Abstract
Morbidity and mortality are reliably lower for the married compared with the unmarried across a variety of illnesses. What is less well understood is how a couple uses their relationship for recommended lifestyle changes associated with decreased risk for illness. Partners for Life compared a patient and partner approach to behavior change with a patient only approach on such factors as exercise, nutrition and medication adherence. Ninety-three patients and their spouses/partners consented to participate (26% of those eligible) and were randomized into either the individual or couples conditon. However, only 80 couples, distributed across conditions, contributed data to the analyses, due to missing data and missing data points. For exercise, there was a significant effect of couples treatment on the increase in activity and a significant effect of couples treatment on the acceleration of treatment over time. Additionally, there was an interaction between marital satisfaction and treatment condition such that patients who reported higher levels of marital distress in the individuals condition did not maintain their physical activity gains by the end of treatment, while both distressed and non-distressed patients in the couples treatment exhibited accelerating gains throughout treatment. In terms of medication adherence, patients in the couples treatment exhibited virtually no change in medication adherence over time, while patients in the individuals treatment showed a 9% relative decrease across time. There were no condition or time effects for nutritional outcomes. Finally, there was an interaction between baseline marital satisfaction and treatment condition such that patients in the individuals condition who reported lower levels of initial marital satisfaction showed deterioration in marital satisfaction, while non- satisfied patients in the couples treatment showed improvement over time.
Keywords: couples, health, cardiac, risk reduction, behavior change
Behavioral change to reduce the risk of cardiac disease is meaningful both in the short and long term. Across medicine and psychology, there is general agreement that for heart patients, adherence to medical recommendations and lifestyle modifications such as eating a heart healthy diet, engaging in regular physical activity, and taking medications according to prescription will improve a patient's chances of recovering from a cardiac event, returning to a previous activity level, and reducing the risk of future cardiac events (Goldsmith, Lindholm, & Bute, 2006).
However, despite robust findings across time and across behaviors, the U.S. Department of Health and Human Services (Services, 2008) reports that most often health behavior change occurs for only the most motivated individuals and is typically limited to a single health behavior rather than multiple behaviors. This report goes on to note that only 3% of the U.S. adult population has adopted all of the multiple behavioral components that characterize a heart-healthy lifestyle. Behavioral change over the long-term is difficult (Services, 2008), and non-adherence rates for lifestyle change recommendations for primary, secondary, or tertiary prevention often exceed 50% (Fappa et al., 2008; Fletcher et al., 2005; Haynes, 1979; Sackett & Snow, 1979).
Finding ways to sustain long term change is therefore essential for effective risk factor intervention. One factor that has become increasingly important in the literature for understanding change is a patient's intimate relationship. The current study is a response to recent calls for improving support from the patient's normal and ongoing social environment for sustaining desired change (Franks et al., 2006).
Specifically, the study assessed patients with coronary artery disease (CAD) as half of them engaged in a multi-faceted behavioral and couples intervention to reduce cardiac risk, specifically in the areas of exercise, nutrition, and medication adherence. The other half of the patients were assigned to a patients only condition. The goal of the intervention was to determine whether the partner's involvement in the intervention and a focus on the relationship between patient and partner could improve long-term maintenance of health behavior change.
Couples and health
The health enhancing aspects of intimate relationships continue to be a robust finding within the behavioral medicine literature. Morbidity and mortality are reliably lower for the married compared with the unmarried across a variety of acute and chronic conditions including cancer, heart disease, and surgery (Kiecolt-Glaser & Newton, 2001). However, not all relationships protect equally. There is further evidence that a positive marital relationship may be conducive to psychological and physical health promotion, whereas conflict-ridden marital relations may be detrimental (Kiecolt-Glaser & Newton, 2001). There are a number of mechanisms through which it is thought that the partner can influence behavior change in a patient including social support (Franks et al., 2006; Franks, Wendorf, Gonzalez, & Ketterer, 2004), shared decision making (Schumm, Skea, McKee, & N'Dow, 2010) or lifestyle management (Donald Baucom, Porter, Kirby, & Hudepohl, 2012). In addition to partner variables, relationship factors such as emotional support, intimacy, conflict, criticism, and solicitous behaviors have also been linked with change in a variety of patient physical and mental health outcomes (Joekes, Maes, & Warrens, 2007; Martire, Lustig, Schulz, Miller, & Helgeson, 2004; Vilchinsky et al., 2011). Finally, relationship communication has specifically been identified as having an important impact on health outcomes, specifically, how couples discuss major life events, their perception of the future, and their medical outcomes, (Eriksson, Asplund, & Svedlund, 2010).
The areas of change in the current study are consistent with previous work on couples and health outcomes. Intimate partners have been included in studies looking at change in exercise (Hong et al., 2005; Oldridge & Jones, 1986), weight loss (Black, Gleser, & Kooyers, 1990; Markey, Markey, & Birch, 2001), and medication adherence (Remien et al., 2005). These studies support the health enhancing properties of close personal relationships. However, in previous studies, the partner's involvement has been poorly defined (e.g., attendance) and has rarely served as a focus of the intervention. In these studies, although the importance of the partner/spouse has been recognized in relation to behaviors such as exercise (Hong et al., 2005) and risk factors such as cardiovascular reactivity (Broadwell & Light, 2005), the partner is only included in assessing what behavioral or relationship factors might influence the change process for the patient, as opposed to the partner and the relationship becoming integral foci of the therapy.
Theoretical Bases for the Intervention
The intervention, Partners for Life, was informed by three broad-based and multi-faceted theories integrated in order to meet the goal of making and maintaining the behavior changes necessary to reduce the risk of a further cardiac event in cardiac patients. First, Cognitive-Behavioral Couples Therapy (CBCT; D. Baucom, Shoham, Mueser, Daiuto, & Stickle, 1998) provided the theoretical background of the couples intervention. It is uniquely appropriate for this population and the goals of the study. It is a communications skills approach predicated upon the idea that partners who experience greater arousal during conflicted interactions are at significantly greater risk of declines in marital satisfaction and health outcomes at a later date (Levenson & Gottman, 1985). Relationship satisfaction was considered likely to play a moderating role in the couples' ability to make and maintain health behavior changes based on the findings that relationships can be supportive of change or unsupportive of change (Kiecolt-Glaser & Newton, 2001); and the direction and course of therapy would be expected to change accordingly.
Second, in keeping with self-determination theory (Deci, 1985) and the focus on “autonomy-supportive” interactions (conveying support and information without being controlling), couples were helped to engage in autonomy-supportive interactions and shared decision making around health and relationship issues. Self determination theory has been used in several studies to explain behavior change concepts. Gay et al. (2011), in a study of 477 adults, found a relationship between exercise and autonomy. For this study, it was of interest to see if self determination theory was built into an intervention, would there be an effect on behavior change.
