Summary
Objectives
To develop a standardized verbal autopsy (VA) training program and evaluate whether its implementation resulted in comparable knowledge required to classify perinatal cause of death (COD) by physicians and non-physicians.
Methods
Training materials, case studies, and written and mock scenarios for this VA program were developed using conventional VA and ICD-10 guidelines. This program was used to instruct physicians and non-physicians in VA methodology using a train-the-trainer model. Written tests of cognitive and applied knowledge required to classify perinatal COD were administered before and after training to evaluate the effect of the VA training program.
Results
53 physicians and non-physicians (nurse-midwives/nurses and Community Health Workers [CHW]) from Pakistan, Zambia, the Democratic Republic of Congo, and Guatemala were trained. Cognitive and applied knowledge mean scores among all trainees improved significantly (12.8 and 28.8% respectively, p<0.001). Cognitive and applied knowledge post-training test scores of nurse-midwives/nurses were comparable to those of physicians. CHW (high-school graduates with 15 months or less formal health/nursing training) had the largest improvements in post-training applied knowledge with scores comparable to those of physicians and nurse-midwives/nurses. However, CHW cognitive knowledge post-training scores were significantly lower than those of physicians and nurses.
Conclusions
With appropriate training in VA, cognitive and applied knowledge required to determine perinatal COD is similar for physicians and nurses-midwives/nurses. This suggests that midwives and nurses may play a useful role in determining COD at the community level, which may be a practical way to improve the accuracy of COD data in rural, remote, geographic areas.
Keywords: perinatal mortality, education, non-physicians, verbal autopsy
Introduction
Early neonatal deaths (death of a newborn <7 days of age) and stillbirths, together known as perinatal deaths, account for 7 m annual deaths worldwide (Lawn et al. 2005, 2006; Stanton et al. 2006; WHO 2007a). Perinatal deaths contribute four percent of the global burden of disease and are the leading cause of the burden of disease measured in disability adjusted life years (DALYs) in low and middle income countries (LMIC) (Lopez et al. 2006). Perinatal deaths are the leading cause of death (COD) among children 0-14 years of age worldwide, and in this age group, cause twice as many deaths as malaria and HIV/AIDS combined (Lopez & Mathers 2006). 98% of these perinatal deaths occur in LMIC, with more than 70% occurring in community settings, often in the home (Bang et al. 2005; Baqui et al. 2006; Sule & Onayade 2006). Furthermore, a high percentage of births and deaths are not recorded in vital registration systems (Carlough & McCall 2005; Lawn et al. 2005; McClure et al. 2007).
Understanding causes of perinatal death, which vary between and within geographic regions, is essential when developing strategies to reduce perinatal mortality. Decisions about health care spending have competing considerations. Paramount among these must be a thorough and accurate understanding of the leading causes of perinatal death. Unfortunately, a major barrier to improving perinatal mortality outcomes and data collection in LMIC is that vital registration systems that include COD are available for only 3% of all perinatal deaths worldwide. Thus, current data on perinatal COD may be inaccurate, and perinatal mortality rates may be underestimated (Jehan et al. 2007).
Several studies have examined causes of community-based perinatal deaths using verbal autopsy (VA) (Hinderaker et al. 2003; Baqui et al 2006; Setel et al. 2006). VA is a technique used to assign probable COD, based on an interview with a primary caregiver (usually the mother) where health registration systems are weak or unavailable. During the interview, a systematic description of the signs, symptoms, and circumstances preceding the death is recorded. Subsequently, a physician panel removed from the site of death independently assigns COD from the interview data (Marsh et al. 1993; Chandramohan et al. 2005; Baiden et al. 2007). VA provides useful data describing causes of perinatal deaths in developing countries and is an important tool to guide health care programs and policy in low-resource settings (Whiting et al. 2006).
The utility of VA may be limited by the lack of a standard, widely applicable methodology to determine COD, such as validated, training techniques for interviewers and physician panels (Soleman et al. 2006). To address this deficiency, we designed a study to develop and evaluate a VA training program. Our objectives were twofold: 1) to develop a standardized VA tool and training program and 2) to evaluate whether implementation of this tool and training program, using a train-the-trainer model, would result in comparable knowledge regarding uniform classification of perinatal COD by non-physicians compared to physicians.
