Abstract
It is well known that cancer is one of the main causes of mortality in the aged population. Recent studies suggest that oncogenic pathways, such as the insulin-like growth factor-1 (IGF-I), Ras, and Akt/PKB, can contribute to both aging and cancer not only by promoting growth and preventing apoptosis, but also by promoting DNA damage and genomic instability. Epidemiological studies suggest that the chronic, low-grade inflammation that accompanies aging also contributes to tissue damage and tumor progression. Coupled with the accumulation of senescent cells and declining immune function, this leads to the generation and survival of cancer cells, possibly explaining why advanced age is the primary risk factor for cancer.
Keywords: aging, cancer, inflammation, immunosenescence, hematopoietic stem cells
I. INTRODUCTION
Cancer is one of the most common causes of morbidity and mortality in the elderly population. The progressive increase in the incidence of many malignant neoplasms with age makes aging the number one risk factor for cancer.1–3 In fact, 50% of new cancers and more than 60% of cancer deaths occur in individuals older than 65.4 The strong association between aging and cancer is also highlighted by the fact that mouse models of lifespan extension have delayed/reduced cancer incidence,5–8 and humans with growth hormone receptor deficiency (GHRD) have a normal lifespan and exhibit reduced cancer incidence.9 This suggests that aging at both the intracellular and tissue levels are key factors leading to cancer cell generation and survival and to the establishment of a tumor mass. Although advanced age is a potent cancer risk factor,10 this relationship is not straightforward because epidemiological studies show that cancer rates increase up to age 90 but plateau thereafter.11 In fact, cancer accounts for 40% of all deaths between ages 40 and 70 but for only 4 % of those amongst centenarians.12 Accordingly, autopsies on Japanese and Italian centenarians have shown that mortality due to cancer is much lower than expected.13,14
Several theories have been proposed to explain the possible link between aging and cancer, ranging from mutation accumulation and activation of oncogenic pathways to senescence and immunological aging. Here, we review various aspects of the aging-cancer relationship and attempt to summarize current knowledge in the field.
II. CONSERVED PRO-GROWTH SIGNALING PATHWAYS
Accumulation of genomic damage due to a lifetime exposure to carcinogens resulting in neoplastic transformation has been demonstrated during aging of mammalian cells.10 However, the contribution of prolonged exposure to carcinogens and of uninduced age-related intracellular errors and damage to carcinogenesis is debated.15–19 Moreover, cancer incidence increases rapidly after middle age whether in an 18 month old mouse, a 20 year old monkey, or a 40 year old human, suggesting that carcinogenesis is not associated with chronological periods but with both the aging rate and aging state of an organism. In fact, mutations that delay aging in most cases also reduce or delay cancer incidence.20–23 Not surprisingly, the signaling pathways that regulate aging also affect genomic integrity, DNA repair, and cellular apoptosis, which may explain part of their effect on cancer. Studies in yeast, worms, flies, and mice suggest that these pro-aging pathways are also those activated by nutrients to promote cellular growth and division indicating that cancer and other age-related diseases can be partially prevented or postponed by switching from a growth to a maintenance mode.24 For example, in yeast, lifespan-extending mutations in genes such as SCH9, the homolog of mammalian S6K, protect against both age- and oxidative stress-dependent genomic instability,25–27 and the C. elegans daf-2 longevity mutations prevent tumorigenesis by triggering apoptosis through stress resistance transcription factor daf-16. The transcriptional targets of daf-16 include genes that influence p53-dependent apoptosis.28
Activating mutations in Ras and Akt/PKB, two of the downstream mediators of IGF-I, and mutations in the IGF-I receptor itself are among those most frequently detected in human cancers.29,30 This is in agreement with a potential role for the IGF-I signaling pathway in promoting age-dependent mutations that lead to the generation of oncogenes and for oncogenes in exacerbating the generation of additional mutations and changes required for cancer progression.24 As inhibitors of apoptosis, these oncogenes are thought to promote cancer by allowing mutated cells to survive and proliferate.30 In addition to promoting the survival of damaged cells, these oncogenes could also actively promote DNA damage in both dividing and nondividing cells. In fact, S. cerevisiae, homologs of mammalian TOR, RAS, AKT, and PKA, promote an age-dependent increase in DNA mutations by elevating superoxide production and increasing DNA damage independently of cell growth.25,27 ROS-dependent DNA damage is possibly a major mediator of age-dependent mutations and cancer in many organisms.24 In support of the conserved effect of certain ROS in DNA damage and cancer, S. cerevisiae lacking the free radical scavengers superoxide dismutases 1 and 2 (SOD1 and SOD2) have a high frequency of mutations,27,31 and similarly increased cancers have been observed in mice lacking SOD1 or SOD2.32,33 Thus IGF-I, and the downstream Ras, Akt/PKB, Tor-S6K, etc. could promote tumorigenesis by increasing oxidative stress in part by decreasing protective enzymes that scavenge ROS.
Reduced growth hormone/insulin-like growth factor 1 (GH/ IGF-I) signaling in mice extends their lifespan and delays/reduces the incidence of age-related pathologies.5,7,8,34 Fibroblasts from the long-lived Ames and Snell dwarf mouse models and the GH receptor knockout models are resistant to hydrogen peroxide and UV light in vitro, thus suggesting that pro-growth pathways negatively regulate resistance to oxidative stress. Hepatocytes from Ames dwarf mice also readily undergo apoptosis compared with wild-type cells following oxidative stress.35 Humans with GHRD have very low IGF-I levels and are protected from cancers even though they have a normal lifespan.9 Mammary epithelial cells incubated with serum from these individuals are protected from DNA damage caused by hydrogen peroxide compared with those incubated with serum from unaffected relatives.9 GHRD serum also promotes apoptosis and cell death, an effect that is reversed by IGF-I.9 These studies are consistent with a role for IGF-I in promoting ROS-dependent DNA damage as well as in promoting survival of damaged, precancerous cells.
III. INFLAMMATION, AGING, AND CANCER
Aging is characterized by an increase in the levels of pro-inflammatory markers, resulting in a state of chronic inflammation or “inflamm-aging.”36 Low-grade, chronic inflammation increases with age and is associated with all-cause mortality risk in older adults.37 Epidemiological studies suggest a strong association between aging, chronic inflammation, and various cancers.38,39 In fact, about 15% of cancers are attributable to infectious agents that are associated with a high degree of inflammation,40 suggesting that the age-dependent inflammation may also play a key role in malignancies of unknown etiology. As mentioned in the previous section, the presence of ROS at the site of inflammation can lead to oxidative damage of DNA resulting in tumorigenesis and cancer progression.24 In the presence of a high level of inflammatory components, transformed cells are able to escape cell death/repair mechanisms and continue to grow and proliferate,38 possibly, as discussed above, due to the activation of anti-apoptotic pathways.