Third, one of the tenets of the transtheoretical model (Prochaska & DiClemente, 1982) is that when a person sees more advantages than disadvantages to being ready to change, they will be more ready and likely to make desired life changes. This often takes the form of form of helping couples determine the pros and cons of any particular behavior change, or helping them determine the decisional balance (DB) of such a change (Janis & Mann, 1977). Much of the educational material provided to the couples revolved around helping patients identify both barriers and pathways to change in an effort to influence patient decision making regarding the adoption of healthy behaviors (for more information on the theoretical background of the project, see Sher et al., 2002).
The current study was designed to investigate the benefits of a comprehensive couples intervention on three health behaviors: nutrition, exercise, and medication management. In a randomized, controlled design, a couples condition (for cardiac patients and their intimate partners) was compared to an individuals (patient only) condition. The following hypotheses were tested:
Hy1. While both conditions would show behavior changes across time, cardiac patients in the couples condition would evidence more change early, and maintain those changes longer.
Hy2. Couples who are more satisfied with their relationships would have a different response to treatment than couples who are dissatisfied in their relationships.
Method
Participants
First, to differentiate among the terms partners, patients and participants, the following terms will be used. The term “participants” will be used generically to indicate those participating in the study. “Patients” will be the person within each couple with the cardiac disease. “Partners” will be used to indicate the spouse or intimate partner of the patient within the couple. Nearly all of the participating cardiac patients and their partners were recruited from two large preventive cardiology clinics and cardiac rehabilitation programs, one in a large Midwestern city and the other in the near suburbs of that city. Other participants responded to television and radio promotions.
Patients were eligible for inclusion in the study if they were diagnosed with CAD or had a significant cardiac event or intervention (e.g. MI, CABG, angioplasty); were married or living for at least 6 months with an intimate partner and their partner agreed to participate; were being treated with lipid lowering medication; were able to participate in regular exercise; and needed to lose weight or implement a low fat diet. Exclusionary criteria included uncontrolled medical conditions such as hypertension, congestive heart failure, diabetes or thyroid disease; inability to read or speak English at a 6th grade level; extensive travel or residence elsewhere during the year of their participation in the study; psychiatric hospitalization within the previous 12 months; and current treatment for drug or alcohol abuse.
Participants were not paid. However, they received treatment at no charge regardless of group assignment. They also received gift certificates to local, healthy grocery stores for the completion of measures. Across the intervention, there were also other, small incentives such as tee-shirts and water bottles with the Partners for Life logo for work-outs.
The 2565 patients screened from both medical clinics for potential participation ranged in age from 18 to 84, with a mean age of 63 (SD=13.6). Fifty-four percent were male. Marital status was as follows: 34% married; 26% single; 29% marital status unknown; 1% living with an intimate partner. Of those screened, 35% were Caucasian, 33% were African American; 8% were Hispanic, 5% were Asian and 19% were of unknown race.
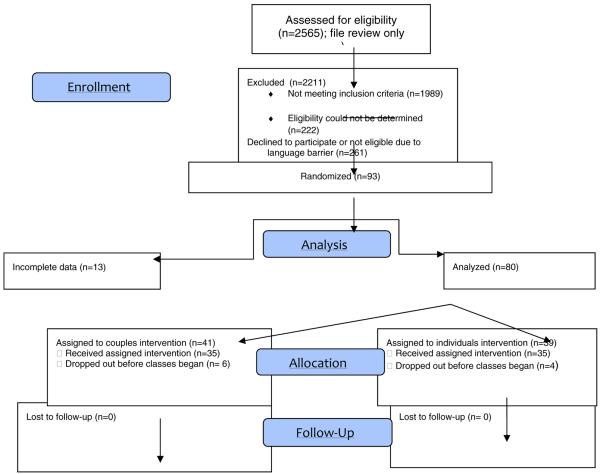
Of the individuals screened, 78% did not meet eligibility criteria to participate, 14% were eligible and for 8%, eligibility was unknown (see Table 1 for CONSORT flow chart). The primary reason for ineligibility was not being married or having a partner, as far as we could tell by medical chart demographic data. The second biggest reason for exclusion was not meeting all of the medical conditions for participating. In terms of condition assignment, stratified randomization was conducted to assure that all groups were matched on ethnicity/race, age, and gender of patient. Although 93 patients were randomized to conditions, only 80 patients contributed data to the analyses. For the 13 participants that were randomized but not included, not enough baseline information was complete, and the participants failed to respond to our attempts to obtain this information, making none of their data usable. There were no demographic differences between the 13 who failed to provide enough baseline data and those whose data were obtained. Table 2 includes the demographics for the 80 patients who were randomized. Of note, 87% of the patients were male, and 33.8% were minorities. The overrepresentation of male patients in the sample appeared to be due to the confluence of two factors: the fact that women exhibit heart disease at a later age than men when they are more likely to be widowed, and second, women in this age range tend to have more concomitant health problems that interfere with their ability to exercise such as orthopedic issues, lung disease, and arthritis. In contrast, the high minority representation of the sample reflects both the demographics of the city as a whole as well as concerted efforts made to recruit minorities.
Table 1.
Consort 2010 Flow Diagram
|
Table 2.
Demographics for Randomized Patients/Partners (N=80)
| Average Age (SD) (N=80) | 60.16 (10.2) | Patient |
| 56.87 (11.7) | Partner | |
|
| ||
| Gender Patient (N=80) | 87.5% (70) | Male |
| 12.5% (10) | Female | |
| Gender Partner (N=80) | 18.3% (17) | Male |
| 81.7% (76) | Female | |
|
| ||
| Race - Patient (N=80) | 65.0% (52) | Caucasian |
| 18.8% (15) | African American | |
| 8.8% (7) | Hispanic | |
| Race – Partner (N=80) | 6.2% (5) | Asian |
| 1.2% (1) | Unknown | |
| 61.2% (49) | Caucasian | |
| 21.2% (17) | African American | |
| 6.2% (5) | Hispanic | |
| 7.5% (6) | Asian | |
| 3.8% (3) | Unknown | |
|
| ||
| Marital Status (N=80) | 92.5% (74) | Married |
| 7.4% (6) | Living Together | |
|
| ||
| Employment Status – Patient (N=80) | 43.8% (35) | Employed Full Time |
| 40.0% (32) | Retired | |
| 1.2% (1) | Unknown | |
| 6.2% (5) | Employed Part Time | |
| 5.0% (4) | Unemployed | |
| Employment Status – Partner (N=80) | 3.8% (3) | Homemaker |
| 33.8% (27) | Employed Full Time | |
| 22.5% (18) | Retired | |
| 16.2% (13) | Unknown | |
| 11.2% (9) | Employed Part Time | |
| 2.5% (2) | Unemployed | |
| 13.8% (11) | Homemaker | |
All statistical models used an “intent to treat” format based upon 80 patients and partners, whether or not they completed the intervention. That is, 80 couples contributed something to each of the models. It should be noted that of these 80, 61 completed the intervention and all follow-up measures. All patients and partners who completed the intervention completed all follow-up measures. Table 3 provides the specifics about drop out in terms of when the drop outs occurred. It should be noted that by far (72%), the majority of the drop outs occurred before classes began. There were no differences in attrition by race, education, age or condition. In fact, much of the attrition occurred before randomization.
