Abstract
Background
HoMBReS was a community-level social network intervention designed to increase sexual health among Latino heterosexual men who were members of a multi-county soccer league.
Methods
We used process data collected each month during 18 months of intervention implementation from each of 15 trained Latino male lay health advisors (known as Navegantes) to explore the activities that Navegantes conducted to increase condom and HIV testing among their social network members.
Results
The Navegantes reported conducting 2,364 activities, for a mean of 8.8 activities per Navegante per month. The most common activity was condom distribution. Most activities were conducted with men; about 2% were conducted with women. Among activities conducted with men, half were conducted with soccer teammates and half with non-teammates.
Conclusions
Latino men’s social networks can be leveraged to promote sexual health within the community. Innovative methods that reach large numbers of community members are needed given the lack of prevention resources for populations disproportionately impacted by HIV and STDs.
Keywords: CBPR, community-based participatory research, Hispanic, HIV/AIDS, immigrant health, Latino, lay health advisor, men’s health, prevention, process evaluation
Introduction
Latinos in the United States (US) continue to carry a disproportionate burden of infectious diseases, including HIV/AIDS. Latinos have the second highest rate of AIDS diagnoses of all racial and ethnic groups and over three times greater AIDS case rate than that of non-Latino whites (Centers for Disease Control and Prevention [CDC], 2009a). Rates of gonorrhea, chlamydia, and syphilis rates are two to four times higher among Latinos than among non-Latino whites (CDC, 2009b). In addition to having a rapidly growing Latino community, many southeastern US states, including North Carolina (NC), consistently lead the US in reported cases of AIDS, gonorrhea, chlamydia, and syphilis (CDC, 2009a, 2009b).
Despite the impact HIV and STDs are having on Latino populations in the US, few resources exist to reduce and eliminate disparities in adverse sexual health outcomes experienced by this vulnerable population. The efficacious interventions that exist (e.g., VOICES/VOCES [O'Donnell, O'Donnell, San Doval, Duran, & Labes, 1998], Modelo de Intervención Psicomédica [MIP; Robles et al., 2004], AMIGAS [Wingood et al., 2011], and HoMBReS-2 [Rhodes, McCoy, et al., 2011]) tend to be small-group interventions and do not reach large numbers of community members.
Innovative strategies to reach large numbers of community members are needed to curb the escalating HIV and STD rates within Latino communities in the US. One strategy used to reduce and eliminate health disparities within vulnerable, “hidden”, and thus neglected communities is the selection, training, and support of lay community members to promote health through the social networks of which they are members. These trained community members are “natural helpers” and often known as village health workers, community health workers, volunteer health workers, community outreach workers, community health service volunteers, public health aides, peer health promoters, community health representatives, community health advocates, or lay health advisors (LHAs). They are thought to be effective because they are ethnically, socio-economically, and experientially similar to members within their existing social networks; are naturally relied on for advice, emotional support, and tangible aid by members of their social networks; possess an intimate understanding of community assets, priorities, and needs; understand what is meaningful to their communities; communicate in a similar language; and can effectively incorporate culture to promote health and prevent diseases within their communities and among those who have traditionally lacked access to adequate care. Generally, they work in community settings, serving as health advisors and referral sources, connecting community members to services, distributing materials, being role models, and advocating on behalf of community members (Eng, Parker, & Harlan, 1997; Eng, Rhodes, & Parker, 2009; Rhodes, Foley, Zometa, & Bloom, 2007; Viswanathan et al., 2010). It has been suggested that trained lay community members may be effective to reach members of growing immigrant Latino communities in the US because they may provide the most tailored and culturally congruent messages (Institute of Medicine & Committee on Prevention and Control of Sexually Transmitted Diseases, 1997; McQuiston & Gordon, 2000; Rhodes et al., 2007).
Despite a broad literature base, evidence of harnessing lay community members to effect change within their social networks is limited, particularly among Latinos; evaluations tend to focus on behavior change and leadership development among natural helpers, not among the community members they are trained to reach (Arcury, Marin, Snively, Hernandez-Pelletier, & Quandt, 2009; Eng et al., 2009; Fernandez, Jacobs, Warren, Sanchez, & Bowen, 2009; Rhodes et al., 2007; Viswanathan et al., 2010; Wang, Brown, Shen, & Tucker, 2011). Of the few existing interventions with evidence of effectiveness at the community level, only one published lay community member-led social network intervention with positive outcomes specifically focused on men and their health priorities (CDC, 2011; Rhodes, Hergenrather, Bloom, Leichliter, & Montaño, 2009). The paucity of male-focused lay community member-led social network interventions is not unique to Latinos, but the reason for this gap is unclear (Eng & Hatch, 1992; Eng et al., 2009; Rhodes et al., 2007); it has been well established that social support has a stronger protective effect against morbidity and mortality for men than for women (Shumaker & Hill, 1991).