Methods
Design and development of the VA tool and training program
The VA tool, training manual, and guidelines for conducting the VA interview were adapted from the previously validated SAmple Vital registration with Verbal AutopsY (SAVVY 2006) instrument (Mswia et al. 2006). The training program consisted of four modules: 1) Causes of stillbirth and early neonatal deaths worldwide; 2) Principles, guidelines, and rules for assigning COD developed from the International Statistical Classification of Diseases and Related Health Problems, tenth revision (ICD-10) (WHO 2005b); 3) Case definitions of maternal and neonatal causes of death with commonly associated signs, symptoms, and complications, and representative case studies to illustrate common perinatal problems in verbal autopsy; and 4) written tests of cognitive and applied knowledge.
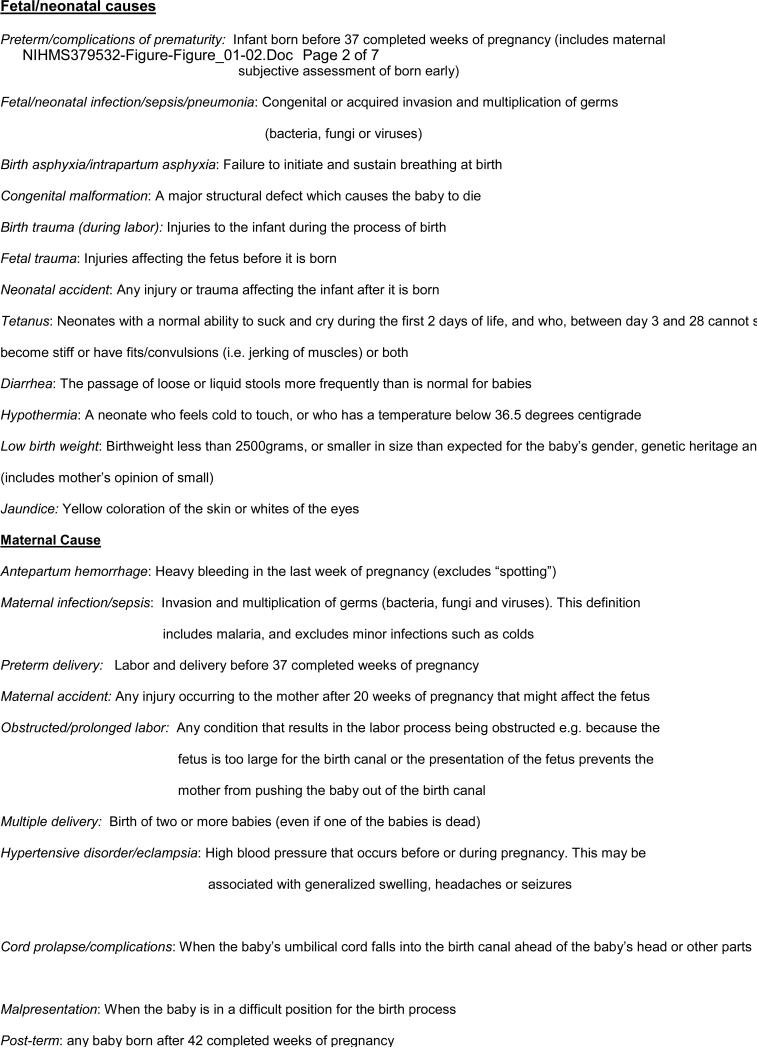
Consistent with ICD-10 classification, the underlying cause of death was defined as the single most important disease or condition which initiated the train of morbid events leading directly to fetal or neonatal death or the circumstances of the accident or violence which produced the fatal injury. The final cause of death was defined as the one factor/disease that was the final event which resulted in the neonatal/fetal death. Contributing factors were all conditions/diseases contributing to neonatal/fetal mortality. Case definitions for the most common underlying, final, or contributing causes of fetal and neonatal death were grouped into maternal and fetal/neonatal causes (Figure 1). These classifications were made to the third character of the ICD-10. To develop these case definitions, all available electronic health and social science reference libraries (including indexed and non-indexed journals) published from 1950-2006 were searched. These included Pub Med/MEDLINE, the Cochrane Reference Library, POPLINE, LILACS, PAHO, African Index Medicus, and EMRO. All papers with an abstract in English were reviewed. Manual reviews of documents and recommendations from the World Health Organization (WHO) and other experts, the Cochrane Reference Library, and monographs on stillbirth and neonatal death from African Ministries of Health and non-governmental organizations such as Saving Newborn Lives and UNICEF were conducted. The training materials were developed and reviewed by an international panel of experts and adapted according to their suggestions. Pilot testing was done using a convenience sample of investigators from the National Institute of Child Health and Human Development Global Network for Women's and Children's Health Research (GN).
