Abstract
Background
Catheter-associated urinary tract infections (CAUTI) are costly, common and often preventable by reducing unnecessary urinary catheter (UC) use.
Methods
To summarise interventions to reduce UC use and CAUTIs, we updated a prior systematic review (through October 2012), and a meta-analysis regarding interventions prompting UC removal by reminders or stop orders. A narrative review summarises other CAUTI prevention strategies including aseptic insertion, catheter maintenance, antimicrobial UCs, and bladder bundle implementation.
Results
30 studies were identified and summarised with interventions to prompt removal of UCs, with potential for inclusion in the meta-analyses. By meta-analysis (11 studies), the rate of CAUTI (episodes per 1000 catheter-days) was reduced by 53% (rate ratio 0.47; 95% CI 0.30 to 0.64, p<0.001) using a reminder or stop order, with five studies also including interventions to decrease initial UC placement. The pooled (nine studies) standardised mean difference (SMD) in catheterisation duration (days) was −1.06 overall (p=0.065) including a statistically significant decrease in stop-order studies (SMD −0.37; p<0.001) but not in reminder studies (SMD, −1.54; p=0.071). No significant harm from catheter removal strategies is supported. Limited research is available regarding the impact of UC insertion and maintenance technique. A recent randomised controlled trial indicates antimicrobial catheters provide no significant benefit in preventing symptomatic CAUTIs.
Conclusions
UC reminders and stop orders appear to reduce CAUTI rates and should be used to improve patient safety. Several evidence-based guidelines have evaluated CAUTI preventive strategies as well as emerging evidence regarding intervention bundles. Implementation strategies are important because reducing UC use involves changing well-established habits.
Keywords: Implementation Science, Health Services Research, Infection Control, Patient Safety, Quality Improvement
The problem
Urinary tract infection (UTI) has long been considered the most common healthcare-associated infection (HAI), with the vast majority of these infections occurring after placement of the convenient, uncomfortable,1 often unnecessary2–4 and easily forgotten urinary catheter.5 With an estimated6 7 449 334 healthcare-associated catheter-associated urinary tract infections (CAUTIs) per year, associated with an additional cost (in 2007) of US$749–10077–9 per admission (or an estimated US$3744 when complicated by blood stream infections),10 it is not surprising that CAUTIs were among the first hospital-acquired conditions selected for non-payment by Medicare as of October 2008,11 and have been further targeted for complete elimination12 as a ‘never event,’ with a national goal to reduce CAUTI by 25% by 2014.13 These national initiatives renewed public and research interest in the prevention of CAUTI, prompting updates of several comprehensive guidelines14–17 and reviews of strategies to prevent CAUTI released since the 2001 Making Health Care Safer report.18
What strategies may prevent catheter-associated urinary tract infections?
Similar to other HAIs — such as central line-associated blood stream infection — many CAUTI prevention strategies have been ‘bundled’ into a composite of multimodal sets of interventions known as ‘bladder bundles.’19 These bundles consist of educational interventions to improve appropriate use and clinical skill in catheter placement, behavioural interventions such as catheter restriction and removal protocols, and use of specific technologies such as the bladder ultrasound. Despite some early success in implementing a bladder bundle19 to reduce urinary catheterisation rates,20 CAUTI prevention has proven challenging for several important reasons. For example, monitoring urinary catheter use and CAUTI rates to inform and sustain urinary catheter-related interventions is very resource intensive. Perhaps more importantly, improving practice regarding urinary catheter placement and removal also requires interventions to change the expectations and habits of nurses, physicians and patients about the need for urinary catheters.
To help organise and prioritise the many potential interventions to prevent CAUTI, we use the conceptual model of the ‘lifecycle of the urinary catheter’21 to highlight that the highest yield interventions to prevent CAUTI will target at least one of the four ‘stages’ of the catheter's ‘life.’ As illustrated in figure 1, the ‘lifecycle’ of the catheter (1) begins with its initial placement, (2) continues when it remains in place, day after day, (3) ceases when it is removed and (4) may start over if another catheter is inserted after removal of the first one.
Figure 1.
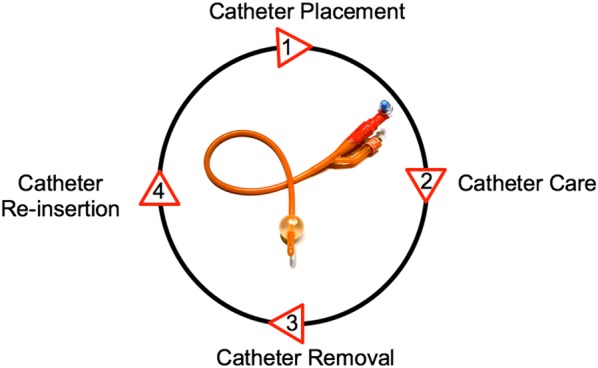
Lifecycle of the urinary catheter.21 This conceptual model illustrates four stages of the urinary catheter lifecycle as targets for interventions to decrease catheter use and catheter-associated urinary tract infection.
Because avoiding unnecessary urinary catheter use is the most important strategy in prevention of CAUTI, we review the evidence on two types of interventions that target unnecessary urinary catheter use: (1) protocols and interventions to decrease unnecessary placement of urinary catheters (catheter lifecycle stage 1), and (2) interventions that prompt removal of unnecessary urinary catheters (catheter lifecycle stage 3).
Review process
The evidence summarised in this chapter was generated using a literature search conducted for a prior systematic review and meta-analysis22 along with a focused update of the published peer-reviewed literature (from August 2008 to October 2012) through a MEDLINE search for intervention studies to reduce use of unnecessary urinary catheters in the acute care of adults. A CINAHL database search was also performed for interventions developed and implemented by nurses related to urinary catheter use. Studies were included if at least one outcome involving catheter use or CAUTI events (table 1) was reported as a result of the intervention, and with a comparison group (either preintervention vs postintervention, or a separate control group). Details of the systematic literature searches and methods employed for selection and reporting of the studies for this review are provided in the online supplementary appendix. The online supplementary appendix table summarises all the intervention studies described in this review, including study designs, patient populations and the interventions employed to avoid unnecessary catheter placement or to prompt catheter removal. This review was supported by the Agency for Healthcare Research and Quality (AHRQ), which had no role in the selection or review of the evidence or the decision to submit this manuscript for publication.
Table 1.
Description of outcomes evaluated (adapted from the prior meta-analysis22)
| Measures of Catheter-associated Urinary Tract Infection (CAUTI) development | Number of CAUTI episodes per 1000 catheter-days was recorded and a rate ratio was calculated to compare preintervention vs postintervention. When rates of both asymptomatic and symptomatic CAUTI were reported separately,57 the rates of symptomatic CAUTI were used for the meta-analysis.22 |
| Cumulative risk of CAUTI during hospitalisation (ie, the percentage of patients who developed CAUTI) was also extracted for each study, and a risk ratio was calculated to compare risks before and after the intervention for the meta-analysis.22 | |
| Measures of urinary catheter use | Mean number of days of urinary catheter use per patient was recorded before and after the intervention, and a standardised mean difference was calculated to compare the two groups for the meta-analysis.22 |
| Percentage of patient days in which the catheter was in place (reported by the study directly, or calculated from ratio of catheter days/patient days if provided in the study), for the comparison group (before intervention or control group) and postintervention | |
| Percentage of patients studied who had a urinary catheter placed during the study period, for the comparison group (before intervention or control group) and postintervention | |
| Need for catheter replacement | Recatheterisation need was extracted as the number and percent of patients who required replacement of a catheter after prior removal of an indwelling catheter. |
What strategies may reduce unnecessary catheter use?