Hombres Manteniendo Bienestary Relaciones Saludables (HoMBReS; Men Maintaining Wellbeing and Healthy Relationships) was a community-level social network intervention that trained immigrant Latino men from the lay community serve as LHAs known as “Navegantes” (“Navigators”) to increase condom use and HIV and sexually transmitted disease (STD) testing among their existing soccer team-based social networks. The development of the HoMBReS intervention (Rhodes et al., 2006) and the results of its pilot evaluation in partnership with Latino soccer leagues in NC have been described; promising results were found (CDC, 2011; Rhodes, Hergenrather, Bloom, et al., 2009). Briefly, at post-intervention assessment, the intervention increased condom use and HIV/STD testing among teammates in the intervention compared to their peers in the comparison control group (Rhodes, Hergenrather, Bloom, et al., 2009).
With data demonstrating the effectiveness of the LHA approach within their soccer team-based social networks to reduce sexual risk among Latino men, we designed this analysis to explore the activities that Navegantes conducted. We examined process data collected from Navegantes throughout the 18 months of implementation of the HoMBReS intervention to offer a snapshot of Navegantes activities. We also outline implications of our findings for subsequent studies using male natural helpers to promote sexual health within their social networks.
Methods
Community-based Participatory Research (CBPR)
This study was guided by our ongoing CBPR partnership comprised of representatives from public health departments, universities, community-based organizations (CBOs), the CDC, and the local Latino community, who have worked together for over a decade (Rhodes, Hergenrather, Griffith, et al., 2009; Rhodes, Hergenrather, et al., 2011; Rhodes, Malow, & Jolly, 2010). Blending the lived experiences of community members, the experiences of organizational representatives based in ongoing public health practice and service provision, and sound science can yield research questions that are more pertinent to community health and wellbeing; study designs and evaluations that are more authentic to community members’ natural ways of doing things; more informed understandings of health-related phenomena; and interventions that are more relevant, culturally congruent, and, consequently, more successful and potentially more sustainable (S. B. Cashman et al., 2008; Eng et al., 2005; Minkler, 2002; Rhodes, 2012; Rhodes, Hergenrather, et al., 2011; Rhodes et al., 2010; Wallerstein et al., 2008). Our partnership adheres to principles that include mutual respect; building upon partner strengths; moving findings into action; and disseminating findings to community members, policy makers, and research and clinical audiences (Rhodes, Hergenrather, et al., 2011).
Because of a lack of interventions designed for Spanish-speaking communities in the US and a desire to meet the prevention needs of this community, our partnership initially collected formative data from Latino men who were part of a large multi-county soccer league of adult immigrant Latino men. Data suggested that sexual health was a priority for immigrant Latino men and interventions were desired; misinformation and myths about HIV and STDs existed; socio-cultural and expectations of masculinity promoted sexual risk; and there were numerous barriers to access and utilize health care in the US. Soccer teams were identified as a naturally existing social structure in which large numbers of sexually active Latino men could be reached through a gender-specific and culturally congruent intervention programming (Rhodes et al., 2006; Rhodes, 2012). Based on these formative data, our partnership developed the HoMBReS intervention.
The HoMBReS Intervention
From 89 existing soccer teams with a total of 1,600–1,800 adult Latino men in a local soccer league in NC, 30 teams were selected and recruited to serve as intervention teams (n=15) and control teams (n=15). The intervention teams included teams from the southern region of the league for two primary reasons. First, formative data already existed on local resources; referral procedures; and healthcare service delivery in this region; and second, intervention and control teams needed to be geographically and socially distinct to minimize contamination. We compared baseline data to determine whether there were significant differences between participants by intervention or control group; however, there were no differences identified between participants in the intervention and control groups at baseline on a variety of variables including: age, country of origin, educational attainment, and accompaniment status (e.g., single, married but in the US alone, with a partner/spouse/wife), income, amount of money sent home, employment status, sexual orientation, mastery, HIV and STD knowledge, sexual behaviors, masculinity, and acculturation (CDC, 2011; Rhodes, Hergenrather, Bloom, et al., 2009).
The project coordinator, a Latino man with a similar immigration experience as members of the soccer league, explained the project to each team, emphasized the expectations of serving as a Navegante in this study, and focused on three key characteristics that the CBPR partnership identified as being key to Navegante success: personal, performance, and situational characteristics. Personal characteristics included attributes such as having a sense of humor and being a natural leader, dedicated, and respectful. The potential Navegante had to be (or have potential to be trained to be) comfortable talking and offering sound advice about sensitive issues (e.g., sexual health and condoms) and remaining discreet. Performance characteristics included the ability of the potential Navegante to read low literacy study materials, complete process data collection forms, and communicate orally; and his willingness to participate in meetings and work with his soccer team-based social networks. Situational characteristics included time availability and access to regular transportation.
