Abstract
Background
The majority of established telestroke services are based on “hub‐and‐spoke” models for providing acute clinical assessment and thrombolysis. We report results from the first year of the successful implementation of a locally based telemedicine network, without the need of 1 or more hub hospitals, across a largely rural landscape.
Methods and Results
Following a successful pilot phase that demonstrated safety and feasibility, the East of England telestroke project was rolled out across 7 regional hospitals, covering an area of 7500 square miles and a population of 5.6 million to enable out‐of‐hours access to thrombolysis. Between November 2010 and November 2011, 142 telemedicine consultations were recorded out‐of‐hours. Seventy‐four (52.11%) cases received thrombolysis. Median (IQR) onset‐to‐needle and door‐to‐needle times were 169 (141.5 to 201.5) minutes and 94 (72 to 113.5) minutes, respectively. Symptomatic hemorrhage rate was 7.3% and stroke mimic rate was 10.6%.
Conclusions
We demonstrate the safety and effectiveness of a horizontal networking approach for stroke telemedicine, which may be applicable to areas where traditional “hub‐and‐spoke” models may not be geographically feasible.
Keywords: NHS, telestroke, thrombolysis
Introduction
Telestroke is becoming a widespread and fast growing practice model for increasing access to thrombolysis. The European Stroke Organisation1 and the American Heart Association/American Stroke Association2 have both issued guidelines encouraging the formation of telestroke networks and development of teleconsultation services. Most current academic medical center‐based telestroke programs are based on variations of the “hub‐and‐spoke”3–4 model, whereby 1 or more regional centers provide expertise via a telecommunication link to peripheral centers. These models may be challenging to implement in largely rural landscapes, where transport links to regional centers present difficulties.
The East of England is a large, predominantly rural region covering 7500 square miles, a population of 5.6 million people, and approximately 6000 stroke patients, annually. Prior to the current telemedicine set up in November 2010, there were 2 regional centers providing thrombolysis 7 days a week, 24 hours a day. Projected ambulance travel time of 45 to 60 minutes from peripheral centers to either one of these 2 regional centers ruled out a 2‐hub model of telestroke in our region. This motivated horizontal organization of the program, which was rolled out following successful completion of a pilot project between September 2009 and January 2010.
Figures from the Department of Health, UK suggest that ≤5% of stroke patients are thrombolyzed on average across the country.5 In our region alone, by increasing the thrombolysis rates to an average of 10%, the estimated cost savings to the National Health Service (NHS) would be nearly £2.7 million, by preventing long‐term disability. Based on figures from the European Safe Implementation of Treatments in Stroke (SITS) database6 for our region for 2009–2010, 382 stroke patients received thrombolysis for stroke. Thus, for an average annual load of 6000 cases, average overall thrombolysis rates are ≈6.36% across the region.
Methods
Organization of the Network
The East of England telestroke project is hosted jointly by the Cambridge University Hospitals NHS Foundation Trust and the regional Strategic Health Authority. The program runs across 7 hospitals (Figure), namely, Ipswich Hospital, James Paget University Hospital, Lister Hospital, Peterborough Hospital, Queen Elizabeth Hospital, Watford General Hospital, and West Suffolk Hospital. All these hospitals are classified as district general hospitals with an inpatient capacity of approximately 500 beds. Detailed bed size figures and annual emergency attendance numbers, as obtained from the NHS Information Centre for Health and Social Care,7 are outlined in the figure. Each of these hospitals runs their own thrombolysis rotas during working hours with on‐site stroke specialists. The main objective of the telemedicine service is to provide real‐time, out‐of‐hours access to thrombolysis, ie, evenings (17:00 to 08:00), weekends and bank holidays. A regional rota of 10 stroke specialists from across the sites has been created to deliver the service. All participating specialists had attended regional thrombolysis training days, had access to case discussions in peer‐review format via regional videoconferencing meetings and were registered users for the European Safe Implementation of Treatments in Stroke (SITS) database. Thrombolysis was administered as per standard clinical guidelines and the time window for thrombolysis was 0 to 4.5 hours. Definition of symptomatic intracranial haemorrhage (sICH) was the same as that from the NINDS trial, ie, any deterioration in neurological status accompanied by intracranial haemorrhage.8–9
Figure 1.