Strategies to avoid unnecessary placement of indwelling urinary catheters
Simply put, patients without urinary catheters do not develop CAUTI. Yet, multiple studies show that between 21% and 55.7%2 4 20 23–25 of urinary catheters are placed in patients who do not have an appropriate indication and, therefore, may not even need a catheter. Over the past decade, several studies have employed interventions to decrease unnecessary catheter placement (described in the online supplementary appendix table). Although educational interventions are a common and important first step to decrease inappropriate catheter use, more effective and potentially more sustainable interventions go a step further by instituting restrictions on catheter placement. Protocols that restrict catheter placement can serve as a constant reminder for providers about the appropriate use of catheters, can suggest alternatives to indwelling catheter use (such as condom catheters or intermittent straight catheterisation), but perhaps most importantly, can generate accountability for placement of each individual urinary catheter. A fairly typical approach for developing a catheter restriction protocol is to begin with a basic list of appropriate catheter uses (such as the list provided in the Centers for Disease Control and Prevention's Healthcare Infection Control Practices Advisory Committee (HICPAC) guideline14); this list (see box 1) can then be tailored to include other indications based on local opinion and specialised patient populations.
Box 1. Indications for indwelling urethral catheter use (from 2009 Centers for Disease Control and Prevention guideline14).
A. Examples of appropriate indications for indwelling urethral catheter use
Patient has acute urinary retention or bladder outlet obstruction
Need for accurate measurements of urinary output in critically ill patients
- Perioperative use for selected surgical procedures:
- Patients undergoing urologic or other surgery on contiguous structures of genitourinary tract
- Anticipated prolonged surgery duration; catheters inserted for this reason should be removed in postanesthesia care unit
- Patients anticipated to receive large-volume infusions or diuretics during surgery
- Need for intraoperative monitoring of urinary output
To assist in healing of open sacral or perineal wounds in incontinent patients
Patient requires prolonged immobilisation (eg, potentially unstable thoracic or lumbar spine, multiple traumatic injuries such as pelvic fractures)
To improve comfort for end-of-life care if needed
B. Examples of inappropriate uses of indwelling catheters
As a substitute for nursing care of the patient or resident with incontinence
As a means to obtain urine for culture or other diagnostic tests when patient can voluntarily void
For prolonged postoperative duration without appropriate indications (eg, structural repair of urethra or contiguous structures, prolonged effect of epidural anesthesia, etc.)
The technology required to implement catheter placement restrictions ranges from low-technology strategies, such as a hospital or unit policy on appropriate catheter placement, or preprinted catheter orders with limited indications, to higher-technology strategies, such as computerised orders24 26–28 for catheter placement. Catheter restriction protocols have been a common component of successful multimodal interventions to decrease catheter use and/or CAUTI rates, including hospital-wide24 interventions and interventions tailored for specific environments, such as the emergency department,23 29 inpatient units20 28 (including general medical26 30 31 surgical32 wards and ICU32–36), and in the periprocedural35 setting. Urinary retention protocols27 31 32 35–37 are a type of catheter restriction protocols that often incorporate the use of a portable bladder ultrasound27 28 31 35 37–41 to verify retention prior to catheterisation, and recommend use of intermittent catheterisation rather than indwelling catheters to manage a common and often temporary issue.
Strategies to prompt removal of unnecessary urinary catheters
Urinary catheters are commonly left in place when no longer needed.4 25 In most hospitals, four steps are required to remove a urinary catheter21: (1) a physician recognises the catheter is in place, (2) the physician recognises the catheter is no longer needed, (3) the physician writes the order to remove the catheter and (4) a nurse removes the catheter. Thus, by default, hours and sometimes days may pass before an unnecessary catheter is recognised and removed. Because every additional day of urinary catheter use increases the patient's risk of infectious42 complications, and catheter use is also associated with non-infectious43 catheter-related complications, interventions that facilitate prompt removal of unnecessary catheters can have a strong impact. We describe below the evidence regarding strategies that may accelerate or bypass some of these four steps to prompt catheter removal.
Perhaps the most important CAUTI prevention strategy after placement of the catheter is to maintain awareness of the catheter's existence (in lifecycle stage 2 of figure 1), as healthcare providers may be unaware the catheter is in place.5 Thus, a key step in prompting removal of unnecessary catheters is frequently (by day or by shift) reminding nurses and physicians that the catheter remains in place. Catheter reminder interventions include a daily checklist24 35 36 44–46 or verbal/written reminder34 47–51 to assess continued catheter need, a sticker reminder on the patient's chart38 52 53 or catheter bag,54 or an electronic24 reminder that a catheter is still in place. Reminder interventions can be generated by nurses, physicians or electronic order sets, and can be targeted to remind either nurses or physicians about the catheter. Some reminder interventions have employed nurses dedicated to detecting unnecessary catheters.24 38 Reminder interventions can also serve to remind clinicians of appropriate catheter indications.
Unfortunately, reminder interventions can also be easy to ignore52 and catheters may remain in place without action. The next type of intervention to prompt removal of unnecessary catheters which goes a step further, is a ‘stop order’ that requires action. Stop orders prompt the clinician (either nurse or physician) to remove the catheter by default after a certain time period has elapsed or condition has occurred, unless the catheter remains clinically appropriate. For example, catheter stop orders can be configured to ‘expire’ in the same fashion as restraint or antibiotic orders, unless action is taken by a clinician. Stop orders directed at physicians24 26 28 31 33 51 require an order to be renewed or discontinued on the basis of review at specific intervals, such as every 24–48 h after admission or postprocedure. Stop orders directed at nurses either require the nurse to obtain a catheter removal order from physicians,30 35 55 or can empower nurses to remove the catheter without requesting a physician order31 33 37 46 56–61 on the basis of an appropriate indication list. Admittedly, implementing a nurse-empowered catheter removal protocol may be less effective than anticipated, as early qualitative research of nurse-empowered interventions indicate some nurses are uncomfortable with this autonomy59 and might not remove catheters as expected.
Benefits and harms
What is the impact of strategies to avoid unnecessary urinary catheter use?
Impact of interventions to avoid unnecessary catheter placement
Multiple before-and-after studies have found that interventions to decrease inappropriate catheter placement (such as catheter placement restrictions and urinary retention protocols) have resulted in a decrease in the use of urinary catheters,23 24 27 28 31 32 34 36 46 62 a lower proportion of catheters in place without a physician order,23 24 26 29 and a reduction in the proportion of catheters in place without an appropriate indication.23 24 29 31
Impact of reminder and stop-order interventions on catheter use and CAUTIs
As an update to our prior systematic review and meta-analysis of 14 studies22 published prior to August 2008, this systematic review (through October 2012) identified a total of 30 studies employing reminders and/or stop orders to prompt removal of unnecessary urinary catheters that reported at least one CAUTI or urinary catheter use measure defined in table 1. Table 2 summarises each of these 30 studies, including the outcomes reported, and a brief summary of the interventions employed (with more details regarding the interventions provided in the online supplementary appendix table). The majority (28) of studies were prepost designs, including three32 50 52 with concurrent controls; one study57 was a randomised control trial (RCT) and one study was a non-randomised crossover trial.26
Table 2.
