Abstract
Cognitive bias modification has recently been discussed as a possible intervention for mental disorders. A specific form of this novel treatment approach is approach-avoidance modification. In order to examine the efficacy of approach-avoidance modification for positive stimuli associated with social anxiety, we recruited 43 individuals with social anxiety disorder and randomly assigned them to a training (implicit training to approach smiling faces) or a control (equal approach and avoidance of smiling faces) condition in three sessions over the course of a one-week period. Dependent measures included clinician ratings, self-report measures of social anxiety, and overt behavior during behavioral approach tasks. No group differences in any of the outcome measures were observed after training. In addition, while individuals in the training group showed increased approach tendency in one of the sessions, this effect was inconsistent across the three sessions and did not result in long-term changes in implicit approach tendencies between the groups over the course of the entire study. These results suggest that approach-avoidance modification might result in short-lasting effects on implicit approach tendencies towards feared positive stimuli, but this modification may not result in meaningful behavioral change or symptom reduction in individuals with social anxiety disorder.
Keywords: social anxiety disorder, approach bias, cognitive bias modification, implicit interventions
Social anxiety disorder (SAD) is a highly prevalent psychological disorder in the United States, affecting approximately 12% of the population over a lifetime course (Kessler, Chiu, Demler, Merikangas, & Walters, 2005). Briefly, this disorder is characterized by a persistent fear of negative evaluation by others in one or more social situations, leading to extreme distress and/or avoidance of social situations. Often, such avoidance leads to significant impairment in forming adequate social relationships, or interferes with educational and career attainment (DSM-IV-T-R, 2000). A number of studies have shown that patients with social anxiety disorder exhibit specific cognitive biases when processing social stimuli (Heinrichs & Hofmann, 2001). Moreover, modifying these biases appears to have a positive effect on social anxiety symptoms and behaviors (e.g., Amir et al., 2009). Cognitive Bias Modification (CBM) paradigms typically aim to change maladaptive cognitive biases through implicit training (i.e., out of conscious awareness of the participant). Recent meta-analyses revealed that CBM paradigms are effective at reducing cognitive biases associated with anxiety and may also be potentially beneficial for reducing anxiety disorder symptoms (Beard, Sawyer, & Hofmann, 2012; Hakamata et al., 2010; Hallion & Ruscio, 2011).
The majority of CBM studies have examined modification to attention bias (termed as CBM-A) via a modified dot probe task. For example, studies targeting attention bias in individuals with social anxiety disorder typically present participants with pairs of faces (neutral or threatening) and train them to direct their attention away from the threatening stimulus by situating the probe in the position of the neutral face whenever it was paired with a threatening one. CBM-A has been shown to result in significant social anxiety reduction from pre- to post-test after multiple sessions of such training (e.g. Amir et al., 2009). However, several replications (which were administered primarily over the internet or in naturalistic settings through use of hand-held, portable devices) have failed to find a specific training effect of CBM-A, and similar symptom reductions are seen even in individuals who are exposed to the non-training version of this task (i.e., when probes equally replace threat and neutral faces) repeatedly over time. That is, all individuals in both control and active conditions have been observed to improve over the course of CBM-A training, although they do so at higher rates than waiting list controls (clinical sample of SAD: Carlbring et al., 2012; high anxiety analogue sample: Enock, Hofmann, & McNally, under review).
A less explored avenue for cognitive modification lies in the modification of automatic approach and avoidance tendencies. One instrument specifically designed to measure implicit approach and avoidance is the Approach-Avoidance Task (AAT; Rinck & Becker, 2007). The AAT measures implicit avoidance and approach of various stimuli by instructing participants to either push a joystick towards the computer screen away from themselves to make the presented stimuli smaller and disappear (“avoid” condition), or pull the joystick away from the screen towards themselves to magnify the presented stimuli (“approach” condition). Participants are not explicitly told to push and pull certain pictures based on their content; rather, they are told to push/pull based on the orientation (portrait/landscape) or hue (gray or brown scale) of the picture, thus measuring implicit reaction times of approach/avoidance.
The AAT has been used extensively as an assessment tool in a range of studies to obtain an implicit measurement of a variety of approach and/or avoidance behaviors (spider fear: Rinck & Becker, 2007; avoidance of crowds with high ratios of angry to neutral faces: Lange, Keijsers, Becker & Rinck, 2008; alcohol use: Wiers, Rinck, Kordts, Houben, & Strack, 2009; pathological skin-picking: Schuck, Keijsers, & Rinck, 2012; obsessive-compulsive disorder: Najmi, Kuckertz, & Amir, 2010). The proposed mechanism upon which the AAT provides implicit assessments of fear lies with response latencies to the indirect instructions of the task; specifically, an individual’s automatic tendency to associate a presented stimulus with an approach behavior, indicating a willingness to come into closer contact with the stimulus, or an avoidance behavior, indicating a reluctance to engage with that stimulus. Further, whereas many implicit measures have studied these automatic, uncontrolled associations, the AAT differs from these by more fully masking the stimulus type that is of most interest (e.g. fear of threatening faces). This is achieved by the non-verbal nature of the task, and by the use of instructions that ask the participant to respond to other unrelated aspects of the stimulus (such as hue or orientation), instead of anything content-related (Dasgupta, 2010).
A study by Heuer, Rinck, and Becker (2007) utilized the AAT to evaluate the implicit avoidance of social stimuli in a group of highly socially anxious (HSA) individuals compared to their low socially anxious counterparts. Heuer and colleagues found significantly higher avoidance behaviors in response to both angry and smiling faces in HSAs; further, for smiling faces, they found a distinct discrepancy between explicit valence and implicit assessment of the approachability to such positive stimuli. Specifically, even though HSAs explicitly rated smiling faces as equally positive as their low-anxious participants, they avoided them significantly more. This discrepancy was not observed in the subjective ratings and behavioral avoidance of angry faces. Thus, participants in this study evidenced greater non-verbalized, implicit avoidance of the positive stimulus, even though they explicitly did not assess these smiling faces as any less pleasant or more threatening as non-anxious individuals, indicating a unique index of avoidance. This finding has since been replicated in other samples of individuals with high social anxiety, with additional evidence that gaze direction (averted or direct) results in the same level of avoidance only in the case of smiling faces, but not angry faces, which are only avoided when the threatening stimulus is facing the participant directly (Roelofs et al., 2010). Such findings of implicit avoidance of positive stimuli are consistent with growing evidence for a significant and distinct fear of positive evaluation in social anxiety (Weeks, Jakatdar, & Heimberg, 2010), and explicit ratings of lower approachability of positive faces (Campbell et al., 2009). The fear of positive evaluation is associated with negative evaluation fears, but appears to represent a separate portion of the overall fear of evaluation that characterizes social anxiety (Rodebaugh, Weeks, Gordon, Langer, & Heimberg, 2012). This feared domain therefore serves as a potentially important potential target for intervention in individuals with SAD.
