Abstract
Background
The mortality rate from cardiovascular disease (CVD) among young adults has declined less than that in the older population, raising concerns about the increasing prevalence of obesity‐related conditions including hypercholesterolemia in the younger population. We investigated the age‐standardized mean levels of serum cholesterols and the prevalence, awareness, treatment and control rates of hyper‐low‐density lipoprotein (LDL)‐cholesterolemia based on age.
Methods and Results
Nationally representative samples of 19 489 subjects aged ≥20 years were analyzed from the Korea National Health and Nutrition Examination Surveys 2008–2010. Hyper‐LDL‐cholesterolemia was individually evaluated by the 2004 National Cholesterol Education Program Adult Treatment Panel III guidelines. Age‐standardized mean levels of total cholesterol, high‐density lipoprotein‐cholesterol, LDL‐cholesterol, and triglycerides were 186.8, 48.0, 112.9, and 136.0 mg/dL, respectively. Age‐standardized prevalence of hyper‐LDL‐cholesterolemia was 23.2% (men, 25.5%; women, 21.8%). Among subjects with hyper‐LDL‐cholesterolemia, awareness and treatment rates were significantly lower in younger adults (<50 years) compared to older adults ≥50 years (awareness, 8.0% versus 21.5%; treatment, 5.1% versus 18.5%, all Ps<0.001), indicating significant discrepancies in awareness and treatment rates of hypercholesterolemia between younger and older adults. Among subjects aware of their hyper‐LDL‐cholesterolemia, younger adults were more likely to have controlled LDL‐cholesterol than the elderly (82.1% versus 67.5%, P<0.001).
Conclusions
Compared to the elderly, significant proportions of young and middle‐aged adults are unaware of their hypercholesterolemia and are not treated with proper lipid‐lowering medications. Early screening, education, and proper management should be stressed in national public healthcare policies to reduce the increasing burden of CVD in the younger population with undiagnosed hypercholesterolemia.
Keywords: cholesterol, epidemiology, hypercholesterolemia, low‐density lipoprotein cholesterol
Introduction
Cardiovascular disease (CVD) is one of the major leading causes of morbidity and mortality worldwide.(2011)–(2008) A high level of total cholesterol (TC) and low‐density lipoprotein cholesterol (LDL‐C) is recognized as a significant contributing factor to the initiation and progression of atherosclerosis, an important risk factor for CVD.(2011)–(2009) Numerous clinical trials have demonstrated the efficacy and safety of lipid‐lowering drugs, primarily statins, in reducing CVD risk.(2005)–(1995) However, a large proportion of adults with high TC and LDL‐C still remain underdiagnosed and undertreated in the United States.(2009) Data from the National Health and Nutrition Examination Survey (NHANES), 2005–2008 shows that 33.5% of adults in the United States aged ≥20 years have high LDL‐C, but only 48.1% of them are treated.(2011) It has been also reported that 49.1% of the United States population with TC ≥240 mg/dL are unaware of their condition.(2003) Based on data from the World Health Organization Multinational Monitoring of Trends and Determinants in Cardiovascular Disease (MONICA) project, the average rate of hypercholesterolemia awareness is only 36% (ranging from 3% [0%] to 62% [65%] in men [women]).(2005) Recently, it has become clear that earlier treatment beginning at age 30 or 35 years can improve the impact of lowering blood cholesterol level on CVD risk, thanks to advances in our understanding of the mechanisms regulating blood cholesterol level and the genes involved in that regulation.(2012) Therefore, early screening, diagnosis, and treatment of hypercholesterolemia are important to decrease the incidence of CVD in high‐risk subjects.
The prevalence of hypercholesterolemia varies considerably among population groups.(2005) Variations in diet, adiposity, and the use of drugs to lower cholesterol level have led to differences in serum cholesterol concentrations across populations and over time.(2011) One recent longitudinal study has clearly demonstrated that CVD mortality is not significantly decreased in young adults compared with older ones over a time period of 20 years,(2007) indicating that a large number of younger adults are not sufficiently protected from CVD deaths in spite of marked developments in pharmacotherapy and intervention techniques to manage CVD. To date, no study has yet examined differences in awareness and treatment rates of hypercholesterolemia between younger and older age groups. Besides the NHANES data from the United States, there are few well‐conducted national reports on awareness, treatment and control rates of hypercholesterolemia in the general population of other countries, especially in Asia.(2004) Therefore, we analyzed data from the Korea National Health and Nutrition Examination Survey (KNHANES) conducted in 2008–2010, which was designed by the Ministry of Health and Welfare to regularly assess the health and nutritional status of the civilian, non‐institutionalized population of Korea. Hyper‐LDL‐cholesterolemia was determined after calculating individual risks by the National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) Guidelines.(2004) The aims of this study were (1) to investigate the levels of serum cholesterols and the prevalence, awareness, treatment, and control of subjects with high LDL‐C and (2) to examine differences in awareness, treatment and control rates between age groups in the general Korean population.
Methods
Study Participants
Data for this current study were derived from the KNHANES conducted in 2008–2010. The KNHANES is a nationwide cross‐sectional study regularly conducted by the Division of Chronic Disease Surveillance, Korea Centers for Disease Control and Prevention of the Ministry of Health and Welfare to assess the general health and nutrition status of the civilian, non‐institutionalized population of Korea.(2013) The KNHANES includes 4 surveys: a health interview survey, a health behavior survey, a health examination survey, and a nutrition survey.(2012) A total of 29 235 individuals participated in the KNHANES 2008–2010 (Figure 1). Among these participants, we excluded individuals who were aged <20 years (n=7664) and whose lipid profiles were not assessed in the survey (n=2082). Finally, a total of 19 489 subjects (8382 men and 11 107 women) were analyzed. Written informed consent was secured from all participants and KNHANES was conducted based on ethical approval by Institutional Review Board of Korea Center for Disease Control and Prevention (No: 2008‐04EXP‐01‐C, 2009‐01CON‐03‐2C, 2010‐02CON‐21‐C).
Figure 1.
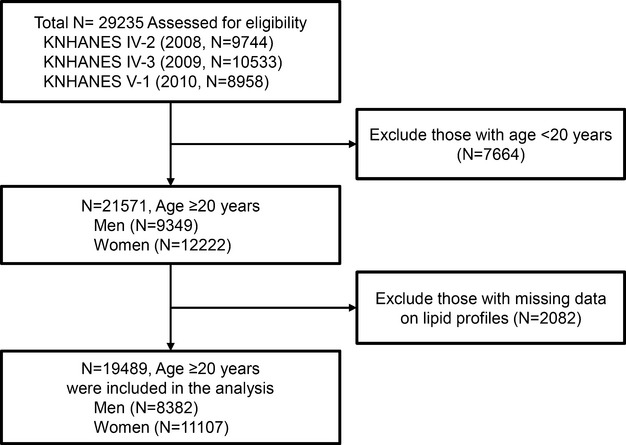
Flow diagram of participant inclusion and exclusion in the Korea National Health and Nutrition Examination Surveys 2008–2010 (KNHANES IV‐2, ‐3, and V‐1).