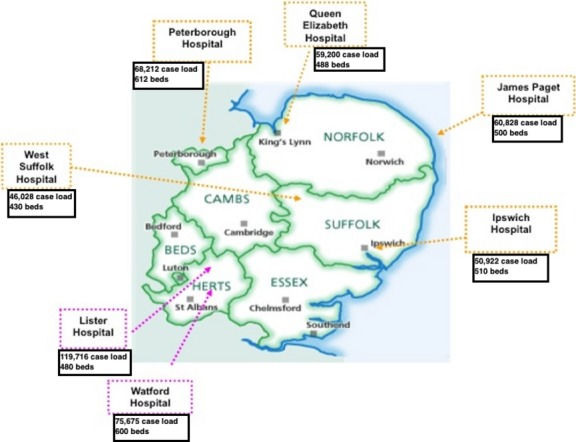
Geographical organization of the East of England telestroke network. As per data from National Health Service (NHS) Information Centre for Health and Social Care, annual overall emergency attendances (case load for all emergency cases, not stroke alone) and hospital bed size for each of the participating sites is shown for 2009–2010, except for Lister Hospital for which these figures were not available and thus 2012–2013 figures have been mentioned.
Technology and Process
The telemedicine cart, provided to the emergency departments of participating hospitals, is comprised of of a PC in a bespoke mobile trolley (Parity Medical®) with an additional high‐resolution CCTV camera mounted on top of the screen. Each consultant has access to a 17′′ laptop coupled to the telemedicine cart using Visimeet® videoconferencing software, allowing rapid access to the virtual consultation “room” accessed by a wired/less connection to a dedicated server on a secure NHS (N3) network. The clinical team at the participating hospital can view and speak to the remote telestroke consultant via the cart, using the camera that can be controlled from both sides.
Approvals
The telemedicine project was reviewed and approved by the institutional review boards at the individual hospitals and the Strategic Health Authority for administration of thrombolysis via standard clinical guidelines.1 Verbal consent was obtained from the patient or next of kin prior to telemedicine consultation.
The project was registered with the institutional review boards at each site for prospective audit data collection, for the pilot phase, and subsequently for the first year of service roll‐out. Anonymized clinical information was retrieved from prospectively recorded audit data.
Statistical Analysis
All data were analyzed using IBM SPSS 19® for Mac. Mean values with standard deviations (SD) and median values with interquartile ranges (IQR) are reported here with comparisons between patients in “thrombolysis” and “no thrombolysis” groups, using 2‐sample t tests and Wilcoxon rank sum test where appropriate, alongside 2‐sided P values.
Results
For safety and feasibility assessment, a pilot phase was run between September 2009 and January 2010 across 4 regional hospitals. Forty‐three telestroke consultations were recorded leading to 15 patients receiving thrombolysis. Mean (range) consultation length was 30 (10 to 70) minutes for the cases that received treatment versus 18 (2 to 55) minutes for the others. Mean age of patients was 72 years (range 54 to 88), median NIHSS 13, mean door‐to‐needle time 56 minutes, mean onset‐to‐needle time 131 minutes and there were no symptomatic hemorrhages; asymptomatic hemorrhage rate was 13.3%.
Following on from the successful pilot phase, 164 consultations were recorded between November 2010 and November 2011. Clinical data were incomplete for 22 cases; hence, 142 cases (Table 1) are included in this report. Overall, 74 patients received thrombolysis. Mean (SD) age of “thrombolysis” group was 69.4 (14.3) years; for “no thrombolysis” group, 65.7 (16) years. Median NIHSS was higher (10 versus 5, P=0.006) in the “thrombolysis” group. Median door‐to‐scan time was comparable (P=0.748) between the 2 groups. For the “thrombolysis” group, median (IQR) door‐to‐needle time was 94 (72 to 113.5) minutes and median (IQR) onset‐to‐needle time was 169 (141.5 to 201.5) minutes.
Table 1.