However, whereas the utility of the AAT as an assessment tool for implicit approach and avoidance has been well supported, there is a distinct scarcity of studies that use the AAT as an intervention to modify fear-related processes. Only a handful of studies to date have been published on the use of the AAT as an intervention, and only one of these tested high socially anxious individuals (Taylor & Amir, 2012). The first two studies using the AAT as an intervention were conducted with populations with substance dependence/abuse issues, where individuals with problematic drinking were trained over either one (Wiers et al., 2010) or four sessions (Wiers, Eberl, Rinck, Becker, & Lindenmeyer, 2011) to avoid pictures of alcohol, and demonstrated a superior outcome (e.g. less alcohol consumed at immediate post-test, lower relapse rates of alcohol dependence at a one-year follow-up) as compared to different versions of control AATs. In another study examining modification of avoidance of OCD-related contamination stimuli, individuals identified as having concerns about contamination-related fears (i.e. two standard deviations above the fear level of the normal population) who were trained to approach such pictures were more likely to take more steps towards their feared objects during a behavioral test than control subjects who completed an AAT where there was equal approach to both contaminated and neutral objects (Amir, Kuckertz, & Najmi, in press). Another study assessing implicit racial attitudes and discrimination showed that non-Black participants subliminally trained to approach pictures of Black individuals demonstrated lower implicit prejudice on the Implicit Association Test, and showed more open body posture and closer physical proximity when engaging in an intimate conversation with a Black confederate, as compared to participants trained to avoid the same stimuli or a control group (Kawakami, Phills, Steele, & Dovidio, 2007).
Most pertinent to the current study was the recent investigation by Taylor and Amir (2012), which used a modified AAT designed specifically for use with a high social anxiety undergraduate sample. In line with the previous assessment studies showing a unique avoidance of stimuli explicitly rated as positive by HSAs (Heuer et al., 2007; Roelofs et al., 2010), the study authors wished to train individuals to approach positive facial stimuli and reduce this discrepancy between subjective report and behavior. Specifically, individuals were trained in a single session to either approach positive face pictures or to engage in a control version of the task where there was no contingency between the emotional nature of the face (positive or neutral expressions) and the joystick movement (pull/approach and sideways/no change), followed by a behavioral test involving a social interaction with an unknown confederate (using a paradigm similar to the one used in the study by Kawakami et al., 2007). Results revealed greater social approach as rated by observers, and a higher willingness expressed by confederates to engage further (even after the experiment had ended) with participants trained to approach positive stimuli. However, the authors also noted that participants in both groups showed similar decreases in subjective anxiety before and after the interaction task, and further, the AAT approach index following training did not significantly mediate the changes in social approach behavioral indices observed between groups.
The current study aims to build on these recent experiments to further elucidate the impact of modifying implicit approach tendencies, and to therefore reveal more information about the potential role of avoidance of positive evaluation in causing and maintaining social anxiety symptoms (Weeks et al., 2010; Rodebaugh et al., 2012). To our knowledge, this is the first study to test (1) whether such a modification is associated with actual behavioral change in individuals with clinical levels of social anxiety, as opposed to high socially anxious analogue samples; and (2) what the effects of multiple training sessions using an AAT intervention would be on short- and long-term approach tendencies in such a clinical sample. Specifically, our study utilized a modified multiple-session version of the AAT whereby individuals with SAD were implicitly trained to approach pictures of smiling faces, and were compared to a control group with similar severity levels of SAD, who underwent the same number of AAT sessions with a control paradigm. We predicted that the AAT would be more effective at modifying approach tendencies than the control condition. In order to demonstrate specificity of the intervention, we also administered measures of depression and related constructs in addition to social anxiety measures.
Methods
Participants
A total of 50 participants were enrolled in the study. Of these, one individual could not complete the study due to technical problems with the computer equipment, two individuals (both in the control condition) never returned for the remainder of the study after the first two sessions, and one individual (who was in the training condition) requested to stop the study after session one because of discomfort with engaging in the computer and behavioral tasks. In addition, two individuals met one or more of the exclusionary criteria at the additional diagnostic assessment conducted during the first session, and one person did not meet the established clinical cut-off score of 30 on the Liebowitz Social Anxiety Scale (LSAS) at pre-test (Mennin et al., 2002). The final sample therefore consisted of 43 completers.
Every participant had a diagnosis of generalized SAD except one subject (who had non-generalized SAD) in the completer sample (N = 43; control condition = 22, training condition = 21). Further, SAD was the principal diagnosis in 41 participants (95.3%) in the completer sample, with one participant having a principal diagnosis of generalized anxiety disorder, and the other having principal panic disorder with agoraphobia. Overall, there was significant diagnostic comorbidity in the sample, with almost half the sample (48.8%) having one additional anxiety or mood disorder. The most common comorbid disorders to SAD were generalized anxiety disorder (32.6%) and anxiety disorder - not otherwise specified, generalized anxiety disorder subtype (11.6%). LSAS scores in the sample ranged from 40 to 106, indicating moderate to severe levels of SAD, with an average LSAS score across the sample of 70.4 (SD = 14.9).
Recruitment announcements for the study called for individuals who often feel uncomfortable or fearful in social situations, and who are interested in participating in “a psychological experiment that looks at a brief computerized intervention that may help [their] fear of interacting with strangers.” Participants were primarily recruited from the community through online community posting sites (e.g. Craigslist). In addition to recruitment from community samples, patients seeking treatment at the Center for Anxiety and Related Disorders (CARD) at Boston University who completed the initial diagnostic assessment at the Center and met DSM-IV diagnostic criteria for SAD (any subtype) were invited to participate while they remained on the CARD treatment waitlist. Eligibility criteria included participation by male or female subjects between the ages of 18 and 55; meeting full criteria (either the generalized or non-generalized subtypes) for DSM-IV Social Anxiety Disorder (DSM-IV-TR, 2000) using the Anxiety Disorders Interview Schedule (ADIS; DiNardo, Brown, & Barlow, 1994), a semi-structured interview assessing clinical thresholds for all anxiety and mood disorders; and an articulated willingness and ability by participants to comply with the requirements of the study protocol. Individuals on psychotropic medications for emotional symptoms were permitted in the study if they were on a stable dose over the past three months.
Exclusionary criteria included individuals who endorsed current suicidal or homicidal ideation, intent, or recent past attempts; the presence of certain higher-risk psychiatric conditions (posttraumatic stress disorder or acute stress disorder, current substance abuse or dependence, bipolar disorder, or any psychotic disorder); any current use of street drugs; absence of appropriate corrective eyesight apparatus for those reporting impairment in vision (i.e. glasses, contacts); physical handicap/injury involving dominant hand to avoid strain on this limb during the repeated joystick task; and limited mental competency, or inability, to provide informed, written consent. In addition, individuals in concurrent psychotherapy were excluded from the study.
Measures
Liebowitz Social Anxiety Scale – Clinician Version (LSAS-CV)
The LSAS-CV (Liebowitz, 1987) is a clinician-administered measure assessing for level of fear and avoidance of 24 social situations (11 social interactional and 13 performance-based) over the past week using a 4-point Likert scale. The measure therefore produces a total score consisting of scores on the fear and avoidance subscales that ranges from 0 to 144. The LSAS-CV has been widely used and shown to have good psychometric properties (Heimberg et al., 1999). For this study, anxiety and avoidance as measured by this instrument consisted of the time period for the week leading up to the pre-test, and then for the level of symptoms since the pre-test until the post-test assessment (a five-day period).