Measurements of Anthropometric and Laboratory Parameters
Blood samples collected from each subject during the survey were processed, refrigerated immediately, transported in cold storage to the central laboratory (Neodin Medical Institute, Seoul, Korea) and analyzed within 24 hours after transportation.(2013) TC, high‐density lipoprotein cholesterol (HDL‐C), triglycerides (TG) and fasting glucose levels were determined using a Hitachi 7600 automated chemistry analyzer (Hitachi, Tokyo, Japan). LDL‐C was calculated using the Friedewald formula: [LDL‐C (mg/dL)=TC (mg/dL)−{HDL‐C (mg/dL)+TG (mg/dL)/5}] if the TG level was low (≤400 mg/dL) and measured directly using the Hitachi 7600 analyzer if the TG level was high (>400 mg/dL).
Body mass index (BMI) was determined as the ratio of weight to height (kg/m2). Standardized health questionnaires were used to determine behavior and lifestyle characteristics including cigarette smoking status (never or past/current). Blood pressure was measured 3 times on the right arm while the individual was in a seated position after at least 5 minutes of rest using a mercury sphygmomanometer (Baumanometer; W.A. Baum Co.). The final blood pressure value was obtained by averaging the second and third blood pressure readings.
Definitions
We applied the definition of obesity in the Asian‐Pacific region (BMI ≥25 kg/m2) to categorize participants as obese.(2011) Diabetes mellitus was defined on the basis of (1) insulin or oral hypoglycemic agent use or (2) fasting plasma glucose ≥126 mg/dL. Impaired fasting glucose was defined as a fasting plasma glucose of 100 to 125 mg/dL.(2010) Subjects were diagnosed as hypertensive if systolic pressure was ≥140 mm Hg, if diastolic pressure was ≥90 mm Hg, or if current antihypertensive medication was used, according to standards based on the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7).(2003) Hyper‐LDL‐cholesterolemia was defined based on the individual's LDL‐C goals recommend by the 2004 update of the ATP III guidelines.(2004) In addition, all participants who currently reported using cholesterol‐lowering agents were considered to have high LDL‐C. Awareness and treatment of hyper‐LDL‐cholesterolemia were examined in the health interview survey by self‐report. Subjects who answered, “yes” to the question “Do you currently have high cholesterol or have you heard from medical personnel that your blood cholesterol level was high?” were considered aware of their high cholesterol. Subjects who reported “yes” to the question “Are you currently using cholesterol‐lowering medication?” were considered to be receiving treatment. Control of hyper‐LDL‐cholesterolemia was defined based on the individual LDL‐C goals suggested by the 2004 update of the ATP III guidelines(2004) after evaluation of their cardiovascular risks (Table 1).
Table 1.
Criteria for Hyper‐LDL‐cholesterolemia and LDL‐cholesterol Control in subjects as defined by the 2004 National Cholesterol Education Program Adult Treatment Panel III Guidelines(2004)
| Risk Category | Definition | |
|---|---|---|
| Hyper‐LDL‐Cholesterolemia | Controlled LDL‐C | |
| High risk: CHD* or CHD risk equivalents* | LDL‐C ≥100 mg/dL (70 mg/dL*) or use of lipid‐lowering medications | LDL‐C <100 mg/dL (70 mg/dL*) |
| Moderate risk: CHD risk factors* ≥2 | LDL‐C ≥130 mg/dL or use of lipid‐lowering medications | LDL‐C <130 mg/dL |
| Low risk: 0 to 1 CHD risk factors | LDL‐C ≥160 mg/dL or use of lipid‐lowering medications | LDL‐C <160 mg/dL |
CHD indicates coronary heart disease; LDL‐C, low‐density lipoprotein cholesterol.
CHD includes history of myocardial infarction, unstable angina, stable angina.
CHD risk equivalents include carotid artery disease (stroke), and diabetes.
Subjects in the category of very high risk: patients with history of acute myocardial infarction, CHD plus (1) diabetes, (2) severe and poorly controlled risk factors (especially continued cigarette smoking), (3) multiple CHD risk factors ≥2.
CHD risk factors include older age (≥55 years for women and ≥45 years for men), current cigarette smoking, hypertension, and low high‐density lipoprotein cholesterol (HDL‐C <40 mg/dL).
Statistical Analysis
The standardized prevalence, awareness, and treatment rates were calculated for sex and age, specific to the Korean population, as provided by the Office for National Statistics in 2010 to adjust and reflect the age structure of the 2010 general population in Korea. We also applied the stratification variables and sampling weights for all analyses designated by the Korean Centers for Disease Control and Prevention, which were derived from the sample design of each survey year.(2012) Sampling weights were applied to all calculations to obtain nationally representative prevalence estimates in Korea. These weights, which account for the demographic characteristics of certain areas where participants were sampled, reflect the unequal probabilities of selection of subjects, participant nonresponse, and poststratification. We stratified our analyses by age, sex, region, and family income (quartiles). Household income was calculated according to the monthly equivalized gross household income (the equivalized gross household income is the total household income divided by the root of the number of household members) and categorized into 4 quartiles as low, low middle, high middle, high. Student t test or one‐way analysis of variance with sampling weights was used to compare variables among genders or age groups. Categorical variables were compared using Rao‐Scott χ2 test with sampling weights. SAS version 9.2 (SAS Institute) and SPSS version 20.0 for Windows (IBM Corp) were used to analyze the complex sampling design of KNHANES and results with a P value <0.05 were considered significant.
Results
Characteristics of the General Korean Population
From KNHANES 2008–2010, 19 489 individuals (6529 in 2008, 7089 in 2009, and 5871 in 2010) were included in our study. Table 2 displays the clinical features of the sample stratified by age. In both men and women, subjects aged 30 to 60 years were recruited more heavily than the other age groups in order to reflect the current age distribution in Korean society. Across all age groups, 31% (26%) men (women) were hypertensive and 11% (9%) men (women) were diabetic. More men than women were overweight/obese and reported a lifetime history of smoking.
Table 2.
Characteristics of Study Subjects in Korea, 2008–2010
| KNHANES 2008–2010 | P Value | ||
|---|---|---|---|
| Male (N=8382) | Female (N=11 107) | ||
| Age, y | 43.9±0.3 | 45.8±0.2 | 0.965 |
| BMI, kg/m2 | 24.0±0.0 | 23.2±0.0 | <0.001 |
| Waist circumference, cm | 84.3±0.3 | 78.0±0.2 | <0.001 |
| SBP, mm Hg | 117.9±0.2 | 113.8±0.3 | <0.001 |
| DBP, mm Hg | 77.6±0.2 | 72.7±0.2 | <0.001 |
| Age groups (years), N (%) | |||
| 20 to 29 | 1029 (12) | 1382 (12) | <0.406 |
| 30 to 39 | 1675 (20) | 2289 (21) | |
| 40 to 49 | 1724 (20) | 2186 (20) | |
| 50 to 59 | 1481 (18) | 1988 (18) | |
| 60 to 69 | 1399 (17) | 1784 (16) | |
| 70+ | 1074 (13) | 1478 (13) | |
| BMI groups, N (%) | |||
| Normal (<23 kg/m2) | 3208 (39) | 5430 (49) | <0.001 |
| Overweight (23 to 25 kg/m2) | 2182 (26) | 2430 (22) | |
| Obese (≥25 kg/m2) | 2969 (35) | 3201 (29) | |
| Hypertension, N (%) | 2582 (31) | 2913 (26) | <0.001 |
| Diabetes, N (%) | 959 (11) | 1000 (9) | <0.001 |
| Cardiovascular disease, N (%) | 212 (3) | 196 (2) | <0.001 |
| Cerebrovascular disease, N (%) | 194 (2) | 184 (2) | <0.001 |
| Smoking | |||
| Current | 3567 (31) | 637 (6) | <0.001 |
| Past | 2247 (27) | 478 (4) | |
| Never | 2568 (42) | 9992 (90) | |
| Family income | |||
| Low | 1532 (19) | 2350 (21) | <0.001 |
| Low middle | 2049 (25) | 2736 (25) | |
| High middle | 2327 (28) | 2911 (27) | |
| High | 2351 (28) | 2908 (27) | |
| Region | |||
| Metropolitan | 3644 (44) | 4919 (44) | 0.518 |
| City | 2860 (34) | 3746 (34) | |
| Rural | 1878 (22) | 2442 (22) | |
Data for continuous variables were expressed as mean±SE. BMI indicates body mass index; DBP, diastolic blood pressure; KNHANES, Korea National Health and Nutrition Examination Surveys; SBP, systolic blood pressure.