Table 3.
number of classes attended
| Frequency | Percent | Valid Percent | Cumulative Percent | |
|---|---|---|---|---|
|
| ||||
| 0 | 25 | 78.1 | 78.1 | 78.1 |
| 1 | 3 | 9.4 | 9.4 | 87.5 |
| 2 | 2 | 6.3 | 6.3 | 93.8 |
| Valid | ||||
| 4 | 1 | 3.1 | 3.1 | 96.9 |
| 5 | 1 | 3.1 | 3.1 | 100.0 |
| Total | 32 | 100.0 | 100.0 | |
Procedure
Both Conditions
Groups included all participants assigned to that condition. Therefore those assigned to the Couple condition were only in a group with others so assigned and the same occurred for the individual groups. All groups (both conditions) met for 18 sessions (12 weekly sessions followed by 6 alternate week sessions over a total of 24 weeks). The groups followed a standard, manualized program. Information regarding nutrition, exercise, and medication adherence as they relate to heart disease was discussed. The groups consisted of a brief didactic presentation and questions and answers about the presentation, followed by either break-out dyadic sessions for the couples condition or a group discussion for the individuals condition. Health behavior topics for both conditions included subjects such as nutrition guidance, exercise “do's and don'ts” and the value of taking medications as prescribed. The final six sessions for both conditions focused on maintenance and relapse prevention.
Couples Condition
The couples intervention groups consisted of up to five patients, their partners, and a therapist. For the couples, the educational component was interspersed with communication skills training, motivation discussions and relationship issues. Break-out groups for the couples consisted of couple-level discussions of the day's topic as well as practice time for the communication skills being taught. Therapists in the couples condition served as a resource for the couples' discussion, observing and making suggestions for the content of the discussion as well as the process. The relationship content in the couples intervention instructed and encouraged patients and their partners to collaborate on making changes in the way they interacted in order to meet make and keep behavior changes as well as the way they interact with each other. For example, they were encouraged to figure out the best way for the partner to help the patient exercise using the communication strategies designed to increase positive interaction behaviors and decrease negative interaction behaviors. The communication skills training using general illness and rehabilitation topics, and involved two components: problem solving and emotional expressiveness training, in keeping with standard CBCT strategies (Epstein & Baucom, 2002).
Individuals Condition
The individuals condition consisted of up to 10 patients and a therapist. No group contained less than 5 individuals. Group discussion focused on the didactic topic of the day as well as personal reflections related to the patients' health, with the therapist again serving as a resource person
Thus, the couples-related components of the intervention (such as communication strategies, social support strategies and general couples issues) were only presented to the couples conditions; the nutrition, exercise, and medication adherence components were the same in both conditions, as was the amount of sessions.
It should be noted that the intervention made no attempt to control for differing levels of “usual care” among the patients. Thus, while some patients could have received cardiac rehabilitation as part of their post-hospital care, others would not have been referred to cardiac rehabilitation, others might have been referred but did not engage in it, and some would not have been referred for such programs, as they are not offered routinely at hospitals within the Chicago area. Thus, no assumptions were made about previous knowledge in the areas covered by the groups; all patients received the same and basic information about exercise, nutrition, and medications.
All patients in the study received prescriptions for cholesterol-lowering medication(s), usually statins, from their cardiologist. Medication throughout the study was obtained from the patient's usual sources and paid for by the patient's insurance coverage. Patients were maintained in the study if their medication dosage was changed, if they were changed to another statin, if an additional cholesterol-lowering medication was prescribed, or if they were switched from a statin to another type of cholesterol-lowering medication. Patients were also maintained in the study if medications became no longer necessary due to behavioral changes or other reasons.
The patients completed assessments at baseline (before groups began), and following the intervention (6 months from beginning of intervention). Follow-up assessments were completed at 12, and 18 months after group sessions began. In addition to these four data collection points, patients also met with the nurse coordinator of the project at the nine-month mark in order for her to download computerized medication information, answer any questions that may have arisen since the intervention ended, and to keep them actively engaged in the project, thus maximizing the chances of complete follow-up data. During all appointments with the nurse coordinator, the following were assessed: blood pressure, heart rate, weight, waist circumference, current medications, lab work including lipid profile, assessment of cardiac health status, lipid medication adherence via a computerized pill bottle cap and exercise adherence. No adverse events were reported for either patients or partners other than those addressed by the study such as a necessary change in medication type.
Therapists
Both the individuals and couples conditions were delivered by three doctoral level clinical psychologists with experience in leading therapy groups. These therapists received approximately 16 hours of training in the interventions prior to meeting with their groups and were provided with weekly, on-going supervision. With the relatively small number of groups in each study condition, it was decided that the best way to control for potentially confounding therapist factors was to have each of the three therapists deliver both the couples and the individual conditions. Potential bias in the delivery of the different interventions was a concern, however. The investigators emphasized that it was important both to the study and to the welfare of the patients that the therapists provide optimal treatment to patients in both conditions; therapists were not aware of the hypotheses of the study. In addition, therapists used manualized treatments, taped their sessions for monitoring by the investigators, and received weekly supervision from selected experts in health behavior change and from the team of investigators. In addition, as noted below, ratings of adherence and quality of treatment were provided by an expert external evaluator who had no other involvement with the investigation beyond being trained in the adherence and quality coding system.
Measures
Demographics
A demographic questionnaire for both patients and partners included questions regarding age, marital status, race/ethnicity, employment status, household income, medical history and psychiatric history.
Weight Loss Measures
Patient weight change in pounds and changes in body mass index (BMI) served as the primary weight dependent measures. BMI also approximated percent body fat, and allowed the investigators to control for percent overweight at baseline (Kraemer, Berkowitz, & Hammer, 1990). BMI and waist circumference were measured by the nurse coordinator of the project, using the same medical scale at each appointment.
Nutrition recalls
Twenty-four hour diet recalls (24HR) for the patients were conducted by a nutritionist (AD) using the Nutrition Data Systems for Research (NDSR) software version 4.03–4.05. Nutrition Data System for Research (NDSR) is a windows based dietary analysis program designed for the collection and analyses of 24-hour dietary recalls and the analysis of food records, menus, and recipes. Calculation of nutrients occur immediately providing data per ingredient, food, meal, and day in report and analysis file formats.
YALE Physical Activity Survey (YPAS; (DiPietro, Caspersen, Ostfeld, & Nadel, 1993; Harada, Chiu, King, & Stewart, 2001)). As a self-report measure of physical activity, the YPAS was administered to the patients at each check-in visit. The YPAS has been shown to have correlation coefficients ranging from 0.42 to 0.65 with several physiological variables.