Teammates nominated and elected one Navegante per intervention team. During a four-session, 16-hour Navegante training, which was held over two consecutive weekends, the 15 Navegantes who represented intervention teams were trained to serve as: (1) health advisors to make referrals to increase knowledge about HIV, STDs, and testing, and increase condom use skills; (2) opinion leaders to bolster positive and reframe negative socio-cultural expectations about what it means to be a man; and (3) community advocates to act on behalf of their communities. The training was based in social cognitive theory (Bandura, 1986; Rhodes et al., 2006) and empowerment education (Freire, 1973; Rhodes et al., 2006). Navegantes were specifically trained to work formally and informally with their soccer team-based social networks (e.g., conducting condom use presentations to their soccer team, talking one-on-one with a teammate about initiating condom use with a new partner). Navegantes were trained to use the ask-advise-assist model (Whitlock, Orleans, Pender, & Allan, 2002). The 15 Navegantes worked with their teammates for 18 consecutive months.
Process Data
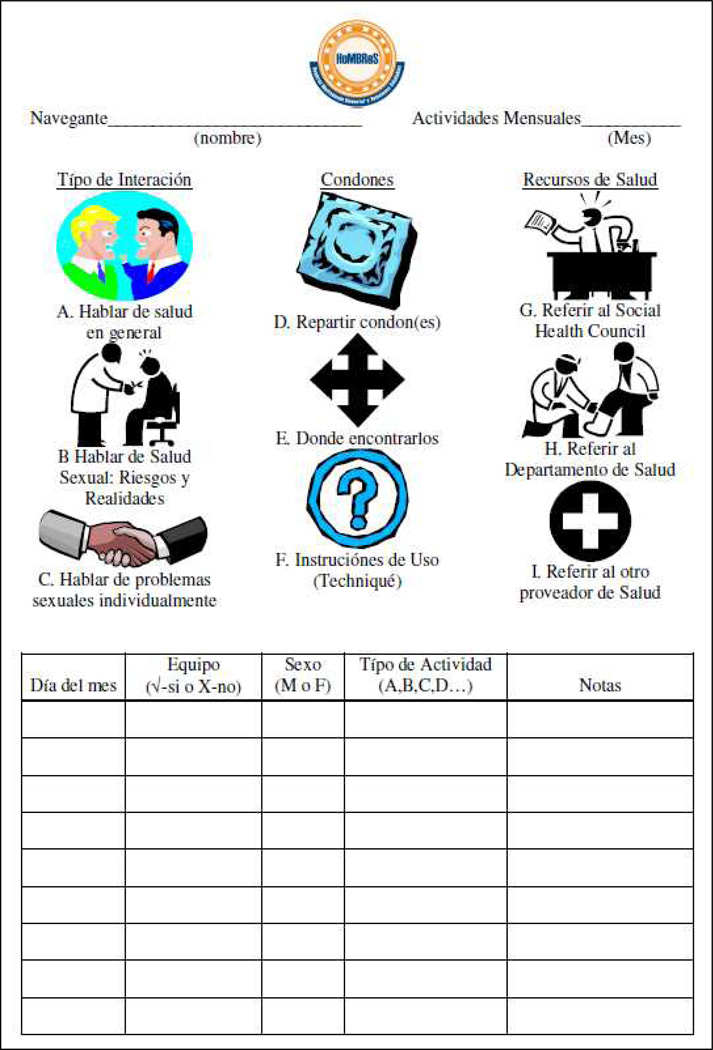
During the development of the intervention, CBPR partnership members developed a Spanish-language Activity Log to collect process data. Navegantes documented their activities on the Activity Log, which we designed to be brief, easily completed, and not require high levels of literacy (See Figure 1). Navegantes documented nine types of activities: talking about (A) health in general, (B) sexual health, and (C) individual sexual problems; (D) distributing condoms, (E) describing where to get condoms, and (F) providing information on the correct use of condoms; and providing referrals to (G) Chatham Social Health Council (a partner CBO), (H) the public health department, or (I) another health provider. Activities could be formal (e.g., leading a planned condom demonstration with social network members) or informal (e.g., casually providing the address of an HIV testing site to a social network member).
Figure 1.
Navegante Activity Log
Navegantes also documented the day of the week that the activity occurred, whether participants in the activity were their soccer teammates and/or included non-teammates, and the sex of participants.
During their training, Navegantes practiced completing the Activity Log. During intervention implementation, Navegantes met each month with the project coordinator to develop their within-group social network and support as Navegantes, plan intervention activities, share experiences, resolve problems, and submit Activity Logs. Each Navegante was compensated $50 per month for his Activity Log. Navegantes were told that compensation was for the Activity Log itself and that if no activities were completed, they should turn in a blank Activity Log; nevertheless, they still would be paid. This approach was designed to reduce the risk of data being falsified.