Figure 1.
Case definitions for maternal and neonatal/fetal underlying, final, and contributing causes of death
Study Setting
This study was conducted within the GN, a multi-country research network committed to improving the health of mothers and infants, building local capacity for performing research, and strengthening scientific and community partnerships. Participating sites included Argentina, Guatemala, Democratic Republic of Congo (DRC), Zambia, Kenya, India, and Pakistan. This VA study involved sites in Guatemala, DRC, Zambia and Pakistan and was conducted between May 2007 and June 2008.
The VA training methods
A train-the-trainer model was used. Initial training was provided by an expert in ICD-10 classification, rules and guidelines for assignment of COD, and VA methodology. Subsequently, nine trainees (eight physicians and one nurse-midwife) from Pakistan, Zambia, the DRC, and Guatemala (designated national coordinators) were trained by this individual over two days. Physician backgrounds included one pediatrician, two internists and five generalists. Upon returning to their respective countries, these trainees trained an additional 53 trainees including 13 physicians and 40 non-physicians. Physician backgrounds included two pediatricians and 11 generalists. The non-physicians consisted of 21 nurse-midwives and 19 Community Health Workers (CHW). CHW included Lady Health Workers (LHW) from Pakistan with 8-12 years of secondary education and 15 months of government health training and community nurses from Guatemala with less than one year of formal nursing education. Study oversight during local training was provided by VA national coordinators. Additionally, a VA core group (CE, WC, LW, EM and BG) conducted telephone conferences with the VA national coordinators to clarify issues that arose during training.
Evaluation
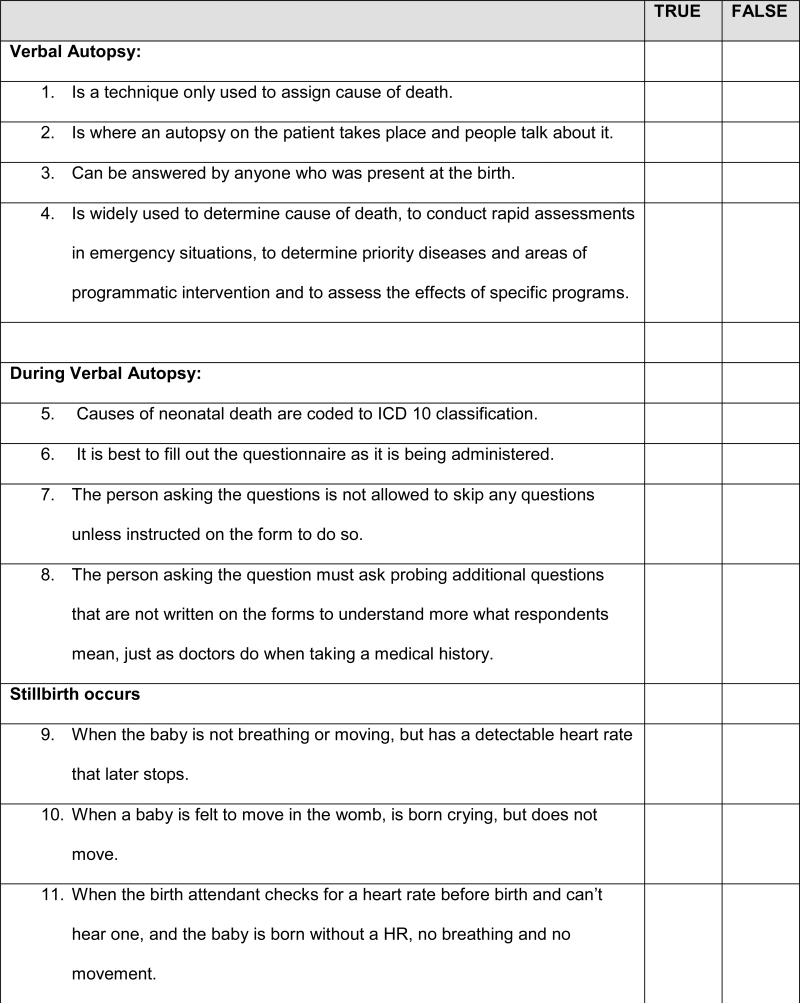
Pre- and post-training tests were administered immediately before and after the completion of a two-day course to evaluate changes in cognitive and applied knowledge. The tests had two modules: 1) Module A (cognitive knowledge module) consisted of 37 true/false questions to evaluate the theoretical knowledge domain and recall of trainees (Figure 2). These questions included assignment of COD based on internationally accepted ICD-10 rules, case definitions used to determine neonatal deaths, and implementation of VA. 2) Module B (applied knowledge module) consisted of case-scenarios which utilized problem-based learning to assess the application of knowledge and decision-making in a given scenario. These case-scenarios included descriptions of circumstances surrounding a stillbirth or early neonatal death from which assignment of COD had to be determined. This module had a maximum of 36 correct answers.