Medication adherence measures
Patient medication adherence was assessed at all regular nurse appointments using the computerized Medication Event Monitoring System (MEMS) from APREX. The MEMS has been used in over 50 studies, including studies of hypertension and cardiovascular disease treatments, as well as studies in which statins were used (Kruse, 1993). The system consists of a computerized pill bottle cap (TrackCap™) that monitors how often and when the bottle is opened and closed, the MEMS Communicator, which reads data from the caps, and MEMS View Software, which permits the data to be downloaded into a computer and converted to a form compatible with SPSS for Windows software, which was used for data analysis.
Dyadic Adjustment Scale (DAS)
The DAS (Spanier, 1976) is perhaps the most widely used measure of relationship satisfaction among married and cohabitating couples (D. H. Baucom & Epstein, 1990). It has demonstrated content, criterion-related, and construct validity (Spanier, 1976). At baseline, for patients in the couples group, mean DAS was 112.7 (S.D. 16.5) and ranged from 80 to 144; 19% of patients in the couples group began treatment in the distressed range (<97). For the patients in the individuals group, mean DAS was 112 (S.D. 17.1) with a range from 75 to 143; 15.8% were in the distressed range.
Treatment fidelity adherence and quality coding system
To evaluate whether the therapists presented session content as intended and performed well during sessions, an experienced clinical psychologist who was otherwise uninvolved with the investigation received 25 hours of specific training on the fidelity adherence and quality coding system. She listened to entire therapy sessions and rated them on 12 items, including three adherence items (e.g., was unscheduled material included), nine specific quality ratings (e.g., was the therapist informative without being pressuring), and an overall rating of session quality, using a 1–7 rating scale for each item. Approximately 25% of the sessions (n=71) for each therapist in each treatment condition were selected randomly to be rated. Therapists were not given feedback regarding scores from the outside rater. The ratings indicated a high level of adherence and quality on each item. The average rating of overall session quality was 5.6 out of a possible 7. Average ratings on all other items ranged from 5.3 to 6.2. A 2 (treatment condition) × 3 (therapist) MANOVA across the 12 items revealed no significant differences in adherence and quality across the treatment conditions [F (12, 50)= 1.08, p > 0.05], therapists [F (36, 146)= 1.35, p > 0.05], or the interaction of the two [F(24, 98)= 1.1, p > 0.05].
Analyses and Results
Statistical Analyses
To examine the impact of couples based treatment on the repeated assessments (baseline, 6 months, 12 months, 18 months), hierarchical linear modeling (Raudenbush & Bryk, 2002; Raudenbush, Byrk, Cheong, & Congdon) was used. The application of HLM in couples data is well suited for the examination of individual change and has been described previously (Atkins et al., 2005; Christensen et al., 2004; Raudenbush, Brennan, & Barnett, 1995). Briefly, growth trajectories were created for each patient in a multistep process that aimed to model the outcome with the simplest possible model. Because of the nature of the expected change, the trajectories were modeled using an intercept (baseline value), slope, and quadratic term. The slope estimated the linear change over time and represented the increase or decrease in the variable. The quadratic term estimated the acceleration or deceleration over time and reflected short term gains in treatment that may be lost over follow-up. The primary analysis consisted of condition differences in the change parameters that were treated as outcomes in the second level of the model.
On completion of the primary analyses, treatment condition differences were analyzed in relation to baseline relationship status as a post hoc analysis. Main effects of these analyses can be found in Table 4. To quantify these differences, the impact of an individual's Dyadic Adjustment Scale (DAS) score was estimated on the intercept, slope, and quadratic parameters in a second level model. The interaction between treatment assignment and DAS score was also evaluated. Significant effects were interpreted as an indication that the factor impacted some element of the change process, and effect sizes are presented according to the methods described by Raudenbush and Liu (Raudenbush & Liu, 2001; see Table 4).
Table 4.
Means (standard deviations) by Group and HLM effects
| Outcome | Time Point | HLM Effect (p values) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6-months | 12-months | 18-months | G | T | T2 | G x T | G x T2 | |
| YPAS | .11 | .02 | .02 | .04 | .04 | ||||
| Individuals | 5070.5 (5738.3) | 5304.5 (3741.1) | 6511.4 (6270.8) | 7087.2 (8663.1) | |||||
| Couples | 3504.9 (2629.1) | 5365.4 (4141.8) | 6287.8 (6504.4) | 5403.3 (3867.1) | |||||
| DAS | .84 | .78 | † | .55 | † | ||||
| Individuals | 112.7 (16.8) | 113.2 (16.6) | 111.2 (17.3) | 112.3 (18.0) | |||||
| Couples | 113.4 (15.4) | 113.7 (14.8) | 114 (14.9) | 113.7 (14.8) | |||||
| Track Caps | .56 | <.01 | † | .80 | † | ||||
| Individuals | 47.7 (46.0) | 87.7 (22.3) | 81.8 (27.0) | 73.1 (36.6) | |||||
| Couples | 57.8 (45.1) | 82.8 (28.2) | 90.6 (21.1) | 84.6 (24.1) | |||||
| BMI | .87 | .82 | .46 | .15 | .19 | ||||
| Individuals | 31 (10.9) | 33.7 (5.9) | 33.4 (6.2) | 33.6 (6.0) | |||||
| Couples | 31.2 (9.0) | 31 (8.3) | 32.4 (5.9) | 41.2 (48.3) | |||||
| KRISTAL TOTAL | .36 | .19 | † | .93 | † | ||||
| Individuals | 2.2 (0.4) | 2.1 (0.4) | 2.2 (0.3) | 2.2 (0.5) | |||||
| Couples | 2.3 (0.5) | 2.4 (0.3) | 2.3 (0.4) | 2.2 (0.3) | |||||
| KRISTAL: SAT FAT | .59 | .25 | † | .82 | † | ||||
| Individuals | 2.2 (0.4) | 2.2 (0.4) | 2.1 (0.4) | 2.3 (0.4) | |||||
| Couples | 2.2 (0.4) | 2.3 (0.4) | 2.3 (0.3) | 2.2 (0.3) | |||||
Only a linear model was estimated for this outcome
G: Group
T: Time
T2: Time squared
An intent-to-treat philosophy was used for creation of the models in that all available data were included in the analyses and not just the complete (i.e. per protocol) cases. Missing values for questionnaire data were singly imputed by SPSS Missing Values Analysis package using regression estimation. The HLM analyses were conducted on the HLM 6.0 (Raudenbush et al., 2004). All other analyses were conducted using SPSS 15.0 (SPSS, Inc. Chicago, IL). Where appropriate all testing is two-tailed with statistical significance interpreted at p <0.05.