The microenvironment of a developing neoplasm is primarily hypoxic and characterized by the presence of a vast leukocyte population including neutrophils, dendritic cells, macrophages, eosinophils, and mast cells, as well as lymphocytes.41 All of these cells are capable of producing an array of growth factors, cytokines, ROS, MMPs, and soluble mediators of cytotoxicity, such as TNF-α, interleukins, and interferons.38,39 Leukocytes and other phagocytic cells can induce DNA damage, by the production of ROS and reactive nitrogen species. Thus, repeated tissue damage associated with chronic inflammation can result in permanent genomic alterations. Tumor associated macrophages (TAMs) are an essential component of the tumor microenvironment and when activated by IL-2, IL-12, and interferons, can kill tumor cells.42,43 However, they can also produce growth factors and angiogenic agents that stimulate tumor cell proliferation.44 TAMs also produce IL-10 which prevents the killing of cancer cells by cytotoxic T cells. Immature dendritic cells that are derived from macrophages can migrate to the lymph nodes and stimulate T lymphocyte activation. However, due to their immaturity, they are frequently defective in this stimulatory capacity.38 Chemokine production by tumor cells is not only used to recruit inflammatory cells but also to regulate their growth and proliferation. Of the various chemokines produced by cancer cells some have been linked to aging such as IL-6, TNFa, COX2, and IL-10.39
IL-6 serum concentrations have been reported to increase with age,45,46 and IL-6 can act as a growth factor for many cell types. Activation of STAT3 by IL-6 is associated with inhibition of apoptosis, increased cell cycle gene expression, and activation of androgen receptor genes.47 Overproduction of IL-6 by tumors can result in increased growth and metastasis owing to its role as a growth and anti-apoptotic factor48 and high IL-6 levels are associated with an adverse prognosis in cancers.49,50 The pro-inflammatory cytokine TNFα also increases with age51 and when chronically produced, can act as an endogenous tumor promoter. High levels of TNFα are detected in many cancers including breast, ovary, prostate, bladder, etc.,52,53 where mRNA and protein expression correlate with the grade of malignancy.
The pro-inflammatory activity of cyclooxygenase, COX, may also play an important role in the aging process and cancer.54 The induction of NFkB by cellular ROS increases the expression of COX-2, the inducible form of COX, which can, in turn, further increase inflammation and cause tissue damage.54 Notably, the pro-inflammatory alleles of COX-2 are under-represented in centenarians.39 Several studies have shown that the pro-inflammatory alleles of COX-2 are associated with cancer.55–57 COX-2 can promote cell proliferation and angiogenesis while inhibiting apoptosis through the production of prostaglandins, thus contributing to cancer progression.39,58 Use of nonsteroidal anti-inflammatory drugs, NSAIDs, that inhibit COX-2 are associated with a reduced risk of malignancies.59
IL-10 is known to play an important role in limiting and eventually terminating inflammatory responses by inhibiting cytokine production by T and NK cells.60,61 Centenarians, who have escaped cancers and show no signs of inflamm-aging express high levels of IL-10, which could be responsible for counteracting the effects of pro-inflammatory molecules.62,63 However, the role of IL-10 in cancer and tumor progression appears to be contradictory. Tumors from cancer patients have higher IL-10 levels compared with normal tissue from controls64 and increased IL-10 expression is also seen in metastatic rather than nonmetastatic tumors suggesting that IL-10 may also contribute to cancer metastases65 in contrast to its anti-angiogenic properties which may deter cancer.66
IV. IMMUNOSENESCENCE
An age-related decline in immune function is related to the onset of many diseases such as cancer, diabetes, cardiovascular, and infectious diseases. A young immune system can prevent cancer by protecting from virus-induced tumors and destroying precancerous cells but also by promptly reducing inflammation once the infectious threat has been eliminated.67 Immunosenescence primarily affects the adaptive immune system and results in a decline in B cell as well as CD4 and CD 8 T cells with a relative increase in NK cells such that the relative lymphocyte count does not change with aging.68 The most noticeable changes to adaptive immunity with aging occur in the T cells and are possibly associated with increased susceptibility to infections, autoimmune disorders, cancers, and chronic inflammatory diseases.69 Although there is no change in total lymphocyte number, there is a dramatic change in the representation of different types of lymphocytes.70
Due to involution of the thymus with age, the naïve T cell population progressively declines and there is an increase in memory T cells.71 Because a diverse repertoire of naïve T cells is required for mounting an immune response to new antigens, this decrease in the naïve T cell population is thought to contribute to the increased susceptibility to infections in elderly individuals.72 Moreover, with aging, there is a progressive increase in clonally expanded populations of CD8 T cells, due to accumulating antigen exposure, both in mice and humans,73,74 resulting in an altered naïve to memory cell ratio. Qualitatively, changes are seen in the CD8 or cytotoxic T lymphocyte population with more cells exhibiting features of replicative senescence.75 CD8 T cells that have undergone replicative senescence also show a permanent suppression of the co-stimulatory molecule CD28 both in vitro and in vivo.76 This co-stimulatory receptor is involved in a variety of T cell functions including activation, proliferation, stabilization of cytokine messenger RNA levels, and glucose metabolism.77In vivo, it has been shown that elderly individuals have a large proportion of CD8 T cells that do not express CD28,76 which is used as a biomarker to assess replicative senescence of T cells in vivo. Studies suggest that an increased proportion of CD8+CD28- T cells is associated with poor antibody responses to influenza vaccination,78 and seropositivity for CMV.68,79 Chronic exposure to the CMV, EBV, and VZV viruses results in clonal expansion and accumulation of CD8 cells that are specific to these viruses.68 In longitudinal studies, chronic CMV infection has been associated with the “immune risk phenotype,” which is characterized by an inverted CD4/CD8 ratio due to accumulation of CD8+CD28- cells and is associated with a poor response to T cell mitogens.80–83 This inverted CD4/CD8 ratio is absent in centenarians and can serve as a predictor for survival.84
A simplified view of immune surveillance suggests that the innate immune system attacks cancer cells by recognizing modified self-antigens and triggers an inflammatory cascade resulting in cancer cell death. It is becoming increasingly clear from mouse models that innate immune responses act as a first line of defense against tumors.85,86 The role of IFN-γ in this process was demonstrated using tumor transplantation in mice treated with neutralizing monoclonal antibodies specific for IFN-γ.85 Mice lacking perforin, an essential component of T cells and NK cells, develop more tumors compared to control mice.87 More recently, it was shown that mice deficient in RAG-2, completely lacking natural killer T (NKT), T, and B cells due to a failure to rearrange lymphocyte antigen receptors, developed sarcomas much more rapidly and frequently after MCA injection compared to controls.88
An opposing view suggests that immune response to tumor cells may be pro-tumorigenic and potentiate the growth of the tumor rather than preventing it.89 Thus the immune system may both prevent and facilitate carcinogenesis and the final outcome of the disease may depend on complex scenarios.90 As described above, with age, there is an accumulation of senescent T cells, which, together with age-related thymic involution, limits the naïve T cell repertoire, resulting in diminished immune surveillance capacity.91 Moreover, chronic exposure to antigenic stimulation may result in “immune exhaustion” which may also lead to defective anti-tumor activity with aging. For example, spontaneous tumors are likely to have co-existed with immune defense systems over extended periods of time and to have interacted chronically with anti-tumor T cells which may render them unrecognizable as antigens.91,92 This is in agreement with what is observed in mice and humans where a significant expansion of CD8 cells and low CD4/CD8 ratio is associated with persistent infections.80–83