Summary of CAUTI and urinary catheter (UC) outcomes reported for studies with reminder or stop-order interventions, evaluated as potential studies to include in meta-analyses
| CAUTI outcomes | Indwelling urinary catheter use outcomes | |||||
|---|---|---|---|---|---|---|
| 1st author (year) | Interventions* | CAUTI per 1000 catheter days | % Patients who developed CAUTI | Mean days of UC use per patient | % Patient days with UC in use | % Patients with UC used |
| Adams (2010)60 | S | 25 → 7.6 | ||||
| Andreessen (2012)28 | P, S, B | 5.6 → 2.9† | All catheterised‡ | |||
| Apisarnthanarak (2007)47 | R | 21.5 → 5.2† | 11.0 → 3.0† | 82 → 84 | ||
| Bruminhent (2010)53 | R | 7.02 → 2.08†§ | All catheterised‡ | |||
| Cornia (2003)26 | P, S, E | 8.8 → 13.8 | 8.0 → 5.0† | All catheterised‡ | ||
| Crouzet (2007)48 | R | 12.3 → 1.8† | 10.6 → 1.1† | 8.4 → 6.7 | All catheterised‡ | |
| Dumigan (1998)33 | P, S, E | 14.3 → 9.2 | 74 → 76 | |||
| Elpern (2009)34 | P, R | 4.7 → 0† | All catheterised‡ | |||
| Fakih (2008)50 | R | 20 → 16† | ||||
| Fuchs (2011)35 | P, S | 2.88 → 1.46 | All catheterised‡ | |||
| Gotelli (2008)56 | S | 24.0 → 17.0 | ||||
| Huang (2004)49 | R | 11.5 → 8.3† | 3.8 → 2.4† | 7.0 → 4.6† | 74.5 → 76.2 | |
| Jain (2006)44 | R, B, A | 3.8 → 2.4 | ||||
| Knoll (2011)24 | P, R, S, B, O | Mean daily UC prevalence: 15.2 → 13.7§ | ||||
| Loeb (2008)57 | S | 2.1 → 2.1 | 5.0 → 3.7† | All catheterised‡ | ||
| Murphy (2007)54 | R, E | Reduced UTI rates by 30%, no details | ||||
| Reilly (2008)36 | P, R, E | 4.7 → 3.0 | 96 → 86 | All catheterised‡ | ||
| Robinson (2007)55 | S | 40.0 → 13.3 | 8.6 → 4.5 | |||
| Roser (2012)61 | P, S, O | CAUTI (details unclear): 45 → 28 | UC ‘Utilisation rates’: ICU: 84 → 68 (not further defined) MedSurg: 16 → 11 | |||
| Rothfield (2010)30 | P, S | 3.2 → 2.4 | 33.3 → 18.5† | 33.3 → 18.8 | ||
| Saint (2005)52 | R | 0.6 → 0.4† | 14 → 13 | |||
| Schultz (2011)37 | P, S | 90–95 → 76–84 | ||||
| Sequin (2010)51 | S | 5.0 → 4.9 | 4.3 → 3.0 | Median 5.0 → 4.0† | 92.7 → 91.2 | |
| Stephan (2006)32 | P, S, E | 45.8 → 18.6† | 5.0 → 3.9† | |||
| Titsworth (2012)46 | P, R, S, B, A, O | 13.3 → 4.0† | UC Utilisation rates of ICU beds with UCs:100 → 73 | |||
| Topal (2005)31 | P, S, E | 36.0 → 19.0† | 19.5 → 12.3 | 16 → 10† | ||
| Van den Broek (2011)38 | P, R, S, O | 12.6 → 12.7 | ICU/CCU: 25.6 → 16.2 Med: 14.9 → 12.5† Neuro: 15.8 → 15.7 Surg: 11.8 → 10.5† |
ICU/CCU: 74 → 81 Med: 14 → 14 Neuro: 20 → 19 Surg: 21 → 19† |
||
| Voss (2009)58 | S | 4.9 → 3.9 | 26 → 10 | 33 → 15.3 | ||
| Weitzel (2008)45 | R | 37 → 6.7 | 8.6 → 4.5 | |||
| Wenger (2010)59 | S, E, A | 2.26 → 1.02† | ||||
A grey-shaded table cell indicates that the outcome was not reported in the study.
*Intervention key (note: interventions described in more detail in online supplementary appendix table).
†Difference of p<0.05 reported between comparison group (before intervention or control) → postintervention group.
‡Not applicable, as only catheterised patients were included for these studies (so 100% catheterised).
§Reporting first published postintervention result, for this study that reported serial postintervention results.
P=Intervention to avoid unnecessary catheter Placement (eg, restricted indications of use, bladder scanner protocols, etc).
R=Reminder intervention that UC is still present, could be directed at either physician or nurse.
S=Stop order intervention, prompting/requiring removal of the UC based on time or clinical criteria.
E=Education regarding UC placement or maintenance.
B=Bladder bundle of interventions (which included UC placement, maintenance care standardisation).
A=Antimicrobial UCs.
O=Other CAUTI or catheter-related interventions, detailed in online supplementary appendix table.
CAUTI, catheter-associated urinary tract infection; CCU, coronary care units; ICU, intensive care units; UTI, urinary tract infection.
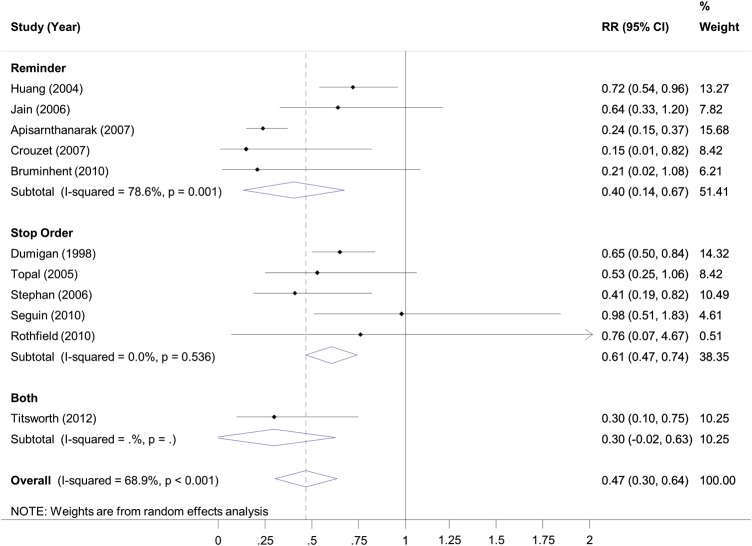
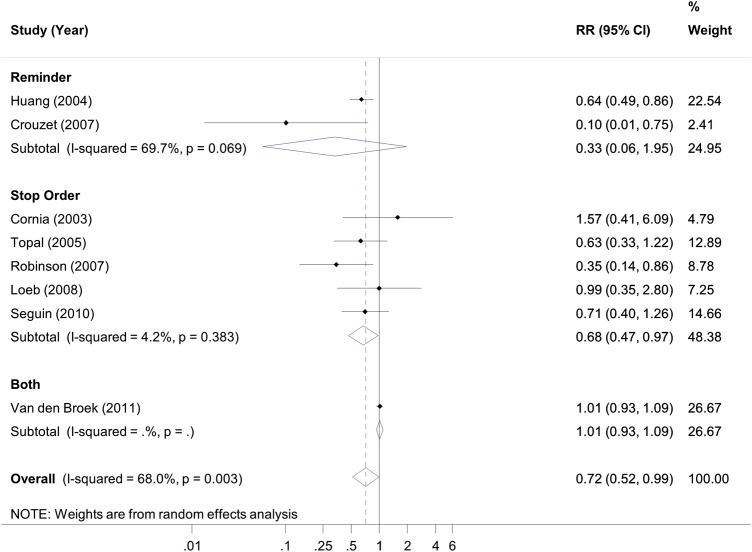
With very similar results to the prior22 meta-analysis, the updated meta-analysis using 11 studies (figure 2, stratified by reminder vs stop order, and also see online supplementary appendix figure, stratified by study's focus on intensive care patients) indicated the rate of CAUTI (episodes per 1000 catheter-days) was reduced by 53% (rate ratio 0.47; 95% CI 0.30 to 0.64, p<0.001) with use of a reminder or stop order, with five of these studies also including interventions to restrict initial catheter placement. Based on this updated meta-analysis, reminders and stop orders could result in large numbers of avoided CAUTI episodes per 1000 catheter-days, particularly when baseline rates of CAUTI are high (table 3). Eight studies provided sufficient detail for pooling of the cumulative risk of CAUTI during the study period; the risk ratio for CAUTI was 0.72 (95% CI 0.52 to 0.99; p=0.045) for the intervention versus comparison groups (figure 3).