Social Phobia Inventory (SPIN)
The SPIN is a self-report measure consisting of 17 Likert-scale items assessing for three domains of social anxiety: fear, avoidance, and physiological arousal (Connor et al., 2000). Scores on the three subscales were combined to yield a total score of symptoms over the past week, with a range of scores from 0 to 68. This measure has demonstrated good test-retest reliability, internal consistency, and convergent and divergent validity (Connor et al., 2000), and served as an additional measure of self-reported SAD symptoms over the course of the study.
Beck Depression Inventory-II (BDI-II)
The BDI-II is a more recent version of the original BDI (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961), a widely used and well-validated tool for the assessment of depressive symptoms. The BDI-II consists of 21 items scored on a 4-point Likert scale (0–3), resulting in a total score ranging from 0 to 63, with higher scores indicating higher levels of depressive symptoms in the past week.
Interpersonal Sensitivity Measure (IPSM)
The original version of the IPSM contains 36 4-point Likert scale items assessing for heightened sensitivity to rejection in social interactions with others. Harb and colleagues (2002) examined the psychometric properties of this measure in individuals seeking treatment for social phobia, given the relevance of this construct in social anxiety pathology. Evidence was found for significant factor loadings of 29 items from the original IPSM, with four of the items having negative factor loadings and therefore being reversed scored (Harb, Heimberg, Fresco, Schneier, & Liebowitz, 2002). Total scores on the 29-item version of this measure (ranging from 29 to 116) were therefore utilized as a measure of hypersensitivity to rejection by others at pre- and post-test.
State-Trait Anxiety Inventory- State version (STAI-B)
The STAI-B is an 8-item self-report measure that assesses current subjective distress levels, and was adapted from the longer 20-item state-trait version (Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983). The measure uses a 4-point Likert scale, and consists of five negative affect items and three positive affect items (that are reversed-scored) to compute a total score ranging from 8 to 32, with higher scores indicating higher negative affect. The 8-item STAI-B has been used widely as a state measure of anxiety and distress, with a particular sensitivity to changes in these constructs as a result of experimental or naturally occurring stressors (Hofmann, Heering, Sawyer, & Asnaani, 2009; Spielberger et al., 1983). This measure was administered at baseline, in anticipation and then after each of the behavioral tasks (see below) as a measure of subjective distress at both pre- and post-assessment.
Behavioral Approach Task (BAT)
Participants underwent two behavioral performance tasks. In the first BAT, participants were instructed to initiate and maintain a conversation with an unknown opposite sex confederate while being videotaped. This is consistent with the paradigm of social interaction utilized in other studies, which show evidence of a higher report of anxiety when interacting with individuals who have the potential to be romantic partners (Heinrichs & Hofmann, 2005). Participants were encouraged to speak with this individual for about 5 minutes, or for as long as they could up to this time. The confederates were trained to maintain a neutral/slightly friendly but passive disposition to ensure that the responsibility of maintaining the conversation fell solely on the participant (Hofmann, Moscovitch, Kim, & Taylor, 2004). For the second BAT, participants were instructed to perform an impromptu speech on any or all of three controversial topics provided just before the start of their speech in front of two confederates (one male and one female) while being videotaped for as long as they could (up to 10 minutes) until they wished to end their speech. For both BATs, participants were given a sign to hold up as an indication that they wished to stop the task. Several behavioral measures were recorded: latencies to start the task as a measure of willingness to engage in the social tasks, length of time participants engaged in the tasks, and participants’ ratings of subjective distress before and after the tasks.
Intervention
Although the test-retest reliability of the AAT is relatively low (r=0.35), the internal consistency is relatively high for a behavioral test, ranging between r = 0.66 and r = 0.70 (Reinecke, Becker, & Rinck, 2010). Further, the AAT has shown robust validity correlations with self-report measures assessing the same construct, in the range of 0.45 – 0.59, depending on the avoidance stimulus being studied. In this version of the AAT, participants were instructed to respond according to picture color rather than contents; using a joystick, they had to pull closer all pictures shown in greyscale (approach), and to push away all pictures shown in sepia (avoidance). A zoom function was used, such that upon pulling the joystick, the pictures grew in size, and upon pushing it, they shrank.
Training stimuli
Participants in the training condition were trained on three occasions to approach pairs of smiling faces (each pair consisted of a male and a female) and avoid checkerboards on 96% of the trials of the training portion of the task because faces were shown predominantly in greyscale and checkerboards in sepia. There were 24 unique male-female face pairs, with the female face placed on the left for 12 pictures, and on the right for the other 12 pictures in both sepia and greyscale tones, to counterbalance the positioning of genders. Consistent with the neutral stimuli utilized in other studies, one checkerboard stimulus was used in both color tones (Heuer et al., 2007). The same stimuli were used across all experimental sittings for both assessment and training trials, but order was randomized to minimize order effects. Face stimuli for the AAT in this study were obtained from the Radboud Faces Database (RaFD; Langner et al., 2010), and had been extensively pre-tested to ensure recognition of the target emotions of interest (anger/unpleasant, happy/pleasant). Pairs of male and female faces were utilized to more closely match the subsequent BATs, which either used a male or female confederate in the interaction BAT (depending on the participant’s gender), or both male and female confederates for the speech BAT. Those in the control condition engaged in a Faces-AAT where they were trained to approach identical pairs of smiling faces and checkerboards at an equal rate (because color was not confounded with contents).
For both versions of the Faces-AAT, each of the three sessions started with a brief block of 14 practice trials (which consisted of equal approach/avoidance to one of the face pairs and the checkerboard used in the task) and 28 assessment trials (equal approach/avoidance of 24 unique face pairs and 4 checkerboards). These were followed by 440 training trials, and another assessment block of 28 trials near the end of the task to measure within-session training effects. For the training condition, there were also 16 control (approach of checkerboards instead of faces) trials interspersed during the major training block to maintain the implicit nature of the task. In total, each session consisted of 546 trials and took about 15–20 minutes.
Procedure
Participants expressing interest in participating in the experiment first underwent a phone screen to determine eligibility on the basis of inclusionary and exclusionary clinical features for the study, lasting about 15 minutes. The Social Anxiety Disorder module of the Anxiety Disorders Interview Schedule (ADIS) was first administered over the phone to determine initial eligibility for the study, i.e. a current clinical threshold of SAD according to DSM-IV criteria. Eligible individuals interested in the study then came in for the on-site screening session which included an extensive assessment of psychiatric history (including the ADIS-IV-L and the LSAS) and completed a battery of psychological self-report measures after providing written informed consent and having the opportunity to ask any questions. If eligibility was determined, random assignment to experimental condition was made at this time. Participants (regardless of condition) were then told they would be completing a series of computer tasks involving a joystick, and tasks where they would have to interact with unknown others.