We double-entered Activity Log data into an Excel spreadsheet to ensure accuracy, corrected the few discrepancies by reviewing the original Activity Log, and then imported data into SPSS 19 (Chicago, IL) for analysis. We calculated frequencies for activities overall, each activity, total activities by month and by day of month, and by soccer team-based social network, non-teammates, and women. We calculated statistically significant differences between activities that included members of soccer team-based social network and activities that included non-teammates; we considered a two-sided P-value < 0.05 as statistically significant.
Human subject review and study oversight were provided by the Institutional Review Board (IRB) of Wake Forest School of Medicine.
Results
Fifteen intervention Navegantes participated, and each completed and turned in an Activity Log each month for 18 months (total of 270 Activity Logs); Navegantes initiated activities in May and concluded in October the following year. Mean age was 31.5 (range 23–60) years, and all self-identified as Latino and were native Spanish speakers with limited English skills. Seventy percent were married and reported less than high school education; 80% reported currently working (Rhodes, Hergenrather, Bloom, et al., 2009).
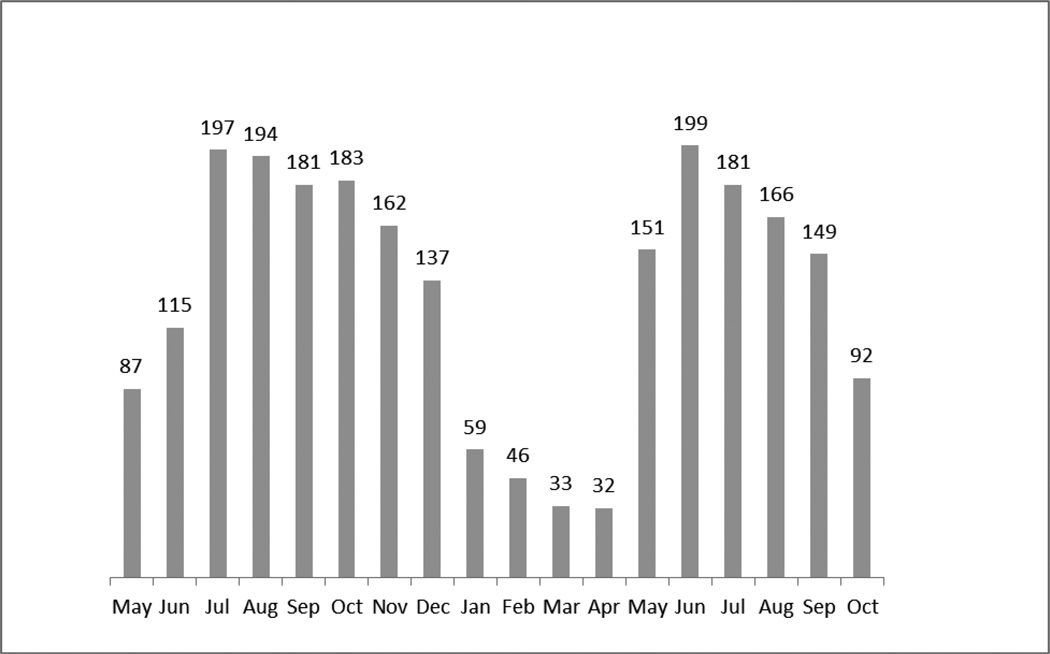
Navegantes engaged in 2,364 activities during implementation. Figure 2 illustrates the total number of activities that Navegantes performed each month during implementation. Navegantes performed the greatest number of activities during the soccer season (i.e., May-December). Navegantes performed the least number of activities during the winter months (i.e., January-April) when the soccer league did not play because of the cold weather.
Figure 2.
Number of Navegante Activities by Month
Each Navegante reported engaging in at least one activity per month; the mean number activities per Navegante was 8.8 activities per month; however, the number of activities by Navegante varied from a minimum of 1.3 to a maximum of 24 activities per month. Frequencies and percentages by Navegante activity and participant (i.e., whether the activity included soccer teammates exclusively, non-teammates, and women) are presented in Table 1.
Table 1.
Frequency of Navegante Activity By Participant Type
| Navegante Activity | Total (% of all activities) |
Teammate only (%) |
Included non- teammate (%) |
Included women (%)1 |
|---|---|---|---|---|
| Talked about health in general | 149 (6.3) | 65 (5.5) | 84 (7.2)* | 2 (4.4) |
| Talked about sexual health, risks, and realities | 439 (18.6) | 181 (15.2) | 258 (22.0)* | 18 (39.1) |
| Talked about individual sexual problems | 352 (13.8) | 144 (12.1) | 208 (17.7)* | 9 (19.6) |
| Distributed condoms | 1,033 (43.7) | 623 (52.3)* | 410 (35.0) | 11 (23.9) |
| Described where to get condoms | 125 (5.3) | 47 (4.0) | 78 (6.7)* | 0 |
| Provided information on the correct use of condoms | 141 (6.0) | 66 (5.5) | 75 (6.4)* | 0 |
| Provided referrals to Chatham Social Health Council | 27 (1.1) | 22 (1.8)* | 5 (0.4) | 3 (6.5) |
| Provided referrals to local health department | 51 (2.2) | 27 (2.3)* | 24 (2.0) | 1 (2.2) |
| Provided referrals to another health provider | 47 (2.0) | 16 (1.3) | 31 (2.6)* | 2 (4.4) |
| TOTAL | 2,364 | 1,191 | 1,173 | 46 |
Women are also included in the non-teammate column.