Figure 2.
Meta-analysis of rate ratios for catheter-associated urinary tract infection episodes per 1000 catheter days, for intervention versus control groups, stratified by type of intervention to prompt catheter removal.
Table 3.
Number of avoided CAUTI episodes per 1000 catheter days
| Baseline rate of CAUTI episodes per 1000 catheter days | Number of avoided CAUTI episodes per 1000 catheter days anticipated by the type of intervention to prompt catheter removal | ||
|---|---|---|---|
| Reminder | Stop order | Overall | |
| 5 | 3.0 | 2.0 | 2.7 (95% CI 1.8 to 3.5) |
| 10 | 6.0 | 4.0 | 5.3 (95% CI 3.6 to 7.0) |
| 20 | 11.9 | 7.9 | 10.6 (95% CI 7.3 to 13.9) |
CAUTI, catheter-associated urinary tract infections.
Figure 3.
Meta-analysis of risk ratios for percentage of patients who developed catheter-associated urinary tract infection, for intervention versus control groups, stratified by type of intervention to prompt catheter removal.
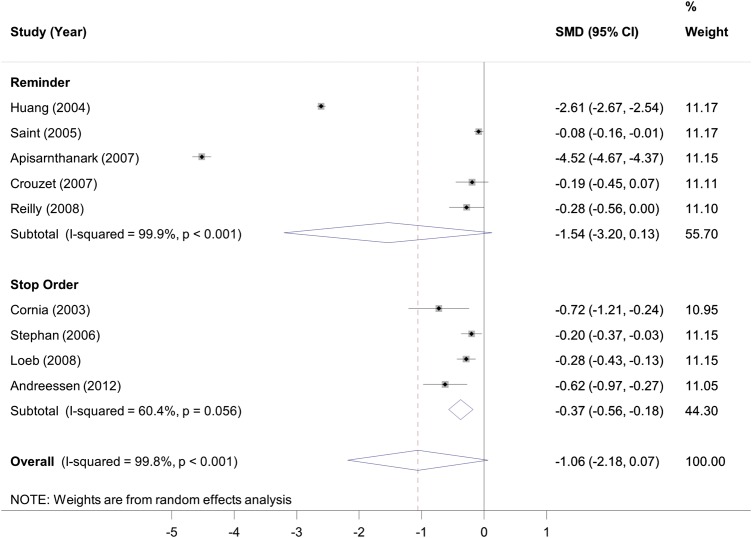
Using nine studies with sufficient detail for pooling (figure 4), the pooled standardised mean difference (SMD) in duration of catheterisation was −1.06 days overall (p=0.065) including a statistically significant decrease in studies that used a stop order (SMD −0.37; p<0.001) but not in those that used a reminder (SMD, −1.54; p=0.071). Many studies reported other outcomes for urinary catheter use (detailed in table 2), but none of the studies identified since the prior meta-analysis provided sufficient detail (eg, number of patients in intervention or control groups, and measures of variability such as SD) to update the prior meta-analyses for these other urinary catheter use outcomes.
Figure 4.
Meta-analysis of the standardised mean difference in days of urinary catheter use, for intervention versus control groups, stratified by type of intervention to prompt catheter removal.
The one RCT57 that used a urinary catheter stop order warrants further discussion. In this study focusing on catheterised general medicine patients, urinary catheter use decreased more in the 347 patients in the stop-order group compared to 345 patients receiving usual care by −1.34 days (95% CI −0.64 to −2.05 days, p<0.001). Unexpectedly, symptomatic CAUTI rates did not change, occurring in 2.1% of both stop-order and usual-care groups (p=0.99). Of note, Loeb et al did not report CAUTIs per 1000 catheter days, so these results could not be included in pooled rate ratios (figure 2), but were included in pooled risk ratios (figure 3). There are several potential reasons why a decrease in CAUTIs was not seen in this study, including high rates of antimicrobial use in both controls and stop-order groups (protective against CAUTI, and a variable not often reported in these comparative studies), and the possibility that a 1-day reduction in catheter use may not be sufficient to demonstrate an effect on the risk of UTI, although the effects on rates of UTI (by tracking catheter days) are not known.
Potential for unintended harm by catheter removal interventions
Interventions that facilitate removal of urinary catheters pose the risk of premature urinary catheter removal, with patients then requiring unnecessary recatheterisation; any catheterisation event is associated with procedure-related discomfort and other potential complications. Thus, monitoring the need for recatheterisation is important to avoid unintended patient harm. In the meta-analysis of reminder and stop-order studies, only four of the 14 studies reported rates of recatheterisation26 48 52 57 with low recatheterisation rates noted in both intervention and control groups. None of the 16 more recent studies involving reminders or stop orders to prompt catheter removal reported data on potential patient harm, such as premature removal.
Summary of other strategies to prevent CAUTI
Several recent evidence-based guidelines14–17 have focused on preventing CAUTI, and have assessed the evidence and provided recommendations for implementing prevention strategies. Key recommendations in the Centers for Disease Control and Prevention (CDC) guideline,14 in addition to appropriate catheter use (box 1), include (1) aseptic insertion of urinary catheters by properly trained personnel, using aseptic technique and sterile equipment (with an exception being that clean technique is appropriate for chronic intermittent catheterisation) and (2) proper urinary catheter maintenance with a sterile, closed drainage system permitting unobstructed urine flow. Aseptic insertion is primarily recommended as a standard of care for which limited evidence exists. Stronger evidence (epidemiological and clinical) supports the importance of a sterile, closed, unobstructed urinary drainage system.
A more controversial topic has been the use of antimicrobial catheters. Based on evidence available before 2010, the most recent CDC guideline recommended14 that antimicrobial catheters should not be used routinely to prevent CAUTI. It suggested that further research was needed both on the effect of silver-alloy-coated catheters in reducing the risk of clinically significant CAUTI outcomes, and on the benefit of silver-alloy-coated catheters in selected patients at high risk of infection. In November 2012, a long-awaited multicentre RCT demonstrated a lack of effectiveness of antimicrobial catheters (including silver-alloy and nitrofurazone-releasing catheters) to provide significant and clinically important reductions in symptomatic CAUTIs.63
Bundles of interventions are also an important strategy, as part of a multimodal approach that focuses efforts on high-yield interventions. For example, one strategy that includes several of the components from the bladder bundle implemented by the Michigan Health and Hospital Association (MHA) Keystone Center for Patient Safety & Quality is the ‘ABCDE’ approach19:
Adherence to general infection control principles is important (eg, hand hygiene, surveillance and feedback, aseptic insertion, proper maintenance, education).
Bladder ultrasound may avoid indwelling catheterisation.
Condom catheters or other alternatives to an indwelling catheter such as intermittent catheterisation should be considered in appropriate patients.
Do not use the indwelling catheter unless you must!
Early removal of the catheter using a reminder or nurse-initiated removal protocol appears warranted.
Several studies24 28 44 46 have included bladder bundles as interventions for decreasing catheter use and/or CAUTI rates, including a statewide initiative20 leading to significant increases in the proportion of catheters used for appropriate indications (from 44.3% to 57.6%, p=0.005).