Baseline Characteristics of Patients in the Telestroke Cohort
| Thrombolysis (N=74) | No Thrombolysis (N=68) | P Value | |
|---|---|---|---|
| Age (y), mean (SD) | 69.4 (14.3) | 65.7 (16) | 0.15 |
| Male:female | 53:21 | 35:33 | 0.02 |
| NIHSS, median (IQR) | 10 (5.75 to 15.25) | 5 (3 to 12.5) | 0.01 |
| Onset to needle (min), median (IQR) | 169 (141.5 to 201.5) | n/a | n/a |
| Door to needle (min), median (IQR) | 94 (72 to 113.5) | n/a | n/a |
| Door to scan (min), median (IQR) | 29.5 (22.5 to 55) | 40 (26 to 51) | 0.75 |
| Hemorrhage rate (NINDS)8 | 7.3% | n/a | n/a |
| In hospital mortality | 8.1% | 7.4% | 0.78 |
| Call duration (min), mean (SD) | 32.9 (15.1) | 26.9 (42.2) | 0.40 |
Mean call duration available for 89 cases overall; n=50 thrombolyzed cases and n=39 for cases not thrombolyzed. Five cases of unknown onset time, none received thrombolysis. Follow‐up scans unavailable in 9 cases that were thrombolyzed, sICH rates 5/69=7.3%. IQR indicates interquartile ranges; NINDS, National Institute of Neurological Disorders and Stroke; NIHSS, National Institutes of Health Stroke Scale.
Among the 68 cases that did not receive thrombolysis, 18 were stroke mimics including migraine, seizures, and functional illness. Reasons for not treating patients with a final diagnosis of stroke included uncertain time of onset (n=7), severe stroke with comorbidities and high hemorrhage risk (n=4), low NIHSS at presentation and/or improving neurological deficit at the time of assessment (n=23), ≥1 recognized contraindications for thrombolysis (n=10),1 hemorrhage on initial CT (n=6), age with comorbidities (n=1, age=93 years). In 2 cases, the reason for not administering treatment was unclear from the available data.
We also provide a comparison of our performance against figures from major published telestroke series across the world (Table 2).
Table 2.
Comparison of Thrombolysis Figures From Representative Published Telestroke Programs Around the World and the East of England (EoE) Project
| TEMPiS10 | REACH11 | STRokE DOC12 | Finnish Telestroke13 | EoE Telestroke | Pilot Results | NINDS Trial8 | |
|---|---|---|---|---|---|---|---|
| Area | Regional | Regional | Regional | National | Regional | Regional | |
| Hub/spoke | 2/12 | 1/8 | 1/4 | 1/5 | n/a | n/a | n/a |
| Thrombolysis n | 106 | 30 | 31/25* | 61 | 74 | 15 | |
| Mean age, y | 68 | 62 | 70.4/69* | 61 | 69 | 72 | 67 |
| Median NIHSS score | 12 | 11.5 | 12.7/9.8** | 10 | 10 | 13 | 14 |
| Mean onset to needle time, min | 141 | 122 | 157.2/143.2* | 130 | 170.1 | 131 | Not reported |
| Mean door to needle time, min | 76 | 104.9 | Not reported | 24 | 94.9 | 56 | Not reported |
| Hemorrhage rate% | 8.5 | 0 | 7/8* | 6.7 | 7.3 | 0 | 6.4 |
| In hospital mortality% | 10.4 | 7 | Not reported | 9.8 | 8.1 | Not reported | Not reported |
n/a not applicable.
Telemedicine/telephone only consultations.
Mean NIHSS described in these studies.
Quarterly audit figures for thrombolysis rates prior to and post commencement of telemedicine are available for 5 of the 7 hospitals (Table 3). Note that the pre‐telemedicine figures represent daytime thrombolysis activity as these hospitals did not have an out‐of‐hours service before telemedicine was set up.
Table 3.
Quarterly Thrombolysis Figures From Audit Data Prior to and After Roll out of the Telemedicine Service
| Hospital | Pre Telemedicine Thrombolysis Rate (%) | Post Telemedicine Thrombolysis Rate (%) |
|---|---|---|
| West Suffolk Hospital | 1 | 12 |
| Peterborough Hospital | 6 | 7 |
| Queen Elizabeth Hospital | 4 | 13 |
| James Paget Hospital | 5 | 14 |
| Ipswich Hospital | 4 | 9 |
Note that these figures were not available for 2 of the 7 hospitals, namely Lister Hospital and Watford Hospital. Pre thrombolysis rates represent daytime activity whereas post telemedicine rates, when the thrombolysis service became 24×7, are overall rates including daytime and out‐of‐hours work.
