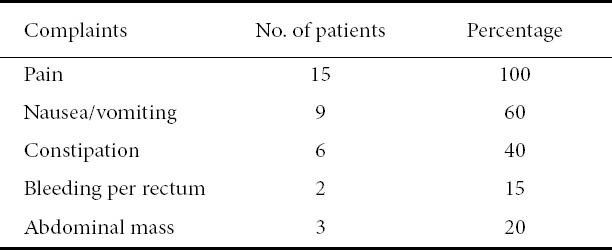
Clinical manifestations: Pain was the most common presenting complaint and was present in all 15 patients (100%). Nausea and vomiting was the second most common feature and was present in 9 patients (60%) followed by constipation. Bleeding per rectum was present in only 2 patients. A palpable mass was found in 3 patients (20%). Six patients (40%) presented with features of acute intestinal obstruction and the rest presented with chronic features (Table 1).
Table 1.
Symptomatology and number of patients
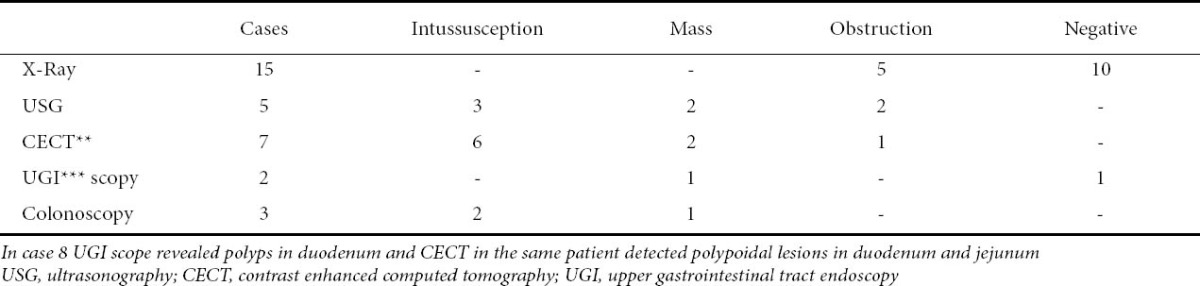
Diagnostic procedures: X-ray, abdominal ultrasound (USG) and contrast-enhanced computed tomography (CECT) of the abdomen were the most commonly used investigative modalities to reach the diagnosis, more so in acute cases. Upper gastrointestinal (UGI) endoscopy and colonoscopy were done in patients with chronic symptoms. X-ray was done in all patients that showed features of intestinal obstruction in the form of multiple air fluid levels in 6 patients (40%). USG was done in 5 patients (33%) and CECT abdomen in 7 patients (46%). Both were sensitive and reliable investigations in diagnosing presence and location of intussusception. UGI endoscopy was done in 2 patients and colonoscopy in 3 patients (Table 2).
Table 2.
Findings of the diagnostic procedures used
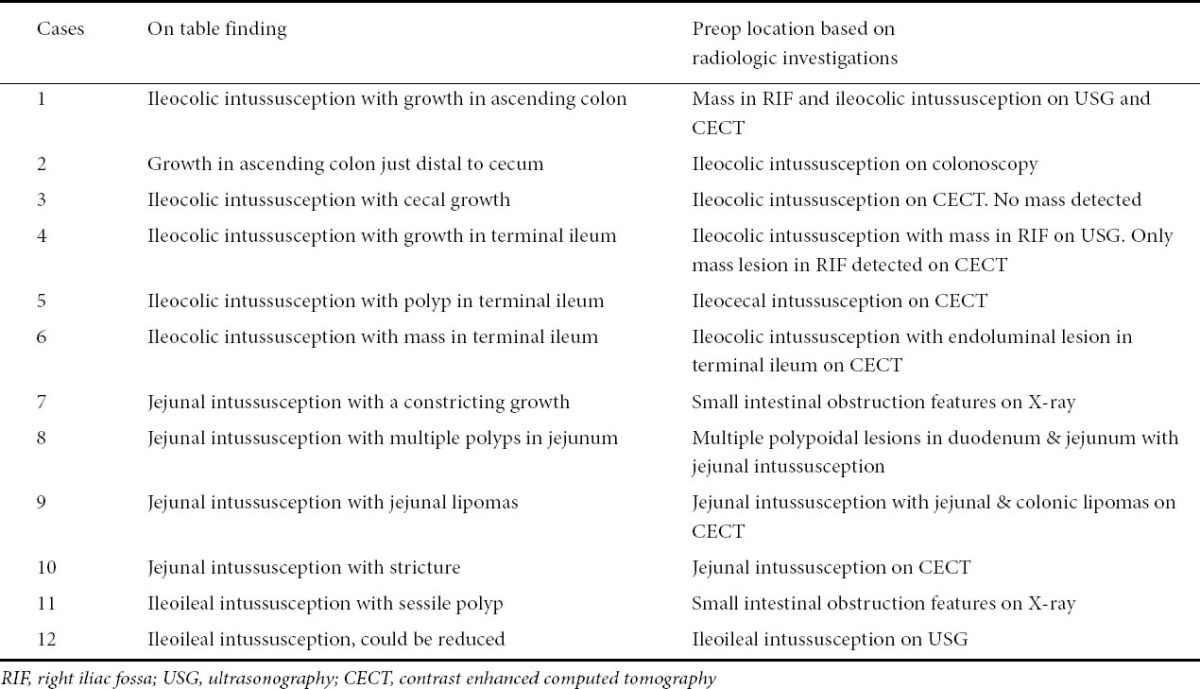
