Abstract
Objectives
The current study examined the diagnostic profiles and clinical characteristics of youth (ages 6–18) referred for diagnostic evaluation to a pediatric mood disorders clinic that specialized in early-onset bipolar disorder.
Method
A total of 250 youth were prescreened in an initial telephone intake and 73 participated in a full diagnostic evaluation. Trained psychologists administered the Schedule for Affective Disorders for Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL) to the child and at least one parent, and a child psychiatrist conducted a separate pharmacological evaluation. Evaluators then met with a larger clinical team for a consensus diagnostic conference.
Results
Based on consensus diagnoses, 13 of the 73 referred youth (18%) met lifetime DSM-IV-TR criteria for bipolar I, II or not otherwise specified (NOS) disorder. The most common Axis I diagnoses were attention deficit-hyperactivity disorder (31/73, 42.5%) and major depressive disorder (23/73, 32%). Of the 73 youth, 27 (37%) were referred to the speciality clinic with a community diagnosis of BSD, but only 7 of these (26%) met the DSM-IV-TR criteria for a bipolar spectrum diagnosis (BD I, II, cyclothymic disorder, or NOS) based on structured interview and consensus diagnoses.
Conclusions
When youth referred for evaluation of BSD are diagnosed using standardized interviews with multiple reporters and consensus conferences, the “true positive” rate for bipolar spectrum diagnoses is relatively low. Reasons for the discrepancy between community and research-based diagnoses of pediatric BSD – including the tendency to stretch the BSD criteria to include children with depressive episodes and only 1–2 manic symptoms - are discussed.
Keywords: bipolar spectrum disorder, hypomania, structured diagnostic evaluations, assessment instruments, child and adolescent
Approximately 28% of adults with bipolar disorder (BD) report symptom onset before 13 years of age, and about 66% before 18 years (1). Early onset is often associated with a treatment-resistant course of BD in adulthood, with a high prevalence of rapid cycling, mixed symptoms, comorbid disorders, suicidal behavior and functional impairment (2, 3). Misdiagnosing BD in children can have significant adverse consequences for the long-term management of the disorder (4).
The prevalence of clinical diagnoses of pediatric BD increased 40-fold between 1993 and 2003 (5), although it is not clear whether this increase reflects true over-diagnosis or the lack of recognition of early-onset BD prior to 1990. It is estimated that approximately 95,000 children and adolescents were receiving medications for bipolar disorder in the United States as of 2001 (6). In contrast, a meta-analysis of 12 clinical studies of pediatric bipolar disorder (including BD I, II, and NOS) found a 2% prevalence rate in the United States as well as in other countries (including Mexico, the Netherlands, Ireland, the United Kingdom, and Spain; 7). Furthermore, there was no evidence of a temporal increase in the community prevalence of BD during the two decades spanned by these studies. The National Comorbidity Survey-Revised reported a 2%–4% prevalence rate of bipolar spectrum disorders (BSDs) among adolescents, defined as bipolar I, II, not otherwise specified, or cyclothymic disorder (8); and a 2.5% lifetime rate of manic episodes among adolescents (9).
Early detection and subsequent treatment of BSDs may reduce the severity, chronicity, and treatment resistance characteristic of the disorder in adulthood (10). Differential diagnosis of BSDs in children and adolescents, however, is especially challenging. First, there is a significant overlap in the symptoms of BSDs and other psychiatric disorders, notably attention deficit hyperactivity disorder (ADHD), conduct disorder, and oppositional defiant disorder (10). Second, symptoms of mania or hypomania in a depressed child or adolescent are often overlooked unless they cause clear functional impairment (11). Third, parents tend to be more reliable reporters of manic symptoms than are children, yet some clinicians rely exclusively on child report (12). Finally, a “backlash” against the possible over-diagnosis of BSDs may have caused some community clinicians to err on the side of using diagnoses such as “mood disorder not otherwise specified” or “intermittent explosive disorder” when there are doubts about the significance of (hypo)manic symptoms (13). These issues may adversely affect the reliability of community diagnoses of BSD.
The primary objective of this study was to examine the diagnostic profiles of youth who were referred to a university-based child and adolescent mood disorders clinic specializing in bipolar disorder. All youth referred to the clinic had been described as having significant mood dysregulation. All had either (a) received a previous mental health evaluation resulting in a bipolar spectrum diagnosis and were seeking a second opinion, or (b) parents who recognized one or more manic symptoms in their child and were interested in diagnostic clarification and treatment recommendations.