Age‐standardized Mean Serum Levels of Total Cholesterol and LDL‐Cholesterol by Age and Gender
The age‐standardized mean serum concentrations of TC, HDL‐C, LDL‐C, and TG were 186.8, 48.0, 112.9, and 136.0 mg/dL, respectively, in Korean adults aged ≥20 years (Table 3). Mean TC level was similar between men and women ≥20 years of age; however, it was significantly different across age groups (Figure 2). Mean serum TC level tended to increase with age up to ≈50 years, after which it declined gradually in men. In contrast, TC level was markedly elevated for women 45 to 55 years old, and they also maintained higher levels compared with those in men >55 years of age (Figure 2A). This indicates that lipid metabolism may be affected by changes in sex hormones such as estrogen in postmenopausal women.(1999) Trends in LDL‐C (Figure 2B) level by age and gender was similar with the patterns observed for TC. In men, LDL‐C level increased until the 40s, after which it declined gradually. In women, LDL‐C level increased until the 50s, showing abrupt elevation between 40s and 50s. This LDL‐C elevation between 40s and 50s in women made the higher LDL‐C level in women compared with men after 50s, while men showed higher LDL‐C level than women until 40s. The mean TG level in men increased until 40s, after that it declined gradually. In contrast, the mean TG level in women increased continuously and showed a higher level than men after 70s. The HDL‐C level showed decreasing tendency with increasing age both in men and women, however the differences among age groups were smaller than other lipid parameters (Table 3). These age‐ and gender‐related differences in serum cholesterol levels could be partly explained by the prevalence of obesity in Korea (Figure 3). Trends in mean TC and LDL levels between men and women were comparable to the changes in BMI, waist circumference, and proportion of subjects with obesity and overweight by ages and gender. In addition, younger men tended to have higher consumption of cigarettes and alcohol but less exercise (data not shown), which might contribute to the increase in cholesterol levels in men aged between 30s and 40s.
Table 3.
Age‐specific and Age‐standardized Mean Values of Serum Lipids in Korea, 2008–2010
| N* | KNHANES 2008–2010 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| TC (mg/dL) | HDL‐C (mg/dL) | LDL‐C (mg/dL) | TG (mg/dL) | ||||||
| Mean | SE | Mean | SE | Mean | SE | Mean | SE | ||
| Aged 20 years and older | 0.496 | <0.0001 | <0.0001 | <0.0001 | |||||
| Total | 32 431 033 | 186.8 | 0.7 | 48.0 | 0.2 | 112.9 | 0.6 | 136.0 | 2.4 |
| Men | 14 776 153 | 186.2 | 1.1 | 45.5 | 0.3 | 111.2 | 1.0 | 159.0 | 4.0 |
| Women | 17 654 880 | 187.3 | 0.9 | 50.5 | 0.3 | 114.6 | 0.8 | 113.1 | 2.1 |
| Aged 30 years and older | 0.559 | <0.001 | <0.001 | <0.001 | |||||
| Total | 27 529 026 | 190.4 | 0.7 | 47.4 | 0.2 | 115.9 | 0.6 | 143.2 | 2.4 |
| Men | 12 444 281 | 189.8 | 1.0 | 45.0 | 0.3 | 113.9 | 0.9 | 168.2 | 4.1 |
| Women | 15 084 745 | 190.9 | 0.9 | 49.8 | 0.3 | 117.8 | 0.8 | 119.0 | 2.1 |
| Total | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| 20 to 29 years | 4 902 007 | 170.3 | 2.2 | 50.9 | 0.8 | 99.2 | 2.0 | 103.1 | 6.1 |
| 30 to 39 years | 6 673 138 | 183.1 | 1.9 | 48.5 | 0.6 | 110.4 | 1.7 | 128.7 | 6.2 |
| 40 to 49 years | 6 860 955 | 190.8 | 2.0 | 48.0 | 0.6 | 115.4 | 1.8 | 146.9 | 8.2 |
| 50 to 59 years | 5 740 767 | 196.3 | 2.3 | 47.4 | 0.7 | 120.0 | 2.2 | 154.0 | 7.9 |
| 60 to 69 years | 4 628 894 | 191.6 | 2.4 | 46.2 | 0.7 | 117.4 | 2.2 | 146.5 | 6.3 |
| 70+ years | 3 625 271 | 193.0 | 2.7 | 45.1 | 0.7 | 120.0 | 2.3 | 142.3 | 5.7 |
| Men | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| 20 to 29 years | 2 331 871 | 170.8 | 3.3 | 47.7 | 1.0 | 99.6 | 3.0 | 121.0 | 10.2 |
| 30 to 39 years | 3 087 356 | 189.3 | 2.8 | 45.1 | 0.8 | 114.6 | 2.6 | 161.4 | 10.5 |
| 40 to 49 years | 3 181 667 | 196.0 | 3.0 | 45.5 | 0.9 | 117.2 | 2.8 | 184.6 | 14.2 |
| 50 to 59 years | 2 622 319 | 190.2 | 3.3 | 44.8 | 0.9 | 112.9 | 3.3 | 178.5 | 13.2 |
| 60 to 69 years | 2 052 452 | 183.4 | 3.5 | 44.9 | 1.1 | 109.7 | 3.3 | 152.3 | 10.5 |
| 70+ years | 1 500 487 | 181.0 | 2.8 | 44.5 | 0.8 | 109.8 | 2.6 | 133.7 | 6.6 |
| Women | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| 20 to 29 years | 2 570 135 | 169.5 | 2.8 | 50.9 | 0.8 | 99.2 | 2.0 | 83.8 | 5.6 |