Results
Although 93 patients were enrolled, only 80 patients contributed at least one score that could be used in the models (all 80 of these participants contributed scores to the analysis). Of the 80 patients in the analysis, 58 contributed scores for all measures at all time points. For most of the measures, 60/80 (75%) patients contributed scores at baseline. There was 21% attrition from the time participants engaged in the study to through the base line follow-ups. Time was the overwhelming reason for drop-out (34%) followed by “partner changed mind” (19%) and change in medical status making it difficult to attend sessions (16%). Other reasons included a personal illness, moving and family illness. One participant indicated that drop-out occurred because he/she “didn't like the classes”. That participant was in the couple condition and attended 2 classes before dropping out.
At baseline, and due to randomization procedures, no outcome variable had different baseline values by treatment condition (p > 0.25). Hypothesis one predicted that the conditions would differ in terms of change across time on the variables of interest (exercise, nutrition and medication adherence). Each of these variables was evaluated separately. Next, the second hypothesis that there would be an interaction between condition and relationship satisfaction was tested, again for the trajectory of each dependent variable separately.
Hypothesis 1: difference in conditions across time
For physical activity, because of the skewed nature of the YPAS data, the log of the scores was used in analysis. Starting levels of physical activity were inversely correlated with slopes (r = −0.74), with lower initial levels of physical activity associated with greater increases in activity over time. The overall increase in YPAS scores over time was also statistically significant: B = .04 (95%CI: 0.001 to 0.079), p = 0.019, showing an effect for both the individuals and couples conditions. Treatment condition assignment also significantly impacted the degree of change in physical activity. There was a significant effect of couples treatment on the increase in activity [B = −0.06 (95%CI: −0.119 to − 0.001), p = 0.043, d = 0.82; large effect size], and a significant effect of couples treatment on the acceleration of treatment over time [B = 0.004 (95%CI: 0 to 0.008), p = 0.038, d = 0.69; a medium to large effect size]. Patients in the individuals treatment changed physical activity at a greater overall rate initially, but the rate decelerated over time (quadratic slope: B = −0.004). In contrast, patients in the couples treatment showed slow but steady improvement in physical activity across treatment and follow-up periods with no flattening out or deterioration (quadratic slope: B = 0.00008), surpassing the control patients at around week 14.
None of the weight loss variables (such as BMI) or nutritional variables changed meaningfully across time or between treatment conditions.
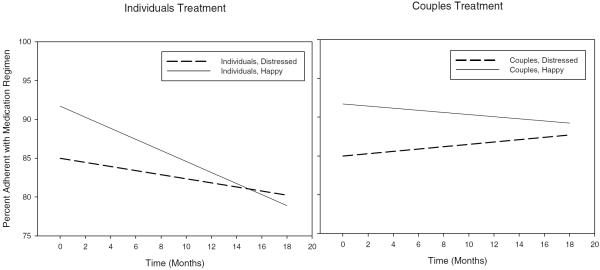
The average rate of change in medication adherence was small and statistically non-significant (B = −0.021 (95%CI: −0.393 to 0.351), p = 0.27), but indicated that participants were taking their medications slightly less often as treatment progressed. Treatment condition assignment non-significantly impacted the degree of change in medication adherence. However, patients in the couples treatment exhibited virtually no change in medication adherence over time, while patients in the individuals treatment exhibited roughly a one-half percent decrease in adherence during each month of the study, or a 9% relative decrease across time (B = 0.50 (95%CI: −0.127 to 1.127), p = 0.125, d = 0.78; large effect size), as illustrated in Figure 3.
Figure 3.
Percent of Medication taken according to prescription
Hypothesis 2: Change across time as moderated by baseline relationship satisfaction
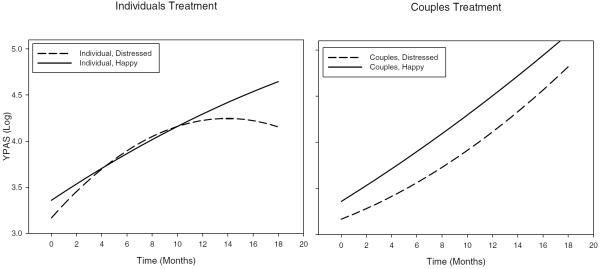
For physical activity, response to treatment was also examined in relation to baseline marital satisfaction. Figure 1 displays the trajectories of activity levels of patients as a function of treatment condition and baseline DAS score. Starting levels of physical activity were not significantly affected by relationship satisfaction (B = 0.006 (95%CI: −0.004 to 0.016), p = 0.23), but relationship satisfaction affected the degree of overall change and reactivity to treatment. Specifically, there was an interaction between marital satisfaction and treatment condition such that patients who reported higher levels of marital distress in the individuals condition did not maintain their physical activity gains by the end of treatment, while both distressed and non-distressed patients in the couples treatment exhibited accelerating gains throughout treatment (quadratic DAS × Condition: B = −0.0002 (95%CI: −0.0004 to 0), p = 0.050).
Figure 1.
YPAS across time, by condition.
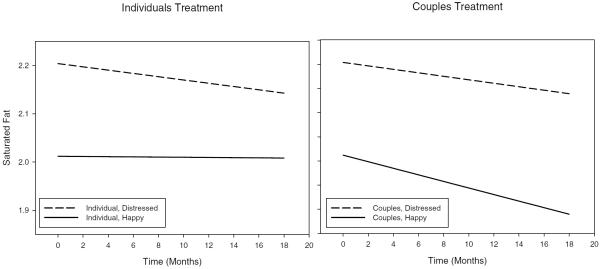
In terms of the nutritional variables, only baseline levels of saturated fat intake were modestly affected by relationship satisfaction (B = −0.006 [95%CI: −0.01 to −0.002], p = 0.049), with increases in initial DAS score associated with a decrease in saturated fat intake (see Figure 2).
Figure 2.
Saturated fat across time, by condition
Starting levels of medication adherence were not significantly affected by relationship satisfaction (B = 0.21 [95%CI: −0.104 to 0.524], p = 0.22), and relationship satisfaction did not significantly interact with treatment to affect the change or reactivity in medication adherence.
Other variables of interest: marital satisfaction
The overall change in marital satisfaction was small and statistically non-significant over the time of the study (B = 0.09 (95%CI: −0.086 to 0.266), p = 0.33), and there was no effect of treatment condition on satisfaction (B = 0.005 (95%CI: −0.348 to 0.358), p = 0.98, d = 0.02). An exploratory analysis was conducted based on the assumption that a couples intervention might affect marital satisfaction differentially over time for couples who started with high or low levels of satisfaction. DAS scores were dichotomized into `not satisfied' (DAS ≥97; mean 90.7) and `satisfied' (DAS >97; mean 117.8) conditions (Jacobson et al., 2000). There was an interaction between baseline marital satisfaction and treatment condition such that patients in the individuals condition who reported lower levels of initial marital satisfaction showed deterioration in marital satisfaction, while non- satisfied participants in the couples treatment showed improvement over time. Patients with higher marital satisfaction maintained their level of satisfaction in both treatments (DAS × Condition: B = 1.2 (95%CI: 0.298 to 2.102), p = 0.009), as illustrated in Figure 4.
Figure 4.