Because of the relatively low threshold for naming bipolar disorder as the primary diagnosis in community settings, we hypothesized that rates of BSDs would be much lower when diagnoses were based on structured interviews with children and one or both parents, independent psychiatrist interviews, and consensus diagnostic conferences. Secondarily, because the average age at onset of BD I and Major Depressive Disorder (MDD) is during late adolescence, we hypothesized that these diagnoses would be more likely among older adolescents than among children or preadolescents.
Methods
Participants
Telephone screening interviews were conducted with all parents who called the UCLA Child and Adolescent Mood Disorders Program (CHAMP) clinic from January 2010 to January of 2012. The CHAMP clinic specializes in the evaluation and pharmacological/psychosocial treatment of youth who meet criteria for a bipolar spectrum disorder. Referrals to the clinic came from outpatient clinics, inpatient and partial hospitals, self-referral, and local community agencies in the greater Los Angeles Area. Eligibility criteria for clinic services included the presence of mood lability, depression, or a previous diagnosis of bipolar disorder by parental report. Youth between the ages of 6 and 19 were included in the present report.
To meet the eligibility criteria for a full evaluation at the clinic, parents needed to endorse symptoms of mania (e.g., elated mood, decreased need for sleep) and evidence of impairment in the school or home environment. Examples of impairment included inappropriate social behavior, declining school performance, hospitalization, residential treatment, or increased family discord. Another path to eligibility was a community diagnosis of bipolar spectrum disorder. Most often, the parents of these children were interested in a second diagnostic opinion and a pharmacological consultation. Children that did not meet the clinic’s telephone screening criteria (e.g., those with symptoms of ADHD or oppositional defiant disorder with no significant mood dysregulation) were referred elsewhere.
Procedures
The diagnostic evaluation consisted of two to three appointments with clinic psychologists and psychiatrists. Diagnoses were obtained using the Schedule for Affective Disorders for Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL; 14). Youth and at least one parent/caregiver were required to participate in the evaluation. Following the semi-structured K-SADS-PL assessment, youth and parent(s) met with one of the clinic’s child psychiatrists for a secondary diagnostic and pharmacological evaluation.
Diagnostic interviews were conducted by doctoral level psychology interns, child psychiatry fellows, and postdoctoral psychology fellows. All intakes were supervised by a licensed clinical psychologist or board certified child and adolescent psychiatrist. Consensus ratings on the KSADS and differential diagnoses were obtained during weekly clinic rounds meetings where the child’s specific symptoms from each of the KSADS modules were reviewed. Consensus diagnoses were assigned based on DSM-IV-TR criteria (15), using data from the KSADS and the psychiatrist evaluation regarding the nature of the symptoms, the associated impairment, and the overall coherence of the clinical picture.
Measures
Diagnostic Instrument
The KSADS-PL is a semi-structured interview designed to assess current (i.e., worst week within the previous month) and past lifetime psychopathology, containing five modules: affective, psychotic, anxiety, disruptive behavior, and substance abuse disorders. All sections of the K-SADS were conducted with each clinically referred youth based on the findings from the core screening modules. The affective disorders module of the K-SADS-PL was replaced with the K-SADS Depression Rating Scale (DRS; 16) and Mania Rating Scale (MRS; 16) for more in-depth evaluation of mood symptoms. These rating scales are based on the original K-SADS items, but provide additional questions regarding affective symptoms, a greater range of response choices (i.e., most items range from 1–6, instead of 1–3), and enhanced anchors for ratings regarding intensity, duration, and frequency of symptoms. These scales have been used reliably in prior studies of pediatric bipolar populations (e.g., 17, 18, 19).
Each KSADS module was conducted separately with the youth and at least one parent, with a consensus rating based on both reports. When the youth and parent(s) disagreed on K-SADS items, they were interviewed conjointly to inform a consensus rating. Inter-rater reliability for the K-SADS-PL and the mood disorders supplements was high. The overall K-SADS-PL kappa coefficients for psychiatric disorders were ≥ 0.8. The clinic’s diagnostic supervisors, both licensed clinical psychologists, posted high reliabilities on K-SADS DRS (.72) and MRS scores (.90).