Several cancers are associated with higher proportion of senescent T cells and a poorer outcome including lung, colorectal, ovarian, lymphoma, and breast.93–97 It is also known that CD8+/CD28- cells can accumulate in elderly individuals,76 and may repress antigen-specific CTL responses. Studies have also shown an increase in frequency of the regulatory CD4 T cell subset (CD4+CD25hi or CD4+Foxp3+) in older individuals, which may or may not contribute to age-related decline in suppressive activity.98
V. CELLULAR SENESCENCE AND CANCER
Senescence is the irreversible arrest of cell proliferation in response to potentially oncogenic stimuli.99,100 This process is known to be regulated by two major tumor suppressor pathways—the p53/p21 and the p16INK4a/pRB.99 Senescent cells accumulate over the lifespan in mice, nonhuman primates, and humans, indicating that senescence may serve as a barrier to the development of cancer. Consistent with this idea, senescent cells have been found in preneoplastic lesions in human tissues.101 One of the major causes of senescence is a gradual shortening of telomeres with each replicative cycle accompanied by limited expression of the enzyme telomerase, which is responsible for telomere elongation to reduce the amount of chromosomal DNA loss during each cell division cycle;102 These two factors result in critical telomeres shortening and irreversible cellular senescence. Dysfunctional telomeres elicit a DNA damage response, where the chromosomal ends are perceived as double strand breaks (DSBs). The DNA damage response activates cell division arrest via activation of p53.99,103 Senescence can also be induced in response to DNA damage such as that caused by oxidative stress, activating a DDR response.104 Other stress signaling such as oncogenic Ras activation (H-RasV12), cytokine signaling, or loss of PTEN can also trigger senescence.99,105,106
In addition to being growth arrested, senescent cells exhibit other characteristic properties, such as the expression of senescenceassociated B-gal (SABgal), vacuolization, and resistance to apoptosis.100 These cells also exhibit the SASP or senescence associated secretory phenotype and secrete many pro-inflammatory cytokines, chemokines, growth factors, and proteases.99 Despite the blocking of tumorigenesis in the senescent cell itself, the process of cellular senescence may actually contribute to cancer. Indeed, there is evidence that senescent cells can promote cancer in mice and stimulate malignant phenotypes in culture. Injection of senescent fibroblasts significantly stimulated the proliferation of mouse and human epithelial tumor cells in immunocompromised mice.99,107–109 Several SASP components such as the MMP's, VEGF, interleukins, etc., have been implicated in this process.108,109 Therefore, cellular senescence can be both anti- and pro-tumor growth. As these cells accumulate with age, they can, by virtue of the SASP, create a microenvironment that favors cancer progression. SASP-induced inflammation can generate ROS that can cause DNA damage.99
VI. HEMATOPOIETIC STEM CELL AGING
Aging of the hematopoietic system is associated with increased myeloid malignancies, anemia, and immune dysfunction.110,111 As with other cancers, the incidence of certain hematopoietic malignancies increases with age.112 As only a small reserve of hematopoietic stem cells sustains the entire blood system throughout life, it is possible that a functional decline in the HSC population with age is responsible for these myeloproliferative disorders. Whole BM and competitive transplantation studies in mice suggest that while the per-cell activity of HSC's decreases with age, the functional output is preserved due to an overall increase in HSC numbers. Whole BM from old donor mice was superior in reconstituting the erythroid compartment of irradiated or unconditioned recipient mice compared to BM from young mice.113–115 Measurement of HSC frequencies in BM from old vs young C57BL/6 mice showed an approximately twofold increase in HSC number in old mice.116,117 Measurement of enriched HSC fractions using cell surface markers to distinguish true HSC's from multipotent progenitors (MPPs) suggests HSC frequencies that are between 6- to 17-fold higher in older mice.118,119 However, the higher number of HSCs not only does not translate in a more effective immune system but is likely to be a central culprit in the immunosenescence described earlier. In fact, competitive transplantation experiments using purified HSC's have shown that HSC function on a per-cell basis is substantially reduced in old mice.120
Studies have shown that lymphopoiesis declines with age in mice and humans.110,121 On the other hand, there is no decrease in myeloid potential, which may even increase with age,122 resulting in a skewing of the lineage potential from lymphopoiesis to myelopoiesis. Transplantation experiments in mice have shown that this myeloid bias is maintained even in young recipients transplanted with old bone marrow cells,123 and xenotransplantation in immunodeficient mice shows that the bias also exists in aged humans.124 There is a marked decline in lymphoid function in the elderly and the overproduction of myeloid cells leads to a pro-inflammatory environment.125 Expression profiling of HSCs confirmed the downregulation of lymphoid specification genes and upregulation of myeloid specification genes in old mice123 and humans.124
VII. CONCLUSION
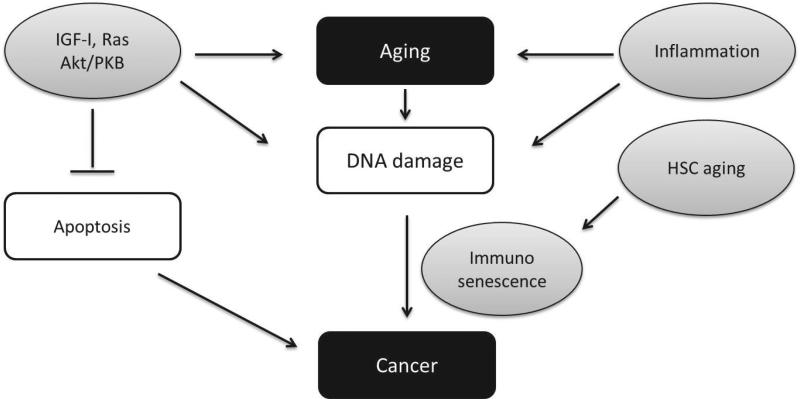
The picture that emerges from the preceding sections is that the multiple factors that contribute to aging also actively or passively promote cancer. As the individual ages, the complex interplay between these systems increases the likelihood of carcinogen-esis. Several of these aging processes confer an early life advantage in terms of growth, reproduction, and survival but are deleterious later in life, a concept known as “antagonistic pleiotropy.” For example, the Ras, Akt/PKB, and TOR pathways promote growth and reproduction and can block apoptosis but also contribute to DNA mutagenesis and the ineffective killing of mutated cells (Fig. 1). Also, the strong immunological response to pathogens early in life is protective but may contribute to the damage of cells and tissues which may promote the development of cancer later in life (Fig. 1.).
FIGURE 1.
Aging, growth factor signaling, immunosenescence, and cancer. Based on data from different model systems, IGF-I and downstream signaling proteins Ras and Akt/PKB as well as chronic inflammation can promote aging and DNA damage thus promoting cancer. The anti-apoptotic activity of IGF-I, Ras, and Akt/PKB prevents the elimination of mutated/damaged cells, further promoting tumorigenesis. Aging of the hematopoietic stem cell system and immunosenescence can provide a favorable environment for the propagation of malignant cells.
Because of immunosenescence but also the aging of the hematopoietic system, elderly patients often experience elevated immunosuppression and have a greater risk of chemotherapy-related death than younger patients, which can limit the dose and frequency of treatments.4,126,127 Development of novel strategies and drugs aimed at selective host/patient protection could reduce the side effects associated with a variety of treatments and also increase the efficacy of the therapy. Studies from long-lived mice and humans have shown that they exhibit delayed/ reduced cancers indicating that it is possible to identify strategies that can delay aging and protect from cancers and other age-related diseases. These strategies may also be useful in enhancing existing cancer treatments in the elderly. We and others have recently shown that fasting or short-term starvation (STS) reduces circulating IGF-I levels by 70% in mice and protects normal but not cancer cells from toxic chemotherapy drugs.128–131 As proto-oncogenes are negative regulators of the protective changes induced by fasting, the great majority of cancer cells do not respond to fasting/STS, thus promoting the differential protection (differential stress resistance) of normal cells. Preliminary studies indicate that fasting is feasible and safe in humans and could protect patients from chemotherapy.132 Although additional clinical testing is necessary, fasting and other similar strategies have the potential to be used in enhancing current treatments in the elderly.