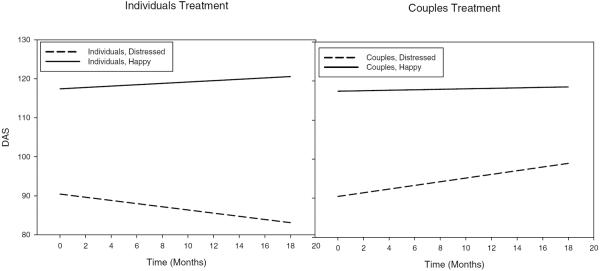
DAS across time, by condition
Discussion
A robust finding throughout the behavioral change literature is that change can be affected by others within the environment of the patient (Kiecolt-Glaser & Newton, 2001), although the exact mechanisms behind this effect have never been reliably determined (Martire et al., 2004). The purpose of this study was to understand if a couple based intervention would prove to be more effective for behavior change following the intervention and across time as opposed to a patient based intervention. The couple based intervention was designed around self-determination theory (Deci, 1985), in that those in the couples condition were helped to engage in autonomy-supportive interactions and shared decision making around health and relationship issues. Second, the couple intervention was based upon cognitive-behavioral couples therapy (Baucom et al., 1998) in that those in the couple condition were helped to improve their communication skills in an effort to have patients and partners work together towards behavior change. Including these additional components onto an educational based intervention designed for patients was hypothesized to be beneficial for behavior change as well as relationship satisfaction.
More specifically, it was expected that both treatment conditions would show a negative quadratic slope based only upon the inclusion of education about behavior change, it was hypothesized that those in the couple condition would experience less reversion to the baseline values. Self-reported exercise and activity levels (YPAS) were most consistent with this hypothesis. Patients in both conditions showed initial gains in exercise levels during the six-month intervention. However, patients in the couple condition showed greater initial improvement in activity than those in the individual condition and more successfully maintained these changes into the follow-up period. Patients in the individual condition changed initially at a greater overall rate but showed substantially decelerating change across time.
The major finding was that activity levels were affected by the interaction between treatment condition and baseline marital satisfaction. Patients with high marital satisfaction showed significant improvement in activity levels throughout the intervention and the follow-up periods, regardless of condition. However, patients beginning the intervention with less satisfaction in their relationships needed to be in the couple condition to show change; less satisfied patients in the individuals condition tended to reverse the exercise gains they initially made.
This finding, although just reaching significance, underscores the importance of a good relationship in making behavior change. Patients who saw their relationships as satisfying appeared to use the relationship to improve their behavior regardless of treatment condition. Those in the couple condition were reinforced for doing so, but those in the individuals condition may have done so naturally, perhaps by sharing their intervention experience with their spouses who were not present in the groups. In contrast, patients who started off dissatisfied in their relationships most likely were not able to use their relationships to support behavior change. Then, because relationships were not a focus of the Individual condition, the importance of support for behavior change was never conveyed to those in the Individual condition. Patients less satisfied with their marriages may also have found this to be a general stressor that made it hard to deal with health behavior change without the assistance of the couple intervention.
With regard to weight loss and nutritional changes, an unexpected finding was that no changes were found on the variables of most interest including BMI, calories and sodium consumed in the diet. It is possible that with the sometimes long lag time (up to 36 months) between the intervention and the cardiac event and/or a formal cardiac rehabilitation program, dietary changes were previously made and had reached a plateau by the time of the study's measurements. However, the average patient BMI at the beginning of the study (33.3) and at the end (33.4) were in a high risk range, and the lack of change in this variable in both conditions remains a concern.
It was also interesting that there was a difference in baseline saturated fat intake with respect to the level of relationship satisfaction. It has been reported previously and consistently that those who are married and satisfied in their marriages take better care of themselves than those who are either unmarried or dissatisfied (e.g. Burman & Margolin, 1992; Kiecolt-Glaser & Newton, 2001). Thus, it was not surprising that patients who started out less satisfied in their relationships had more saturated fat in their diet than those who started out more satisfied.
For medication adherence, although there was no statistically significant difference in adherence to medication between conditions or by relationship satisfaction, those in the individual treatment exhibited a nine percent relative decrease in compliance by the end of the study. Although statistically non-significant, the large effect size may indicate a benefit of having the patient's partner involved in the medication adherence process.
As for marital satisfaction, similar to our other findings, the change in marital satisfaction over time is also a function of the interaction between marital distress at baseline and treatment condition. Specifically, patients who reported lower levels of satisfaction at baseline and were randomized to the individual condition became even less satisfied with their marriage across time. Conversely, patients with lower satisfaction placed into the couples condition improved in marital satisfaction. Although a decrease in relationship satisfaction across time was unexpected, one possibility for this finding is that as patients in the individuals condition learned ways to change their own behavior in order to reduce risk, their partner may not have been on board with making those changes because they were not included in the group and thus did not receive this information. This lack of behavior change on the partner's part may then have frustrated the patient further when they started out already less satisfied with their relationships. Thus, these results suggest that if patients start out relatively unhappy in their relationships, in order to improve their relationship that relationship needs to be a focus of the intervention. And, because relationship satisfaction has been consistently found to be associated with positive behavior changes, this is all the more important when talking about cardiac patients.
Limitations to the current research
An important limitation to the study was the fact that only 28% of eligible patients agreed to participate in the intervention, making statistical power considerations an important factor in the interpretation of the study's findings. With our condition sizes, we had reliable power (power = .80) to detect only large effect sizes (d ~ 0.65). Because of this, it is difficult to distinguish between the absence of meaningful treatment condition effects, versus the simple lack of power to detect them. For this reason, and to assist in interpreting the effect sizes, we provide standardized effect sizes throughout the manuscript. Further, the conducted modeling approach assumes that data are missing at random, yet the verity of this assumption is often questionable. While we know from satisfaction surveys that those who participated (in both conditions) were very satisfied with the intervention, confirmed by the fact that there were no drop-outs in either condition between the intervention and the follow-up, the results can only be cautiously generalized to a cardiac population as a whole. Clearly, this was a group of patients and partners who were committed to the change process, whether or not they ultimately changed. Thus, the findings with these participants cannot be generalized to less motivated patients. In fact, this major limitation of interpretation necessitates more streamlined interventions for this population. Although the lengthy intervention described herein does rule out many possible patients that might have benefited from it, the importance of the inclusion of a partner in a more time limited intervention should not be dismissed. In fact, additional ways to include the partner in a behavior change program for cardiac risk reduction might be as simple as including the partner in standard cardiac rehabilitation programs which would at least expose the partner to the importance and type of changes necessary, if not necessarily focusing any part of the intervention on the partner or the relationship. This “partner attendance” method can be compared to a method similar to the one described here to more fully understand the scope of what is required of the partner for change.