Youth were assigned mood disorder diagnoses including BD (I, II, or Not Otherwise Specified, or NOS), major depressive disorder (MDD), and mood disorder NOS. BD-NOS was defined as the presence of clinically relevant BD symptoms that did not fulfill the DSM-IV criteria for BD-I or BD-II. Because the diagnosis of BD-NOS is defined by exclusion in DSM-IV-TR, we used the operational definition from the Course and Outcome in Bipolar Youth (COBY) study: a period that included elated mood plus two DSM-IV “B” symptoms, or irritable mood plus 3 “B” symptoms, along with a change in level of functioning that lasted a minimum of 4 hours within a 24-hour period, and were present for a minimum of 4 lifetime days (20). Note that this operational definition combines cyclothymic disorder with BD-NOS. BD-NOS was only diagnosed if the (hypo)manic symptoms represented a change from the child’s usual mood and behavioral states. In addition to mood disorder diagnoses, youth were assessed for and assigned other Axis I diagnoses for which they met DSM-IV-TR criteria.
Results
Sample composition
There were a total of 250 cases screened by telephone; 96 (38%) met screening criteria (i.e., evidence of mood instability and functional impairment) and were invited to undergo a full psychiatric evaluation. Of the 96 eligible youth, 76 (79%) appeared for the first appointment, and 73 of these 76 (96%) completed the full intake procedures. Youth who were evaluated had a mean age of 12.82 (SD = 3.48); 35 (48%) were girls and 38 (52%) were boys. The sample was primarily Caucasian and non-Hispanic (see Table 1).
Table 1.
Sample Demographics, Treatment History, and Medication (N = 73)
| Mean Age, yrs. | 12.82 (SD = 3.48) |
| Sex | |
| Male | 38 (52%) |
| Female | 35 (48%) |
| Racial Group | |
| Caucasian | 60 (82%) |
| African-American | 2 (3%) |
| Asian | 3 (4%) |
| Pacific Islander | 1 (1%) |
| Other | 2 (3%) |
| *Declined to answer | 5 (7%) |
| Hispanic Ethnicity | 11 (15%) |
| Prior outpatient treatment, no. (%) yes | 44 (60%) |
| Prior inpatient treatment, no. (%) yes | 26 (36%) |
| Medication, no. (%) on psychotropics | 54 (73%) |
| Antidepressant | 28 (38%) |
| Antipsychotic | 30 (41%) |
| Mood stabilizers | 35 (48%) |
| Alpha-adrenergic agents | 18 (25%) |
Diagnostic findings
Prior to presenting to the CHAMP clinic, a majority of the youth who received an evaluation (n = 44, 60%) had participated in outpatient treatment and over one-third (n = 26, 36%) had received prior inpatient treatment (Table 1). After completing the full diagnostic evaluation, however, only 9 youth (12%) met criteria for a primary bipolar I diagnosis; one child (1%) met criteria for a bipolar II diagnosis, and three (4%) met criteria for bipolar NOS (overall rate of BSD = 17.8%).
According to caregiver report, 27 of the 73 youth (37%) had received a prior diagnosis of BD I, II, or BD-NOS from at least one mental health professional. Of these 27, only 7 (26%) were assigned a BD diagnosis based on the CHAMP diagnostic procedures and consensus conference (Table 2). The 20 youth with a prior BD diagnosis who were not assigned a BD diagnosis all met criteria for at least one of two general diagnostic categories—non-bipolar mood disorders (i.e. MDD, dysthymia, or mood NOS; n = 15) or ADHD (n = 5) (see Table 3).
Table 2.
Agreement of Prior Community Diagnoses and Clinic Diagnoses at Intake
| Diagnosis based on clinic evaluation | ||||
|---|---|---|---|---|
| Diagnosis Prior to Intake | Agree | Disagree | % Agreement | |
| Bipolar Disorder (I & II) | 6 | 18 | 25% | |
| Bipolar Disorder NOS | 1 | 2 | 33% | |
| Depression Spectrum | 11 | 4 | 73% | |
| Schizoaffective Disorder | 1 | 0 | 100% | |
| Psychosis NOS | 0 | 1* | 0% | |
| Attention Deficit Hyperactivity Disorder | 11 | 6 | 65% | |
| Oppositional Defiant Disorder | 1 | 2 | 33% | |
| Aspergers/Autism Spectrum | 4 | 1 | 80% | |
| Anxiety Diagnoses | 3 | 2 | 40% | |
Note. The table does not include 17 patients who had not been given a community diagnosis prior to the clinic evaluation. The single child with psychosis NOS was rediagnosed with schizoaffective disorder.