Implementation considerations
What methods have been used to improve the implementation of interventions to prevent catheter-associated urinary tract infections?
Because reducing unnecessary catheter use often requires changing well-established habits and beliefs of nurses and physicians, the challenge of implementation should not be underestimated. To facilitate implementation of practices to prevent CAUTI, the Michigan Keystone Bladder Bundle Initiative19 20 used the Johns Hopkins University collaborative model for transformational change. This model is based, in part, on the ‘four Es’: Engage, Educate, Execute, Evaluate.64 During the ‘Engage’ and ‘Educate’ steps, hospitals were provided information in multiple formats and a toolkit describing the intervention steps and outcomes measures. In the ‘Execute’ step, the hospital was strongly encouraged to choose one nurse champion50 65 (eg, a case manager, nurse coordinator, or clinical nurse specialist) to lead the initiative and organise a bladder bundle team, including at least one physician, and to participate in workshops and conference calls with other participating hospitals to provide additional expert content and practical coaching. Also during the ‘Execute’ step, daily patient rounds (which in some hospitals were called a ‘catheter patrol’) were recommended to assess catheter presence and necessity, and provide feedback to specific units and re-evaluate strategies in progress. Hospitals were also encouraged to implement more active strategies for prevention, such as a catheter reminder system or promoting the use of catheter alternatives by developing protocols or making sure the necessary supplies were readily available. In the ‘Evaluate’ phase, hospitals were asked to assess improvements in catheter use and appropriateness according to specified indications and to address any barriers to progress and sustainability.
Implementation challenges within CAUTI prevention should be expected66 and managed accordingly. Qualitative assessment focusing on HAI prevention has identified two important potential barriers to HAI preventive efforts: ‘active resisters’ and ‘organisational constipators.’67 Active resisters are hospital personnel who vigorously and openly oppose changes in practice, as a matter of habit or culture (eg, ‘just not how they were trained’). Management of active resisters often requires those in authority to mandate compliance, collect data and provide feedback.67 A ‘champion’ who is influential, or a peer of the resisting staff, may also help to overcome active resistance.65 66 ‘Organisational constipators’ are usually mid-level or high-level executives who act as barriers to change by preventing or delaying certain actions needed to implement new practices.67 Strategies to address an organisational constipator are to include this person in early discussions to improve buy-in and motivation, working around the person, or replacing the constipator.
A unique challenge to expect when implementing urinary catheter removal strategies is reluctance by some nurses to remove the catheter,66 even when the nurse is ‘empowered’ to do so. In some cases, nurses may be active resisters due to disagreement with the catheter policy and/or a desire to avoid the inconveniences and increased frequency of patient contact required for the care of incontinence and catheter alternatives. There is also a competing pressure on nurses to mitigate development of hospital-acquired pressure ulcers—leading to perception that urinary catheters could lessen risk of skin breakdown despite being only indicated14 for patients with incontinence and open sacral wounds. Other nurses report they simply do not feel comfortable59 removing the catheter without explicit orders from the physician, which is ironic considering that many nurses place catheters without orders. Nursing comfort with catheter removal can be increased59 with peer support and education, and may be facilitated by directly addressing the workload concerns associated with the removal of indwelling catheters. Indeed, a survey of nurses30 during implementation of a nurse-empowered catheter removal protocol indicated increased nursing and patient satisfaction, despite the expected increase in workload. Recent successful and sustainable multimodal interventions to decrease catheter use including nurse-driven efforts had bedside nurses who, by survey,62 viewed themselves as responsible for evaluation of catheter presence and need, had confidence in their knowledge, and viewed physicians as receptive to their requests regarding catheter removal.
Even though CAUTI is a very common HAI, Krein and colleagues reported that CAUTI preventive practice use is lagging behind efforts to prevent central line-associated bloodstream infection and ventilator-associated pneumonia,68 with room for improvement in adopting catheter removal and CAUTI preventive strategies demonstrated again in two recent large surveys of hospitals69 and ICUs.70 Fortunately, many resources exist (http://www.catheterout.org) to help hospitals develop and implement programmes to decrease catheter use and prevent CAUTI, including a range of tools and educational materials to address implementation challenges. Hospital and unit-level leadership also play a key role in preventing infection.71
Monitoring and providing feedback on catheter use and CAUTI rates
Inappropriate urinary catheter use is an easy habit to start and a difficult one to break.21 Consequently, many studies20 33 have emphasised the importance of on-going surveillance and feedback as an intervention to reduce HAIs, such as CAUTI, and sustain20 24 62 prevention efforts. New national efforts to reduce CAUTI (http://www.onthecuspstophai.org/stop-cauti/) incorporate periodic feedback to participating units on urinary catheter use and CAUTI rates. The CAUTI rates evaluated include the National Healthcare Safety Network (NHSN) and the newly described population-based rates.72 The population-based CAUTI rate incorporates both the NHSN rate and the device utilization ratio, to account for interventions focused on reduction in catheter use and improvements in placement and maintenance.
Important next steps to address CAUTI involve developing strategies to decrease the effort, and resources required to monitor catheter use and CAUTI rates. Advanced informatics tools have recently been shown to increase the impact of this feedback loop to the extent that rates of CAUTI were lower in facilities that deployed these tools compared to those that did not.73 Careful selection or development of datasets used for implementing hospital payment changes and public reporting for CAUTI events is also recommended. Unfortunately, the current administrative data used to implement non-payment11 for hospital-acquired CAUTIs, and to publicly report hospital performance, likely captures few CAUTI events, given documentation and coding challenges74 to translate a UTI event from a medical record into hospital-acquired CAUTI in the administrative datasets.
What is the cost of implementing a CAUTI prevention program?
The cost of implementing a CAUTI prevention programme will vary based on the level of technology used (eg, computerised vs preprinted catheter orders, and whether portable bladder ultrasounds are purchased) and the time invested in implementing and evaluating the interventions. Saint and colleagues, in their study of a written urinary catheter reminder generated by a research nurse to remind physicians which of their inpatients had urinary catheters,52 found that the intervention was either cost-neutral or modestly cost-saving depending on the assumptions made. More recently, a study38 of five hospitals in The Netherlands employed a multimodal intervention including reminders in four hospitals, and a stop order in the fifth hospital. The programme was found to be cost saving, with the mean amount saved being €537 (or ∼US$700) per 100 hospitalised patients.
Discussion
In summary, healthcare providers should strongly consider employing interventions to avoid unnecessary catheter placement (such as catheter placement restrictions) and to prompt removal of unnecessary catheters by reminders and stop orders, with special consideration for nurse-initiated removal protocols. The strength of the evidence is moderate to high. These interventions appear to be low cost, low risk, effective and sustainable20 24 62 strategies to address a common hospital-acquired infection in the USA, with some unique but not impossible challenges for implementation. Moreover, UTIs are increasingly caused by multidrug-resistant organisms (MDROs) including strains that are resistant to all available therapeutic agents;75 76 preventing CAUTI may help patients avoid MDRO infection.
Identifying and supporting an appropriate ‘champion’ who is influential among staff can be crucial to help overcome resistance to change behaviour regarding catheter use and facilitate the adoption of preventive strategies. Monitoring and providing feedback of catheter use and CAUTI rates is important in the implementation and continued use of CAUTI preventive strategies. Furthermore, reducing indwelling catheter use addresses the non-infectious complications of urinary catheter use such as catheter-related patient discomfort and immobility. Unfortunately, hospitals’ surveys have repeatedly demonstrated low and only slowly improving adoption of CAUTI preventive strategies, such as reminders, stop orders and condom catheters compared to higher rates of adoption of antimicrobial urinary catheters in non-federal hospitals.68 Yet, the negative results of a recent randomised controlled trial on the effectiveness of antimicrobial urinary catheters63 is expected to translate into reduced use of these catheters.