Figure 2.
Module A (Cognitive knowledge) : Questions used to assess cognitive knowledge
Statistical Analysis
Average pre- and post-training test scores were calculated for all participants and by professional background (physician, nurse midwife/nurse and CHW). Differences between pre- and post-training test scores (overall and for each professional group) were analyzed using a paired t-test. To compare scores of both cognitive and applied knowledge modules across professional groups, regression models were calculated using physicians as the reference standard.
Results
All trainees demonstrated significant improvement in cognitive and applied knowledge following training (13 ± 10% improvement in cognitive knowledge and 29± 23 % improvement in applied knowledge, p <0.01, Table 1). Nurse-midwives/nurses and CHWs scored significantly lower on cognitive knowledge pre-training tests compared to physicians (64%±15% and 50% ±17%, vs. 75% ±11%), while post-training, the scores of nurse-midwives/nurses were comparable to those of physicians (77% ±18% vs. 86% ±9%, respectively). All groups had similar percentage changes in cognitive knowledge from pre-training test scores.
Table 1.
Scores on pre- and post-tests by professional group
| n | Pre-training test score Mean (SD) | Post-training test score Mean (SD) | Percentage change from pre-training test score | P-value (change from pre-training test)b | |
|---|---|---|---|---|---|
| COGNITIVE KNOWLEDGE | |||||
| All | 53 | 62 (18) | 75 (18) | 13 (10) | <0.001 |
| Physician | 13 | 75 (11) | 86 (9) | 11 (6) | <0.001 |
| Nurse midwife / Nurse | 21 | 64 (15) | 77 (18) | 13 (12) | <0.001 |
| Community health workera | 19 | 50 (17) | 64 (19) | 14 (10) | <0.001 |
| APPLIED KNOWLEDGE | |||||
| All | 52 | 44 (23) | 72 (20) | 29 (23) | <0.001 |
| Physician | 12 | 62 (15) | 77 ( 10) | 15 (16) | 0.009 |
| Nurse midwife / Nurse | 21 | 53 (20) | 75 (19) | 22 (18) | <0.001 |
| Community health workera | 19 | 24 (12) | 67 (25) | 44 (22) | <0.001 |
Community health workers include community nurses from Guatemala who received less than one year of formal nursing education and Lady Health Workers (LHW) from Pakistan. LHWs are Pakistani government employees with 8-12 years of education and 15 months basic government health training.
Differences between pre- and post-training test mean scores were tested using a paired t-test.