Location: Most of the intussusceptions were in the small bowel 8/15 (53.3%), 6 (40%) had ileocolic and 1 colonic intussusception. Table 3 shows intraoperative findings in the operated cases and correlation with preoperative radiological and endoscopic findings. CT and USG abdomen were reliable investigations in our study in defining the site of intussusception (Table 3).
Table 3.
Intraoperative findings and preoperative investigations
Treatment: Twelve patients in our study underwent laparotomy (6 for acute and 6 for chronic symptoms). In 1 patient with colonic intussusception, colonoscopic reduction was possible. One patient with small bowel intussusception was not willing to have any further intervention and 1 patient could not be operated in view of poor general physical condition.
Among 6 patients operated for small bowel intussusception, intraoperative reduction was possible in only 1 patient. All others underwent resection anastomosis. Five patients with ileocolic intussusception underwent right hemicolectomy and 1 with ileocecal intussusception underwent resection of terminal ileum and cecum followed by ileoascending anastomosis.
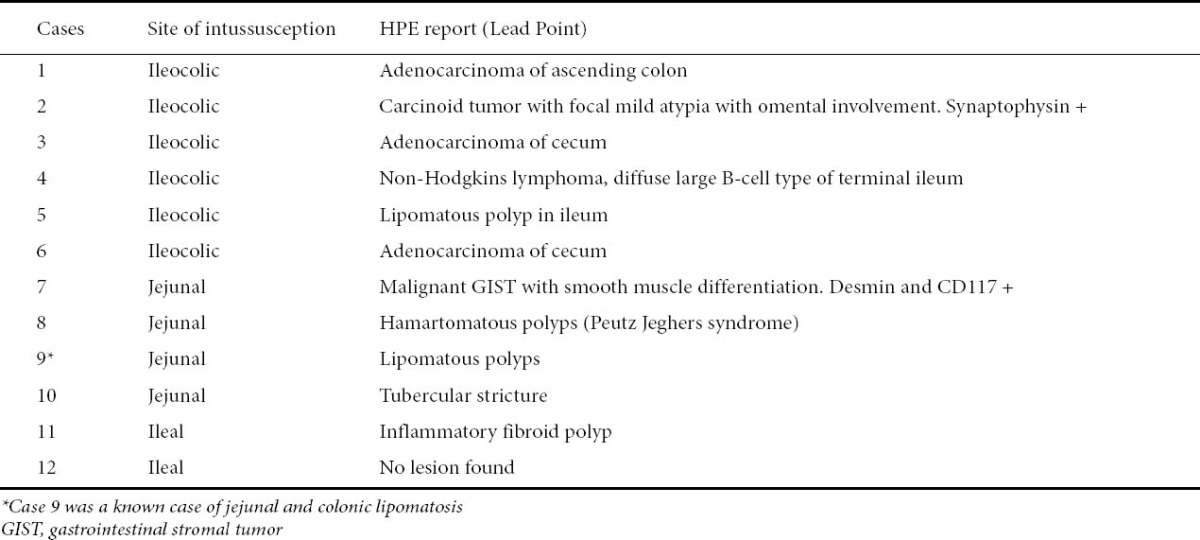
Histopathological examination (HPE): The majority of patients had malignancy as a lead point. Table 4 shows the histopathological diagnosis of the cause of intussusception in operated cases.