Interest and resources for preventing CAUTI is likely to grow due to expanding national initiatives focused on reducing hospital-acquired infections, including CAUTI, being implemented with a combination of mandated public reporting and reduced pay to hospitals. Current prevention efforts include a 50-state initiative—‘On the CUSP: Stop CAUTI’—that is funded by the AHRQ and led by the Health Research and Educational Trust (HRET) of the American Hospital Association. AHRQ has made available a toolkit for CAUTI prevention (http://www.onthecuspstophai.org/on-the-cuspstop-cauti/toolkits-and-resources/). This initiative is providing resources and implementation expertise to hospitals and state organisations that are beginning CAUTI prevention programmes, with a goal of reducing CAUTI rates by 25% by focusing on high-yield interventions such as those reducing urinary catheter use.
Key summary points.
Multiple before-and-after studies have found that interventions to decrease inappropriate catheter placement (such as catheter placement restrictions or urinary retention protocols) have resulted in decreased catheter use, fewer catheters in place without physician orders, and fewer catheters in place without an appropriate indication.
An updated systematic review and meta-analysis found that catheter reminders or stop orders decreased catheter-associated urinary tract infections (CAUTIs) by 53%. An updated literature review identified many recent interventions with reminders or stop orders reducing CAUTI rates and/or urinary catheter use.
Bundles of interventions focusing on strategies to reduce unnecessary catheter use (by avoiding unnecessary placement and prompting removal) and decrease CAUTI rates by general infection control principles (hand hygiene, surveillance/feedback, aseptic insertion, etc) have been successful, particularly when coupled with implementation strategies to address common barriers encountered when trying to change well-established habits of physicians and nurses.
The role of antimicrobial catheters in preventing CAUTI has been addressed by a recent large randomised controlled trial showing no significant additional benefit in reducing symptomatic CAUTIs.
CAUTI prevention costs vary by programme, but such programmes have been demonstrated to be cost saving.
Supplementary Material
Acknowledgments
We thank Andrew Hickner, MSI, for conducting the update of the literature search and for providing assistance with references and manuscript editing, and Whitney Townsend, MLIS, for performing the literature search for the original22 systematic review.
Footnotes
Contributors: JM and SS designed the systematic review, conceived the manuscript, and assembled the authorship team. JM performed the systematic review and abstracted the data required for the review overall (as summarised in text and tables) and the meta-analysis, and wrote the first draft of the manuscript. JM and MAMR had full access to the data reviewed and analysed for this study; MAMR conducted the meta-analysis, and interpreted the results. JM and MAMR take responsibility for the integrity and accuracy of the data for the meta-analysis; JM (the guarantor) also takes responsibility for the integrity and accuracy of all data summarised in the manuscript. MAMR and SS also reviewed and revised the manuscript critically for important intellectual content. SLK, MGF, and RNO also contributed substantially to design of the manuscript, and reviewed and edited the manuscript for important intellectual content. All authors approved the final version to be published.
Funding: This work was supported by funding from the Agency for Healthcare Research and Quality (AHRQ), US Department of Health and Human Services (Contract No. HHSA-290-2007-10062I). AHRQ reviewed contract deliverables to ensure adherence to contract requirements and quality, and a copyright release was obtained from AHRQ prior to submission of this manuscript.
Competing interests: Some of the authors have also received grant support from the Agency for Healthcare Research and Quality (AHRQ Award 1R010HS018344-01A1 to JM, MAMR and SS, and Award 1K08-HS019767-01 to JM) and the National Institute of Diabetes and Digestive and Kidney Diseases (Award R21-DK078717, to SS), and the National Institute of Nursing Research (Award R01-NR010700, to SLK and SS). JM is a recipient of the National Institutes of Health Clinical Loan Repayment Program for 2009 to 2013. Authors have also received support for the development and implementation of the ‘On the CUSP: Stop CAUTI’ Initiative serving as members of the National Leadership Team (SK, MGF, SS), technical expert panel (RNO), and core national faculty (JM, RNO, MAMR), through a subcontract with Health Research and Educational Trust through AHRQ. MGF also receives support from the Ascension Health Hospital Engagement Network effort to prevent healthcare-associated infections and Michigan Health & Hospital Association Hospital Engagement Network to reduce CAUTI. RNO is also a member of speakers’ bureau for Ethicon, Inc., Sage Products and Avid Education Partners, LLC; and serves as a consultant to Premier Inc, and previously served as a consultant for Bard Medical. SS has received numerous honoraria and speaking fees from academic medical centres, hospitals, specialty societies, state-based hospital associations, group-purchasing organisations (eg, VHA, Premier), and non-profit foundations (eg, Michigan Health and Hospital Association, Institute for Healthcare Improvement) for lectures about catheter-associated urinary tract infection and implementation science. JM has received numerous honoraria from academic medical centers, hospitals, specialty societies and state-based hospital associations for lectures related to catheter-associated urinary tract infection. Author(s) declare no competing financial interests exist. All statements expressed in this work are those of the authors and should not in any way be construed as official opinions or positions of the RAND Corporation, US Department of Veterans Affairs, AHRQ, or the US Department of Health and Human Services.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Saint S, Lipsky BA, Baker PDet al. Urinary catheters: what type do men and their nurses prefer? J Am Geriatr Soc 1999;47:1453–7 [DOI] [PubMed] [Google Scholar]
- 2.Gokula RR, Hickner JA, Smith MA. Inappropriate use of urinary catheters in elderly patients at a midwestern community teaching hospital. Am J Infect Control 2004;32:196–9 [DOI] [PubMed] [Google Scholar]
- 3.Fakih MG, Shemes SP, Pena MEet al. Urinary catheters in the emergency department: very elderly women are at high risk for unnecessary utilization. Am J Infect Control 2010;38:683–8 [DOI] [PubMed] [Google Scholar]
- 4.Jain P, Parada JP, David Aet al. Overuse of the indwelling urinary tract catheter in hospitalized medical patients. Arch Intern Med 1995;155:1425–9 [PubMed] [Google Scholar]
- 5.Saint S, Wiese J, Amory JKet al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med 2000;109:476–80 [DOI] [PubMed] [Google Scholar]
- 6.Klevens RM, Edwards JR, Richards CL, Jret al. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep 2007;122:160–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scott R. The direct medical costs of healthcare-associated infections in US hospitals and the benefits of prevention. March 2009. Publication No. CS200891-A. http://www.cdc.gov/hai/pdfs/hai/scott_costpaper.pdf; (accessed 10 May 2013).
- 8.Anderson DJ, Kirkland KB, Kaye KSet al. Underresourced hospital infection control and prevention programs: penny wise, pound foolish?. Infect Control Hosp Epidemiol 2007;28:767–73 [DOI] [PubMed] [Google Scholar]
- 9.Tambyah PA, Knasinski V, Maki DG. The direct costs of nosocomial catheter-associated urinary tract infection in the era of managed care. Infect Control Hosp Epidemiol 2002;23:27–31 [DOI] [PubMed] [Google Scholar]
- 10.Greene MT, Chang R, Kuhn Let al. Predictors of hospital-acquired urinary tract-related bloodstream infection. Infect Control Hosp Epidemiol 2012;33:1001–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Department of Health and Human Services, Centers for Medicare & Medicaid Services. Medicare program; changes to the hospital inpatient prospective payment systems and fiscal year 2009 rates. Fed Regist 2008;73:48473–91 [Google Scholar]
- 12.Cardo D, Dennehy PH, Halverson Pet al. Moving toward elimination of healthcare-associated infections: a call to action. Am J Infect Control 2010;38:671–5 [DOI] [PubMed] [Google Scholar]
- 13.Department of Health and Human Services (HHS) HHS Action Plan to Prevent Healthcare-Associated Infections, Appendix G 2009. http://www.hhs.gov/ash/initiatives/hai/appendices.html#appendix_g (accessed 8 Dec 2012).