ABBREVIATIONS
- GH
growth hormone
- GHRD
growth hormone receptor deficiency
- IGF-I
insulin-like growth factor 1
- SASP
senescence associated secretory phenotype
- ROS
reactive oxygen species
- MMP
matrix metallo proteinase
- IL
interleukin
- TAM
tumor associated macrophage
- TNF
tumor necrosis factor
- COX
cyclooxygenase
- NK
natural killer
- STS
short term starvation
- DSR
differential stress resistance
- MCA
3-methylcholanthrene
- HSC
hematopoietic stem cells
REFERENCES
- 1.Cutler RG, Mattson MP. The adversities of aging. Ageing Res Rev. 2006;5(3):221–38. doi: 10.1016/j.arr.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 2.Parkin DM, Bray FI, Devesa SS. Cancer burden in the year 2000. The global picture. Eur J Cancer. 2001;37(Suppl 8):S4–66. doi: 10.1016/s0959-8049(01)00267-2. [DOI] [PubMed] [Google Scholar]
- 3.Peto J. Cancer epidemiology in the last century and the next decade. Nature. 2001;411(6835):390–5. doi: 10.1038/35077256. [DOI] [PubMed] [Google Scholar]
- 4.Wedding U, Pientka L, Hoffken K. Quality-of-life in elderly patients with cancer: a short review. Eur J Cancer. 2007;43(15):2203–10. doi: 10.1016/j.ejca.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Coschigano KT, Holland AN, Riders ME, List EO, Flyvbjerg A, Kopchick JJ. Deletion, but not antagonism, of the mouse growth hormone receptor results in severely decreased body weights, insulin, and insulin-like growth factor I levels and increased life span. Endocrinology. 2003;144(9):3799–810. doi: 10.1210/en.2003-0374. [DOI] [PubMed] [Google Scholar]
- 6.Holzenberger M, Dupont J, Ducos B, Leneuve P, Geloen A, Even PC, Cervera P, Le Bouc Y. IGF-1 receptor regulates lifespan and resistance to oxidative stress in mice. Nature. 2003;421(6919):182–7. doi: 10.1038/nature01298. [DOI] [PubMed] [Google Scholar]
- 7.Ikeno Y, Bronson RT, Hubbard GB, Lee S, Bartke A. Delayed occurrence of fatal neoplastic diseases in ames dwarf mice: correlation to extended longevity. J Gerontol A Biol Sci Med Sci. 2003;58(4):291–6. doi: 10.1093/gerona/58.4.b291. [DOI] [PubMed] [Google Scholar]
- 8.Brown-Borg HM, Borg KE, Meliska CJ, Bartke A. Dwarf mice and the ageing process. Nature. 1996;384(6604):33. doi: 10.1038/384033a0. [DOI] [PubMed] [Google Scholar]
- 9.Guevara-Aguirre J, Balasubramanian P, Guevara-Aguirre M, Wei M, Madia F, Cheng CW, Hwang D, Martin-Montalvo A, Saavedra J, Ingles S, de Cabo R, Cohen P, Longo VD. Growth hormone receptor deficiency is associated with a major reduction in pro-aging signaling, cancer, and diabetes in humans. Sci Transl Med. 2011;3(70):70ra13. doi: 10.1126/scitranslmed.3001845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DePinho RA. The age of cancer. Nature. 2000;408(6809):248–54. doi: 10.1038/35041694. [DOI] [PubMed] [Google Scholar]
- 11.Yancik R, Ries LA. Cancer in older persons: an international issue in an aging world. Semin Oncol. 2004;31(2):128–36. doi: 10.1053/j.seminoncol.2003.12.024. [DOI] [PubMed] [Google Scholar]
- 12.Bonafe M, Barbi C, Storci G, Salvioli S, Capri M, Olivieri F, Valensin S, Monti D, Gonos ES, De Benedictis G, Franceschi C. What studies on human longevity tell us about the risk for cancer in the oldest old: data and hypotheses on the genetics and immunology of centenarians. Exp Gerontol. 2002;37(10-11):1263–71. doi: 10.1016/s0531-5565(02)00137-7. [DOI] [PubMed] [Google Scholar]
- 13.Franceschi C, Motta L, Motta M, Malaguarnera M, Capri M, Vasto S, Candore G, Caruso C. The extreme longevity: the state of the art in Italy. Exp Gerontol. 2008;43(2):45–52. doi: 10.1016/j.exger.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 14.Miyaishi O, Ando F, Matsuzawa K, Kanawa R, Isobe K. Cancer incidence in old age. Mech Ageing Dev. 2000;117(1-3):47–55. doi: 10.1016/s0047-6374(00)00136-6. [DOI] [PubMed] [Google Scholar]
- 15.Anisimov VN. [Life span and tumor incidence in animals of various species]. Eksperimental'naia onkologiia. Prodolzhitel'nost'zhizni i chastota vozniknoveniia opukholei u zhivotnykh raznykh vidov. 1987;9(5):17–23. 60. [PubMed] [Google Scholar]
- 16.Anisimov VN. Biology of aging and cancer. Cancer Control. 2007;14(1):23–31. doi: 10.1177/107327480701400104. [DOI] [PubMed] [Google Scholar]
- 17.Miller RA. Gerontology as oncology. Research on aging as the key to the understanding of cancer. Cancer. 1991;68(11 Suppl):2496–501. doi: 10.1002/1097-0142(19911201)68:11+<2496::aid-cncr2820681503>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 18.Peto R, Parish SE, Gray RG. There is no such thing as ageing, and cancer is not related to it. IARC Sci Publ. 1985;(58):43–53. [PubMed] [Google Scholar]
- 19.Peto R, Roe FJ, Lee PN, Levy L, Clack J. Cancer and ageing in mice and men. Br J Cancer. 1975;32(4):411–26. doi: 10.1038/bjc.1975.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Campisi J, Vijg J. Does damage to DNA and other macromolecules play a role in aging? If so, how? J Gerontol A Biol Sci Med Sci. 2009;64(2):175–8. doi: 10.1093/gerona/gln065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fontana L, Partridge L, Longo VD. Extending healthy life span—from yeast to humans. Science. 2010;328(5976):321–6. doi: 10.1126/science.1172539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Longo VD, Finch CE. Evolutionary medicine: from dwarf model systems to healthy centenarians? Science. 2003;299(5611):1342–6. doi: 10.1126/science.1077991. [DOI] [PubMed] [Google Scholar]
- 23.Maslov AY, Vijg J. Genome instability, cancer and aging. Biochim Biophys Acta. 2009;1790(10):963–9. doi: 10.1016/j.bbagen.2009.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Longo VD, Lieber MR, Vijg J. Turning anti-ageing genes against cancer. Nat RevMol Cell Biol. 2008;9(11):903–10. doi: 10.1038/nrm2526. [DOI] [PubMed] [Google Scholar]
- 25.Fabrizio P, Gattazzo C, Battistella L, Wei M, Cheng C, McGrew K, Longo VD. Sir2 blocks extreme life-span extension. Cell. 2005;123(4):655–67. doi: 10.1016/j.cell.2005.08.042. [DOI] [PubMed] [Google Scholar]
- 26.Madia F, Gattazzo C, Wei M, Fabrizio P, Burhans WC, Weinberger M, Galbani A, Smith JR, Nguyen C, Huey S, Comai L, Longo VD. Longevity mutation in SCH9 prevents recombination errors and premature genomic instability in a Werner/Bloom model system. J Cell Biol. 2008;180(1):67–81. doi: 10.1083/jcb.200707154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Madia F, Wei M, Yuan V, Hu J, Gattazzo C, Pham P, Goodman MF, Longo VD. Oncogene homologue Sch9 promotes age-dependent mutations by a super-oxide and Rev1/Polzeta-dependent mechanism. J Cell Biol. 2009;186(4):509–23. doi: 10.1083/jcb.200906011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pinkston-Gosse J, Kenyon C. DAF-16/FOXO targets genes that regulate tumor growth in Caenorhabditis elegans. Nat Genet. 2007;39(11):1403–9. doi: 10.1038/ng.2007.1. [DOI] [PubMed] [Google Scholar]