Nurse-midwives/nurses had a 50% greater percentage change from pre-test and attained similar scores to physicians when applied knowledge was assessed. CHWs post-training applied knowledge scores (67±25%) were nearly triple that of their pre-training scores (24±12%). Of the three professional groups, CHWs had the largest percentage change from pre-training test scores, which was approximately double that of nurse midwives and nurses and triple that of physicians. Nevertheless, their post-training test scores remained significantly lower than physicians and nurse midwives/nurses.
By contrast to nurse-midwives/nurses who scored significantly lower on cognitive knowledge pre-training tests compared to physicians, yet post-training had comparable scores to those of physicians (Table 2), CHWs post-training cognitive knowledge test scores remained significantly different compared to those of physicians.
Table 2.
Regression models comparing cognitive knowledge scores across professional groups
| Score | B | SE | p |
|---|---|---|---|
| Pre-training test | |||
| Community health worker | −25.6 | 5.3 | <0.001 |
| Nurse/Midwife | −10.9 | 5.2 | 0.041 |
| Physician | REF | ||
| Post- training test | |||
| Community health worker | −22.3 | 6.0 | <0.001 |
| Nurse/Midwife | −9.5 | 5.8 | 0.110 |
| Physician | REF | ||
| Difference (Post - Pre) | |||
| Community health worker | 3.2 | 3.6 | 0.374 |
| Nurse/Midwife | 1.38 | 3.5 | 0.696 |
| Doctor | REF |
Note: B = unstandardized regression coefficient; REF = reference category. Comparisons between CHW and nurse/midwves on the following: pre-training test (B(SE) = −14.67 (4.65); p=0.003); post- training test (B(SE) = −12.83 (5.24); p = 0.018); difference score (B(SE) = 1.84(3.16); p=0.563).
Nurse-midwives/nurses applied knowledge pre and post-training test results were comparable to physicians, in contrast to pre-training test scores of CHW which were significantly different to physicians (Table 3). Post-training applied knowledge test scores of all professional groups were comparable.
Table 3.
Regression models comparing applied knowledge scores across professional groups
| Score | B | SE | p |
|---|---|---|---|
| Pre- training test | |||
| Community health worker | −38.2 | 6.0 | < .001 |
| Nurse/Midwife | −9.0 | 5.9 | .132 |
| Physician | REF | ||
| Post-test | |||
| Community health worker | −9.4 | 7.4 | .212 |
| Nurse/Midwife | −2.4 | 7.3 | .746 |
| Physician | REF | ||
| Difference (Post - Pre) | |||
| Community health worker | 28.8 | 7.2 | < .001 |
| Nurse/Midwife | 6.6 | 7.0 | .350 |
| Doctor | REF |
Note: B = unstandardized regression coefficient; REF = reference category. Comparisons between CHWs and nurse/midwves on the followng: pre-training test (B(SE) = −29.14 (5.15); p < .001); post-training test (B(SE) = −7.01 (6.38); p=.277); difference scores (B(SE) = 22.14 (6.16); p < .001).
Discussion
Using a train-the-trainer model, our standardized educational program resulted in improvement in post-training test scores compared to pre-training test scores among all health workers in all sites. The train-the-trainer model was chosen for several reasons: 1) it utilizes active-mode learning and multimodal techniques involving dialogue between participants and instructors; 2) there is widespread experience with this mode of learning within the Global Network as it has been employed within previous studies; (McClure et al. 2007) and 3) it has demonstrated utility as a method of diffusing knowledge (Trabeau et al. 2008). Train-the-trainer models have many advantages including increasing trainers’ knowledge, promotion of ownership, and increasing local capacity. Additionally, the relatively low-cost of this train-the-trainer methodology may make this an attractive consideration for VA scale-up in resource-constrained countries.
One of the major limitations of the widespread use of VA for describing perinatal COD has been the lack of harmonization of perinatal VA tools, field procedures and training, and assignment of COD methods (Soleman et al. 2006). In November 2006 (after the development of our tool used for this study), the WHO tasked an expert panel to harmonize the numerous verbal autopsy tools then in use (Baiden et al. 2006). This effort resulted in the publication of a manual on ascertaining and attributing COD that is currently being used in at least 6 countries (WHO 2007c). How widely this document will be utilized is uncertain; however its development appears to be an important step in standardizing tools and procedures for VA. The development and evaluation of a standardized training methodology has been a missing link in the widespread use of VA, and our study attempted to address this.