Table 3.
Prior Diagnoses Reported at Intake versus Diagnoses Based on Structured Diagnostic Interviews
| Diagnosis from specialty clinic | ||||
|---|---|---|---|---|
| Prior Diagnosis | Bipolar Spectrum | Non-Bipolar Mood | Other Diagnosis | |
| Bipolar Spectrum | 7 | 15 | 5 | |
| Non-Bipolar Mood | 0 | 12 | 4 | |
| Other Diagnosis | 2 | 3 | 8 | |
| No Prior Diagnosis | 4 | 4 | ||
Sixteen youth (22%) presented to the clinic with prior diagnoses of non-bipolar mood disorders from a mental health professional (i.e. MDD, dysthymia, mood NOS, or schizoaffective disorder; table 3). The clinic’s agreement rate with pre-existing diagnoses of depression spectrum disorder was 73% (11 of 15). Only one youth presented with schizoaffective disorder, and this diagnosis was confirmed by CHAMP clinicians. None of the youth entering the clinic with a non-bipolar mood disorder diagnosis were assigned a BD diagnosis. Two youth who were referred to the clinic with a primary diagnosis of ADHD were classified with a BSD based on CHAMP procedures.
A total of 17 children (23%) entered the clinic without any previous diagnosis; 3 of these children met criteria for BD I and 1 met criteria for BD NOS. Additionally, 3 were diagnosed with MDD and 5 with mood disorder NOS. The remaining 7 children were assigned a variety of diagnoses (including ODD, anxiety disorders, an autism spectrum disorder, or a psychotic disorder; see Tables 2 and 3).
Comorbid disorders
Children met an average of 2.2 (SD = .93, range = 1–5) Axis-I diagnoses based on K-SADS consensus diagnoses. Comorbid disorders – defined as concurrent non-mood disorders in youth who had a primary mood disorder diagnosis - included anxiety spectrum disorders (n = 29, 40%), ADHD (n= 31, 43%), and ODD (n = 18, 25%) (Table 3). Of the 17 children previously diagnosed with ADHD, the CHAMP evaluation concurred in 11 cases (65%).
Prior medication use
Upon entry to the clinic, 54 of the 73 youth (74%) were currently being prescribed psychiatric medications; nineteen (26%) were not taking any psychiatric medications (Table 1). The majority of the participants were taking a combination of psychiatric medications (e.g., an atypical antipsychotic with an anticonvulsant); the totals for each medication class are provided in Table 1. At presentation to the clinic, youth were prescribed an average of 2.10 psychotropic medications (SD = 1.74), with a range of 0 to 7.
Age-related diagnostic trends
Diagnostic trends differed for younger youth (ages 6–12; n = 31) and adolescents (ages 13–19; n = 42). BD-I diagnoses were more common in adolescents (n = 8) than in younger children (n = 1; X2 (1, N = 73) = 4.13, p < .05) and MDD diagnoses were somewhat more common in older (n = 17) than younger participants (n = 6; X2(1, N = 73) = 3.69, p = .055). The diagnosis of mood disorder NOS was more common among younger children than among adolescents (X2 (1, N = 73) = 6.68, p = .010). ADHD, ODD, and anxiety diagnoses were equally distributed among younger children and adolescents (Figure 1). For adolescents, there was no correlation between gender and diagnosis. In youth under age 13, boys were more likely to have an ADHD diagnosis than were girls (t(32) = 2.138, p < .05).
Figure 1.
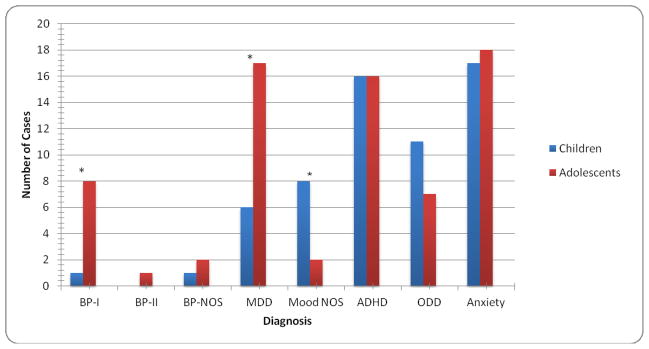
Diagnostic Frequencies by Age: Children (6–12 yrs.) compared to Adolescents (13–19 yrs)
There was no difference in the number of psychiatric medications taken between these two age groups. There was also no difference in the rate at which different types of medications were prescribed to school-aged children and adolescents, except for alpha-2 agonists. The school-aged group was prescribed alpha-2 agonists at a higher rate than adolescents (t(53) = 47.89, p < .05).