=Statistically significant differences at p<.01 between activities that included teammates only versus activities that included non-teammates.
Overall, the most common activity conducted by the Navegantes was condom distribution, comprising nearly half of all activities; about one in five activities conducted by Navegantes included discussions of sexual health, risks, and realities of HIV and STDs. The least common activities that Navegantes conducted included referrals to Chatham Social Health Council, local health departments, and other health providers.
About half (50.38%) of all Navegante activities were conducted exclusively with teammates; the other half included non-teammates. However, Navegantes conducted over 98% of their activities with other men; only 46 activities included women.
Significant differences were identified for each of the nine documented activities depending on the composition of the group (i.e., soccer team-based social network members only or non-teammates included). Navegantes distributed condoms more frequently and provided more referrals to Chatham Social Health Council and local health departments when activities included only their soccer team-based social network members. In contrast, Navegantes talked about health in general, sexual health, and individual sexual problems; described where to get condoms, provided information on the correct use of condoms, and provided referrals to other providers more often when non-teammates were included in the activities.
Navegantes were most active during the weekend. Half of activities conducted occurred during the weekend when soccer games occurred; 18.3% of all activities on Saturday and 32.2% on Sunday (See Table 2).
Table 2.
Number of Activities by Day of the Week
| Day of Week | Number of activities (%) |
|---|---|
| Monday | 169 (7.2) |
| Tuesday | 265 (11.2) |
| Wednesday | 227 (9.6) |
| Thursday | 260 (11.0) |
| Friday | 246 (10.4) |
| Saturday | 433 (18.3) |
| Sunday | 764 (32.3) |
Discussion
Little is known about the activities of natural helpers and what they do after being trained to promote behavior change within their social networks (Ayala, Vaz, Earp, Elder, & Cherrington, 2010; Eng et al., 2009; Rhodes et al., 2007; Viswanathan et al., 2010). This analysis of available process evaluation data provides insight into the activities engaged in by Latino male Navegantes, who were part of the HoMBReS intervention, to increase condom use and HIV and STD testing within their naturally existing social networks.
Several findings deserve highlighting. First, there was a “start-up” period, after training, during the first two months of intervention implementation. This time period could reflect the time in which Navegantes became more familiar and comfortable with their roles. However, this time period also could reflect the time it took for members within their social networks to understand the roles of the Navegantes and begin to rely on them for support related to sexual health.
Furthermore, Navegantes were more likely to perform activities during the soccer season. Although we trained them to work with their teammates, it was not clear whether they would have sufficient time to serve as Navegantes during the soccer season. However, the Navegantes performed fewer activities during the winter months when the teams were not training or playing. It was not previously clear whether activities would increase or decrease with the increase or decrease of soccer activities; after all, Navegantes were trained to work with their members of their soccer team-based social networks formally and informally without regard to the context in which activities occurred. Interventions designed to meet the needs of Latino men through soccer teams, need to consider the seasonality of soccer and the implications of seasonality on reach and engagement of social network members. Third, Navegantes also conducted more activities on Saturdays and Sundays when the teams met to play soccer; half of all activities were conducted on the weekend days. We do not know, however, where these activities occurred, whether in soccer fields or at other locations (e.g., at a soccer team member’s home).
Fourth, although each Navegante reported engaging in at least one activity per month, the range was broad with one Navegante reporting 24 activities in a single month. Further research is needed to explore the underlying reasons for these differences and evaluate the necessary dose needed to promote change among social network members. Because each social network member may need a different dose of the intervention, future process and outcome evaluations of social network interventions should explore ways to link exposure to activities of each social network member to his outcome data. The transtheoretical stages of change model (Prochaska, DiClemente, & Norcross, 1992) may be useful in determining the dose required for each social network member based on his readiness to change. Activity Logs could be expanded to include who specifically participated in each activity conducted by the Navegante. Thus, outcomes could be better explored in order to determine the necessary dose and number and type of activities warranted. An advantage of natural helping is the ability to tailor helping to the precise needs of social network members. For example, a social network member may need merely clarification to facilitate change (e.g., getting tested for HIV) while another may need more ongoing social support to facilitate the same change. We did not capture this level of detail within this study.
Fifth, condom distribution was the most common activity. This may be an easy and/or effective strategy for a Navegante to establish himself as an expert and/or communicate his willingness to discuss sensitive subjects.