Session 1
Participants were first asked to sit quietly in the experimental room for 5 minutes to obtain a baseline measure of subjective distress on a scale of 1–10 and they also completed a baseline STAI-B. This was followed by administration of the behavioral outcome measures. After a short 5–10 minute break and recovery period, participants were assessed for subjective distress to ensure a return to baseline levels, after which the participant then engaged in either a training AAT where they were indirectly instructed to approach smiling faces (training condition), or a control AAT where they were instructed to avoid and approach smiling faces and the neutral stimulus an equal number of times.
Session 2
Participants completed a self-report version of the LSAS, and then engaged in either another training AAT or control AAT identical to what they engaged in during the first training session (which had occurred two days prior).
Session 3
Participants came in two days after Session 2 and completed another 5-minute baseline period to assess baseline subjective distress and STAI-B for session 3. This was followed by one final training/control session of the same length and number of trials. Participants then completed all the same outcome measures and tasks, i.e. clinician-administered LSAS, a full battery of self-report questionnaires identical to pre-assessment, and BATs as they did at pre-test in Session 1 with new unknown confederates and new speech topics.
At the end of Session 3, participants were assessed for what they believed the purpose of the experiment was, to verify that the study condition indeed remained blind to the participant and the implicit nature of the study was preserved. In addition, they indicated how much they felt their social anxiety symptoms had improved over the course of the study, their belief about which condition they were in (training or control), and their confidence level (from 0–100) about being in the training condition. They were then thoroughly debriefed and received payment for their participation for all three days of the study. The entire time commitment to the study did not exceed five hours (i.e. two and a half hours at Session 1, half an hour at Session 2, and two hours at Session 3), and participants were paid $75 for completing the entire experiment. All study procedures were reviewed and approved by Boston University’s Institutional Review Board.
Study Design
The study followed a double-blind randomized approach, such that the condition of the participant (AAT training versus control AAT) was unknown to the participant, to the experimenter conducting the study, and to the confederates engaging in the BATs with the participant. In addition, assignment to each experimental arm was made randomly. The BATs were always presented as the last assessment measure (because of the highest potential of these behavioral tasks to cause carryover effects on the other outcomes due to the generation of significant anxiety). Finally, to account for order effects, there were two sets of speech topics presented that were counterbalanced at pre- and post-assessment across participants to ensure there were no biases occurring from exposure to certain speech topics at pre-test versus post-test.
Results
Descriptive and baseline characteristics of sample
Participants had an average age of 27.6 years (SD = 9.0), were 53.5% Caucasian, 69.8% female, and 37.2% reported being employed full- or part-time. The groups did not significantly differ in distribution of age, race, gender or employment status.
Baseline LSAS, SPIN, BDI-II, and IPSM scores, along with baseline STAI-B change scores at anticipation and end of each of the BATs (conversation and speech) are shown in Table 1. There was a significant difference between groups at pre-test with the control group scoring higher than the training condition group on the SPIN (45.5 vs. 37.1, F (1, 41) = 6.69, p = .013), with a similar trend on the LSAS (74.6 vs. 66.1, F (1, 41) = 3.75, p = .060). There were no differences between the conditions on the other self-report, behavioral, or implicit measures at baseline.
Table 1.
Pre-assessment and post-assessment scores on outcome measures across condition.
| Training Condition Mean (SD) |
Control Condition Mean (SD) |
|||
|---|---|---|---|---|
| Pre | Post | Pre | Post | |
| AAT approach tendency | 20.8 (53.6) | 14.9 (55.4) | 19.9 (67.4) | −8.95 (58.3) |
| LSAS | 66.1 (14.0) | 59.5 (19.9) | 74.6 (14.8) | 70.0 (20.4) |
| SPIN | 37.1 (10.4)a | 31.8 (10.3)a | 45.5 (10.9)b | 42.1 (11.4)b |
| BDI-II | 12.2 (8.4) | 10.2 (7.8) | 13.2 (13.4) | 12.9 (12.8) |
| IPSM-29 | 80.3 (11.0) | 82.0 (10.4) | 79.5 (10.7) | 82.1 (11.3) |
| Latency in seconds (interaction BAT) | 15.1 (14.7) | 16.1 (13.5) | 14.1 (18.5) | 9.2 (7.7) |
| Total duration of task in seconds (interaction BAT) | 273.1 (66.7) | 281.7 (49.1) | 245.6 (103.5) | 243.3 (92.7) |
| Anticipation STAI-B (interaction BAT) | 5.5 (4.3) | 3.0 (3.7) | 4.7 (4.2) | 4.7 (5.2) |
| Post-task STAI-B (interaction BAT) | 4.9 (4.6) | 2.8 (4.2) | 2.5 (5.6) | 2.4 (7.2) |
| Latency in seconds (interaction BAT) | 9.0 (12.2) | 7.5 (7.7) | 12.2 (21.0) | 7.9 (13.2) |
| Total duration of task in seconds (interaction BAT) | 279.3 (189.1) | 241.2 (157.1) | 225.6 (172.9) | 234.0 (181.0) |
| Anticipation STAI-B (speech BAT) | 8.5 (4.5) | 6.4 (4.8) | 8.5 (4.6) | 8.0 (5.4) |
| Post-task STAI-B (speech BAT) | 7.9 (6.2) | 6.2 (4.6) | 8.3 (5.5) | 6.0 (8.1) |
Note. The table shows pre-assessment and post-assessment mean scores and standard deviations (SD) on all outcome measures of participants in both conditions of the study; a, b subscripts denote significantly different values at p<0.05 between conditions at each time point; AAT = Approach-Avoidance Task; LSAS = Liebowitz Social Anxiety Scale; SPIN = Social Phobia Inventory; BDI-II = Beck Depression Inventory-II; IPSM-29 = Interpersonal Sensitivity Measure – 29 item version; BAT = Behavioral Approach Task; Latency = time taken to begin task; Duration = time spent engaging in task; STAI-B = 8-item State-Trait Anxiety Inventory, state version.
Effect of AAT in modifying approach tendency
Before data analysis, the AAT data were assessed for outliers; the fastest and slowest 1% of all reaction times (RTs) were excluded, and then median RTs from the rest of the data-points were computed for each participant. The mean RTs for each of the 6 assessment points (pre- and post-assessment within each of the three sessions) showed moderate internal consistency (Cronbach’s alpha = 0.57). In addition, accuracy rates in both the assessment and training phases were high (97%) given the ease of the task, with no significant differences between groups. A one-way analysis of variance (ANOVA) showed that both groups were similar in their levels of initial approach bias on the AAT, which was defined as the average median RT to pull (approach) smiling faces subtracted from the average median RT to push (avoid) smiling faces (Table 1). Higher, more positive values on this measure therefore indicate higher approach tendencies (i.e. faster reaction times to pulling smiling faces). Approximately two thirds (63.6%) of both the training and control groups showed an initial positive approach bias (as indicated by values greater than zero, i.e. faster reaction times to pulling versus pushing smiling faces, on this index).