Table 4.
Histopathological diagnosis of the cause of intussusception in operated cases
Discussion
Intussusception is uncommon in adults when compared to pediatric population. It is estimated that only 5% of all intussusceptions occur in adults and approximately 5% of bowel obstructions in adults are the result of intussusceptions [10]. In more than 90% of cases, an identifiable lesion resulting in a lead point is demonstrable, with a neoplasm accounting for 65% cases [11,12]. Therefore, AI requires surgical management tailored to the most highly suspected pathology. The clinical presentation of AI varies considerably. The most common presenting symptoms are abdominal pain, nausea, and emesis in the acute presentation, seen in only 20% of AI [13]. Intermittent abdominal pain and vomiting are the major symptoms of subacute or chronic AI [12]. The classic pediatric presentation of intussusceptions (abdominal pain, mass, blood per rectum) is rarely found in adults [5,8-10], and there were no patients in our study with this triad. Other findings are constipation, diarrhea, bleeding, and abdominal distention [5,8,9]. Common physical findings include abdominal distention, decreased or absent bowel sounds, guaiac-positive stool, and abdominal mass. Because of the variability in clinical presentation and the impreciseness of diagnostic imaging, it is not uncommon for the diagnosis to be made only at the time of laparotomy [10].
Several imaging techniques may help to precisely identify the causative lesion preoperatively. Plain abdominal x-ray is typically the first diagnostic tool which reveals the presence of intestinal obstruction, particularly in acute cases. Contrast studies can help to identify the site and cause of AI, particularly in chronic cases. UGI series may show a ‘stacked coin’ or ‘coiled spring’ appearance [14]. Barium enema examination may be useful in patients with colonic or ileocolic intussusception in which a ‘cup-shaped’ filling defect is a characteristic finding [9]. In our series barium studies were not used. USG has been used to evaluate suspected intussusception. The classic features include the ‘target and doughnut sign’ on transverse view and the ‘pseudo-kidney sign’ in the longitudinal view [10,14].
In our study, USG was used on 5 occasions and it was diagnostic in 3 patients. The major disadvantage of USG is masking by gas-filled loops of bowel and operator dependency [10,15]. Abdominal CT scan has been reported to be the most useful imaging modality and has been shown to be a useful test in evaluating patients when a mass is present on physical examination [11]. It may define the location, the nature of the mass, its relationship to the surrounding tissues and it may stage the patient with suspected malignancy causing the intussusception. The characteristic features of CT scan include a target mass enveloped with eccentrically located areas of low density. Later a layering effect occurs as a result of longitudinal compression and venous congestion of the intussusceptions [9,10]. In our study, 7 patients had abdominal CT scans preoperatively and were diagnostic in 6 patients. Flexible sigmoidoscopy and colonoscopy are of paramount importance in evaluating intussusceptions presenting with subacute or chronic large bowel obstruction [10]. Colonoscopy was used in 3 of our patients as a diagnostic tool. It may not be advisable to perform endoscopic biopsy or polypectomy in those individuals with long-term symptoms because of the high risk of perforation, which is more likely to happen in the phase of chronic tissue ischemia and perhaps necrosis because of vascular compromise in intussusceptions [16].
There is no universal approach to the treatment of AI. Most authors agree that laparotomy is mandatory, based on the likelihood of an underlying pathologic lesion [14]. There has been controversy associated with the option of preliminary reduction of the intussusception before resection vs. primary resection without reduction. The theoretic objections to reduction of grossly viable bowel with mucosal necrosis are: 1) intraluminal seeding and venous embolization of malignant cells in the region of ulcerated mucosa [16]; and 2) possible perforation during manipulation and increased risk of anastomotic complications in the face of edematous and inflamed bowel [3,5,9]. Reduction should not be attempted if there are signs of bowel ischemia or inflammation [11]. Based on a high incidence of an underlying malignancy, which may be difficult to confirm intraoperatively, many authors recommend primary resection whenever possible [5,14]. For colonic intussusception, most recent reports recommend a selective approach to resection, keeping in mind that the site of intussusceptions tends to correlate with the lesion being benign or malignant [9,10].