Sixth, Navegantes conducted about half of activities with soccer team-based social network member and half with non-teammates. This finding illustrates the potential to reach beyond each Navegante’s soccer team-based social network. However, the type of activities engaged in with community differed based on whether someone was a member of a soccer team-based social network or another social network. Navegantes were more likely to distribute condoms and provide referrals to Chatham Social Health Council and local health departments when activities included their soccer team-based social networks exclusively than when the activities included non-teammates. This may be the result of a Navegante assumption that the materials (e.g., condoms) that they were provided in this intervention study were to be distributed to their teammates only. Further, because representatives from Chatham Social Health Council and local health departments were part of the CBPR partnership that developed the intervention and were included in the Navegante training, it could be that Navegantes also assumed that these two resources were again for their soccer team-based social networks as opposed to non-teammate social networks. Future studies should better explore how trained natural helpers make decisions about resource distribution. Future research also should explore whether interventions like HoMBReS are effective in promoting behavioral change beyond the social networks utilized for intervention evaluation. In the case of HoMBReS, we do not know whether those reached (but from whom no data were collected) changed behavior (e.g., increased condom use or HIV/STD testing).
Finally, Navegantes reported implementing few activities with women. This finding makes sense in at least two ways. Navegantes were trained to work with other men, specifically members of their soccer team-based social networks; Navegantes were not trained to initiate discussions or use the ask-advise-assist model with women. Further, Latino men may be less likely to discuss issues related to sex and sexual health with women given adherence to cultural values that discourage discussions of sex (R. Cashman, Eng, Simán, & Rhodes, 2011; Hirsch, Higgins, Bentley, & Nathanson, 2002; Organista, 2007). However, nearly a third of total activities that the Navegantes reported conducting included talking about sexual health, risks, and realities (18.6%), and talking about individual sexual problems (13.8%). This is most likely due to the election of Navegantes who were willing to “break” sexual silence and the careful training and ongoing support of Navegantes that may have helped Navegantes meet the sexual health needs of other men in their social networks. Further research may be warranted to determine whether male Navegantes, who undergo training to reach women, can reach women within their social networks in the same ways they are able to reach other men.
Implications for Research and Practice
Our CBPR partnership took the lessons learned from these process findings to enhance the intervention to further meet the sexual priorities and needs of Latino men. For example, we developed Spanish-language DVD vignettes that serve as triggers for discussion and provide role modeling during Navegante training. Vignettes include (1) a vignette designed to role model how to use naturally occurring opportunities to help other men; and (2) the process of getting tested in a health department through the eyes of a non-English-speaking Latino man.
We also added training for Navegantes to use some of the vignettes with their social network members. The vignette that follows a Latino man through the HIV/STD testing process, for example, allows social network members to identify the challenges they will face (e.g., limited interpreters, requests for picture identification) and learn how these challenges can be overcome them (e.g., eventually an interpreter will be available, Latino men are eligible for testing without identification). This addition also has resulted in a provision of a portable DVD player that Navegantes can borrow if there is not one available locally.
Navegantes also take a tour of each public health department within their catchment area to increase their comfort level with understanding the local processes of assessing and utilizing services. This tour is designed to increase referrals to these resources and is conducted in partnership with health department personnel to ensure that Navegantes meet, learn the names of, and build trust (based on initial impression) with key individuals within the health department, including front desk staff, interpreters, and clinical staff.
Furthermore, after the Navegantes are trained, we added an event with each soccer team-based social network to inaugurate the role of their Navegante. This event is designed to once again explain the intervention, outline the type of training the Navegante received, and promote his knowledge base and various roles. This inauguration includes representation from the CBPR partnership to provide further “credibility” to the Navegante within the community.
Limitations
There are limitations of this analysis that should be acknowledged. First, linkages between the three roles of the Navegantes (e.g., health advisors, opinion leaders, and community advocates) and the data collected on the Activity Logs were not precise; we did not measure the role of Navegantes serving as opinion leaders or community advocates. We also were not able to distinguish between one-on-one activities and group activities which Navegantes conducted. Similarly, we were unable to determine whether activities that included non-teammates, also included teammates. Finally, we could not determine dose; because we did not collect data describing with whom the Navegante interacted, we do not know how many activities a social network member received and/or required to effect behavior (i.e., consistently using condoms or getting tested for HIV). Future iterations of the Activity Log should explore what data can be reliably collected to provide better insights to quantify the activities of Navegantes while keeping data collection burden at a minimum.
Conclusions
The Navegantes who were trained in the HoMBReS intervention averaged nearly nine activities per month for 18 months; the vast majority of these activities were conducted with other men, demonstrating that Latino men can be elected, trained, and successfully serve as LHAs for other men within their social networks. Such a finding is important given the lack of examples in both research and practice of harnessing male natural helpers to promote health and prevent disease. Moreover, male-led and male-focused LHA interventions could address health disparities among large numbers of vulnerable men in the US, a population whose health promotion and disease prevention needs have been traditionally neglected (Treadwell & Ro, 2003). Future research should explore the use of natural helpers to effectively meet other men’s health priorities (e.g., occupational health, diabetes) and the potential to harness other types of social networks (as opposed to soccer team-based social networks).