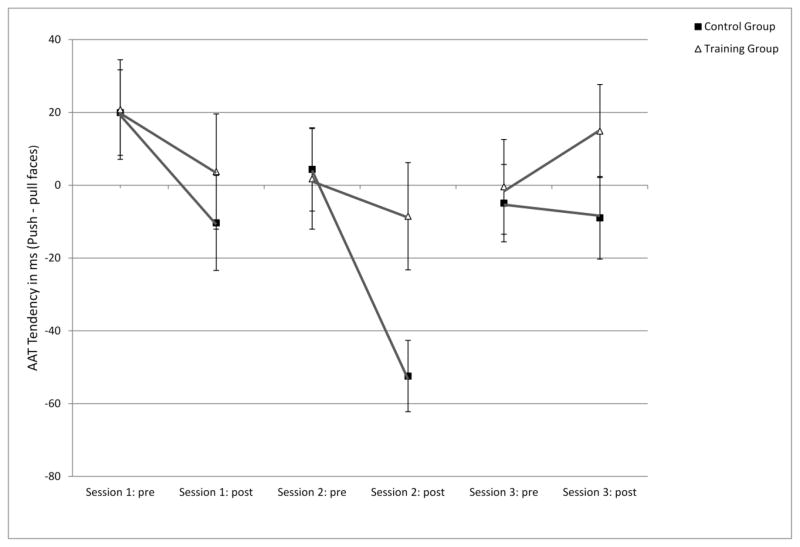
To determine changes in the approach bias within each of the three sessions, a 3 (Session: 1, 2, 3) × 2 (Time assessment: pre-training, post-training) × 2 (Condition: training group, control group) mixed ANOVA was conducted to determine changes in AAT approach tendency between groups at the three repeated assessment points. This analysis did not reveal any significant interaction effects. Further, as shown in Figure 1, the two groups did not significantly differ in change on approach index at session 1. However, in session 2, the training group showed maintenance of their initial approach bias whereas the control group showed a significant decrease in approach bias, (−10 ms (SD = 55 ms) vs. −57 ms (SD = 83 ms), F (1,41) = 6.49, p = .015, partial eta squared = .14). In session 3, the training group showed the expected increase in approach bias, and the control group maintained their initial approach bias, but this difference did not meet statistical significance.
Figure 1.
Mean approach-avoidance index at pre- and post-assessment points for all three sessions.
Note. The figure shows mean approach tendency (reaction times for pulling faces subtracted from reaction times for pushing faces) at each of the pre- and post-test time points in each experimental sitting. AAT: Approach-Avoidance Task; Sessions 1–3: each experimental sitting; Pre: pre-test assessment of tendency in the session; Post: post-test assessment of tendency in the session.
Long-term effect of approach training
Whereas there were significant differences between training and control group within session 2 and an observed training effect in the expected direction in session 3, the two groups did not differ in their long-term approach tendencies (Figure 1). Specifically, even though the AAT was successful in maintaining approach tendencies in the training group within at least one of the experimental sessions, the within-between ANOVA did not reveal a statistically significant difference between the AAT approach index at the final assessment point at the end of session 3 and the initial assessment point in the beginning of session 1 (change scores: −6 ms (SD = 66 ms) in training group vs. −29 ms (SD = 89 ms) in control group, F (1,41) = 0.53, p = .472, partial eta squared = .01). Further, at the pre-training assessment point at the start of each of the three training sessions, the two groups did not differ in their approach tendency (Session 1: 21 ms (SD = 54 ms) vs. 20 ms (SD = 67 ms), F (1,41) = 0.00, p = .964; Session 2: 2 ms (SD = 63 ms) vs. 4 ms (SD = 55 ms), F (1,41) = 0.02, p = .888; Session 3: −0.4 ms (SD = 43 ms) vs. −5 ms (SD = 60 ms), F (1,41) = 0.08, p = .781; all training versus control).
Effect of AAT training on clinical outcomes
A 2 by 2 between-groups analysis of covariance (ANCOVA) was used to determine the strength of changes on all dependent measures (self-report scores, subjective distress, and behavioral measures) from pre- to post-AAT intervention between the independent factor of condition. This test allowed us to most adequately improve the power of the between-group analyses by including baseline scores on all independent measures as covariates in each corresponding analysis. These analyses revealed largely no significant interaction or main effects on any of the dependent measures at post-test, even after controlling for baseline scores on all measures (Table 1). The only exception was a significant difference between groups in the latency time to start the conversation BAT, with the training group showing increased latencies for this task by session 3 than controls (i.e. an increase of 0.9 seconds vs. a decrease of 4.9 seconds, F (1,34) = 4.54, p = .040, partial eta squared = 0.12).
Effect of AAT training on clinical outcomes in whole sample
The overall sample improved significantly from pre- to post-test on several measures. Specifically, repeated measures ANOVA showed significant reductions in the whole sample from pre- to post-test on the clinician-administered LSAS (F (1,42) = 6.79, p = .013, Cohen’s d = .31), the SPIN (F (1,42) = 11.66, p = .001, Cohen’s d = .37), and STAI-B scores at the end of the speech BAT (F (1,37) = 4.27, p = 0.046, Cohen’s d = .34), as shown in Table 2. Participants did not show significant changes on the BDI-II or the other BAT measures (latency/time spent in both BATs, or remainder of subjective distress ratings).
Table 2.
Repeated measures analysis of variance pre-post in dependent variables: entire sample.
| Outcome measure | Mean (SD) (Pre-test) | Mean (SD) (Post-test) | F-value (dfbetween, dfwithin) | Cohen’s d |
|---|---|---|---|---|
| AAT approach tendency | 20.35(60.36) | 2.70(57.51) | 2.17(1,42) | 0.30 |
| LSAS | 70.40(14.85) | 64.88(20.61) | 6.79(1,42)* | 0.31 |
| SPIN | 41.44 (11.35) | 37.07 (11.99) | 11.66(1,42)** | 0.37 |
| BDI-II | 12.74(11.09) | 11.60(10.63) | 2.07(1,42) | 0.10 |
| IPSM-29 | 80.56(10.80) | 82.06(10.73) | 1.31(1,35) | 0.14 |
| BAT Interaction – Latency (seconds) | 15.15(16.85) | 12.49(11.71) | 1.02(1,36) | 0.18 |
| BAT Interaction – Duration (seconds) | 261.32(86.69) | 260.60(77.81) | 0.01(1,39) | 0.01 |
| BAT Interaction – Anticipation STAI-B | 5.15(4.28) | 3.98(4.62) | 2.44(1,39) | 0.26 |
| BAT Interaction – Post-task STAI-B | 3.53(5.42) | 2.58(6.10) | 1.05(1,37) | 0.16 |
| BAT Speech – Latency (seconds) | 11.31(17.73) | 7.72(10.87) | 3.78(1,38) | 0.24 |
| BAT Speech – Duration (seconds) | 248.13(182.66) | 237.20(168.53) | 0.53 (1,39) | 0.06 |
| BAT Speech – Anticipation STAI-B | 8.49(4.56) | 7.23(5.18) | 1.77 (1,38) | 0.26 |
| BAT Speech – Post-task STAI-B | 8.21 (5.85) | 6.03(6.70) | 4.27(1,37)* | 0.35 |
Note. The table shows differences and effect sizes for entire sample from pre- to post-test on all outcome measures using repeated measures analysis of variance. SD = standard deviation; F = F statistic; dfbetween = degrees of freedom between groups; dfwithin = degrees of freedom within groups;
p < 0.05;
p < 0.01;
AAT = Approach-Avoidance Task; LSAS = Liebowitz Social Anxiety Scale; SPIN = Social Phobia Inventory; BDI-II = Beck Depression Inventory-II; IPSM-29 = Interpersonal Sensitivity Measure, 29-item version; BAT = behavioral approach test; Latency = time taken to begin task; Duration = time spent engaging in task; STAI-B = 8-item State-Trait Anxiety Inventory, state version. Cohen’s d (estimate of effect size) was calculated using the formula d = Mean1−Mean2/√[(SD12 + SD22)/2], as outlined in Dunlap et al., 1996.