Studies of non-physician or mid-level provider-led clinical services both in LMIC and high income countries suggest that with adequate training, mid-level providers are able to conduct specified clinical tasks previously thought to be solely within the domain of physicians (Orfaly et al 2005; Burr et al. 2006; Murphy et al. 2008). The paucity of physicians in LMIC has prompted many countries to actively explore and institute service provision by mid-level providers (Braveman & Roemer 1985; Kyriacos et al. 2005; Malawi MOH 2007). The most common method used to determine COD in VA has been by physician panels which generally consist of two to three physicians. These physicians independently determine COD for each death, together discuss differences in their responses, and complete the process by providing a single underlying COD (Garenne & Faveaus 2006; Fantahun et al. 2006). The overall goal of our study was to determine if non-physician providers could be trained to use VA to accurately assign perinatal COD. Our results demonstrate that nurse-midwives/nurses can achieve a level of both cognitive and applied knowledge comparable to that of physicians, to assign COD using VA. This was most evident for the module that tested applied knowledge using case scenarios. These case scenarios were intended to represent the realities of determining community-based COD and require high-order problem-solving skills. Given the critical lack of perinatal mortality data, particularly in rural areas, our results suggest that with uniform training, nurses and midwives may be a valuable resource in determining COD at the community level and may thus contribute to strengthening data systems in rural, remote, geographic areas.
Despite having significantly lower pre-training test scores on both cognitive and applied knowledge modules, CHWs who have considerably less health training than nurses, midwives, and physicians demonstrated a remarkable increase in cognitive and applied knowledge. This increase was most striking in the applied knowledge module where their post-training test scores were nearly triple that of their pre-training test scores and their percentage change from pre-training test scores double that of nurse-midwives/nurses and triple that of physicians. Perhaps surprisingly, given that they had attained comparable applied knowledge scores to other health professionals, CHWs cognitive knowledge post-training test scores were significantly lower than those of physicians and nurse midwives/nurses. This may be because the concepts tested in this module, such as ICD -10 nomenclature and rules, are less familiar to CHW compared to concepts of application of known illnesses tested by case scenarios. It is unclear whether the level of CHW cognitive knowledge may be adequate to qualify them to reliably assign an underlying COD given the timeframe of training provided.
In addition to educating participants on detailed clinical aspects of COD ascertainment, a primary goal of this study was to incorporate in the training program a module which addressed the derivations of various indicators of childhood mortality. These included case definitions, methods, formulae and data sources for the numerators and denominators utilized. We believe that adequate comprehension of these aspects is essential for VA reviewers to understand the relevance and significance of their tasks in COD ascertainment and to understand the impact of their decisions in such cases on the mortality measures which form the overall objective of their activity.
It bears emphasizing that the accuracy in COD ascertainment is largely dependent on the quality of VA data collection, which has its own determinants in terms of interviewer training, respondent characteristics, recall periods and language utilized (Soleman et al. 2006). Therefore, good quality data collection would facilitate accuracy in COD ascertainment, particularly by nurse-midwives, who would apply condition-specific diagnostic algorithms with limited clinical experience in cases where there is ambiguity in the information in the completed VA questionnaire.
The major strengths of this study were the extent of data standardization, the study oversight provided by trainers, and the community-based focus and diversity of the clinical settings. Additionally, each trainee served as his/her own control, minimizing confounders in results. There are a number of limitations to this report. The relatively small sample size for the subject groups, particularly physicians, confers reduced statistical power and generalizability of this study. Although this study evaluated the change in specific short-term cognitive level following the development of a VA training program, the ultimate test of this program is whether in the field, non-physicians can determine COD comparably to physicians. A larger adequately powered study comparing responses by non-physicians to physician panels using this VA tool and educational program may demonstrate broad applicability and is currently underway.