Adults with intussusception have an organic lesion within the intussusception in 70-90% of cases. Malignancy seems to be the cause in 20-50% [14,16-18]. In our review, 50% of patients harbored malignant lesions. If the large bowel only is considered, then the likelihood of cancer is 50-65%. The vast majority of these lesions arise as a primary lesion, in which resection without reduction is recommended [5,8-10,14]. The exception to this rule may be patients with sigmoidorectal intussusceptions secondary to a carcinoma, in which reduction before the resection may save the patient an abdominoperineal resection and a permanent colostomy. However, even this option remains controversial. For small bowel intussusception, initial reduction of externally viable bowel before resection is recommended in recent reports [9,19]. The incidence of malignancy as the cause of small intestinal intussusception ranges from 1-40%, and the vast majority are metastatic [5,8-10,14]. Thus, the recommendation of initial reduction and then resection allowing bowel preservation is prudent. The algorithm for evaluating a patient with adult intussusception is presented in Fig.1.
Figure 1.
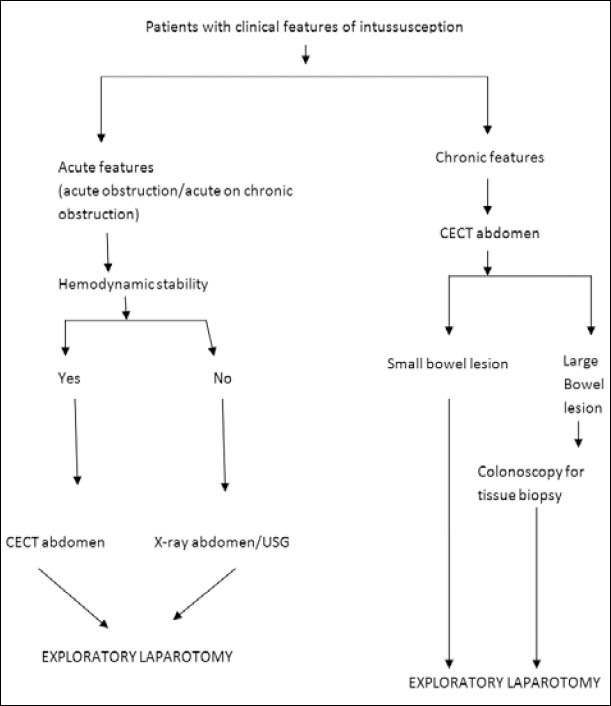
Algorithm for evaluating a patient with adult intussusception
USG, ultrasonography; CECT, contrast enhanced computed tomography
Conclusions
AI is an infrequent problem. The diagnosis of this condition can be difficult as symptoms are often non-specific and episodic. It is important to have a high index of suspicion as there is no ‘gold standard’ diagnostic test. Treatment usually requires resection of the involved bowel segment. Reduction can be attempted in small bowel intussusception if the segment involved is viable or malignancy is not suspected; however, a more careful approach is recommended in colonic intussusception because of a significantly higher chance of malignancy. In contrast to its pediatric counterpart, the treatment almost always is surgical.