Expectancy Effects
Finally, we examined the association between expectancy effects by participants and performance on all dependent variables at post-test. Specifically, participants were asked after the experiment (before they were debriefed) about (1) whether they believed they improved over the course of the study (not at all, somewhat, and significantly), and (2) the degree to which they believed they were in the “active” condition of the study (on a scale of 0–100), without this term being defined for the participant, thereby allowing participants to make their own judgments about whether there was an active intervention that they perceived to be targeting their symptoms.
The majority (64.1%) of participants reported some (44.2%) or significant improvement (14.0%), but there were no significant differences between condition groups in terms of how much participants felt they improved over the course of the study (χ2 (2, N = 39) = 3.32, p = .190). In addition, certainty of being in the active condition did not predict significant changes in any of the dependent measures. Further, roughly half (54%) of participants endorsed a belief of at least 60 out of 100 that they were in the active condition of the study. The two groups did not differ in terms of how many people in each group believed they were in the active condition of the study (χ2 (1, N = 43) = 0.05, p = .817), and only one person out of the entire sample guessed that the active component of the study was through the use of the AAT, indicating that the blind, implicit nature of the AAT intervention remained intact.
Discussion
This study aimed to elucidate the ability of the AAT to modify implicit approach behaviors towards positive facial stimuli in a clinical sample of SAD, to explore the maintenance of any training effects over multiple sessions, and to assess the association of training with a variety of clinical and behavioral outcomes. First, the AAT was partially successful in maintaining approach tendencies towards smiling faces in session 2 in the training group, with evidence of improvement in approach tendency in session 3 in this group, indicating some short-term effectiveness in modifying this cognitive target in individuals with SAD. However, this training effect was not maintained between sessions, such that both groups came into sessions 2 and 3 with similar levels of approach and avoidance, despite different approach behaviors on the AAT at the end of each prior session. Also, more than half of participants in each group started the study with an initial approach bias, which has also been observed in other studies using high social anxiety samples (Taylor & Amir, 2012). Further, approach bias is a relative index, and while non-anxious controls were not included in the present study, it is expected (and has been observed elsewhere) that they would likely show an even greater approach bias for positive faces than individuals with SAD (Heuer et al., 2007; Campbell et al., 2009).
We expected an increased willingness to engage with confederates (measured by reduced latency to be ready for the BATs, spending a longer time engaging in the social tasks, and less subjective distress before and after each BAT) as a result of decreasing participants’ fear of positive evaluation through approach training to smiling faces. Yet, the only significant result that emerged for the between-group analyses on multiple measures of behavioral avoidance was a longer latency in the training group to engage in the speech task at post-test; as a result, it is difficult to ascertain whether this was a true effect of the training, or simply due to chance. Furthermore, the current study did not reveal a specific effect of the training condition of the AAT on any of the other outcome measures assessed. Yet, both groups improved on several key measures of interest, including clinician-rated LSAS symptom scores, self-report SPIN scores, and behavioral indices (i.e. subjective distress at the end of the speech BAT). In addition, improvements in these outcome measures were not predicted by expectancy effects by participants, namely degree of belief of being in the active condition or beliefs about how much they improved over the course of the study.
Only one study thus far has conferred specific benefit to individuals actively trained to approach feared positive emotional stimuli (Taylor & Amir, 2012). However, this study differed from the present study in several key ways. Specifically, the previous study used approach (pull) versus no avoidance movement (sideways), as compared to the approach (pull) and avoid (push) features of the AAT used in this study. Similarly, Taylor and Amir (2012) utilized neutral faces as the neutral stimuli as opposed to the non-social checkerboard stimuli used in the current study, which could have an impact on the strength of the training of implicit social approach behaviors (and the simultaneous training of “avoidance” behaviors of neutral stimuli). Such procedural differences could result in potentially different implicit training targets.
Further, the study by Taylor and Amir (2012) utilized an analogue undergraduate sample with average LSAS scores that were distinctly lower than participants’ scores in the current study. The current study’s clinical sample is much more relevant to our understanding of how the AAT works in SAD patients than any previous study. Related to this, an important consideration is that unlike previous successes with the AAT in training avoidance of appetitive stimuli as seen in substance use (Wiers et al., 2010; Wiers et al., 2011), the training in SAD requires the strengthening of approach tendencies to aversive stimuli, which is a conceptually different implicit target. It is conceivable that approach to feared objects in a clinical sample is a more complex and emotionally-laden process, which is also consistent with the observation that the training effects of the active condition were resistant to long-term maintenance over the three sessions, and even evidence for efficacy of short-term modification within the experimental sittings was limited and inconsistent.
There are several important limitations to acknowledge in this pilot study of AAM. First, with the final sample consisting of just over 20 completers in each group, inadequate power was an important potential limitation. Additionally, the current study purposefully did not include a waitlist control group to parse out the effects of repeated measurement on the outcome changes in the whole sample, since this was not a primary aim of this study. Thus, we must consider the possibility that other factors may have contributed to the symptom improvements observed in the whole sample over the course of the study, such as repeatedly meeting with study staff to discuss social anxiety concerns, coming to the lab multiple times and engaging in social stressor tasks, and completing the assessment measures. However, attention bias modification studies with a waitlist arm have found a significant and superior outcome for both training and control training groups over waitlist (Enock et al., under review). Further, a meta-analysis pooling the effect sizes for LSAS change in each treatment arm of CBM studies of SAD has found a combined Cohen’s d effect size of .32 (small effect) for waitlist/no intervention conditions (n = 10 studies; Kuckertz & Amir, in preparation).
Using the formula outlined by Cohen (1988) and Dunlap, Cortina, Vaslow & Burke (1996), the current study had an effect size of .31 for decrease on the LSAS and .37 for decrease on the SPIN in the entire sample, which translates to small to medium effect sizes of the AAT compared to no treatment, regardless of condition. It therefore appears that the sample on the whole did not improve considerably more than what would be expected from a waitlist condition, and we did not find support for the idea that variable doses of approach-avoidance modification may have beneficial effects on symptom reduction, as compared to no exposure to such a modification. The study by Taylor and Amir (2012) similarly found that approach index following training did not significantly mediate the improvements in the behavioral outcomes assessed in their study. Clearly, more investigation is needed to better understand the mechanisms of the benefit observed in these studies, and to more definitively examine how any training (control or active) compares to none.