Discussion
The present study sought to compare, at the individual patient level, the consistency of pediatric bipolar disorder diagnoses by community providers and by clinicians at an outpatient mood disorders clinic that used structured diagnostic interviews and consensus diagnosis conference procedures. Families came to the clinic for diagnostic clarification regarding their child or adolescent, most typically because the child had received a community diagnosis of BD or the parent suspected the same. The methods used in the mood disorders clinic were similar to those used in research studies of pediatric mood disorders (e.g., 7, 20, 21). Based on community diagnoses, there were approximately twice as many children with a BSD diagnosis (27/56, or 48%) than a MDD diagnosis (12/56, or 21%) (17 children did not have a prior diagnosis). However, the ratio found in the clinic was nearly the inverse. The prevalence of a BD spectrum diagnosis based on clinic proceures was approximately 18% (13/73), whereas the prevalence of any other mood disorder diagnosis (predominantly MDD or mood NOS) was 53% (39/73). Overall, our findings suggest that community diagnoses of mood disorder have moderate positive predictive value, but low sensitivity relative to structured diagnostic interviews and consensus conferences.
Because the clinic’s population was not a representative sample of all children and has a referral bias given its advertised specialization (bipolar disorder and other disorders involving mood dysregulation), a high prevalence of mood disorders was expected; however, proportions of BSD to non-bipolar mood spectrum diagnoses were expected to be more in line with the general population. The clinic’s ratio of 2.5 unipolar depression cases per 1 bipolar spectrum case appears consistent with the overall distribution of mood spectrum disorders in epidemiological samples and many clinical samples (22). The rate of all types of mood disorder were higher in the clinic than in the general population, consistent with the referral pattern enriching the sample (23).
A relationship between age and diagnosis emerged, such that adolescents (ages 13–19) were more prone to meeting full criteria for a mood disorder diagnosis than were children (ages 6–12). A diagnosis of bipolar I disorder in children under 13 was extremely rare (only seen 1 time in 73 clinic cases). Whereas the clinical literature finds a high rate of conversion from BD NOS or BD II to BD I in young children who are followed for periods of 18 months to 5 years (e.g., 20, 24, 25), the timing and/or triggers for conversion are not well understood at this time. Although our data are preliminary, they are consistent with the literature suggesting a higher rate of spectrum forms of mood disorders in childhood and preadolescence, with the likelihood of acute (hypo)manic or depressive episodes increasing with age. Recent prevalence research has shown that rates of full mania (BD I) double in late adolescence as compared to early adolescence (9).
Although there were clear age differences in diagnoses, the medications that youth were prescribed in the community were very similar across age groups. This similarity may reflect the limited options for mood stabilizing or antidepressant agents available to psychiatrists working with children or adolescents with mood disorders.
These findings underscore the importance of using semi-structured interviews, such as the K-SADS, with a collaborative consensus team approach (26, 27). The process of conducting a full diagnostic assessment ensures that the clinician goes through each Axis I module, and systematically considers the DSM-IV-TR criteria for each disorder. Using tests that are statistically supported and validated is crucial for making accurate diagnoses (28). Youth with BD who do not receive a proper initial diagnosis may receive treatment that is inappropriate or ineffective, contributing to a more deteriorating course of the illness (29). For example, undetected BD can lead to improper or less effective pharmacological treatments (e.g., antidepressants; 30). Conversely, giving an unwarranted BSD diagnosis can lead to pharmacological treatment that is dangerous and causes serious side effects (31). Using objective and statistically validated measures (like the K-SADS) was an essential part of the study’s intake process and was a crucial step in formulating the diagnostic conclusions.