| 30 to 39 years | 3 585 782 | 176.5 | 2.4 | 52.2 | 0.8 | 106.0 | 2.1 | 93.6 | 5.1 |
| 40 to 49 years | 3 679 289 | 185.3 | 2.5 | 50.7 | 0.8 | 113.6 | 2.2 | 107.4 | 5.7 |
| 50 to 59 years | 3 118 448 | 202.6 | 3.1 | 50.1 | 0.9 | 127.0 | 2.7 | 129.3 | 7.1 |
| 60 to 69 years | 2 576 442 | 199.0 | 3.1 | 47.3 | 0.9 | 124.1 | 2.8 | 141.2 | 7.1 |
| 70+ years | 2 124 784 | 201.0 | 2.9 | 45.6 | 0.8 | 126.8 | 2.6 | 148.4 | 6.1 |
| BMI | |||||||||
| Men | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Normal (<23 kg/m2) | 5 632 240 | 167.6 | 2.2 | 52.8 | 0.9 | 97.6 | 2.1 | 88.6 | 3.6 |
| Overweight (23 to 25 kg/m2) | 3 798 065 | 182.0 | 0.6 | 46.9 | 0.2 | 108.5 | 0.5 | 141.9 | 2.1 |
| Obese (≥25 kg/m2) | 5 268 321 | 194.9 | 0.8 | 42.7 | 0.2 | 116.8 | 0.8 | 193.4 | 3.4 |
| Women | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Normal (<23 kg/m2) | 8 773 860 | 171.2 | 1.3 | 55.9 | 0.5 | 100.5 | 1.1 | 75.4 | 1.9 |
| Overweight (23 to 25 kg/m2) | 3 852 600 | 183.6 | 0.5 | 51.6 | 0.2 | 111.9 | 0.4 | 102.0 | 1.0 |
| Obese (≥25 kg/m2) | 4 954 241 | 196.6 | 0.8 | 46.9 | 0.2 | 122.1 | 0.7 | 142.3 | 2.1 |
| Hypertension status | |||||||||
| Men | <0.001 | <0.001 | 0.001 | <0.001 | |||||
| Normal | 6 701 147 | 183.4 | 0.7 | 45.7 | 0.2 | 111.0 | 0.6 | 140.2 | 2.5 |
| Prehypertension | 3 819 198 | 191.5 | 0.9 | 45.9 | 0.3 | 114.1 | 0.9 | 171.4 | 3.7 |
| Hypertension | 4 255 807 | 190.1 | 0.9 | 44.5 | 0.3 | 111.1 | 0.8 | 191.2 | 3.9 |
| Women | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Normal | 10 454 237 | 181.1 | 0.5 | 51.9 | 0.2 | 110.2 | 0.5 | 96.2 | 1.1 |
| Prehypertension | 2 812 447 | 196.6 | 1.0 | 49.6 | 0.3 | 121.8 | 0.9 | 127.3 | 2.5 |
| Hypertension | 4 388 196 | 199.0 | 0.9 | 47.4 | 0.3 | 122.7 | 0.8 | 149.5 | 2.1 |
| Diabetes status | |||||||||
| Men | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Normal | 9 913 431 | 185.0 | 0.6 | 46.0 | 0.2 | 111.6 | 0.5 | 143.9 | 2.0 |
| Impaired fasting glucose | 3 283 344 | 195.5 | 1.1 | 44.8 | 0.3 | 115.3 | 1.0 | 195.4 | 4.5 |
| Diabetes | 1 579 377 | 185.6 | 1.6 | 42.4 | 0.4 | 107.4 | 1.4 | 198.0 | 6.3 |
| Women | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Normal | 13 357 760 | 184.7 | 0.5 | 51.4 | 0.2 | 113.0 | 0.4 | 102.4 | 1.0 |
| Impaired fasting glucose | 2 709 976 | 198.7 | 1.1 | 48.6 | 0.3 | 123.4 | 1.0 | 136.5 | 3.0 |
| Diabetes | 1 587 144 | 198.1 | 1.6 | 45.5 | 0.4 | 120.2 | 1.4 | 169.2 | 4.5 |
| Family income | |||||||||
| Men | <0.001 | 0.892 | <0.001 | 0.518 | |||||
| Low | 2 518 044 | 181.9 | 1.3 | 45.5 | 0.4 | 107.1 | 1.2 | 153.9 | 4.6 |
| Low middle | 3 677 051 | 185.8 | 0.9 | 45.6 | 0.3 | 110.8 | 0.9 | 158.1 | 3.2 |
| High middle | 4 197 725 | 186.4 | 0.9 | 45.4 | 0.3 | 111.4 | 0.8 | 159.8 | 3.5 |
| High | 4 141 301 | 188.4 | 0.8 | 45.6 | 0.2 | 112.8 | 0.7 | 161.0 | 3.8 |
| Women | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Low | 3 548 542 | 193.6 | 1.0 | 48.1 | 0.3 | 119.1 | 0.8 | 136.4 | 2.7 |
| Low middle | 4 535 130 | 186.7 | 0.8 | 50.4 | 0.3 | 114.3 | 0.7 | 112.5 | 1.9 |
| High middle | 4 605 368 | 183.7 | 0.8 | 51.2 | 0.2 | 111.4 | 0.7 | 107.1 | 1.6 |
| High | 4 624 677 | 183.9 | 0.9 | 52.2 | 0.3 | 112.3 | 0.7 | 98.6 | 1.5 |
| Region | |||||||||
| Men | 0.881 | 0.265 | 0.855 | 0.610 | |||||
| Metropolitan | 6 984 504 | 186.0 | 0.8 | 45.5 | 0.2 | 111.3 | 0.6 | 157.5 | 2.7 |
| City | 4 784 729 | 186.5 | 0.9 | 45.4 | 0.2 | 111.0 | 0.8 | 160.7 | 3.2 |
| Rural | 3 006 919 | 186.4 | 1.0 | 45.9 | 0.4 | 110.9 | 1.0 | 159.8 | 4.3 |
| Women | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Metropolitan | 8 533 767 | 185.9 | 0.7 | 51.3 | 0.2 | 113.1 | 0.6 | 109.2 | 1.5 |
| City | 5 676 734 | 185.3 | 0.7 | 51.0 | 0.2 | 113.2 | 0.6 | 108.5 | 1.7 |
| Rural | 3 444 379 | 191.0 | 1.0 | 48.8 | 0.3 | 117.7 | 0.9 | 124.2 | 2.2 |
BMI indicates body mass index; HDL‐C, high‐density lipoprotein cholesterol; LDL‐C, low‐density lipoprotein cholesterol; SE, standard error; TC, total cholesterol; TG, triglycerides.
Weighted numbers of subjects.
Figure 2.
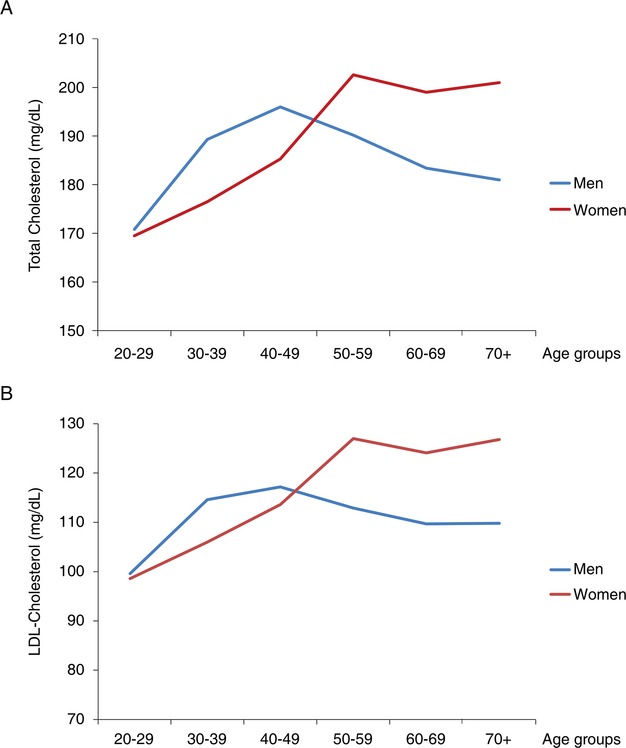
Trends in age‐standardized mean serum lipid levels in Korean subjects. A, Serum levels of total cholesterol. B, Serum levels of LDL‐cholesterol. Blue line (men); red line (women). LDL indicates low‐density lipoprotein.