- 14.Gould CV, Umscheid CA, Agarwal RKet al. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol 2010;31:319–26 [DOI] [PubMed] [Google Scholar]
- 15.Hooton TM, Bradley SF, Cardenas DDet al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis 2010;50:625–63 [DOI] [PubMed] [Google Scholar]
- 16.Lo E, Nicolle L, Classen Det al. Strategies to prevent catheter-associated urinary tract infections in acute care hospitals. Infect Control Hosp Epidemiol 2008;29(Suppl 1):S41–50 [DOI] [PubMed] [Google Scholar]
- 17.Greene L, Marx J, Oriola S. An APIC Guide to the elimination of catheter-associated urinary tract infections (CAUTIs): developing and applying facility-based prevention interventions in acute and long-term care settings 2008. http://www.apic.org/Resource_/EliminationGuideForm/c0790db8-2aca-4179-a7ae-676c27592de2/File/APIC-CAUTI-Guide.pdf (accessed 8 Dec 2012).
- 18.Saint S. Chapter 15. Prevention of Nosocomial Urinary Tract Infections. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evidence Report/Technology Assessment. Vol 43 AHRQ Publication No. 01-E058. Rockville, MD: Agency for Healthcare Research and Quality, 2001:149–62. http://www.ahrq.gov/clinic/ptsafety/pdf/chap15.pdf (accessed 8 Dec 2012). [Google Scholar]
- 19.Saint S, Olmsted RN, Fakih MGet al. Translating health care-associated urinary tract infection prevention research into practice via the bladder bundle. Jt Comm J Qual Patient Saf 2009;35:449–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fakih MG, Watson SR, Greene MTet al. Reducing inappropriate urinary catheter use: a statewide effort. Arch Intern Med 2012;172:255–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meddings J, Saint S. Disrupting the life cycle of the urinary catheter. Clin Infect Dis 2011;52:1291–3 [DOI] [PubMed] [Google Scholar]
- 22.Meddings J, Rogers MA, Macy Met al. Systematic review and meta-analysis: reminder systems to reduce catheter-associated urinary tract infections and urinary catheter use in hospitalized patients. Clin Infect Dis 2010;51:550–60 [DOI] [PubMed] [Google Scholar]
- 23.Fakih MG, Pena ME, Shemes Set al. Effect of establishing guidelines on appropriate urinary catheter placement. Acad Emerg Med 2010;17:337–40 [DOI] [PubMed] [Google Scholar]
- 24.Knoll BM, Wright D, Ellingson Let al. Reduction of inappropriate urinary catheter use at a Veterans Affairs hospital through a multifaceted quality improvement program. Clin Infect Dis 2011;52:1283–90 [DOI] [PubMed] [Google Scholar]
- 25.Gardam MA, Amihod B, Orenstein Pet al. Overutilization of indwelling urinary catheters and the development of nosocomial urinary tract infections. Clin Perform Qual Health Care 1998;6:99–102 [PubMed] [Google Scholar]
- 26.Cornia PB, Amory JK, Fraser Set al. Computer-based order entry decreases duration of indwelling urinary catheterization in hospitalized patients. Am J Med 2003;114:404–7 [DOI] [PubMed] [Google Scholar]
- 27.Patrizzi K, Fasnacht A, Manno M. A collaborative, nurse-driven initiative to reduce hospital-acquired urinary tract infections. J Emerg Nurs 2009;35:536–9 [DOI] [PubMed] [Google Scholar]
- 28.Andreessen L, Wilde MH, Herendeen P. Preventing catheter-associated urinary tract infections in acute care: the bundle approach. J Nurs Care Qual 2012;27:209–17 [DOI] [PubMed] [Google Scholar]
- 29.Gokula RM, Smith MA, Hickner J. Emergency room staff education and use of a urinary catheter indication sheet improves appropriate use of foley catheters. Am J Infect Control 2007;35:589–93 [DOI] [PubMed] [Google Scholar]
- 30.Rothfeld AF, Stickley A. A program to limit urinary catheter use at an acute care hospital. Am J Infect Control 2010;38:568–71 [DOI] [PubMed] [Google Scholar]
- 31.Topal J, Conklin S, Camp Ket al. Prevention of nosocomial catheter-associated urinary tract infections through computerized feedback to physicians and a nurse-directed protocol. Am J Med Qual 2005;20:121–6 [DOI] [PubMed] [Google Scholar]
- 32.Stephan F, Sax H, Wachsmuth Met al. Reduction of urinary tract infection and antibiotic use after surgery: a controlled, prospective, before-after intervention study. Clin Infect Dis 2006;42:1544–51 [DOI] [PubMed] [Google Scholar]
- 33.Dumigan DG, Kohan CA, Reed CRet al. Utilizing national nosocomial infection surveillance system data to improve urinary tract infection rates in three intensive-care units. Clin Perform Qual Health Care 1998;6:172–8 [PubMed] [Google Scholar]
- 34.Elpern EH, Killeen K, Ketchem Aet al. Reducing use of indwelling urinary catheters and associated urinary tract infections. Am J Crit Care 2009;18:535–41; quiz 542 [DOI] [PubMed] [Google Scholar]
- 35.Fuchs MA, Sexton DJ, Thornlow DKet al. Evaluation of an evidence-based, nurse-driven checklist to prevent hospital-acquired catheter-associated urinary tract infections in intensive care units. J Nurs Care Qual 2011;26:101–9 [DOI] [PubMed] [Google Scholar]
- 36.Reilly L, Sullivan P, Ninni Set al. Reducing foley catheter device days in an intensive care unit: using the evidence to change practice. AACN Adv Crit Care 2006;17:272–83 [DOI] [PubMed] [Google Scholar]
- 37.Schultz P, Aljawawdeh A, Hopp T. EB105: Reducing use of indwelling urinary catheters with a nurse-driven protocol. Crit Care Nurse 2011;31:e42–e42 (Abstract) [Google Scholar]
- 38.van den Broek PJ, Wille JC, van Benthem BHBet al. Urethral catheters: can we reduce use? BMC Urology 2011;11:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee YY, Tsay WL, Lou MFet al. The effectiveness of implementing a bladder ultrasound programme in neurosurgical units. J Adv Nurs 2007;57:192–200 [DOI] [PubMed] [Google Scholar]
- 40.Frederickson M, Neitzel JJ, Miller EHet al. The implementation of bedside bladder ultrasound technology: effects on patient and cost postoperative outcomes in tertiary care. Orthop Nurs 2000;19:79–87 [DOI] [PubMed] [Google Scholar]
- 41.Slappendel R, Weber EW. Non-invasive measurement of bladder volume as an indication for bladder catheterization after orthopaedic surgery and its effect on urinary tract infections. Eur J Anaesthesiol 1999;16:503–6 [DOI] [PubMed] [Google Scholar]
- 42.Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med 2002;113(Suppl 1A):5S–13S [DOI] [PubMed] [Google Scholar]
- 43.Aaronson DS, Wu AK, Blaschko SDet al. National incidence and impact of noninfectious urethral catheter related complications on the Surgical Care Improvement Project. J Urol 2011;185:1756–60 [DOI] [PubMed] [Google Scholar]
- 44.Jain M, Miller L, Belt Det al. Decline in ICU adverse events, nosocomial infections and cost through a quality improvement initiative focusing on teamwork and culture change. Qual Saf Health Care 2006;15:235–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Weitzel T. To cath or not to cath? Nursing 2008;38:20–1 [DOI] [PubMed] [Google Scholar]