Related to the potential `motivated participant' effect, results should be interpreted cautiously because it was the self-report data that changed across time. There are at least two alternate explanations for the findings. First, it is possible that cognitive dissonance was at play here in that participants reported more change because they worked so hard to obtain it. Second, it is well known that self report data can be positively skewed due the relationship that participants have formed with the research team and their subsequent desire to `present well'. Although a full discussion of such a `placebo' effect is beyond the scope of this paper, a very thorough explanation exists on the American Cancer Association website (http://www.cancer.org/treatment/treatmentsandsideeffects/treatmenttypes/placebo-effect). An argument against these possibilities is that participants changed differentially across treatment groups as a function of baseline DAS. If this was purely a self-report issue, differential change would not be expected because patients in both groups as well as those satisfied and not satisfied reported change. However, it stands to reason that more objective ratings of change need to be explored in future research.
Also, only a small percentage of patients in the study were female. While we understand why it was difficult to reaching married female cardiac patients, with only 13% females we cannot generalize our findings to women with cardiac disease. In contrast, the high percentage of ethnic and racial minority participation is a plus and helps to offset the gender homogeneity.
Third, these findings generalize only to patients living with intimate partners. Generalizability to other family or social relationships cannot be made.
Finally, our intervention involved much work for both the researchers and the participants (18 sessions total). While scientifically important with respect to internal validity, this burden will not translate to busy cardiology practices. A better way to intervene at the couples level for those who will benefit most should be found. The importance of developing interventions that will fit into the envirionments in which they will be used has been discussed in length by Glasgow and Kledges in their work (e.g. Glasgow & Klesges, 2003; Klesges, 2005).
Conclusion
This project was an important step forward in understanding the effect of a couples intervention on behavior change in a vulnerable population of cardiac patients, and particularly the importance of a satisfying intimate relationship on the behavior change process. An interesting and general finding was that a baseline variable (accessible by behavior change clinicians before initiating treatment) could be used to predict treatment success for several of the outcomes in that the level of relationship distress predicted response to treatment in several areas. More specifically, it appears that cardiac patients reduce their risk factors, particularly exercise, best when they are in satisfied relationships, where they may naturally include the partner in their change decisions. When they are unhappy, however, they can benefit from a couples focused intervention for risk reduction. Without such an intervention for patients in unhappy marriages, their risk profile does not improve, and in many cases it gets worse. Although a couples approach to behavior change may require additional clinical effort, it could be the key to sustained change for those who need it the most.
Acknowledgments
This grant was funded by the National Institutes of Health: Heart, Lung, and Blood Institute grant #5 RO1 HL62158-02.
References
- Atkins D, Berns S, George W, Doss B, Gattis K, Christensen A. Prediction of response to treatment in a randomized clinical trial of marital therapy. Journal of Consulting and Clinical Psychology. 2005;73(5):893–903. doi: 10.1037/0022-006X.73.5.893. [DOI] [PubMed] [Google Scholar]
- Baucom D, Porter LS, Kirby JS, Hudepohl J. Couple-based interventions for medical problems. Behavior Therapy. 2012;43(1):61–76. doi: 10.1016/j.beth.2011.01.008. doi: 10.1016/j.beth.2011.01.008. [DOI] [PubMed] [Google Scholar]
- Baucom D, Shoham V, Mueser KT, Daiuto AD, Stickle T. Empirically supported couple and family interventions for marital distress and adult mental health problems. Journal of Consulting and Clinical Psychology. 1998;66:53–88. doi: 10.1037//0022-006x.66.1.53. [DOI] [PubMed] [Google Scholar]
- Baucom DH, Epstein NH. Cognitive-Behavioral Marital Therapy. Brunner/Mazel; New York: 1990. [Google Scholar]
- Black DR, Gleser LJ, Kooyers KJ. A meta-analytic evaluation of couples weight-loss programs. Health Psychology. 1990;9(3):330–347. doi: 10.1037//0278-6133.9.3.330. [DOI] [PubMed] [Google Scholar]
- Broadwell SD, Light KC. Hostility, Conflict and Cardiovascular Responses in Married Couples: A Focus on the Dyad. International Journal of Behavioral Medicine. 2005;12(3):142–152. doi: 10.1207/s15327558ijbm1203_3. [DOI] [PubMed] [Google Scholar]
- Burman B, Margolin G. Analysis of the association between marital relationships and health problems: an interactional perspective. Psychological Bulletin. 1992;112:39–63. doi: 10.1037/0033-2909.112.1.39. [DOI] [PubMed] [Google Scholar]
- Christensen A, Atkins DC, Berns S, Wheeler J, Baucom DH, Simpson LE. Traditional versus integrative behavioral couple thereapy for signficiantly and chronically distressed married couples. Journal of Consulting and Clinical Psychology. 2004;72(2):176–191. doi: 10.1037/0022-006X.72.2.176. [DOI] [PubMed] [Google Scholar]
- Deci EL, Ryan RM. Intrinsic Motivation and Self-determination in Human Behavior. Plenum; New York: 1985. [Google Scholar]
- DiPietro L, Caspersen A, Ostfeld A, Nadel E. A survey for assessing physical activity among older adults. Medicine & Science in Sports & Exercise. 1993;25:628–642. [PubMed] [Google Scholar]
- Epstein NB, Baucom D. Enhanced Cognitive-Behavioral Therapy for Couples. American Psychological Association; Washington, D.C.: 2002. [Google Scholar]
- Eriksson M, Asplund K, Svedlund M. Couples' thoughts about and expectations of their future life after the patient's hospital discharge following acute myocardial infarction. Journal of Clinical Nursing. 2010;19(23–24):3485–3493. doi: 10.1111/j.1365-2702.2010.03292.x. doi: 10.1111/j.1365-2702.2010.03292.x. [DOI] [PubMed] [Google Scholar]
- Fappa E, Yannakoulia M, Pitsavos C, Skoumas I, Valourdou S, Stefanadis C. Lifestyle intervention in the management of metabolic syndrome: could we improve adherence issues? Nutrition. 2008;24(3):286–291. doi: 10.1016/j.nut.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Fletcher B, Berra K, Ades P, Braun LT, Burke L, Durstine J, et al. Managing abnormal blood lipids: a collaborative approach. Circulation. 2005;112(20):3184–3209. doi: 10.1161/CIRCULATIONAHA.105.169180. [DOI] [PubMed] [Google Scholar]