Given its potential to meet the prevention needs of large numbers of members within vulnerable communities, this approach harnessing the existing social networks of community members also should be further explored within other populations including Latino men who have sex with men (MSM) and Latina women. Overall our arsenal to prevent HIV and STD infection is limited, and it is imperative to develop, test, and identify, strategies to effectively reach large numbers of community members if we hope to substantially reduce infection rates. Given their potential reach, natural helpers as a community asset may be particularly key to reduce the HIV epidemic within vulnerable communities that are disproportionately affected.
References
- Arcury TA, Marin A, Snively BM, Hernandez-Pelletier M, Quandt SA. Reducing farmworker residential pesticide exposure: evaluation of a lay health advisor intervention. Health Promot Pract. 2009;10(3):447–455. doi: 10.1177/1524839907301409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayala GX, Vaz L, Earp JA, Elder JP, Cherrington A. Outcome effectiveness of the lay health advisor model among Latinos in the United States: an examination by role. Health Educ Res. 2010;25(5):815–840. doi: 10.1093/her/cyq035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs: Prentice-Hall; 1986. [Google Scholar]
- Cashman R, Eng E, Simán F, Rhodes SD. Exploring the sexual health priorities and needs of immigrant Latinas in the southeastern US: A community-based research approach. AIDS Education and Prevention. 2011;23(3):236–248. doi: 10.1521/aeap.2011.23.3.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cashman SB, Adeky S, Allen AJ, Corburn J, Israel BA, Montaño J, Eng E. The power and the promise: working with communities to analyze data, interpret findings, and get to outcomes. Am J Public Health. 2008;98(8):1407–1417. doi: 10.2105/AJPH.2007.113571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report. Vol. 19. Atlanta: 2009a. [Google Scholar]
- Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance, 2008. Atlanta, GA: U.S. Department of Health and Human Services; 2009b. [Google Scholar]
- Centers for Disease Control and Prevention. 2011 Compendium of Evidence-Based HIV Prevention Interventions. Atlanta, GA: US Department of Health and Human Services; 2011. [Google Scholar]
- Eng E, Hatch JW. Networking between agencies and Black churches: The lay health advisor model. In: Pargament KI, Maton KI, Hess RE, editors. Religion and Prevention in Mental Health: Research, Vision, and Action. 1992. [Google Scholar]
- Eng E, Moore KS, Rhodes SD, Griffith D, Allison L, Shirah K, Mebane E. Insiders and outsiders assess who is "the community": Participant observation, key informant interview, focus group interview, and community forum. In: Israel BA, Eng E, Schulz AJ, Parker E, editors. Methods for Conducting Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2005. pp. 77–100. [Google Scholar]
- Eng E, Parker E, Harlan C. Lay health advisor intervention strategies: a continuum from natural helping to paraprofessional helping. Health Educ Behav. 1997;24(4):413–417. doi: 10.1177/109019819702400402. [DOI] [PubMed] [Google Scholar]
- Eng E, Rhodes SD, Parker EA. Natural helper models to enhance a community's health and competence. In: DiClemente RJ, Crosby RA, Kegler MC, editors. Emerging Theories in Health Promotion Practice and Research. Vol. 2. San Francisco, CA: Jossey-Bass; 2009. pp. 303–330. [Google Scholar]
- Fernandez MI, Jacobs RJ, Warren JC, Sanchez J, Bowen GS. Drug use and Hispanic men who have sex with men in South Florida: implications for intervention development. AIDS Educ Prev. 2009;21(5 Suppl):45–60. doi: 10.1521/aeap.2009.21.5_supp.45. [DOI] [PubMed] [Google Scholar]
- Freire P. Education for critical consciousness. New York, NY: Seabury Press; 1973. [Google Scholar]
- Hirsch JS, Higgins J, Bentley ME, Nathanson CA. The social constructions of sexuality: Marital infidelity and sexually transmitted disease-HIV risk in a Mexican migrant community. Am J Public Health. 2002;92(8):1227–1237. doi: 10.2105/ajph.92.8.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine, & Committee on Prevention and Control of Sexually Transmitted Diseases. The hidden epidemic: Confronting sexually transmitted diseases. Washington, DC: National Academy Press; 1997. [Google Scholar]
- McQuiston C, Gordon A. The timing is never right: Mexican views of condom use. Health Care Women Int. 2000;21(4):277–290. doi: 10.1080/073993300245140. [DOI] [PubMed] [Google Scholar]
- Minkler M, Wallerstein N. Improving health education through community building organization and community building: a health education perspective. In: Minkler M, editor. Community Organizing and Community Building for Health. New Brunswick, NJ: Rutgers University Press; 2002. pp. 30–52. [Google Scholar]