In addition to conducting a semi-structured interview, using converging pieces of evidence to reach a diagnosis (e.g., examining risk factors or the use of a probability nomogram) increases the validity of diagnoses (23, 32). In the CHAMP clinic, multiple clinicians worked together to evaluate risk factors (family history, medical history, environmental concerns), prior diagnoses, and current symptomatic presentation in order to reach a final diagnosis. Of course, the proposed approach is more costly than is typically allowed within community mental health settings, although it may reduce costs over the long-term when compared to the costs associated with misdiagnosis.
Limitations
We did not collect comprehensive data on the source of community referrals. With only a past diagnosis provided by the parents of the youth, we were not able to determine whether this diagnosis was from a community or another research program, nor how the diagnosis was determined. This limitation prevented more fine-grained analyses of false-negatives in the diagnosis of particular youth. Thus, we were able to evaluate the portion of community mood diagnoses that were confirmed via KSADS and consensus diagnoses, but we do not know what portion of cases not referred to the clinic had undetected bipolar disorder. There is substantial evidence that community diagnoses of bipolar spectrum disorders can have low sensitivity to hypomania (33, 34), undermining the detection of bipolar II, cyclothymic disorder, and bipolar NOS.
We also did not collect information on why bipolar diagnoses were given. Some of the children and adolescents who met DSM-IV-TR criteria for MDD had 1–2 (hypo)manic symptoms. The limited co-occurrence of (hypo)manic symptoms and depression appears to have a worse long-term prognosis than “pure” depression (35, 36). There is evidence that community diagnosticians overemphasize the role of individual manic symptoms (e.g., anger outbursts) in making pediatric bipolar diagnoses (37). It is also possible that community practitioners, when evaluating adolescents, only interviewed the youth and did not obtain supplemental information from parents or other caregivers, which often improves the reliability of mood disorder diagnoses (12).
Additionally, the sample size was limited, with only 73 youth being evaluated between the clinic’s opening in January of 2010 and January of 2012. This sample size, along with a wide variety of diagnostic categories and comorbidities among patients, limited the ability to compare specific diagnostic categories to each other. For example, comparing youth who only had BD I to youth who only had MDD was not possible because many youth in each group had comorbid ADHD or anxiety as well. Finally, the data were cross-sectional. It is possible that some of the cases currently presenting with depression will develop hypomanic or manic episodes in the future (25, 38).
The absence of data on the dosages of medications prescribed to each child in community treatment limited the conclusions from the medication analyses. Because many youth had received a prior diagnosis, comparing medication by classification (rather than dose within each classification) does not illustrate the full picture of these youths’ psychopharmacological experiences.
Conclusion
A majority of the youth evaluated in a pediatric mood disorders specialty clinic met DSM-IV-TR criteria for a mood spectrum disorder, while a minority met criteria for bipolar disorder. Agreement rates between prior community-based diagnoses and the mood specialty clinic’s diagnoses were particularly low for BSDs. After using standardized interviews with multiple reporters and consensus diagnostic conferences, the clinic’s rate of BSDs (17.8%) was consistent with previously reported specialty clinic rates of BD (23). Full mood disorder diagnoses (BD I or II, or MDD) were more common among adolescents than younger-aged children, whereas diagnoses of mood disorder NOS were significantly more prevalent in children under 13.
Results suggest that after a careful diagnostic evaluation using semi-structured interviews (e.g., K-SADS) with the youth and at least one parent, only a small percent of youth referred for evaluation of a BSD actually met DSM-IV-TR criteria for bipolar disorder. The practices of combining a structured diagnostic assessment of both the child and parent(s), a physician medical evaluation, and a team consensus conference to assign diagnoses, may account for lower rates of BSD diagnoses seem in our research clinic compared to the community.
Footnotes
All authors declare no conflicts of interest.