- Franks MM, Stephens MAP, Rook K, S., Franklin B, A., Keteyian S, J., Artinian N, T. Spouses' Provision of Health-Related Support and Control to Patients Participating in Cardiac Rehabilitation. Journal of Family Psychology. 2006;20(2):311. doi: 10.1037/0893-3200.20.2.311. [DOI] [PubMed] [Google Scholar]
- Franks MM, Wendorf CA, Gonzalez R, Ketterer M. Aid and influence: health promoting exchanges of older married partners. Journal of Social and Personal Relationships. 2004;21(4):431–445. [Google Scholar]
- Gay J, Saunders R, Dowda M. The Relationship of Physical Activity and the Built Environment within the Context of Self-Determination Theory. Annals of Behavioral Medicine. 2011;42(2):188–196. doi: 10.1007/s12160-011-9292-y. doi: 10.1007/s12160-011-9292-y. [DOI] [PubMed] [Google Scholar]
- Glasgow RW, Klesges LM. Evaluating and enhancing the reach dessimination of health promotion interventions: The Behaivor Change Consortium Retrieved October. 2003;25:2005. [Google Scholar]
- Goldsmith DJ, Lindholm KA, Bute JJ. Dilemmas of talking about lifestyle changes among couples coping with a cardiac event. Social Science & Medicine. 2006;63(8):2079–2090. doi: 10.1016/j.socscimed.2006.05.005. [DOI] [PubMed] [Google Scholar]
- Harada N, Chiu V, King A, Stewart A. An evaluation of three self-report physical activity instruments for older adults. Medicine & Science in Sports & Exercise. 2001;33:962–970. doi: 10.1097/00005768-200106000-00016. [DOI] [PubMed] [Google Scholar]
- Haynes RB. Introduction. In: Haynes RB, Taylor DW, Taylor DW, Sackett DL, editors. Compliance in health care. Johns Hopkins University Press; Baltimore: 1979. [Google Scholar]
- Hong T, B., Franks M, M., Gonzalez R, Keteyian S, J., Franklin B, A., Artinian N, T. A Dyadic Investigation of Exercise Support Between Cardiac Patients and Their Spouses. Health Psychology [PsycARTICLES] 2005;24(4):430. doi: 10.1037/0278-6133.24.4.430. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Follette WC, Revenstorf D, Baucom DH, Hahlweg K, Margolin G. Variability in outcome and clinical significance of behavioral marital therapy: A reanalysis of outcome data. Prevention & Treatment. 2000;3 doi: 10.1037//0022-006x.52.4.497. [DOI] [PubMed] [Google Scholar]
- Janis IL, Mann L. Decision making: A psychological analysis of conflict, choice, and commitment. Free Press; New York, NY US: 1977. [Google Scholar]
- Joekes K, Maes S, Warrens M. Predicting quality of life and self-management from dyadic support and overprotection after myocardial infarction. British Journal of Health Psychology. 2007;12(4):473–489. doi: 10.1348/135910706X118585. doi: 10.1348/135910706x118585. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Newton TL. Marriage and health: His and hers. Psychological Bulletin. 2001;127(4):472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Klesges LM, Estabrooks PA, Dzewaltowski DA, Bull SS, Glasgow RE. Beginning with the Application in Mind: Designing and planning health behavior change interventions to enhance dissemination. Annals of Behavior Medicine. 2005;29(Suppl):66–75. doi: 10.1207/s15324796abm2902s_10. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Berkowitz RI, Hammer LD. Methodological difficulties in studies of obesity. I. Measurement issues. 1990;12:112–118. [Google Scholar]
- Kruse W, Nikolaus T, Rampmaier J, Weber E, Schierf G. Actual versus prescribed timing of lovastatin doses assessed with electronic compliance monitoring. European Journal of Clinical Pharmacology. 1993;44:211–215. doi: 10.1007/BF00315385. [DOI] [PubMed] [Google Scholar]
- Levenson RW, Gottman JM. Physiological and affective predictors of change in relationship satisfaction. Journal of Personality and Social Psychology. 1985;49:85–94. doi: 10.1037//0022-3514.49.1.85. [DOI] [PubMed] [Google Scholar]
- Markey C, Markey PM, Birch L, L. Interpersonal Predictors of Dieting Practices Among Married Couples. Journal of Family Psychology [PsycARTICLES] 2001;15(3):464. doi: 10.1037//0893-3200.15.3.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire L, M., Lustig AP, Schulz R, Miller GE, Helgeson VS. Is It Beneficial to Involve a Family Member? A Meta-Analysis of Psychosocial Interventions for Chronic Illness. Health Psychology. 2004;23(6):599. doi: 10.1037/0278-6133.23.6.599. [DOI] [PubMed] [Google Scholar]
- Oldridge NB, Jones NL. Preventive use of exercise rehabilitation after myocardial infarction. Acta Med Scand. 1986;711(Suppl):123–129. doi: 10.1111/j.0954-6820.1986.tb08940.x. [DOI] [PubMed] [Google Scholar]
- Prochaska DO, DiClemente CC. Transtheoretical therapy: Toward a more integrative model of change. Psychotherapy Theory, Research and Practice. 1982;19:276–288. [Google Scholar]
- Raudenbush SW, Brennan RT, Barnett RC. A multivariate hierarchical model for studying psychological change within married couples. Journal of Family Psychology. 1995;9:161–174. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- Raudenbush SW, Byrk AS, Cheong YF, Congdon RT. HLM 6: Hierarchical Linear and Nonlinear Modeling. Scientific Software International; Lincolnwood, IL: 2004. [Google Scholar]
- Raudenbush SW, Liu X. Effects of study duration, frequency of observation, and sample size on power in studies of group differences in polynomial change. Psychological Methods. 2001;6(4):387–401. [PubMed] [Google Scholar]
- Remien RH, Stirratt MJ, Dolezal C, Dognin JS, Wagner GJ, Carballo-Dieguez A, Jung TM. Couple-focused support to improve HIV medication adherence: A randomized controlled trial. AIDS. 2005;19(8):807–814. doi: 10.1097/01.aids.0000168975.44219.45. [DOI] [PubMed] [Google Scholar]
- Sackett DL, Snow JC. The magnitude and measurement of compliance. In: Haynes RB, Taylor DW, Sackett DL, editors. Compliance in health care. Johns Hopkins University Press; Baltimore: 1979. [Google Scholar]
- Schumm K, Skea Z, McKee L, N'Dow J. 'They're doing surgery on two people': A meta-ethnography of the influences on couples treatment decision making for prostate cancer. Health Expectations: An International Journal of Public Participation in Health Care & Health Policy. 2010;13(4):335–349. doi: 10.1111/j.1369-7625.2010.00624.x. doi: 10.1111/j.1369-7625.2010.00624.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Services, D. o. H. a. H. Translating basic behavioral and social sciences discoeries into interventions to reduce obesity. 2008. [Google Scholar]
- Sher TG, Bellg AJ, Braun L, Domas A, Rosenson R, Canar WJ. Partners for Life: A theoretical approach to developing an intervention for cardiac risk reduction. Health Education Research. 2002;17:597–605. doi: 10.1093/her/17.5.597. [DOI] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976;38:15–28. [Google Scholar]
- Vilchinsky N, Dekel R, Leibowitz M, Reges O, Khaskia A, Mosseri M. Dynamics of support perceptions among couples coping with cardiac illness: The effect on recovery outcomes. Health Psychology. 2011;30(4):411–419. doi: 10.1037/a0023453. doi: 10.1037/a0023453. [DOI] [PubMed] [Google Scholar]