- 29.Rodriguez-Viciana P, Tetsu O, Oda K, Okada J, Rauen K, McCormick F. Cancer targets in the Ras pathway. Cold Spring Harbor Symp Quant Biol. 2005;70:461–7. doi: 10.1101/sqb.2005.70.044. [DOI] [PubMed] [Google Scholar]
- 30.Toker A, Yoeli-Lerner M. Akt signaling and cancer: surviving but not moving on. Cancer Res. 2006;66(8):3963–6. doi: 10.1158/0008-5472.CAN-06-0743. [DOI] [PubMed] [Google Scholar]
- 31.Fabrizio P, Battistella L, Vardavas R, Gattazzo C, Liou LL, Diaspro A, Dossen JW, Gralla EB, Longo VD. Superoxide is a mediator of an altruistic aging program in Saccharomyces cerevisiae. J Cell Biol. 2004;166(7):1055–67. doi: 10.1083/jcb.200404002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Busuttil RA, Garcia AM, Cabrera C, Rodriguez A, Suh Y, Kim WH, Huang TT, Vijg J. Organ-specific increase in mutation accumulation and apoptosis rate in CuZn-superoxide dismutase-deficient mice. Cancer Res. 2005;65(24):11271–5. doi: 10.1158/0008-5472.CAN-05-2980. [DOI] [PubMed] [Google Scholar]
- 33.Van Remmen H, Ikeno Y, Hamilton M, Pahlavani M, Wolf N, Thorpe SR, Alderson NL, Baynes JW, Epstein CJ, Huang TT, Nelson J, Strong R, Richardson A. Life-long reduction in MnSOD activity results in increased DNA damage and higher incidence of cancer but does not accelerate aging. Physiol Genomics. 2003;16(1):29–37. doi: 10.1152/physiolgenomics.00122.2003. [DOI] [PubMed] [Google Scholar]
- 34.Flurkey K, Papaconstantinou J, Miller RA, Harrison DE. Lifespan extension and delayed immune and collagen aging in mutant mice with defects in growth hormone production. Proc Natl Acad Sci U S A. 2001;98(12):6736–41. doi: 10.1073/pnas.111158898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kennedy MA, Rakoczy SG, Brown-Borg HM. Long-living Ames dwarf mouse hepatocytes readily undergo apoptosis. Exp Gerontol. 2003;38(9):997–1008. doi: 10.1016/s0531-5565(03)00164-5. [DOI] [PubMed] [Google Scholar]
- 36.Franceschi C, Bonafe M, Valensin S, Olivieri F, De Luca M, Ottaviani E, De Benedictis G. Inflamm-aging. An evolutionary perspective on immunosenescence. Ann N Y Acad Sci. 2000;908:244–54. doi: 10.1111/j.1749-6632.2000.tb06651.x. [DOI] [PubMed] [Google Scholar]
- 37.Bruunsgaard H, Pedersen M, Pedersen BK. Aging and proinflammatory cytokines. Curr Opin Hematol. 2001;8(3):131–6. doi: 10.1097/00062752-200105000-00001. [DOI] [PubMed] [Google Scholar]
- 38.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–7. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vasto S, Carruba G, Lio D, Colonna-Romano G, Di Bona D, Candore G, Caruso C. Inflammation, ageing and cancer. Mech Ageing Dev. 2009;130(1-2):40–5. doi: 10.1016/j.mad.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 40.Parkin DM, Pisani P, Ferlay J. Global cancer statistics. CA: Cancer J Clin. 1999;49(1):33–64. doi: 10.3322/canjclin.49.1.33. [DOI] [PubMed] [Google Scholar]
- 41.Allavena P, Garlanda C, Borrello MG, Sica A, Mantovani A. Pathways connecting inflammation and cancer. Curr Opin Genet Dev. 2008;18(1):3–10. doi: 10.1016/j.gde.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 42.Brigati C, Noonan DM, Albini A, Benelli R. Tumors and inflammatory infiltrates: friends or foes? Clin Exp Metastasis. 2002;19(3):247–58. doi: 10.1023/a:1015587423262. [DOI] [PubMed] [Google Scholar]
- 43.Tsung K, Dolan JP, Tsung YL, Norton JA. Macrophages as effector cells in interleukin 12-induced T cell-dependent tumor rejection. Cancer Res. 2002;62(17):5069–75. [PubMed] [Google Scholar]
- 44.Mantovani A, Bottazzi B, Colotta F, Sozzani S, Ruco L. The origin and function of tumor-associated macrophages. Immunol Today. 1992;13(7):265–70. doi: 10.1016/0167-5699(92)90008-U. [DOI] [PubMed] [Google Scholar]
- 45.Ershler WB, Sun WH, Binkley N, Gravenstein S, Volk MJ, Kamoske G, Klopp RG, Roecker EB, Daynes RA, Weindruch R. Interleukin-6 and aging: blood levels and mononuclear cell production increase with advancing age and in vitro production is modifiable by dietary restriction. Lymphokine Cytokine Res. 1993;12(4):225–30. [PubMed] [Google Scholar]
- 46.Wei J, Xu H, Davies JL, Hemmings GP. Increase of plasma IL-6 concentration with age in healthy subjects. Life Sci. 1992;51(25):1953–6. doi: 10.1016/0024-3205(92)90112-3. [DOI] [PubMed] [Google Scholar]
- 47.Maggio M, Guralnik JM, Longo DL, Ferrucci L. Interleukin-6 in aging and chronic disease: a magnificent pathway. J Gerontol A Biol Sci Med Sci. 2006;61(6):575–84. doi: 10.1093/gerona/61.6.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Culig Z, Steiner H, Bartsch G, Hobisch A. Interleukin-6 regulation of prostate cancer cell growth. J Cell Biochem. 2005;95(3):497–505. doi: 10.1002/jcb.20477. [DOI] [PubMed] [Google Scholar]
- 49.Belluco C, Olivieri F, Bonafe M, Giovagnetti S, Mammano E, Scalerta R, Ambrosi A, Franceschi C, Nitti D, Lise M. -174 G>C polymorphism of interleukin 6 gene promoter affects interleukin 6 serum level in patients with colorectal cancer. Clin Cancer Res. 2003;9(6):2173–6. [PubMed] [Google Scholar]
- 50.Hong DS, Angelo LS, Kurzrock R. Interleukin-6 and its receptor in cancer: implications for translational therapeutics. Cancer. 2007;110(9):1911–28. doi: 10.1002/cncr.22999. [DOI] [PubMed] [Google Scholar]
- 51.Fagiolo U, Cossarizza A, Scala E, Fanales-Belasio E, Ortolani C, Cozzi E, Monti D, Franceschi C, Paganelli R. Increased cytokine production in mononuclear cells of healthy elderly people. Eur J Immunol. 1993;23(9):2375–8. doi: 10.1002/eji.1830230950. [DOI] [PubMed] [Google Scholar]
- 52.Naylor MS, Stamp GW, Foulkes WD, Eccles D, Balkwill FR. Tumor necrosis factor and its receptors in human ovarian cancer. Potential role in disease progression. J Clin Invest. 1993;91(5):2194–206. doi: 10.1172/JCI116446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357(9255):539–45. doi: 10.1016/S0140-6736(00)04046-0. [DOI] [PubMed] [Google Scholar]
- 54.Chung HY, Cesari M, Anton S, Marzetti E, Giovannini S, Seo AY, Carter C, Yu BP, Leeuwenburgh C. Molecular inflammation: underpinnings of aging and age-related diseases. Ageing Res Rev. 2009;8(1):18–30. doi: 10.1016/j.arr.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hou L, Grillo P, Zhu ZZ, Lissowska J, Yeager M, Zatonski W, Zhu G, Baccarelli A, Chanock SJ, Fraumeni JF, Jr, Chow WH. COX1 and COX2 polymorphisms and gastric cancer risk in a Polish population. Anticancer Res. 2007;27(6C):4243–7. [PubMed] [Google Scholar]