Figure 3.
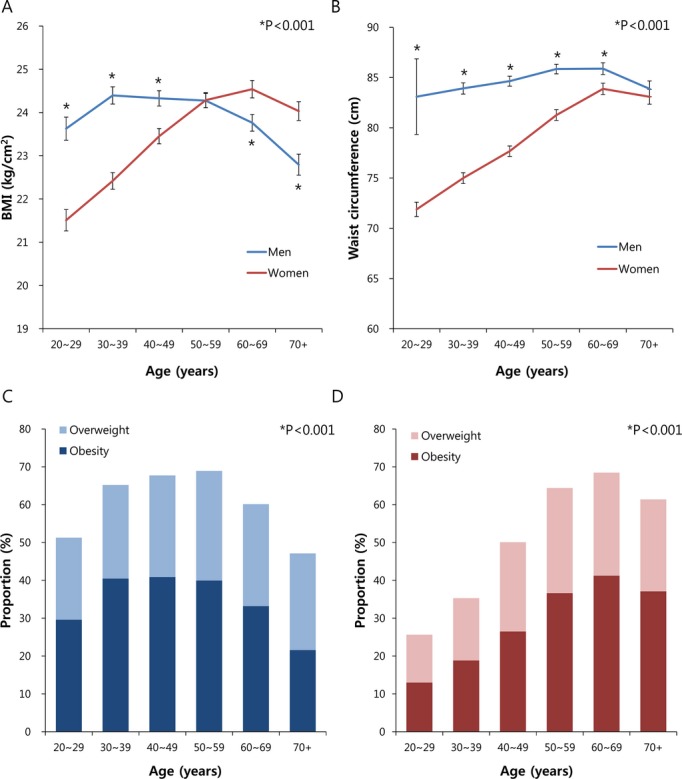
Trends in obesity related parameters and prevalence of obesity in Korean subjects. A, Age‐standardized mean body mass index (BMI) in men and women. Blue line (men); red line (women). *P<0.001 for comparisons between men and women at each age group. Error bars indicate 95% confidence intervals. B, Age‐standardized mean waist circumference in men and women. Blue line (men); red line (women). *P<0.001 for comparisons between men and women at each age group. Error bars indicate 95% confidence intervals. C, Prevalence of obesity and overweight subjects in Korean men. Light blue bars (overweight, 23 kg/m2≤BMI<25 kg/m2); dark blue bars (obesity, BMI ≥25 kg/m2). *P<0.001 for comparisons among age groups. D, Prevalence of obesity and overweight subjects in Korean women. Light red bars (overweight, 23 kg/m2≤BMI<25 kg/m2); dark red bars (obesity, BMI ≥25 kg/m2). *P<0.001 for comparisons among age groups.
Age‐standardized mean levels of TC, LDL‐C, and TG were significantly higher in women living in rural Korea compared to those in urban areas, whereas no significant difference was observed in men based on residence (Table 3). In terms of economic status, men with higher incomes tended to have higher TC and LDL‐C levels, and women with higher incomes had significantly lower levels of TC, LDL‐C, and TG. Unexpectedly, subjects with impaired fasting glucose showed higher levels of TC and LDL‐C than diabetic or normal subjects, regardless of gender. Furthermore, TC, LDL‐C, and TG levels were significantly increased in both prehypertensive and hypertensive subjects compared with the normotensive population.
Prevalence and Awareness of Hyper‐LDL‐Cholesterolemia
The overall age‐standardized prevalence of hyper‐LDL‐cholesterolemia, determined by individual risk based on the ATP III guideline was 23.2% (Figure 4A). Particularly, young and middle‐aged adults (<50 years) showed significantly lower prevalence of hyper‐LDL‐cholesterolemia (3.5% to 18.9%) compared with older individuals (35.6% to 48.2%). The prevalence of subjects with high LDL‐C increased with age until the 50s and reached a plateau in men, while it gradually increased over the entire age range in women (Figure 5A).
Figure 4.
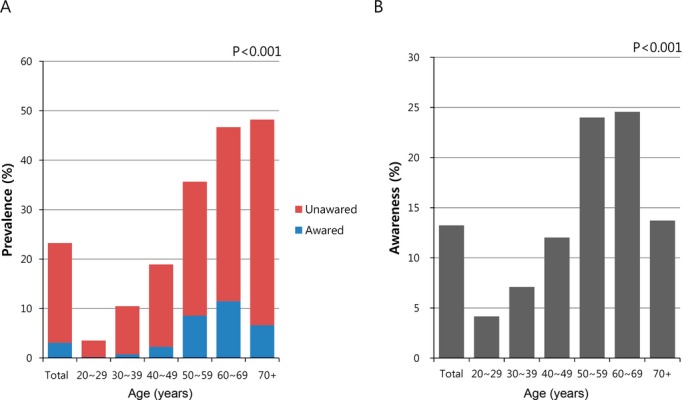
Prevalence and awareness of high LDL‐cholesterol among adults in the KHNANES 2008–2010 stratified by age. A, Prevalence of hyper‐LDL‐cholesterolemia. Blue bars (subjects aware of their high LDL‐C); red bars (subjects unaware of their high LDL‐C). B, Awareness of hyper‐LDL‐cholesterolemia. KHNANES indicates Korea National Health and Nutrition Examination Survey; LDL, low‐density lipoprotein.
Figure 5.
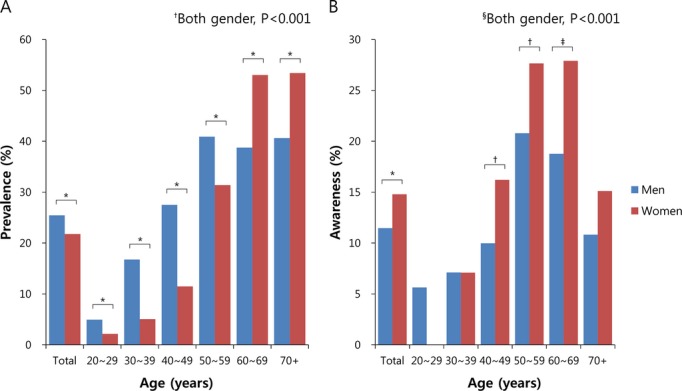
Prevalence and awareness of high LDL‐cholesterol among adults from the KHNANES dataset stratified by gender and age. Blue bars (men); red bars (women). A, Prevalence of hyper‐LDL‐cholesterolemia. *P<0.001 for comparisons between men and women at each age group. †P<0.001 for comparisons among different age groups in the same gender. B, Awareness of hyper‐LDL‐cholesterolemia. *P<0.001, †P<0.05, and ‡P<0.01 for comparisons between men and women at a certain age group. §P<0.001 for comparisons among different age groups in the same gender. KHNANES indicates Korea National Health and Nutrition Examination Survey; LDL, low‐density lipoprotein.
Among all subjects with a high LDL‐C or those who reported using cholesterol‐lowering medications, the overall proportion of those who were aware of their hyper‐LDL‐cholesterolemia was 13.2% (Figure 4B). The awareness of high LDL‐C was significantly low in young and middle‐aged population (aged <50 years, 4.2% to 12%), compared with individuals aged between 50 and 69 years (24.0% to 24.6%). It gradually increased with age until 60s (from 4.2% to 24.6%), whereas significantly decreased in the elderly aged ≥70 years. In terms of gender, women were more aware of their condition than men (Figure 5B, 14.8% versus 11.5%). The difference of awareness between genders was especially prominent in ages >40 years.