Conclusion
We developed a VA educational package, implemented it using a train-the-trainer methodology, and assessed the short-term change of trainees’ cognitive and applied knowledge following its introduction. All types of health providers showed improvement in post-training test scores compared to pre-training test scores. Mid-level providers (nurses and midwives) demonstrated comparability to physicians in post-training cognitive and applied knowledge test scores. CHWs demonstrated a large increase in post-training test scores when compared to pre-training test scores, although it is unclear whether CHW are adequately equipped to reliably assign perinatal COD using VA. With appropriate training in VA, nurses and midwives may be able to determine perinatal COD with accuracy comparable to that of physicians, and therefore may play a useful role in determining and improving accuracy of COD data in rural, remote, geographic areas.
Acknowledgement
This work was funded by grants from the National Institutes of Child Health and Human Development (U01 HD 40636) and the Bill and Melinda Gates Foundation.
References
- Baiden F, Bawah A, Biai S, et al. Setting international standards for verbal autopsy. Bull World Health Organ. 2007;85:570–571. doi: 10.2471/BLT.07.043745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bang AT, Reddy HM, Bang RA, Deshmukh MD. Why do neonates die in rural Gadchiroli, India? (Part II): estimating population attributable risks and contribution of multiple morbidities for identifying a strategy to prevent deaths. J Perinatol. 2005;25(Suppl 1):S35–43. doi: 10.1038/sj.jp.7211270. [DOI] [PubMed] [Google Scholar]
- Baqui AH, Darmstadt GL, Williams EK, et al. Rates, timing and causes of neonatal deaths in rural India: implications for neonatal health programmes. Bull World Health Organ. 2006;84:706–713. doi: 10.2471/blt.05.026443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman PA, Roemer MI. Health personnel training in the Nicaraguan health system. Int J Health Serv. 1985;15:699–705. doi: 10.2190/C0NM-T69A-1UB8-YFQ1. [DOI] [PubMed] [Google Scholar]
- Burr CK, Storm DS, Gross E. A faculty trainer model: increasing knowledge and changing practice to improve perinatal HIV prevention and care. AIDS Patient Care STDS. 2006;20:83–92. doi: 10.1089/apc.2006.20.183. [DOI] [PubMed] [Google Scholar]
- Carlough M, McCall M. Skilled birth attendance: what does it mean and how can it be measured? A clinical skills assessment of maternal and child health workers in Nepal. Int J Gynaecol Obstet. 2005;89:200–208. doi: 10.1016/j.ijgo.2004.12.044. [DOI] [PubMed] [Google Scholar]
- Chandramohan D, Soleman N, Shibuya K, Porter J. Ethical issues in the application of verbal autopsies in mortality surveillance systems. Trop Med Int Health. 2005;10:1087–1089. doi: 10.1111/j.1365-3156.2005.01510.x. [DOI] [PubMed] [Google Scholar]
- Fantahun M, Fottrell E, Berhane Y, Wall S, Hogberg U, Byass P. Assessing a new approach to verbal autopsy interpretation in a rural Ethiopian community: the InterVA model. Bull World Health Organ. 2006;84:204–210. doi: 10.2471/blt.05.028712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garenne M, Fauveau V. Potential and limits of verbal autopsies. Bull World Health Organ. 2006;84:164–165. [PMC free article] [PubMed] [Google Scholar]
- Hinderaker SG, Olsen BE, Bergsjo PB, et al. Avoidable stillbirths and neonatal deaths in rural Tanzania. BJOG. 2003;110:616–623. [PubMed] [Google Scholar]
- Jehan I, McClure EM, Salat S, et al. Stillbirths in an urban community in Pakistan. Am J Obstet Gynecol. 2007;197:257, e1–8. doi: 10.1016/j.ajog.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyriacos U, Jordan S, van den Heever J. The biological sciences in nursing: a developing country perspective. J Adv Nurs. 2005;52:91–103. doi: 10.1111/j.1365-2648.2005.03555.x. [DOI] [PubMed] [Google Scholar]
- Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: when? Where? Why? Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- Lawn JE, Shibuya K, Stein C. No cry at birth: global estimates of intrapartum stillbirths and Lawn JE, Wilczynska-Ketende K, Cousens SN. (2006) Estimating the causes of 4 million neonatal deaths in the year 2000. Int J Epidemiol. 2006;35:706–718. doi: 10.1093/ije/dyl043. [DOI] [PubMed] [Google Scholar]
- Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- Lopez AD, Mathers CD. Measuring the global burden of disease and epidemiological transitions: 2002-2030. Ann Trop Med Parasitol. 2006;100:481–499. doi: 10.1179/136485906X97417. [DOI] [PubMed] [Google Scholar]
- Malawi Ministry of Health . Five Year National Strategic Plan for Accelerated Childhood Survival and Development. Malawi Ministry of Health Publication; 2007. [Google Scholar]
- Marsh D, Majid N, Rasmussen Z, Mateen K, Khan AA. Cause-specific child mortality in a mountainous community in Pakistan by verbal autopsy. J Pak Med Assoc. 1993;43:226–229. [PubMed] [Google Scholar]
- McClure EM, Nalubamba-Phiri M, Goldenberg RL. Stillbirth in developing countries. Int J Gynaecol Obstet. 2006;94:82–90. doi: 10.1016/j.ijgo.2006.03.023. [DOI] [PubMed] [Google Scholar]
- McClure EM, Carlo WA, Wright LL, et al. Evaluation of the educational impact of the WHO Essential Newborn Care course in Zambia. Acta Paediatr. 2007;96:1135–1138. doi: 10.1111/j.1651-2227.2007.00392.x. [DOI] [PubMed] [Google Scholar]
- Mswia R, Setel P, Hemed Y, Whiting D, Williams D. Sample Vital Registration with Verbal Autopsy : Key informants manual; Verbal autopsy interviewers manual. 2006 [Google Scholar]
- Murphy MA, Neequaye S, Kreckler S, Hands LJ. Should we train the trainers? Results of a randomized trial. J Am Coll Surg. 2008;207:185–190. doi: 10.1016/j.jamcollsurg.2008.02.032. [DOI] [PubMed] [Google Scholar]
- Orfaly RA, Frances JC, Campbell P, Whittemore B, Joly B, Koh H. Train-the-trainer as an educational model in public health preparedness. J Public Health Manag Pract Suppl. 2005:S123–127. doi: 10.1097/00124784-200511001-00021. [DOI] [PubMed] [Google Scholar]
- Setel PW, Whiting DR, Hemed Y, et al. Validity of verbal autopsy procedures for determining cause of death in Tanzania. Trop Med Int Health. 2006;11:681–96. doi: 10.1111/j.1365-3156.2006.01603.x. [DOI] [PubMed] [Google Scholar]
- Soleman N, Chandramohan D, Shibuya K. Verbal autopsy: current practices and challenges. Bull World Health Organ. 2006;84:239–245. doi: 10.2471/blt.05.027003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton C, Lawn JE, Rahman H, Wilczynska-Ketende K, Hill K. Stillbirth rates: delivering estimates in 190 countries. Lancet. 2006;367:1487–1494. doi: 10.1016/S0140-6736(06)68586-3. [DOI] [PubMed] [Google Scholar]
- Sule SS, Onayade AA. Community-based antenatal and perinatal interventions and newborn survival. Niger J Med. 2006;15:108–114. doi: 10.4314/njm.v15i2.37091. [DOI] [PubMed] [Google Scholar]
- Trabeau M, Neitzel R, Meischke H, Daniell WE, Seixas NS. A comparison of “Train-the-Trainer” and expert training modalities for hearing protection use in construction. Am J Ind Med. 2008;51:130–7. doi: 10.1002/ajim.20499. [DOI] [PubMed] [Google Scholar]
- Whiting DR, Setel PW, Chandramohan D, Wolfson LJ, Hemed Y, Lopez AD. Estimating cause-specific mortality from community- and facility-based data sources in the United Republic of Tanzania: options and implications for mortality burden estimates. Bull World Health Organ. 2006;84:940–948. doi: 10.2471/blt.05.028910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization World Health Report -Make Every Mother and Child Count. 2005a [Google Scholar]
- World Health Organization International Statistical Classification of Diseases 10th Revision. (Second Edition) 2005b [Google Scholar]
- World Health Organization Ascertaining and Attributing Cause of Death. A Manual on Verbal Autopsy. 2007 [Google Scholar]