- O'Donnell CR, O'Donnell L, San Doval A, Duran R, Labes K. Reductions in STD infections subsequent to an STD clinic visit. Using video-based patient education to supplement provider interactions. Sex Transm Dis. 1998;25(3):161–168. doi: 10.1097/00007435-199803000-00010. [DOI] [PubMed] [Google Scholar]
- Organista KC. Solving Latino psychosocial and health problems: Theory, practice, and populations. Hoboken, NJ: John Wiley and Sons; 2007. [Google Scholar]
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47(9):1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Rhodes SD. Demonstrated effectiveness and potential of CBPR for preventing HIV in Latino populations. In: Organista KC, editor. HIV Prevention with Latinos: Theory, Research, and Practice. New York, NY: Oxford; 2012. pp. 83–102. [Google Scholar]
- Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: A qualitative systematic review. Am J Prev Med. 2007;33(5):418–427. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Hergenrather KC, Bloom FR, Leichliter JS, Montaño J. Outcomes from a community-based, participatory lay health advisor HIV/STD prevention intervention for recently arrived immigrant Latino men in rural North Carolina, USA. AIDS Educ Prev. 2009;21(Supplement 1):104–109. doi: 10.1521/aeap.2009.21.5_supp.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Hergenrather KC, Griffith D, Yee LJ, Zometa CS, Montaño J, T VA. Sexual and alcohol use behaviours of Latino men in the south-eastern USA. Cult Health Sexy. 2009;11(1):17–34. doi: 10.1080/13691050802488405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Hergenrather KC, Montano J, Remnitz IM, Arceo R, Bloom FR, Bowden WP. Using community-based participatory research to develop an intervention to reduce HIV and STD infections among Latino men. AIDS Educ Prev. 2006;18(5):375–389. doi: 10.1521/aeap.2006.18.5.375. [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Hergenrather KC, Vissman AT, Stowers J, Davis AB, Hannah A, Marsiglia FF. Boys must be men, and men must have sex with women: A qualitative CBPR study to explore sexual risk among African American, Latino, and white gay men and MSM. American Journal of Men's Health. 2011;5(2):140–151. doi: 10.1177/1557988310366298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Malow RM, Jolly C. Community-based participatory research: a new and not-so-new approach to HIV/AIDS prevention, care, and treatment. AIDS Educ Prev. 2010;22(3):173–183. doi: 10.1521/aeap.2010.22.3.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, McCoy TP, Vissman AT, DiClemente RJ, Duck S, Hergenrather KC, Eng E. A randomized controlled trial of a culturally congruent intervention to increase condom use and HIV testing among heterosexually active immigrant Latino men. AIDS Behav. 2011;15(8):1764–1775. doi: 10.1007/s10461-011-9903-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles RR, Reyes JC, Colon HM, Sahai H, Marrero CA, Matos TD, Shepard EW. Effects of combined counseling and case management to reduce HIV risk behaviors among Hispanic drug injectors in Puerto Rico: a randomized controlled study. J Subst Abuse Treat. 2004;27(2):145–152. doi: 10.1016/j.jsat.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Shumaker SA, Hill DR. Gender differences in social support and physical health. Health Psychol. 1991;10(2):102–111. doi: 10.1037//0278-6133.10.2.102. [DOI] [PubMed] [Google Scholar]
- Treadwell HM, Ro M. Poverty, race, and the invisible men. Am J Public Health. 2003;93(5):705–707. doi: 10.2105/ajph.93.5.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viswanathan M, Kraschnewski JL, Nishikawa B, Morgan LC, Honeycutt AA, Thieda P, Jonas DE. Outcomes and costs of community health worker interventions: a systematic review. Med Care. 2010;48(9):792–808. doi: 10.1097/MLR.0b013e3181e35b51. [DOI] [PubMed] [Google Scholar]
- Wallerstein N, Oetzel J, Duran B, Tafoya G, Belone L, Rae R. What predicts outcomes in CBPR? In: Minkler M, Wallerstein N, editors. Community-Based Participatory Research: From Process to Outcomes. San Francisco, CA: Wiley; 2008. pp. 371–392. [Google Scholar]
- Wang K, Brown K, Shen SY, Tucker J. Social network-based interventions to promote condom use: a systematic review. AIDS Behav. 2011;15(7):1298–1308. doi: 10.1007/s10461-011-0020-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med. 2002;22(4):267–284. doi: 10.1016/s0749-3797(02)00415-4. [DOI] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ, Villamizar K, Er DL, DeVarona M, Taveras J, Jean R. Efficacy of a health educator-delivered HIV prevention intervention for Latina women: a randomized controlled trial. Am J Public Health. 2011;101(12):2245–2252. doi: 10.2105/AJPH.2011.300340. [DOI] [PMC free article] [PubMed] [Google Scholar]