Treatment and Control of Hyper‐LDL‐Cholesterolemia
Figure 6 describes the treatment and control of hyper‐LDL‐cholesterolemia stratified by age. The overall treatment rate among subjects with high LDL‐C was estimated to be 10.2% (Figure 6A). The distribution of treatment rates across age showed a similar pattern with that of awareness rates; young and middle‐aged adults (aged 20 to 49 years) had significantly lower treatment rates, whereas older subjects (≥50 years) showed higher rates of treatment (2.4% to 8.5% versus 12.8% to 22.0%, P<0.001). The treatment rate for the subjects who were already aware of their condition was much higher (52.3%, Figure 6B). Similarly, among individuals aware of high LDL‐C, young and middle‐aged adults were less likely to be treated for high cholesterol than elderly subjects (19.3% to 48.9% versus 72.9% to 92.0%, P<0.001). Of all ages, the treatment rate showed a modest increase in women compared with men except for the ages between 40 and 49 (Figure 7A and 7B).
Figure 6.
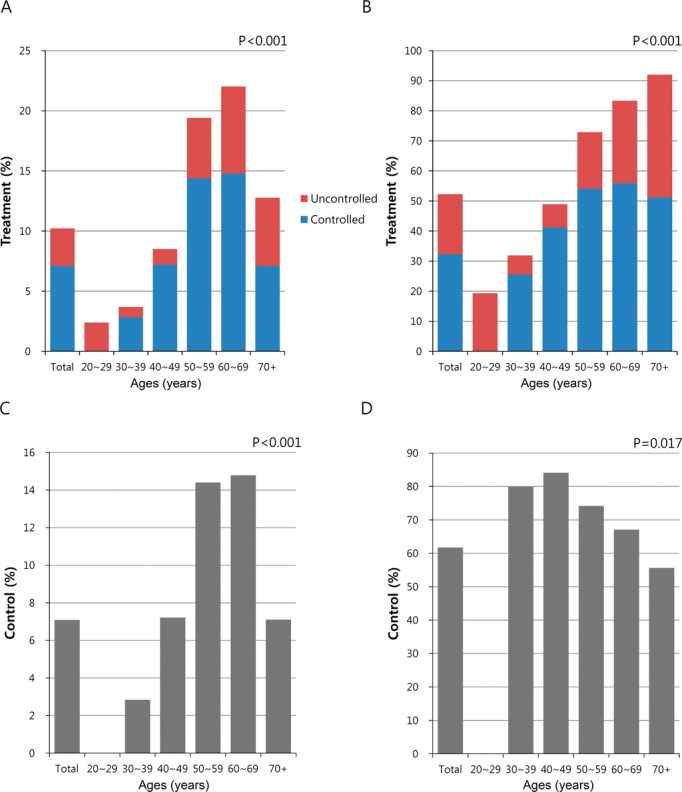
Treatment and control rates of high LDL‐cholesterol among adults in the KHNANES 2008–2010 stratified by age. A, Treatment rates among all individuals with high LDL‐C. B, Treatment rates among individuals aware of their high LDL‐C. Blue bars (controlled subjects according to their individual LDL‐C goals); red bars (uncontrolled subjects according to their individual LDL‐C goals). C, Control rates among all individuals with high LDL‐C. D, Control rates among individuals treated for their high LDL‐C. KHNANES indicates Korea National Health and Nutrition Examination Survey; LDL, low‐density lipoprotein.
Figure 7.
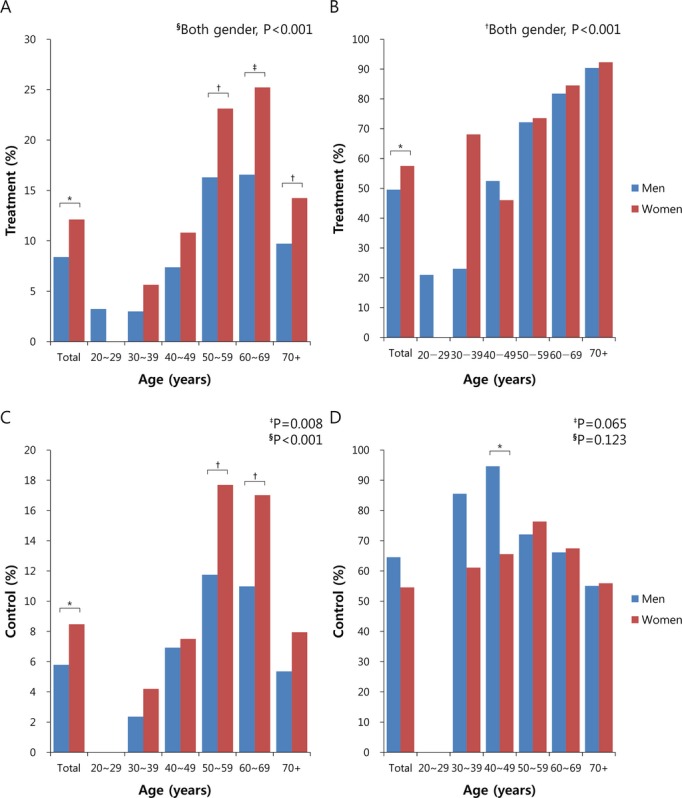
Treatment and control rates of high LDL‐C among adults in the KHNANES 2008–2010 stratified by gender and age. Blue bars (men); red bars (women). A, Treatment rates among all individuals with high LDL‐C. *P<0.001, †P<0.05, and ‡P<0.01 for comparisons between men and women at a certain age group. §P<0.001 for comparisons among different age groups in the same gender. B, Treatment rates among individuals aware of their high LDL‐C. *P<0.001 for comparison between men and women. †P<0.001 for comparisons among different age groups in the same gender. C, Control rates among all individuals with high LDL‐C. *P<0.001 and †P<0.05 for comparisons between men and women at a certain age group. P‐values for comparisons among different age groups in ‡men and in §women. D, Control rates among individuals treated for their high LDL‐C. *P<0.01 for comparison between men and women at a certain age group. P‐values for comparisons among different age groups in ‡men and in §women. KHNANES indicates Korea National Health and Nutrition Examination Survey; LDL‐C, low‐density lipoprotein cholesterol.
Among participants who reported using cholesterol‐lowering medications, the proportion of subjects who achieved LDL‐C levels below their individual LDL‐C goals was 61.7% (Figure 6D). Contrary to the findings above, young or middle‐aged adults (<50 years) had significantly higher LDL‐C control rates compared with the older population aged ≥50 years (80% to 84.1% versus 55.6% to 74.2%, P<0.001). Particularly, younger men aged <50 years were more likely to have their LDL‐C at goal when compared with women (Figure 7D). The overall average control rate was 7.1% among all subjects defined as high LDL‐C (Figure 6C).