Summary Box
What is already known:
Adult intussusception (AI) is a rare entity and differs from childhood intussusceptions in its presentation, etiology, and treatment
It requires a high index of suspicion
What the new findings are:
Small-bowel intussusceptions should be reduced before resection whenever possible if the underlying etiology is suspected to be benign or if the resection required without reduction is deemed to be massive
Large bowel should generally be resected without reduction because pathology is mostly malignant
Biography
Kasturba Medical College, Manipal University, Manipal, India
Footnotes
Conflict of Interest: None
References
- 1.Cochran AA, Higgins GL, 3rd, Strout TD. Intussusception in traditional pediatric, nontraditional pediatric and adult patients. Am J Emerg Med. 2011;29:523–527. doi: 10.1016/j.ajem.2009.11.023. [DOI] [PubMed] [Google Scholar]
- 2.Bhandarwar AH, Tayade MB, Kori CG, Borisa AD, Sameer V. Ceco-colic intussusception in an adult: a rare case report. Updates Surg. 2011 Aug 18; doi: 10.1007/s13304-011-0104-5. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 3.Garg PK. Idiopathic adult intussusception. Saudi J Gastroenterol. 2010;16:305–306. doi: 10.4103/1319-3767.70625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ibrahim D, Patel NP, Gupta M, Fox JC, Lotfipour S. Ileocecal intussusception in the adult population: case series of two patients. West J Emerg Med. 2010;11:197–200. [PMC free article] [PubMed] [Google Scholar]
- 5.Ghaderi H, Jafarian A, Aminian A, Mirjafari Daryasari SA. Clinical presentations, diagnosis and treatment of adult intussusception, a 20 years survey. Int J Surg. 2010;8:318–320. doi: 10.1016/j.ijsu.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 6.Sanders GB, Hagan WH, Kinnaird DW. Adult intussusceptions and carcinoma of the colon. Ann Surg. 1958;147:796–804. [PMC free article] [PubMed] [Google Scholar]
- 7.Brayton D, Norris WJ. Intussusception in adults. Am J Surg. 1954;88:32–43. doi: 10.1016/0002-9610(54)90328-1. [DOI] [PubMed] [Google Scholar]
- 8.Guillén Paredes MP, Campillo Soto A, Martín Lorenzo JG, et al. Adult intussusception - 14 case reports and their outcomes. Rev Esp Enferm Dig. 2010;102:32–40. doi: 10.4321/s1130-01082010000100005. [DOI] [PubMed] [Google Scholar]
- 9.De Zoysa MI, Halahakoon C. Pre-operative hydrostatic reduction of intussusception in an adult. Ceylon Med J. 2009;54:130–131. doi: 10.4038/cmj.v54i4.1455. [DOI] [PubMed] [Google Scholar]
- 10.Demirkan A, Yağmurlu A, Kepenekci I, Sulaimanov M, Gecim E, Dindar H. Intussusception in adult and pediatric patients: two different entities. Surg Today. 2009;39:861–865. doi: 10.1007/s00595-009-3979-8. [DOI] [PubMed] [Google Scholar]
- 11.Wang N, Cui XY, Liu Y, et al. Adult intussusception: a retrospective review of 41 cases. World J Gastroenterol. 2009;15:3303–3308. doi: 10.3748/wjg.15.3303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pisano G, Manca A, Farris S, Tatti A, Atzeni J, Calò PG. Adult idiopathic intussusception: a case report and review of the literature. Chir Ital. 2009;61:223–229. [PubMed] [Google Scholar]
- 13.Yalamarthi S, Smith RC. Adult intussusception: case reports and review of literature. Postgrad Med J. 2005;81:174–177. doi: 10.1136/pgmj.2004.022749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gorospe EC. Adult intussusception presenting with target sign. Scient World J. 2008;8:1154–1155. doi: 10.1100/tsw.2008.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bousseaden A, Afifi R, Essamri W, et al. Adult colocolic intussusception diagnosed by ultrasonography: a case report. J Med Case Reports. 2011;5:294. doi: 10.1186/1752-1947-5-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Godara R, Garg P, Dalal S, Nityasha Singla SL. Adult intussusception -a case series from rural India. Trop Doct. 2007;37:258–260. doi: 10.1258/004947507782333134. [DOI] [PubMed] [Google Scholar]
- 17.Chiang JM, Lin YS. Tumor spectrum of adult intussusception. J Surg Oncol. 2008;98:444–447. doi: 10.1002/jso.21117. [DOI] [PubMed] [Google Scholar]
- 18.Chang CC, Chen YY, Chen YF, Lin CN, Yen HH, Lou HY. Adult intussusception in Asians: clinical presentations, diagnosis, and treatment. J Gastroenterol Hepatol. 2007;22:1767–1771. doi: 10.1111/j.1440-1746.2007.04907.x. [DOI] [PubMed] [Google Scholar]
- 19.Kim JH, Lee KM, Yun SH, et al. Ileocecal intussusception in an adult: a case report. Turk J Gastroenterol. 2007;18:50–52. [PubMed] [Google Scholar]