Discussion
Our series demonstrates that a locally based model for telestroke consultations is deliverable and safe. The novelty of this structure is that local stroke physicians participate in the regional service; thus delivery is not dependent on regional centers. This has advantages for local specialists in that they retain competencies in treating sufficient numbers of thrombolysis cases, even though their own services are relatively small; while more effectively sharing the burden of overnight call for low‐frequency, high‐impact events. Also, it has potential logistic advantages in organizing follow‐up care. This hubless model of organization of our telestroke network is what distinguishes it from the majority of other successfully running telestroke services across the world.3–4 Keeping services local has particular advantages in relatively large rural landscapes by minimizing dependence on regional transport services and developing rehabilitation and follow‐up care for patients closer to where they live.
Our figures compare well with published telemedicine series, apart from slightly longer door‐to‐needle and onset‐to‐needle time, which may partly be a reflection of our geographical location and transport challenges.2–3 While our door to scan times are comparable to published UK‐wide time metrics from the SITS database for a similar time period (Median onset‐to‐needle=150 minutes, door‐to‐needle=65 minutes, door‐to‐scan=31 minutes)14 and the Stroke Improvement National Audit Programme published by the Royal College of Physicians, UK15 (Median door‐to‐needle=60 minutes, door‐to‐scan=32 minutes), our door‐to‐needle and onset‐to‐needle times could be improved further. Attempts, such as involvement of on‐site specialist nurses, are underway for further improvement. However, the differences need to be interpreted in light of the fact that the telemedicine service runs for out‐of‐hours only and direct comparisons or out‐of‐hours figures are not available for each site or separately from national audit figures.
Our teleconsultation thrombolysis rate (52.1%) approaches the highest figure reported to date, from the Finnish telestroke network (57.5%)13 and compares well with earlier models such as TEMPiS (29.8%)10 and REACH (15.5%).11 The high rate of thrombolysis may suggest that the service may be currently underutilized. Besides, the number of overall consultations in the first year of service roll out is smaller than some of the well‐established telestroke projects like TEMPiS.16 Thus, our model has potential for a greater impact on thrombolysis delivery with further establishment of its role. As outlined earlier, average overall thrombolysis rate in our region is around 6%. Table 3 shows an increase in thrombolysis activity for the hospitals, where quarterly audit data for overall thrombolysis rates were available before and after commencing telemedicine.
Symptomatic hemorrhage rate of 7.3% is at par with other series and early trial data (Table 2). Also, noteworthy is that no cases of in‐hospital mortality occurred due to hemorrhage, indicating safety of the approach.
Mean call duration data (available for n=89 cases; Table 1) did not differ between the 2 groups (P=0.395). Median NIHSS was lower, as expected, in the “no thrombolysis” group, with presence of stroke mimics and cases with improving neurological deficits.
It would be interesting to examine whether there is meaningful variability in how well the network works for different hospitals and whether the success depends on local expertise and/or varying patient populations. While Table 3 highlights this variability, the sample size for the project data is too small to examine such factors for each site individually. Further long‐term data would be needed to investigate these systematically.
One of the limitations in our data is the unavailability of long‐term clinical outcomes. Currently, the project is successfully running across 14 hospitals, from which further clinical data collection is in progress. Also, cost savings and resource implications merit further assessment.
Conclusion
In summary, the East of England telestroke project has demonstrated safe and efficacious delivery of an out‐of‐hours thrombolysis service across regional hospitals in a large rural landscape.
Sources of Funding
This study was supported by East of England SHA.
Disclosures
None.
Acknowledgments
Jim Bibby, East of England Strategic Health Authority, for IT support. Genevieve Dalton, East of England Strategic Health Authority and Anglia Stroke and Heart Network, for support with management issues. S.A. was supported by a National Institute of Health Research Biomedical Centre Grant to Clinical Neurosciences, Cambridge, UK.