Discussion
Under the increasing prevalence of CVD‐related risk factors such as high TC or LDL‐C, hypertension and obesity, 1 of every 3 deaths in the United States is attributable to CVD, and strikingly, about 20% of CVD deaths occur before the age of 65 years. Similarly, mortality rates from ischemic heart disease in Korea have increased >3 times during 15 years.(2001) After statins were first introduced as a lipid‐lowering drug in the 1980s, the Cholesterol Treatment Trialists' Collaborators reported an ≈20% relative risk reduction with statins for major vascular events per 38.6 mg/dL (1 mmol/L) decrease in LDL‐C,(2012) demonstrating the preponderance of evidence of the benefit of statins on CVD. Although there have been significant advances in the research of the epidemiology of and preventive medicine for CVD, the burden of public disease still remains high and may be increasing in the future(2005) as the rate of obesity increases, populations age, and physical activity levels decrease. In the era of statins and the obesity epidemic, we investigated the prevalence, awareness, treatment, and control of adults with high cholesterol based on age using a national public health survey dataset in Korea.
To date, not many studies have investigated the prevalence, awareness, treatment, and control rates of high blood cholesterol level in the general population of Asia.(2004) Our study population is representative of the general Korean population as a whole because the KNHANES is an official, nationwide database that reflects the geographic and demographic differences found in Korea. In general, for Korean adults ≥20 years of age, the age‐standardized mean values of TC, HDL‐C, LDL‐C, and TG were 186.8, 48.0, 112.9, and 136.0 mg/dL, respectively. Compared with previous data from the KNHANES 2005,(2012) the mean levels of TC, HDL‐C, and TG slightly increased (from 183.2, 45.0, and 133.7 mg/dL in KNHANES 2005), while LDL‐C was nearly unchanged (113.1 mg/dL). This deteriorating trend toward dyslipidemia may be due to an increase in the prevalence of metabolic syndrome in Korea.(2011) Mean levels of LDL‐C and TG in Korean adults were higher when compared with a national dataset of Chinese adults from 2001, whereas HDL‐C was lower (TC, HDL‐C, LDL‐C, TG; 186, 51.7, 109.5, 128.1 mg/dL, respectively).(2004) Although mean TC, HDL‐C, and LDL‐C values were significantly lower than those found in United States adults from the NHANES 2010 (TC, HDL‐C, LDL‐C; 196, 52.5, 116 mg/dL, respectively),(2012) the serum TG level was markedly increased in Korean adults (136 versus 110 mg/dL), indicating the possible impact of genetic or ethnic effects on lipid metabolism.
Despite the small number of studies regarding the prevalence of hypercholesterolemia in the general populations of Asian countries, the prevalence of hyper‐LDL‐cholesterolemia in Korea was quite similar to that of China, 23.2% in our survey and 24.8% (LDL‐C ≥130 mg/dL) in China.(2004) However, the Chinese study did not assess LDL‐C levels by individual risk status, which may overestimate the prevalence of hyper‐LDL‐cholesterolemia. In the United States,(2010) the prevalence of LDL‐C ≥130 mg/dL is 35%, which is significantly higher than in Asian countries.
Our study has several distinguishable features. First, in younger adults (<50 years), men had significantly higher levels of TC and LDL‐C, while women showed markedly elevated values of TC and LDL‐C compared with men when they became older than 50 years. These findings are likely to be associated with the age and gender difference in obesity prevalence in Korea, suggesting that intensive modification in lifestyles to control body weight should be necessary especially for younger men (<50 years) and older women (≥50 years). Second, pharmacotherapy for high LDL‐C was more effective in the young and middle‐aged population (30 to 49 years, 82.1%) than in elderly subjects (≥60 years, 61.6%) with average control rates of 61.7%. This figure is lower than that of 69% from the NHANES 2005–2008 conducted in adults ≥20 years old,(2011) 75% to 77% from the Multi‐Ethnic Study of Atherosclerosis in 2000–2002,(2006) and 81% from a national Chinese study with adults 35 to 74 years of age in 2000–2001,(2004) whereas is higher than that of 56.1% from the Health Survey for England in 2003.(2006) Hypercholesterolemia control rates vary depending on the population and country, with rates ranging from 18% to 100%.(2005) Third, the overall treatment rate for subjects with high LDL‐C was 10.2% in Korea. This rate is markedly lower when we compare the treatment rate from a United States population that reported a rate of 48%(2011) as well as rates of other chronic diseases in Korea; the treatment rates for hypertension(2008) and diabetes(2009) were 66% and 49%, respectively. However, the treatment rate for subjects who were aware of their high LDL‐C was noticeably increased to 52.3%. Considering the impact of hypercholesterolemia on the development of CVD, vigorous efforts are necessary within the public health field to provide proper education and counsel about the screening and management of hypercholesterolemia to laypersons. Lastly, awareness and treatment rates of high LDL‐C were significantly lower in younger adults <50 years old (awareness, 8.0%; treatment, 5.1%) compared with those who were ≥50 years old (21.5%; 18.5%), although the prevalence of high LDL‐C was not high in young or middle‐aged adults. This suggests that there is a large proportion of undiagnosed subjects who are at high risk for CVD among young or middle‐aged individuals. Based on our findings, we can assume that, out of 100 subjects with hyper‐LDL‐cholesterolemia aged <50 years, 8 are aware of their condition, 5 are being treated with cholesterol‐lowering agents, and 3 subjects have their LDL‐C levels under control, implying that 97% of young and middle‐aged individuals will remain as potentially high‐risk subjects for CVD.(2012) Consistent with our results, the study from the NHANES 2005–2008 reported that the treatment rate for high LDL‐C was 11% in adults aged 20 to 39 years but 48% and 64% in adults aged 40 to 64 years or ≥65 years, respectively.(2011)
Recent data demonstrates that trends in mortality rates from CVD among young adults have declined less rapidly than the rates in the older population over the past 20 years,(2007) raising concerns about young adults with a high risk for CVD death. This unfavorable finding is a result of an increasing prevalence of obesity‐related conditions such as metabolic syndrome,(2004) hypertension,(2003) and hypercholesterolemia(2005) in the young and middle‐aged population. Although NCEP ATP III guidelines define men who are ≥45 years old and women who are at least ≥55 years old as high risk for CVD,(2004) our data clearly suggest that more attention should be paid to younger subjects who may be undiagnosed for hypercholesterolemia in order to alleviate the increasing trend of CVD among young adults.
The present study has some potential limitations that should be addressed in future investigations. First, as these findings were derived from a cross‐sectional study, it is difficult to conclude that lower rates of awareness and treatment in young and middle‐aged adults can directly lead to an increase in the incidence of future CVD events. Subsequent prospective studies are needed to validate this hypothesis and support our findings. Second, we could not perform additional analyses to identify putative reasons for why the younger age groups had a lower awareness of their cholesterol condition due to the lack of related information in the dataset.
The present results demonstrate that significant proportions of young and middle‐aged adults are unaware of their hyper‐LDL‐cholesterolemia and are not treated with proper lipid‐lowering medications. Considering the impact of CVD on an individual's quality of life and the public health burden of the disease, intensive efforts in national public healthcare policy regarding early screening and education is indispensable to decrease potentially high‐risk individuals for CVD. Further research is warranted to confirm the impact of low awareness and treatment rates in young adults on development of CVD and to establish effective screening tools for identifying individuals with hyper‐LDL‐cholesterolemia.
Sources of Funding
This work was supported by the Korea Science and Engineering Foundation (KOSEF) grant funded by the Korea government (MEST) (No. 2010‐0028367).
Disclosures
None.