Another phenomenon observed in attention retraining is that individuals with a larger initial attentional bias for threat show greater training effects after re-training, which is reflected in better improvements on outcomes of interest (Amir, Taylor, & Donahue, 2011). This is important to consider in the current findings, given that the majority of individuals in both groups actually presented with an initial approach (and not avoidance) bias before any experimental manipulation occurred. This suggests a possible analogous explanation for the null results observed here: approach training might be clinically helpful only for patients who exhibit a clear avoidance bias before training, not for patients who have a (possibly weak) initial approach bias already. We sought to explore whether the AAT training could be differentially beneficial in the current study; however, given the small sample size, each of the 4 experimental cells (training/initial avoidance bias, training/initial approach bias, control/initial avoidance bias, control/initial approach bias) were too small to adequately investigate this issue. Since the importance of the initial bias has been observed in attention retraining paradigms only, it certainly requires more extensive examination in the realm of approach-avoidance modification.
In addition, it would have been beneficial to use an independent measure of approach/avoidance tendencies (e.g. whole body steps forward or backwards as used in Stins et al., 2011) as a way to test the generalizeability and efficacy of the AAT in modifying participants’ implicit approach and avoidance behaviors, and as a measure of convergent validity of the AAT paradigm. Another feature to note in the current study is the relatively short time-frame between the final training session and the post-treatment assessment (which all occurred in the final session), which could possibly limit the full impact of the final training session on observable change in social behavior and reported social anxiety symptoms. The post-assessment should have occurred ideally in a follow-up period. However, this was not logistically feasible. Finally, other studies have utilized the same number of unique neutral stimuli as target stimuli (Wiers et al., 2010; Taylor & Amir, 2012; Kawakami et al., 2007), which was not the case in the current study and which may have negatively influenced the strength of the training effect towards smiling faces.
A plethora of interesting areas for future research emerge from the current findings. First and foremost, given the small sample size of the current study, it is imperative that the results found here are replicated to validate the current findings. That is, while it is possible that significant effects were not evident due to the sample size limitation, it is equally feasible that these differences between the training and control group do not exist. Follow-up studies may not find it necessary to hold multiple training sessions for individuals with high social anxiety, given our observation that the training effect of the AAT lasted only within one session (with no maintenance of the training effect over the three experimental sittings). Alternatively, many more training sessions might be necessary to achieve maintenance of training effects over sessions, therefore the number of training sessions would be important to investigate further.
Moreover, the AAT may need to be modified and tested to determine whether certain design features (e.g. use of happy faces for approach and angry faces for avoidance instead of neutral objects for avoidance) may result in successful training of approach and avoidance tendencies in individuals with social anxiety. In addition, all future designs are advised to include a waitlist arm to more fully determine the strength of the effects of repeated AAM exposure for both training and control versions of these tasks, and to parse out whether extraneous factors (e.g. repeated measurement of symptoms and the BATs) are actually responsible for the overall improvement observed for the whole sample in this study on several outcomes. Finally, it is important to consider whether the effects of approach training may show some benefit in certain subgroups of individuals; for instance, in those presenting with a certain diagnostic picture (i.e. with or without comorbidity of other psychological disorders), or in those presenting with higher initial avoidance bias.
Despite its limitations, the current pilot study offers several unique aspects that, to our knowledge, have never been implemented to date. Specifically, this study utilized a clinical sample, conducted trainings over multiple sessions, and assessed the effects of approach training to positive stimuli on a wide variety of outcomes (including self-report, implicit measures, and multiple behavioral indices). Participants were representative in severity level and comorbid diagnostic patterns of a clinical sample of SAD, and were demographically diverse. Further, this study aimed to provide pilot data to begin the examination on whether the AAT can be used as a viable alternative intervention or augmentation to traditional treatments of SAD, by targeting the notably distinct and significant fear of positive evaluation in this disorder (Weeks et al., 2010; Rodebaugh et al., 2012).
If replication studies reveal the same effect as the current one, this task may not provide the additional benefit to assessment and treatment of clinical social anxiety symptoms as we had hoped. However, if future studies (unlike the current one) can consistently show that targeting implicit features of SAD results in a meaningful reduction in the disorder symptoms, this might diversify the treatment options for those individuals with social anxiety who are hesitant about seeking more traditional therapy approaches because of stigma or other biases. In either case, the possibilities for additional research are numerous and exciting as we move forward to better our understanding of effective treatment for these emotional symptoms.
Acknowledgments
Stefan Hofmann is a paid consultant of Merck Pharmaceutical (Schering-Plough) for work unrelated to this study. This study was partially supported by NIMH grants MH-078308 and MH-081116 awarded to Stefan Hofmann. Eni Becker and Mike Rinck were supported by the Behavioural Science Institute of Radboud University Nijmegen, The Netherlands.
The authors are grateful to Frank Leonhardt for programming the AAT. Moreover, they would like to acknowledge the following research assistants who provided crucial and much-appreciated assistance with the project on multiple domains, including data entry, recruitment advertising, serving as study confederates, and reliability video coding: Imke Vonk, Dan Brager, Rachel Kaufmann, Brian Hall, Myles Rizvi, Brian Gambardella, and Rebecca Grossman. Without their hard work and dedication, the study would never have come to fruition.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: APA; 2000. text revision. [Google Scholar]
- Amir N, Beard C, Taylor CT, Klumpp H, Elias J, Burns M, Chen X. Attention training in individuals with generalized social phobia: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2009;77:961–73. doi: 10.1037/a0016685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir N, Kuckertz JM, Najmi S. The effect of modifying automatic action tendencies on overt avoidance behaviors. Emotion. doi: 10.1037/a0030443. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir N, Taylor CT, Donohue MC. Predictors of response to an attention modification program in generalized social phobia. Journal of Consulting and Clinical Psychology. 2011;79:533–541. doi: 10.1037/a0023808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Ward C, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Beard C, Sawyer AT, Hofmann SG. Efficacy of attention bias modification using threat and appetitive stimuli: A meta-analytic review. Behavior Therapy. 2012;43:724–740. doi: 10.1016/j.beth.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlbring P, Apelstrand M, Sehlin H, Amir N, Rousseau A, Hofmann S, Andersson G. Internet-delivered attention modification training in individuals with social anxiety disorder - A double blind randomized controlled trial. BMC Psychiatry. 2012;12:66. doi: 10.1186/1471-244X-12-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Connor KM, Davidson JT, Churchill L, Sherwood A, Foa E, Weisler RH. Psychometric properties of the Social Phobia Inventory (SPIN): New self-rating scale. The British Journal Of Psychiatry. 2000;176:379–386. doi: 10.1192/bjp.176.4.379. [DOI] [PubMed] [Google Scholar]