References
- 1.European Stroke Organisation (ESO) Executive Committee, ESO Writing Committee Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis. 2008; 25:457-507 [DOI] [PubMed] [Google Scholar]
- 2.Schwamm LH, Holloway RG, Amarenco P, Audebert HJ, Bakas T, Chumbler NR, Handschu R, Jauch EC, Knight WA, Levine SR, Mayberg M, Meyer BC, Meyers PM, Skalabrin E, Wechsler LRAmerican Heart Association Stroke Council, Interdisciplinary Council on Peripheral Vascular Disease A review of the evidence for the use of telemedicine within stroke systems of care: a scientific statement from the American Heart Association/American Stroke Association. Stroke. 2009; 40:2616-2634 [DOI] [PubMed] [Google Scholar]
- 3.Silva GS, Farrell S, Shandra E, Viswanathan A, Schwamm LH. The status of telestroke in the United States: a survey of currently active stroke telemedicine programs. Stroke. 2012; 43:2078-2085 [DOI] [PubMed] [Google Scholar]
- 4.de Bustos EM, Vuillier F, Chavot D, Moulin T. Telemedicine in stroke: organizing a network‐rationale and baseline principles. Cerebrovasc Dis. 2009; 27suppl 4:1-8 [DOI] [PubMed] [Google Scholar]
- 5.Intercollegiate Stroke Working Party Public Report for England, Wales and Northern Ireland. 2011;1–96 Available at: http://www.rcplondon.ac.uk/sites/default/files/national-sentinel-stroke-audit-2010-public-report-and-appendices_0.pdf Accessed January 20, 2014.
- 6.Safe Implementation of Treatments in Stroke (SITS) registry 2011. Available at: https://sitsinternational.org/homefoldercontent/publications/sits-publications Accessed January 20, 2014.
- 7.NHS Information Centre for Health and Social Care 2011. Available at: http://data.gov.uk/publisher/nhs-information-centre-for-health-and-social-care Accessed January 20, 2014.
- 8.NINDS rtPA Stroke Study Group Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995; 333:1581-1587 [DOI] [PubMed] [Google Scholar]
- 9.Derex L, Nighoghossian N. Intracerebral haemorrhage after thrombolysis for acute ischaemic stroke: an update. J Neurol Neurosurg Psychiatry. 2008; 79:1093-1099 [DOI] [PubMed] [Google Scholar]
- 10.Audebert HJ, Kukla C, Clarmann von Claranau S, Kühn J, Vatankhah B, Schenkel J, Ickenstein GW, Haberl RL, Horn MTEMPiS Group Telemedicine for safe and extended use of thrombolysis in stroke: the Telemedic Pilot Project for Integrative Stroke Care (TEMPiS) in Bavaria. Stroke. 2005; 36:287-291 [DOI] [PubMed] [Google Scholar]
- 11.Wang S, Gross H, Lee SB, Pardue C, Waller J, Nichols FT, Adams RJ, Hess DC. Remote evaluation of acute ischemic stroke in rural community hospitals in Georgia. Stroke. 2004; 35:1763-1768 [DOI] [PubMed] [Google Scholar]
- 12.Meyer BC, Raman R, Hemmen T, Obler R, Zivin JA, Rao R, Thomas RG, Lyden PD. Efficacy of site‐independent telemedicine in the STRokE DOC trial: a randomised, blinded, prospective study. Lancet Neurol. 2008; 7:787-795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sairanen T, Soinila S, Nikkanen M, Rantanen K, Mustanoja S, Färkkilä M, Pieninkeroinen I, Numminen H, Baumann P, Valpas J, Kuha T, Kaste M, Tatlisumak TFor the Finnish Telestroke Task Force Two years of Finnish Telestroke: thrombolysis at spokes equal to that at the hub. Neurology. 2011; 76:1145-1152 [DOI] [PubMed] [Google Scholar]
- 14.British Association of Stroke Physicians 2011. [cited 2013]. Available at: http://www.basp.ac.uk/Portals/2/BASP%20Masterclass%20Mar%202011%20Thrombolysis%20evidence%20update%20handout.pdf Accessed January 20, 2014.
- 15.Stroke Improvement National Audit Programme. http://www.rcplondon.ac.uk/sites/default/files/sinap-comprehensive-public-report-2012.pdf [Google Scholar]
- 16.Audebert HJ, Schenkel J, Heuschmann PU, Bogdahn U, Haberl RLTelemedic Pilot Project for Integrative Stroke Care Group Effects of the implementation of a telemedical stroke network: the Telemedic Pilot Project for Integrative Stroke Care (TEMPiS) in Bavaria, Germany. Lancet Neurol. 2006; 5:742-748 [DOI] [PubMed] [Google Scholar]