References
- Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio‐metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011; 32:590-597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQueen MJ, Hawken S, Wang X, Ounpuu S, Sniderman A, Probstfield J, Steyn K, Sanderson JE, Hasani M, Volkova E, Kazmi K, Yusuf S. Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): a case‐control study. Lancet. 2008; 372:224-233 [DOI] [PubMed] [Google Scholar]
- Farzadfar F, Finucane MM, Danaei G, Pelizzari PM, Cowan MJ, Paciorek CJ, Singh GM, Lin JK, Stevens GA, Riley LM, Ezzati M. National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country‐years and 3.0 million participants. Lancet. 2011; 377:578-586 [DOI] [PubMed] [Google Scholar]
- Kuklina EV, Yoon PW, Keenan NL. Trends in high levels of low‐density lipoprotein cholesterol in the United States, 1999–2006. JAMA. 2009; 302:2104-2110 [DOI] [PubMed] [Google Scholar]
- Carroll MD, Lacher DA, Sorlie PD, Cleeman JI, Gordon DJ, Wolz M, Grundy SM, Johnson CL. Trends in serum lipids and lipoproteins of adults, 1960–2002. JAMA. 2005; 294:1773-1781 [DOI] [PubMed] [Google Scholar]
- Downs JR, Clearfield M, Weis S, Whitney E, Shapiro DR, Beere PA, Langendorfer A, Stein EA, Kruyer W, Gotto AM., Jr Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998; 279:1615-1622 [DOI] [PubMed] [Google Scholar]
- Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW, McKillop JH, Packard CJ. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995; 333:1301-1307 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Vital signs: prevalence, treatment, and control of high levels of low‐density lipoprotein cholesterol—United States, 1999–2002 and 2005–2008. MMWR Morb Mortal Wkly Rep. 2011; 60:109-114 [PubMed] [Google Scholar]
- Ford ES, Mokdad AH, Giles WH, Mensah GA. Serum total cholesterol concentrations and awareness, treatment, and control of hypercholesterolemia among US adults: findings from the National Health and Nutrition Examination Survey, 1999 to 2000. Circulation. 2003; 107:2185-2189 [DOI] [PubMed] [Google Scholar]
- Tolonen H, Keil U, Ferrario M, Evans A. Prevalence, awareness and treatment of hypercholesterolaemia in 32 populations: results from the WHO MONICA Project. Int J Epidemiol. 2005; 34:181-192 [DOI] [PubMed] [Google Scholar]
- Steinberg D, Grundy SM. The case for treating hypercholesterolemia at an earlier age: moving toward consensus. J Am Coll Cardiol. 2012; 60:2640-2642 [DOI] [PubMed] [Google Scholar]
- Ford ES, Capewell S. Coronary heart disease mortality among young adults in the U.S. from 1980 through 2002: concealed leveling of mortality rates. J Am Coll Cardiol. 2007; 50:2128-2132 [DOI] [PubMed] [Google Scholar]
- He J, Gu D, Reynolds K, Wu X, Muntner P, Zhao J, Chen J, Liu D, Mo J, Whelton PK. Serum total and lipoprotein cholesterol levels and awareness, treatment, and control of hypercholesterolemia in China. Circulation. 2004; 110:405-411 [DOI] [PubMed] [Google Scholar]
- Grundy SM, Cleeman JI, Merz CN, Brewer HB, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Stone NJ. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004; 110:227-239 [DOI] [PubMed] [Google Scholar]
- Korea Centers for Disease Control and Prevention, Ministry of Health and Welfare, South Korea Korea National Health and Nutrition Examination Survey (KNHANES). Available at: http://knhanes.cdc.go.kr/ Accessed November 11, 2013
- Lee YH, Bang H, Kim HC, Kim HM, Park SW, Kim DJ. A simple screening score for diabetes for the Korean population: development, validation, and comparison with other scores. Diabetes Care. 2012; 35:1723-1730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SG, Lee YH, Kim KJ, Lee W, Kwon OH, Kim JH. Additive association of vitamin D insufficiency and sarcopenia with low femoral bone mineral density in noninstitutionalized elderly population: the Korea National Health and Nutrition Examination Surveys 2009–2010. Osteoporos Int. 2013; 24:2789-2799 [DOI] [PubMed] [Google Scholar]
- Oh SW. Obesity and metabolic syndrome in Korea. Diabetes Metab J. 2011; 35:561-566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010; 33suppl 1:S62-S69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003; 289:2560-2572 [DOI] [PubMed] [Google Scholar]
- Lee MH, Kim HC, Ahn SV, Hur NW, Choi DP, Park CG, Suh I. Prevalence of dyslipidemia among Korean adults: Korea National Health and Nutrition Survey 1998–2005. Diabetes Metab J. 2012; 36:43-55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Aloysio D, Gambacciani M, Meschia M, Pansini F, Bacchi Modena A, Bolis PF, Massobrio M, Maiocchi G, Peruzzi E. The effect of menopause on blood lipid and lipoprotein levels. The Icarus Study Group. Atherosclerosis. 1999; 147:147-153 [DOI] [PubMed] [Google Scholar]
- Suh I. Cardiovascular mortality in Korea: a country experiencing epidemiologic transition. Acta Cardiol. 2001; 56:75-81 [DOI] [PubMed] [Google Scholar]
- Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, Voysey M, Gray A, Collins R, Baigent C. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta‐analysis of individual data from 27 randomised trials. Lancet. 2012; 380:581-590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, Hayflick L, Butler RN, Allison DB, Ludwig DS. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005; 352:1138-1145 [DOI] [PubMed] [Google Scholar]
- Lim S, Shin H, Song JH, Kwak SH, Kang SM, Won Yoon J, Choi SH, Cho SI, Park KS, Lee HK, Jang HC, Koh KK. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998–2007. Diabetes Care. 2011; 34:1323-1328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll MD, Kit BK, Lacher DA, Shero ST, Mussolino ME. Trends in lipids and lipoproteins in US adults, 1988–2010. JAMA. 2012; 308:1545-1554 [DOI] [PubMed] [Google Scholar]
- Cohen JD, Cziraky MJ, Cai Q, Wallace A, Wasser T, Crouse JR, Jacobson TA. 30‐year trends in serum lipids among United States adults: results from the National Health and Nutrition Examination Surveys II, III, and 1999–2006. Am J Cardiol. 2010; 106:969-975 [DOI] [PubMed] [Google Scholar]
- Goff DC, Jr, Bertoni AG, Kramer H, Bonds D, Blumenthal RS, Tsai MY, Psaty BM. Dyslipidemia prevalence, treatment, and control in the Multi‐Ethnic Study of Atherosclerosis (MESA): gender, ethnicity, and coronary artery calcium. Circulation. 2006; 113:647-656 [DOI] [PubMed] [Google Scholar]
- Primatesta P, Poulter NR. Levels of dyslipidaemia and improvement in its management in England: results from the Health Survey for England 2003. Clin Endocrinol (Oxf). 2006; 64:292-298 [DOI] [PubMed] [Google Scholar]
- Kim KI, Chang HJ, Cho YS, Youn TJ, Chung WY, Chae IH, Choi DJ, Kim CH. Current status and characteristics of hypertension control in community resident elderly Korean people: data from a Korean longitudinal study on health and aging (KLoSHa study). Hypertens Res. 2008; 31:97-105 [DOI] [PubMed] [Google Scholar]
- Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998–2005. Diabetes Care. 2009; 32:2016-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford ES, Giles WH, Mokdad AH. Increasing prevalence of the metabolic syndrome among U.S. adults. Diabetes Care. 2004; 27:2444-2449 [DOI] [PubMed] [Google Scholar]
- Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003; 290:199-206 [DOI] [PubMed] [Google Scholar]