References
- 1.Perlis RH, Miyahara S, Marangell LB, et al. Long-term implications of early onset in bipolar disorder: Data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD) Biol Psychiatry. 2004;55(9):875–881. doi: 10.1016/j.biopsych.2004.01.022. [DOI] [PubMed] [Google Scholar]
- 2.Luby JL, Navsaria N. Pediatric bipolar disorder: evidence for prodromal states and early markers. J Child Psychol Psychiatry. 2010;51(4):459–471. doi: 10.1111/j.1469-7610.2010.02210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Youngstrom E, Van Meter A, Algorta GP. The bipolar spectrum: myth or reality? Current Psychiatry Reports. 2010;12:479–489. doi: 10.1007/s11920-010-0153-3. [DOI] [PubMed] [Google Scholar]
- 4.Parens E, Johnston J. Controversies concerning the diagnosis and treatment of bipolar disorder in children. Child Adoles Psychiatr Ment Health. 2010;10(4):9. doi: 10.1186/1753-2000-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moreno C, Laje G, Blanco C, et al. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry. 2007;64(9):1032–1039. doi: 10.1001/archpsyc.64.9.1032. [DOI] [PubMed] [Google Scholar]
- 6.Hellander I. A review of data on the health sector of the united states --january 2002. Int J Health Serv. 2002;32(3):579–599. doi: 10.2190/64HR-U27H-C3TQ-0JXL. [DOI] [PubMed] [Google Scholar]
- 7.Van Meter AR, Moreira AL, Youngstrom EA. Meta-analysis of epidemiologic studies of pediatric bipolar disorder. J Clin Psychiatry. 2011;72(9):1250–1256. doi: 10.4088/JCP.10m06290. [DOI] [PubMed] [Google Scholar]
- 8.Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the national comorbidity survey replication. Arch Gen Psychiatry. 2007;64:543–552. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Merikangas KR, Cui L, Kattan G, et al. Mania With and Without Depression in a Community Sample of US Adolescents. Arch Gen Psychiatry. 2007 doi: 10.1001/archgenpsychiatry.2012.38. [DOI] [PubMed] [Google Scholar]
- 10.Kim EY, Miklowitz DJ. Childhood mania, attention deficit hyperactivity disorder and conduct disorder: A critical review of diagnostic dilemmas. Bipolar Disord. 2002;4(4):215–225. doi: 10.1034/j.1399-5618.2002.01191.x. [DOI] [PubMed] [Google Scholar]
- 11.Bhargava Raman RP, Sheshadri SP, Janardhan Reddy YC, et al. Is bipolar II disorder misdiagnosed as major depressive disorder in children? J Affect Disord. 2007;98(3):263–266. doi: 10.1016/j.jad.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 12.Youngstrom EA, Findling RL, Calabrese JR. Effects of adolescent manic symptoms on agreement between youth, parent, and teacher ratings of behavior problems. J Affect Disord. 2004;82:5–S16. doi: 10.1016/j.jad.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 13.Youngstrom EA, Youngstrom JK, Starr M. Bipolar Diagnoses in Community Mental Health: Achenbach CBCL Profiles and Patterns of Comorbidity. Biol Psychiatry. 2005;58:569–575. doi: 10.1016/j.biopsych.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Kaufman J, Birmaher B, Brent DA, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adoles Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 15.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2001. Text Revision. [Google Scholar]
- 16.Axelson D, Birmaher BJ, Brent D, et al. A preliminary study of the kiddie schedule for affective disorders and schizophrenia for school-age children mania rating scale for children and adolescents. J Child Adolesc Psychopharmacol. 2003;13(4):463–470. doi: 10.1089/104454603322724850. [DOI] [PubMed] [Google Scholar]
- 17.Axelson D, Birmaher B, Strober M, et al. Phenomenology of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006;63(10):1139–1148. doi: 10.1001/archpsyc.63.10.1139. [DOI] [PubMed] [Google Scholar]
- 18.Hunt JI, Dyl J, Armstrong L, et al. Frequency of manic symptoms and bipolar disorder in psychiatrically hospitalized adolescents using the K-SADS mania rating scale. J Child Adol Psychopharmacol. 2005;15(6):918–930. doi: 10.1089/cap.2005.15.918. [DOI] [PubMed] [Google Scholar]