- Dasgupta N. Implicit Measures of Social Cognition Common Themes and Unresolved Questions. Journal of Psychology. 2010;218:54–57. [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Client Interview Schedule. New York, NY: Oxford University Press; 1994. [Google Scholar]
- Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1:170–177. [Google Scholar]
- Enock PM, Hofmann SG, McNally RJ. Attention bias modification treatment via iPhone and other handheld devices to reduce social anxiety and worry: a randomized controlled trial under review. [Google Scholar]
- Hakamata Y, Lissek S, Bar-Haim Y, Britton JC, Fox NA, Leibenluft E, Pine DS. Attention bias modification treatment:A meta-analysis toward the establishment of novel treatment for anxiety. Biological Psychiatry. 2010;68:982–990. doi: 10.1016/j.biopsych.2010.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallion LS, Ruscio AM. A meta-analysis of the effect of cognitive bias modification on anxiety and depression. Psychological Bulletin. 2011;137:940–958. doi: 10.1037/a0024355. [DOI] [PubMed] [Google Scholar]
- Harb GC, Heimberg RG, Fresco DM, Schneier FR, Liebowitz M. The psychometric properties of the Interpersonal Sensitivity Measure in social anxiety disorder. Behaviour Research And Therapy. 2002;40:961–980. doi: 10.1016/s0005-7967(01)00125-5. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Horner KJ, Juster HR, Safren SA, Brown EJ, Schneier FR, Liebowitz MR. Psychometric properties of the Liebowitz Social Anxiety Scale. Psychological Medicine. 1999;29:199–212. doi: 10.1017/s0033291798007879. [DOI] [PubMed] [Google Scholar]
- Heinrichs N, Hofmann SG. Information processing in social phobia: A critical review. Clinical Psychology Review. 2001;21:751–770. doi: 10.1016/s0272-7358(00)00067-2. [DOI] [PubMed] [Google Scholar]
- Heinrichs N, Hofmann SG. Cognitive Assessment of Social Anxiety: A Comparison of Self-report and Thought Listing Methods. Cognitive Behaviour Therapy. 2005;34:3–15. doi: 10.1080/16506070410030106. [DOI] [PubMed] [Google Scholar]
- Heuer K, Rinck M, Becker ES. Avoidance of emotional facial expressions in social anxiety: The Approach–Avoidance Task. Behaviour Research and Therapy. 2007;45:2990–3001. doi: 10.1016/j.brat.2007.08.010. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Heering S, Sawyer AT, Asnaani A. How to handle anxiety: The effects of reappraisal, acceptance, and suppression strategies on anxious arousal. Behaviour Research and Therapy. 2009;47:389–394. doi: 10.1016/j.brat.2009.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Moscovitch DA, Kim H, Taylor AN. Changes in self-perception during treatment of social phobia. Journal of Consulting and Clinical Psychology. 2004;72:588–596. doi: 10.1037/0022-006X.72.4.588. [DOI] [PubMed] [Google Scholar]
- Kawakami K, Phills CE, Steele JR, Dovidio JF. (Close) distance makes the heart grow fonder: Improving implicit racial attitudes and interracial interactions through approach behaviors. Journal Of Personality And Social Psychology. 2007;92:957–971. doi: 10.1037/0022-3514.92.6.957. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuckertz JM, Amir N. A selective meta-analysis comparing cognitive bias modification to other evidence-based psychosocial programs for social anxiety disorder in preparation. [Google Scholar]
- Lange WG, Keijsers G, Becker ES, Rinck M. Social anxiety and the evaluation of social crowds: Explicit and implicit measures. Behaviour Research and Therapy. 2008;46:932–943. doi: 10.1016/j.brat.2008.04.008. [DOI] [PubMed] [Google Scholar]
- Langner O, Dotsch R, Bijlstra G, Wigboldus DJ, Hawk ST, van Knippenberg A. Presentation and validation of the Radboud Faces Database. Cognition And Emotion. 2010;24:1377–1388. [Google Scholar]
- Liebowitz MR. Social phobia. Modern Problems of Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Mennin DS, Fresco DM, Heimberg RG, Schneier FR, Davies SO, Liebowitz MR. Screening for social anxiety disorder in the clinical setting: Using the Liebowitz Social Anxiety Scale. Journal Of Anxiety Disorders. 2002;16:661–673. doi: 10.1016/s0887-6185(02)00134-2. [DOI] [PubMed] [Google Scholar]
- Najmi S, Kuckertz J, Amir N. Automatic avoidance tendencies in individuals with contamination-related obsessive-compulsive symptoms. Behaviour Research and Therapy. 2010;48:1058–1062. doi: 10.1016/j.brat.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinecke A, Becker ES, Rinck M. Three indirect tasks assessing implicit threat associations and behavioral response tendencies: Test-retest reliability and validity. Journal of Psychology. 2010;218:4–11. [Google Scholar]
- Rinck M, Becker ES. Approach and avoidance in fear of spiders. Journal of Behavior Therapy and Experimental Psychiatry. 2007;38:105–120. doi: 10.1016/j.jbtep.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Weeks JW, Gordon EA, Langer JK, Heimberg RG. The longitudinal relationship between fear of positive evaluation and fear of negative evaluation. Anxiety, Stress & Coping: An International Journal. 2012;25:167–182. doi: 10.1080/10615806.2011.569709. [DOI] [PubMed] [Google Scholar]
- Roelofs K, Putman P, Schouten S, Lange WG, Volman I, Rinck M. Gaze direction differentially affects avoidance tendencies to happy and angry faces in socially anxious individuals. Behaviour Research and Therapy. 2010;48:290–294. doi: 10.1016/j.brat.2009.11.008. [DOI] [PubMed] [Google Scholar]
- Schuck K, Keijsers GPJ, Rinck M. Implicit responses to skin irregularities predict symptom severity and treatment susceptibility in pathological skin picking. Journal of Behavior Therapy and Experimental Psychiatry. 2012;43:685–691. doi: 10.1016/j.jbtep.2011.09.004. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE, Vagg PR, Jacobs GA. Manual for the state-trait anxiety inventory (form Y) Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- Stins JF, Roelofs K, Villan J, Kooijman K, Hagenaars MA, Beek PJ. Walk to me when I smile, step back when I’m angry: Emotional faces modulate whole-body approach–avoidance behaviors. Experimental Brain Research. 2011;212:603–611. doi: 10.1007/s00221-011-2767-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor CT, Amir N. Modifying automatic approach action tendencies in individuals with elevated social anxiety symptoms. Behaviour Research and Therapy. 2012;50:529–536. doi: 10.1016/j.brat.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks JW, Jakatdar TA, Heimberg RG. Comparing and contrasting fears of positive and negative evaluation as facets of social anxiety. Journal Of Social And Clinical Psychology. 2010;29:68–94. [Google Scholar]
- Wiers RW, Rinck M, Kordt R, Houben K, Strack F. Retraining automatic action-tendencies to approach alcohol in hazardous drinkers. Addiction. 2010;105:279–287. doi: 10.1111/j.1360-0443.2009.02775.x. [DOI] [PubMed] [Google Scholar]
- Wiers RW, Eberl C, Rinck M, Becker ES, Lindenmeyer J. Retraining automatic action tendencies changes alcoholic patients approach bias for alcohol and improves treatment outcome. Psychological Science. 2011;22:490–497. doi: 10.1177/0956797611400615. [DOI] [PubMed] [Google Scholar]