- 56.Moons LM, Kuipers EJ, Rygiel AM, Groothuismink AZ, Geldof H, Bode WA, Krishnadath KK, Bergman JJ, van Vliet AH, Siersema PD, Kusters JG. COX-2 CA-haplotype is a risk factor for the development of esophageal adenocarcinoma. Am J Gastroenterol. 2007;102(11):2373–9. doi: 10.1111/j.1572-0241.2007.01373.x. [DOI] [PubMed] [Google Scholar]
- 57.Shen J, Gammon MD, Terry MB, Teitelbaum SL, Neugut AI, Santella RM. Genetic polymorphisms in the cyclooxygenase-2 gene, use of nonsteroidal anti-inflammatory drugs, and breast cancer risk. Breast Cancer Res. 2006;8(6):R71. doi: 10.1186/bcr1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fosslien E. Review: molecular pathology of cyclooxygenase-2 in cancer-induced angiogenesis. Ann Clin Lab Sci. 2001;31(4):325–48. [PubMed] [Google Scholar]
- 59.Thun MJ, Henley SJ, Patrono C. Nonsteroidal anti-inflammatory drugs as anticancer agents: mechanistic, pharmacologic, and clinical issues. J Natl Cancer Inst. 2002;94(4):252–66. doi: 10.1093/jnci/94.4.252. [DOI] [PubMed] [Google Scholar]
- 60.de Waal Malefyt R, Abrams J, Bennett B, Figdor CG, de Vries JE. Interleukin 10(IL-10) inhibits cytokine synthesis by human monocytes: an autoregulatory role of IL-10 produced by monocytes. J Exp Med. 1991;174(5):1209–20. doi: 10.1084/jem.174.5.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ding L, Shevach EM. IL-10 inhibits mitogen-induced T cell proliferation by selectively inhibiting macrophage costimulatory function. J Immunol. 1992;148(10):3133–9. [PubMed] [Google Scholar]
- 62.Lio D, Scola L, Crivello A, Colonna-Romano G, Candore G, Bonafe M, Cavallone L, Marchegiani F, Olivieri F, Franceschi C, Caruso C. Inflammation, genetics, and longevity: further studies on the protective effects in men of IL-10 -1082 promoter SNP and its interaction with TNF-alpha -308 promoter SNP. J Med Genet. 2003;40(4):296–9. doi: 10.1136/jmg.40.4.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Salvioli S, Capri M, Bucci L, Lanni C, Racchi M, Uberti D, Memo M, Mari D, Govoni S, Franceschi C. Why do centenarians escape or postpone cancer? The role of IGF-1, inflammation and p53. Cancer Immunol Immunother. 2009;58(12):1909–17. doi: 10.1007/s00262-008-0639-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Salazar-Onfray F, Lopez MN, Mendoza-Naranjo A. Paradoxical effects of cytokines in tumor immune surveillance and tumor immune escape. Cytokine Growth Factor Rev. 2007;18(1-2):171–82. doi: 10.1016/j.cytogfr.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 65.Dummer W, Becker JC, Schwaaf A, Leverkus M, Moll T, Brocker EB. Elevated serum levels of interleukin-10 in patients with metastatic malignant melanoma. Melanoma Res. 1995;5(1):67–8. doi: 10.1097/00008390-199502000-00008. [DOI] [PubMed] [Google Scholar]
- 66.Stearns ME, Rhim J, Wang M. Interleukin 10 (IL-10) inhibition of primary human prostate cell-induced angiogenesis: IL-10 stimulation of tissue inhibitor of metalloproteinase-1 and inhibition of matrix metalloproteinase (MMP)-2/MMP-9 secretion. Clin Cancer Res. 1999;5(1):189–96. [PubMed] [Google Scholar]
- 67.Swann JB, Smyth MJ. Immune surveillance of tumors. J Clin Invest. 2007;117(5):1137–46. doi: 10.1172/JCI31405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.McElhaney JE, Effros RB. Immunosenescence: what does it mean to health outcomes in older adults? Curr Opin Immunol. 2009;21(4):418–24. doi: 10.1016/j.coi.2009.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fulop T, Larbi A, Kotb R, de Angelis F, Pawelec G. Aging, immunity, and cancer. Discov Med. 2011;11(61):537–50. [PubMed] [Google Scholar]
- 70.Effros RB, Dagarag M, Spaulding C, Man J. The role of CD8+ T-cell replicative senescence in human aging. Immunol Rev. 2005;205:147–57. doi: 10.1111/j.0105-2896.2005.00259.x. [DOI] [PubMed] [Google Scholar]
- 71.Aspinall R, Andrew D. Thymic involution in aging. J Clin Immunol. 2000;20(4):250–6. doi: 10.1023/a:1006611518223. [DOI] [PubMed] [Google Scholar]
- 72.Nikolich-Zugich J, Slifka MK, Messaoudi I. The many important facets of T-cell repertoire diversity. Nat Rev Immunol. 2004;4(2):123–32. doi: 10.1038/nri1292. [DOI] [PubMed] [Google Scholar]
- 73.Callahan JE, Kappler JW, Marrack P. Unexpected expansions of CD8-bearing cells in old mice. J Immunol. 1993;151(12):6657–69. [PubMed] [Google Scholar]
- 74.Schwab R, Szabo P, Manavalan JS, Weksler ME, Posnett DN, Pannetier C, Kourilsky P, Even J. Expanded CD4+ and CD8+ T cell clones in elderly humans. J Immunol. 1997;158(9):4493–9. [PubMed] [Google Scholar]
- 75.Boucher N, Dufeu-Duchesne T, Vicaut E, Farge D, Effros RB, Schachter F. CD28 expression in T cell aging and human longevity. Exp Gerontol. 1998;33(3):267–82. doi: 10.1016/s0531-5565(97)00132-0. [DOI] [PubMed] [Google Scholar]
- 76.Effros RB, Boucher N, Porter V, Zhu X, Spaulding C, Walford RL, Kronenberg M, Cohen D, Schachter F. Decline in CD28+ T cells in centenarians and in long-term T cell cultures: a possible cause for both in vivo and in vitro immunosenescence. Exp Gerontol. 1994;29(6):601–9. doi: 10.1016/0531-5565(94)90073-6. [DOI] [PubMed] [Google Scholar]
- 77.Effros RB. Editorial: T cell memory, bone marrow, and aging: the good news. J Leukocyte Biol. 2012;91(2):185–7. doi: 10.1189/jlb.0811438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Goronzy JJ, Fulbright JW, Crowson CS, Poland GA, O'Fallon WM, Weyand CM. Value of immunological markers in predicting responsiveness to influenza vaccination in elderly individuals. J Virol. 2001;75(24):12182–7. doi: 10.1128/JVI.75.24.12182-12187.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Almanzar G, Schwaiger S, Jenewein B, Keller M, Herndler-Brandstetter D, Wurzner R, Schonitzer D, Grubeck-Loebenstein B. Long-term cytomegalovirus infection leads to significant changes in the composition of the CD8+ T-cell repertoire, which may be the basis for an imbalance in the cytokine production profile in elderly persons. J Virol. 2005;79(6):3675–83. doi: 10.1128/JVI.79.6.3675-3683.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hadrup SR, Strindhall J, Kollgaard T, Seremet T, Johansson B, Pawelec G, thor Straten P, Wikby A. Longitudinal studies of clonally expanded CD8 T cells reveal a repertoire shrinkage predicting mortality and an increased number of dysfunctional cytomegalovirus-specific T cells in the very elderly. J Immunol. 2006;176(4):2645–53. doi: 10.4049/jimmunol.176.4.2645. [DOI] [PubMed] [Google Scholar]