- 19.Miklowitz DJ, Axelson DA, Birmaher B, et al. Family-focused treatment for adolescents with bipolar disorder: results of a 2-year randomized trial. Arch of Gen Psychiatry. 2008;65(9):1053–1061. doi: 10.1001/archpsyc.65.9.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Birmaher B, Axelson D, Goldstein B, et al. Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: The course and outcome of bipolar youth (COBY) study. Am J Psychiatry. 2009;166(7):795–804. doi: 10.1176/appi.ajp.2009.08101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fristad MA, Frazier TW, Youngstrom EA, et al. What differentiates children visiting outpatient mental health services with bipolar spectrum disorder from children with other psychiatric diagnoses? [Research Support, N.I.H Extramural] Bipolar Disord. 2012;14(5):497–506. doi: 10.1111/j.1399-5618.2012.01034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. S0890-8567(10)00476-4 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Youngstrom EA, Freeman AJ, Jenkins MM. The assessment of children and adolescents with bipolar disorder. Child Adolest Psychiatr Clin N Am. 2009;18:353–390. doi: 10.1016/j.chc.2008.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Axelson DA, Birmaher B, Strober MA, et al. Course of subthreshold bipolar disorder in youth: Diagnostic progression from bipolar disorder not otherwise specified. J Am Acad Child Adol Psychiatry. 2011;50(10):1001–1016. doi: 10.1016/j.jaac.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nadkarni RB, Fristad MA. Clinical course of children with a depressive spectrum disorder and transient manic symptoms. Bipolar Disorders. 2010;12:494–503. doi: 10.1111/j.1399-5618.2010.00847.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Galanter CA, Patel VL. Medical decision making: a selective review for child psychiatrists and psychologists. J Child Psychol Psychiatry. 2005;46:675–689. doi: 10.1111/j.1469-7610.2005.01452.x. [DOI] [PubMed] [Google Scholar]
- 27.Jenkins MM, Youngstrom EA, Youngstrom JK, et al. Generalizability of evidence-based assessment recommendations for pediatric bipolar disorder. Psychol Assess. 2011 doi: 10.1037/a0025775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garb HN. Practicing psychological assessment. Am Psychol. 2002;57(11):990–991. doi: 10.1037/0003-066X.57.11.990b. [DOI] [PubMed] [Google Scholar]
- 29.Geller B, Tillman R, Craney JL, et al. Four-year prospective outcome and natural history of mania in children with a prepubertal and early adolescent bipolar disorder phenotype. Arch Gen Psychiatry. 2004;61:459–467. doi: 10.1001/archpsyc.61.5.459. [DOI] [PubMed] [Google Scholar]
- 30.Altshuler LL, Post RM, Leverich GS, et al. Antidepressant-induced mania and cycle acceleration: A controversy revisited. Am J Psychiatry. 1995;152(8):1130–1138. doi: 10.1176/ajp.152.8.1130. [DOI] [PubMed] [Google Scholar]
- 31.Wilens TE, Prince JB, Spencer T, et al. An open trial of bupropion for the treatment of adults with attention-deficit/hyperactivity disorder and bipolar disorder. Biol Psychiatry. 2003;54(1):9–16. doi: 10.1016/S0006-3223(02)01664-5. [DOI] [PubMed] [Google Scholar]
- 32.Youngstrom E. Pediatric bipolar disorder. In: Mash EJ, Barkley RA, editors. Assessment of childhood disorders. 4. New York: Guilford Press; 2007. pp. 253–304. [Google Scholar]
- 33.Hirschfeld RM. Bipolar spectrum disorder: improving its recognition and diagnosis. J Clin Psychiatry. 2001;62 (Suppl 14):5–9. [PubMed] [Google Scholar]
- 34.Zimmermann P, Bruckl T, Nocon A, et al. Heterogeneity of DSM-IV major depressive disorder as a consequence of subthreshold bipolarity. Arch Gen Psychiatry. 2009;66:1341–1352. doi: 10.1001/archgenpsychiatry.2009.158. 66/12/1341 [pii] [DOI] [PubMed] [Google Scholar]
- 35.Nusslock R, Frank E. Subthreshold bipolarity: diagnostic issues and challenges. Bipolar Disord. 2011;13:587–603. doi: 10.1111/j.1399-5618.2011.00957.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goldberg JF, Perlis RH, Bowden CL, et al. Manic symptoms during depressive episodes in 1,380 patients with bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2009;166(2):173–181. doi: 10.1176/appi.ajp.2008.08050746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leibenluft E. Severe mood dysregulation, irritability, and the diagnostic boundaries of bipolar disorder in youths. Am J Psychiatry. 2011;168(2):129–142. doi: 10.1176/appi.ajp.2010.10050766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hillegers MHJ, Reichart CG, Wals M, et al. Five-year prospective outcome of psychopathology in the adolescent offspring of bipolar parents. Bipolar Disord. 2005;7:344–350. doi: 10.1111/j.1399-5618.2005.00215.x. [DOI] [PubMed] [Google Scholar]