- 46.Titsworth WL, Hester J, Correia Tet al. Reduction of catheter-associated urinary tract infections among patients in a neurological intensive care unit: a single institution's success. J Neurosurg 2012;116:911–20 [DOI] [PubMed] [Google Scholar]
- 47.Apisarnthanarak A, Thongphubeth K, Sirinvaravong Set al. Effectiveness of multifaceted hospitalwide quality improvement programs featuring an intervention to remove unnecessary urinary catheters at a tertiary care center in Thailand. Infect Control Hosp Epidemiol 2007;28:791–8 [DOI] [PubMed] [Google Scholar]
- 48.Crouzet J, Bertrand X, Venier AGet al. Control of the duration of urinary catheterization: impact on catheter-associated urinary tract infection. J Hosp Infect 2007;67:253–7 [DOI] [PubMed] [Google Scholar]
- 49.Huang WC, Wann SR, Lin SLet al. Catheter-associated urinary tract infections in intensive care units can be reduced by prompting physicians to remove unnecessary catheters. Infect Control Hosp Epidemiol 2004;25:974–8 [DOI] [PubMed] [Google Scholar]
- 50.Fakih MG, Dueweke C, Meisner Set al. Effect of nurse-led multidisciplinary rounds on reducing the unnecessary use of urinary catheterization in hospitalized patients. Infect Control Hosp Epidemiol 2008;29:815–19 [DOI] [PubMed] [Google Scholar]
- 51.Seguin P, Laviolle B, Isslame Set al. Effectiveness of simple daily sensitization of physicians to the duration of central venous and urinary tract catheterization. Intensive Care Med 2010;36:1202–6 [DOI] [PubMed] [Google Scholar]
- 52.Saint S, Kaufman SR, Thompson Met al. A reminder reduces urinary catheterization in hospitalized patients. Jt Comm J Qual Patient Saf 2005;31:455–62 [DOI] [PubMed] [Google Scholar]
- 53.Bruminhent J, Keegan M, Lakhani Aet al. Effectiveness of a simple intervention for prevention of catheter-associated urinary tract infections in a community teaching hospital. Am J Infect Control 2010;38:689–93 [DOI] [PubMed] [Google Scholar]
- 54.Murphy D, Francis K, Litzenberger Met al. Reducing urinary tract infection: a nurse-initiated program. Pa Nurse 2007;62:20. [PubMed] [Google Scholar]
- 55.Robinson S, Allen L, Barnes MRet al. Development of an evidence-based protocol for reduction of indwelling urinary catheter usage. Medsurg Nurs 2007;16:157–61 [PubMed] [Google Scholar]
- 56.Gotelli JM, Merryman P, Carr Cet al. A quality improvement project to reduce the complications associated with indwelling urinary catheters. Urologic Nursing 2008;28:465–7 [PubMed] [Google Scholar]
- 57.Loeb M, Hunt D, O'Halloran Ket al. Stop orders to reduce inappropriate urinary catheterization in hospitalized patients: a randomized controlled trial. J Gen Intern Med 2008;23:816–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Voss AB. Incidence and duration of urinary catheters in hospitalized older adults: before and after implementing a geriatric protocol. J Gerontol Nurs 2009;35:35–41 [DOI] [PubMed] [Google Scholar]
- 59.Wenger JE. Cultivating quality: reducing rates of catheter-associated urinary tract infection. Am J Nurs 2010;110:40–5 [DOI] [PubMed] [Google Scholar]
- 60.Adams D, Bucior H, Day Get al. HOUDINI: make that urinary catheter disappear—nurse-led protocol. J Infect Prev 2012;13:44–6 [Google Scholar]
- 61.Roser L, Altpeter T, Anderson Det al. A nurse driven Foley catheter removal protocol proves clinically effective to reduce the incidents of catheter related urinary tract infections. Am J Infect Control 2012;40:e92–93 (Abstract) [Google Scholar]
- 62.Fakih MG, Rey JE, Pena MEet al. Sustained reductions in urinary catheter use over 5 years: Bedside nurses view themselves responsible for evaluation of catheter necessity. Am J Infect Control 2013;41:236–9 [DOI] [PubMed] [Google Scholar]
- 63.Pickard R, Lam T, Maclennan Get al. Antimicrobial catheters for reduction of symptomatic urinary tract infection in adults requiring short-term catheterisation in hospital: a multicentre randomised controlled trial. Lancet 2012;380:1927–35 [DOI] [PubMed] [Google Scholar]
- 64.Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ 2008;337:a1714. [DOI] [PubMed] [Google Scholar]
- 65.Damschroder LJ, Banaszak-Holl J, Kowalski CPet al. The role of the champion in infection prevention: results from a multisite qualitative study. Qual Saf Health Care 2009;18:434–40 [DOI] [PubMed] [Google Scholar]
- 66.Saint S, Kowalski CP, Forman Jet al. A multicenter qualitative study on preventing hospital-acquired urinary tract infection in US hospitals. Infect Control Hosp Epidemiol 2008;29:333–41 [DOI] [PubMed] [Google Scholar]
- 67.Saint S, Kowalski CP, Banaszak-Holl Jet al. How active resisters and organizational constipators affect health care-acquired infection prevention efforts. Jt Comm J Qual Patient Saf 2009;35:239–46 [DOI] [PubMed] [Google Scholar]
- 68.Krein SL, Kowalski CP, Hofer TPet al. Preventing hospital-acquired infections: a national survey of practices reported by U.S. hospitals in 2005 and 2009. J Gen Intern Med 2012;27:773–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fink R, Gilmartin H, Richard Aet al. Indwelling urinary catheter management and catheter-associated urinary tract infection prevention practices in Nurses Improving Care for Healthsystem Elders hospitals. Am J Infect Control 2012;40:715–20 [DOI] [PubMed] [Google Scholar]
- 70.Conway LJ, Pogorzelska M, Larson Eet al. Adoption of policies to prevent catheter-associated urinary tract infections in United States intensive care units. Am J Infect Control 2012;40:705–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Saint S, Kowalski CP, Banaszak-Holl Jet al. The importance of leadership in preventing healthcare-associated infection: results of a multisite qualitative study. Infect Control Hosp Epidemiol 2010;31:901–7 [DOI] [PubMed] [Google Scholar]
- 72.Fakih MG, Todd Greene M, Kennedy EHet al. Introducing a population-based outcome measure to evaluate the effect of interventions to reduce catheter-associated urinary tract infection. Am J Infect Control 2012;40:359–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Palumbo AJ, Loveless PA, Moll MEet al. Evaluation of healthcare-associated infection surveillance in Pennsylvania hospitals. Infect Control Hosp Epidemiol 2012; 33:105–11 [DOI] [PubMed] [Google Scholar]
- 74.Meddings J, Saint S, McMahon LF., Jr Hospital-acquired catheter-associated urinary tract infection: documentation and coding issues may reduce financial impact of Medicare's new payment policy. Infect Control Hosp Epidemiol 2010;31:627–33 [DOI] [PubMed] [Google Scholar]
- 75.Centers for Disease Control and Prevention (CDC) Carbapenem-Resistant Enterobacteriaceae Containing New Delhi Metallo-Beta-Lactamase in Two Patients—Rhode Island. MMWR Morb Mortal Wkly Rep 2012;61:446–8 [PubMed] [Google Scholar]
- 76.Marchaim D, Chopra T, Bogan Cet al. The burden of multidrug-resistant organisms on tertiary hospitals posed by patients with recent stays in long-term acute care facilities. Am J Infect Control 2012;40:760–5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.