- 81.Olsson J, Wikby A, Johansson B, Lofgren S, Nilsson BO, Ferguson FG. Age-related change in peripheral blood T-lymphocyte subpopulations and cytomegalovirus infection in the very old: the Swedish longitudinal OCTO immune study. Mech Ageing Dev. 2000;121(1-3):187–201. doi: 10.1016/s0047-6374(00)00210-4. [DOI] [PubMed] [Google Scholar]
- 82.Wikby A, Johansson B, Olsson J, Lofgren S, Nilsson BO, Ferguson F. Expansions of peripheral blood CD8 T-lymphocyte subpopulations and an association with cytomegalovirus seropositivity in the elderly: the Swedish NONA immune study. Exp Gerontol. 2002;37(2-3):445–53. doi: 10.1016/s0531-5565(01)00212-1. [DOI] [PubMed] [Google Scholar]
- 83.Wikby A, Nilsson BO, Forsey R, Thompson J, Strindhall J, Lofgren S, Ernerudh J, Pawelec G, Ferguson F, Johansson B. The immune risk pheno-type is associated with IL-6 in the terminal decline stage: findings from the Swedish NONA immune longitudinal study of very late life functioning. Mech Ageing Dev. 2006;127(8):695–704. doi: 10.1016/j.mad.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 84.Strindhall J, Nilsson BO, Lofgren S, Ernerudh J, Pawelec G, Johansson B, Wikby A. No Immune Risk Profile among individuals who reach 100 years of age: findings from the Swedish NONA immune longitudinal study. Exp Gerontol. 2007;42(8):753–61. doi: 10.1016/j.exger.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 85.Dighe AS, Richards E, Old LJ, Schreiber RD. Enhanced in vivo growth and resistance to rejection of tumor cells expressing dominant negative IFN gamma receptors. Immunity. 1994;1(6):447–56. doi: 10.1016/1074-7613(94)90087-6. [DOI] [PubMed] [Google Scholar]
- 86.Dunn GP, Bruce AT, Ikeda H, Old LJ, Schreiber RD. Cancer immunoediting: from immunosurveillance to tumor escape. Nat Immunol. 2002;3(11):991–8. doi: 10.1038/ni1102-991. [DOI] [PubMed] [Google Scholar]
- 87.Street SE, Cretney E, Smyth MJ. Perforin and interferon-gamma activities independently control tumor initiation, growth, and metastasis. Blood. 2001;97(1):192–7. doi: 10.1182/blood.v97.1.192. [DOI] [PubMed] [Google Scholar]
- 88.Shankaran V, Ikeda H, Bruce AT, White JM, Swanson PE, Old LJ, Schreiber RD. IFNgamma and lymphocytes prevent primary tumour development and shape tumour immunogenicity. Nature. 2001;410(6832):1107–11. doi: 10.1038/35074122. [DOI] [PubMed] [Google Scholar]
- 89.Prehn RT, Prehn LM. The flip side of immune surveillance: immune dependency. Immunol Rev. 2008;222:341–56. doi: 10.1111/j.1600-065X.2008.00609.x. [DOI] [PubMed] [Google Scholar]
- 90.Zitvogel L, Tesniere A, Kroemer G. Cancer despite immunosurveillance: immunoselection and immunosubversion. Nat Rev Immunol. 2006;6(10):715–27. doi: 10.1038/nri1936. [DOI] [PubMed] [Google Scholar]
- 91.Chou JP, Effros RB. T cell replicative senescence in human aging. Curr Pharm Des. 2013;19(9):1680–98. doi: 10.2174/138161213805219711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pawelec G, Lustgarten J, Ruby C, Gravekamp C. Impact of aging on cancer immunity and immunotherapy. Cancer Immunol Immunother. 2009;58(12):1907–8. doi: 10.1007/s00262-009-0743-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gruber IV, El Yousfi S, Durr-Storzer S, Wallwiener D, Solomayer EF, Fehm T. Down-regulation of CD28, TCR-zeta (zeta) and up-regulation of FAS in peripheral cytotoxic T-cells of primary breast cancer patients. Anticancer Res. 2008;28(2A):779–84. [PubMed] [Google Scholar]
- 94.Meloni F, Morosini M, Solari N, Passadore I, Nascimbene C, Novo M, Ferrari M, Cosentino M, Marino F, Pozzi E, Fietta AM. Foxp3 expressing CD4+ CD25+ and CD8+CD28- T regulatory cells in the peripheral blood of patients with lung cancer and pleural mesothelioma. Human Immunol. 2006;67(1-2):1–12. doi: 10.1016/j.humimm.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 95.Urbaniak-Kujda D, Kapelko-Slowik K, Wolowiec D, Dybko J, Halon A, Jazwiec B, Maj J, Jankowska-Konsur A, Kuliczkowski K. Increased percentage of CD8+CD28- suppressor lymphocytes in peripheral blood and skin infiltrates correlates with advanced disease in patients with cutaneous T-cell lymphomas. Postepy Hig Med Dosw (Online) 2009;63:355–9. [PubMed] [Google Scholar]
- 96.Ye SW, Wang Y, Valmori D, Ayyoub M, Han Y, Xu XL, Zhao AL, Qu L, Gnjatic S, Ritter G, Old LJ, Gu J. Ex-vivo analysis of CD8+ T cells infiltrating colorectal tumors identifies a major effector-memory subset with low perforin content. J Clin Immunol. 2006;26(5):447–56. doi: 10.1007/s10875-006-9040-4. [DOI] [PubMed] [Google Scholar]
- 97.Webb JR, Wick DA, Nielsen JS, Tran E, Milne K, McMurtrie E, Nelson BH. Profound elevation of CD8+ T cells expressing the intraepithelial lymphocyte marker CD103 (alphaE/beta7 Integrin) in high-grade serous ovarian cancer. Gynecol Oncol. 2010;118(3):228–36. doi: 10.1016/j.ygyno.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 98.Gregg R, Smith CM, Clark FJ, Dunnion D, Khan N, Chakraverty R, Nayak L, Moss PA. The number of human peripheral blood CD4+ CD25 high regulatory T cells increases with age. Clin Exp Immunol. 2005;140(3):540–6. doi: 10.1111/j.1365-2249.2005.02798.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Campisi J. Aging, cellular senescence, and cancer. Ann Rev Physiol. 2013;75:685–705. doi: 10.1146/annurev-physiol-030212-183653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Campisi J, d'Adda di Fagagna F. Cellular senescence: when bad things happen to good cells. Nat Rev Mol Cell Biol. 2007;8(9):729–40. doi: 10.1038/nrm2233. [DOI] [PubMed] [Google Scholar]
- 101.Prieur A, Peeper DS. Cellular senescence in vivo: a barrier to tumorigenesis. Curr Opin Cell Biol. 2008;20(2):150–5. doi: 10.1016/j.ceb.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 102.Dimri GP. What has senescence got to do with cancer? Cancer Cell. 2005;7(6):505–12. doi: 10.1016/j.ccr.2005.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Takai H, Smogorzewska A, de Lange T. DNA damage foci at dysfunctional telomeres. Curr Biol. 2003;13(17):1549–56. doi: 10.1016/s0960-9822(03)00542-6. [DOI] [PubMed] [Google Scholar]
- 104.Chen QM, Prowse KR, Tu VC, Purdom S, Linskens MH. Uncoupling the senescent phenotype from telomere shortening in hydrogen peroxide-treated fibroblasts. Exp Cell Res. 2001;265(2):294–303. doi: 10.1006/excr.2001.5182. [DOI] [PubMed] [Google Scholar]
- 105.Alimonti A, Nardella C, Chen Z, Clohessy JG, Carracedo A, Trotman LC, Cheng K, Varmeh S, Kozma SC, Thomas G, Rosivatz E, Woscholski R, Cognetti F, Scher HI, Pandolfi PP. A novel type of cellular senescence that can be enhanced in mouse models and human tumor xenografts to suppress prostate tumorigenesis. J Clin Invest. 2010;120(3):681–93. doi: 10.1172/JCI40535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Serrano M, Lin AW, McCurrach ME, Beach D, Lowe SW. Oncogenic ras provokes premature cell senescence associated with accumulation of p53 and p16INK4a. Cell. 1997;88(5):593–602. doi: 10.1016/s0092-8674(00)81902-9. [DOI] [PubMed] [Google Scholar]
- 107.Coppe JP, Kauser K, Campisi J, Beausejour CM. Secretion of vascular endothelial growth factor by primary human fibroblasts at senescence. J Biol Chem. 2006;281(40):29568–74. doi: 10.1074/jbc.M603307200. [DOI] [PubMed] [Google Scholar]
- 108.Liu D, Hornsby PJ. Senescent human fibroblasts increase the early growth of xenograft tumors via matrix metalloproteinase secretion. Cancer Res. 2007;67(7):3117–26. doi: 10.1158/0008-5472.CAN-06-3452. [DOI] [PubMed] [Google Scholar]
- 109.Campisi J. Aging and cancer cell biology, 2007. Aging Cell. 2007;6(3):261–3. doi: 10.1111/j.1474-9726.2007.00292.x. [DOI] [PubMed] [Google Scholar]
- 110.Linton PJ, Dorshkind K. Age-related changes in lymphocyte development and function. Nat Immunology. 2004;5(2):133–9. doi: 10.1038/ni1033. [DOI] [PubMed] [Google Scholar]
- 111.Rossi DJ, Jamieson CH, Weissman IL. Stems cells and the pathways to aging and cancer. Cell. 2008;132(4):681–96. doi: 10.1016/j.cell.2008.01.036. [DOI] [PubMed] [Google Scholar]
- 112.Warren LA, Rossi DJ. Stem cells and aging in the hematopoietic system. Mech Ageing Dev. 2009;130(1-2):46–53. doi: 10.1016/j.mad.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Harrison DE. Mouse erythropoietic stem cell lines function normally 100 months: loss related to number of transplantations. Mech Ageing Dev. 1979;9(5-6):427–33. doi: 10.1016/0047-6374(79)90083-6. [DOI] [PubMed] [Google Scholar]
- 114.Harrison DE. Long-term erythropoietic repopulating ability of old, young, and fetal stem cells. J Exp Med. 1983;157(5):1496–504. doi: 10.1084/jem.157.5.1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Morrison SJ, Wandycz AM, Akashi K, Globerson A, Weissman IL. The aging of hematopoietic stem cells. Nat Med. 1996;2(9):1011–6. doi: 10.1038/nm0996-1011. [DOI] [PubMed] [Google Scholar]
- 116.Harrison DE, Astle CM, Stone M. Numbers and functions of transplantable primitive immunohematopoietic stem cells. Effects of age. J Immunol. 1989;142(11):3833–40. [PubMed] [Google Scholar]
- 117.de Haan G, Van Zant G. Dynamic changes in mouse hematopoietic stem cell numbers during aging. Blood. 1999;93(10):3294–301. [PubMed] [Google Scholar]
- 118.Chambers SM, Shaw CA, Gatza C, Fisk CJ, Donehower LA, Goodell MA. Aging hematopoietic stem cells decline in function and exhibit epigenetic dysregulation. PLoS Biol. 2007;5(8):e201. doi: 10.1371/journal.pbio.0050201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Pearce DJ, Anjos-Afonso F, Ridler CM, Eddaoudi A, Bonnet D. Age-dependent increase in side population distribution within hematopoiesis: implications for our understanding of the mechanism of aging. Stem Cells. 2007;25(4):828–35. doi: 10.1634/stemcells.2006-0405. [DOI] [PubMed] [Google Scholar]
- 120.Dykstra B, Olthof S, Schreuder J, Ritsema M, de Haan G. Clonal analysis reveals multiple functional defects of aged murine hematopoietic stem cells. J Exp Med. 2011;208(13):2691–703. doi: 10.1084/jem.20111490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Miller JP, Allman D. The decline in B lymphopoiesis in aged mice reflects loss of very early B-lineage precursors. J Immunol. 2003;171(5):2326–30. doi: 10.4049/jimmunol.171.5.2326. [DOI] [PubMed] [Google Scholar]
- 122.Signer RA, Montecino-Rodriguez E, Witte ON, McLaughlin J, Dorshkind K. Age-related defects in B lymphopoiesis underlie the myeloid dominance of adult leukemia. Blood. 2007;110(6):1831–9. doi: 10.1182/blood-2007-01-069401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Rossi DJ, Bryder D, Zahn JM, Ahlenius H, Sonu R, Wagers AJ, Weissman IL. Cell intrinsic alterations underlie hematopoietic stem cell aging. Proc Natl Acad Sci U S Am. 2005;102(26):9194–9. doi: 10.1073/pnas.0503280102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Pang WW, Price EA, Sahoo D, Beerman I, Maloney WJ, Rossi DJ, Schrier SL, Weissman IL. Human bone marrow hematopoietic stem cells are increased in frequency and myeloid-biased with age. Proc Natl Acad Sci U S Am. 2011;108(50):20012–7. doi: 10.1073/pnas.1116110108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ergen AV, Goodell MA. Mechanisms of hematopoietic stem cell aging. Exp Gerontol. 2010;45(4):286–90. doi: 10.1016/j.exger.2009.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Wedding U, Honecker F, Bokemeyer C, Pientka L, Hoffken K. Tolerance to chemotherapy in elderly patients with cancer. Cancer Control. 2007;14(1):44–56. doi: 10.1177/107327480701400106. [DOI] [PubMed] [Google Scholar]
- 127.Minami H, Ohe Y, Niho S, Goto K, Ohmatsu H, Kubota K, Kakinuma R, Nishiwaki Y, Nokihara H, Sekine I, Saijo N, Hanada K, Ogata H. Comparison of pharmacokinetics and pharmacodynamics of docetaxel and Cisplatin in elderly and non-elderly patients: why is toxicity increased in elderly patients? J Clin Oncol. 2004;22(14):2901–8. doi: 10.1200/JCO.2004.10.163. [DOI] [PubMed] [Google Scholar]
- 128.Lee C, Raffaghello L, Brandhorst S, Safdie FM, Bianchi G, Martin-Montalvo A, Pistoia V, Wei M, Hwang S, Merlino A, Emionite L, de Cabo R, Longo VD. Fasting cycles retard growth of tumors and sensitize a range of cancer cell types to chemo-therapy. Sci Transl Med. 2012;4(124):124ra27. doi: 10.1126/scitranslmed.3003293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lee C, Safdie FM, Raffaghello L, Wei M, Madia F, Parrella E, Hwang D, Cohen P, Bianchi G, Longo VD. Reduced levels of IGF-I mediate differential protection of normal and cancer cells in response to fasting and improve chemotherapeutic index. Cancer Res. 2010;70(4):1564–72. doi: 10.1158/0008-5472.CAN-09-3228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Safdie F, Brandhorst S, Wei M, Wang W, Lee C, Hwang S, Conti PS, Chen TC, Longo VD. Fasting enhances the response of glioma to chemo- and radiotherapy. PloS One. 2012;7(9):e44603. doi: 10.1371/journal.pone.0044603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Shi Y, Felley-Bosco E, Marti TM, Orlowski K, Pruschy M, Stahel RA. Starvation-induced activation of ATM/Chk2/p53 signaling sensitizes cancer cells to cisplatin. BMC Cancer. 2012;12:571. doi: 10.1186/1471-2407-12-571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Safdie FM, Dorff T, Quinn D, Fontana L, Wei M, Lee C, Cohen P, Longo VD. Fasting and cancer treatment in humans: A case series report. Aging. 2009;1(12):988–1007. doi: 10.18632/aging.100114. [DOI] [PMC free article] [PubMed] [Google Scholar]