Abstract
Objective
Although oral health (OH) problems are common during pregnancy, little is known about individual characteristics or behaviors relating to clinically assessed OH during pregnancy. This cross-sectional study describes the clinical OH status of a sample of pregnant women, examines relationships between sociodemographic factors and OH, behavioral factors and OH, and the influence of behavior on the relationships between sociodemographic clusters and OH. Baseline data were utilized from a pilot intervention study promoting OH during pregnancy.
Methods
Participants (n=99), recruited from CenteringPregnancy® prenatal care groups completed: questionnaires addressing race/ethnicity, income, education, dental insurance, oral hygiene practices, and dental care utilization; and clinical examinations for periodontal probing depths (PD), bleeding on probing (BOP), plaque assessment, and visual detection of untreated decay. Chi-squares and one-way ANOVAs with Tukey’s Studentized Range Test of planned comparisons were conducted to examine bivariable relationships between both sociodemographic and behavioral characteristics to OH status. Multivariable logistic regression analyses tested whether the effects of sociodemographic variables on OH status might be mediated by behaviors, including self-reported oral hygiene and recent dental visits.
Results
Forty-five percent of the sample had untreated decay and the mean percentage of sites with BOP=18%. Bivariable analyses of sociodemographic factors indicated that compared to Whites, Hispanic women had greater % of sites with: BOP, PD ≥5mm plus BOP, and Plaque Index (PI) scores of ≥2, all p=0.05; and greater untreated decay (Chi-square 13.3, p<0.001). Lower income was related to greater untreated decay (Chi-square 7.6, p<0.01). Compared to the highest education level, the lowest level group had higher % BOP, p<0.05. Public dental insurance (versus private) was associated with greater % BOP, PD ≥5mm plus BOP, both p<0.05, and greater untreated decay (Chi-square 16.9, p<0.001). Regarding behaviors, lacking a past 6 month dental visit was related to greater: BOP, PD ≥5mm plus BOP, and PI ≥2 (F range 6.2–8.7, p<0.01–0.05); and greater untreated decay (Chi-square 12.0, p<0.001). Self-reported optimal oral hygiene was related to lower % BOP and PD ≥5mm plus BOP (F range 4.5–6.7, both p<0.05). Mediation analyses indicated that there were significant indirect effects of racial/ethnic differences on OH outcomes via having a recent dental visit (OR range 1.2–1.9). However, significant differences between the Hispanic and White groups remained.
Conclusions
This study highlights sociodemographic disparities in clinical OH during pregnancy, the importance of dental care, and provides useful findings for tailoring interventions for expectant mothers and their infants.
Introduction
Pregnancy marks a time of significant physiological changes throughout the body, including a higher susceptibility to periodontal disease (1). Hormonal, immunological and vascular changes may exacerbate gingival inflammation in response to irritants such as plaque, resulting in “pregnancy gingivitis” in 60–70% of women (2, 3). Severity increases around the 2nd month of pregnancy, peaking in the 8th month (4). While these changes confer vulnerability in oral health (OH) to all women during pregnancy, many factors independent of pregnancy may also play an important role. Three key domains present in some conceptual models of health (5–7) include personal characteristics (e.g., demographics, socioeconomic status), health behaviors (e.g., health practices and health care utilization), and the broader social context and environment (e.g., health care system). The complex and dynamic interactions among these influences and their resulting impact on OH status for pregnant women are not well understood.
Racial/ethnic and socioeconomic factors associated with OH status are well documented in the general U.S. population, highlighting that minority and lower-income groups have poorer OH (8–10). However, little has been reported on sociodemographic disparities in clinically assessed OH within the U.S. population of pregnant women. One clinical study of periodontal status during pregnancy found that black women were more likely than white women to have periodontal disease (11). Other studies have identified similar racial/ethnic- (12) and income-related disparities (12, 13), however these studies rely on self-reported OH status.
The influence of health behaviors, including health practices and health care utilization, on health status is well established. OH behaviors during pregnancy have been linked to improved OH: plaque removal through proper oral hygiene self-care can minimize the level of gingival inflammation (14); and utilizing professional dental care during pregnancy improves periodontal health (15, 16). Some health behavior models place utilization of care or access to care in a proximal position to health outcomes, suggesting that the effects of other factors including personal characteristics may be influenced through or mediated by health care utilization. (6, 7, 17). Several large population-based surveys of pregnant women show low OH care utilization and disparities by sociodemographic characteristics (13, 18–20). These disparities suggest that utilization may play a mediating role between sociodemographic factors and OH status.
The paucity of studies of clinically assessed OH during pregnancy and related factors creates a gap in the ability to fully understand and address the OH needs of this population. Also lacking is research utilizing mediation analyses that could provide a more comprehensive view of relationships between sociodemographic factors and OH status and how behavioral factors, such as OH hygiene practices and dental care utilization might affect those relationships. To address these gaps, the objectives of this study are to: 1) describe the clinical OH status of a group of pregnant women; using the Andersen Model (6) as a guide 2) examine bivariable relationships between sociodemographic, behavioral characteristics and OH status (gingival status, plaque levels, and untreated decay); and 3) examine whether the effects of sociodemographic factors related to OH status are mediated by OH behaviors (brushing and flossing, recent dental visit). We hypothesized that: 1) non-white women and those of low socioeconomic status will have poorer clinically assessed OH compared to their white and higher socioeconomic status counterparts; and 2) two OH behaviors, oral hygiene practices and dental care utilization, mediate associations between sociodemographic factors and OH status.
Methods
Baseline data were used from the CenteringPregnancy® Oral Health Promotion (CPOP) study, a pilot project testing an OH educational intervention for pregnant women attending CenteringPregnancy® (CP®), a group prenatal care program consisting of 10 sessions. CPOP was approved by the University of California San Francisco’s Committee on Human Research and California Pacific Medical Center’s Institutional Review Board.
Women attending 4 CP® sites (2 intervention and 2 control, each with one English- and one Spanish-language site) in the San Francisco Bay Area were recruited and consented for the CPOP study (baseline n=99) during the first or second CP® session in person by study staff. Study procedures were explained, including dental examinations and questionnaires for all participants, and the addition of 2 brief OH education sessions for women in the intervention groups. Questionnaires (available upon request) included sociodemographic information, self-reported OH status, knowledge, attitudes, and behaviors. Items used in the present analysis included age, race/ethnicity, family income, insurance status, level of education, oral hygiene practices, and dental care utilization. Questionnaire items were drawn from validated surveys, including the National Health and Nutrition Examination Survey, the National Health Interview Survey, and the Maternal and Infant Health Assessment (MIHA) (21). The questionnaire was translated from English into Spanish (Mexican) by a professional translation service and back translated by a native Spanish-speaking research assistant. Prior to use, the questionnaire was reviewed by Spanish speaking CP® women in a focus group and was found to be acceptable and easy to understand. The research assistant was trained on the questionnaire administration and evaluated through practice sessions. Questionnaires were administered in person (91%) or over the phone (9%) in English or Spanish, using the Questionnaire Development System software, QDS™, version 2.6 (NOVA Research Company, Bethesda, MD).
Baseline dental exams (n=94) took place at CP® sites, using a portable dental chair with air/water syringe, fiber-optic light, disposable gloves, mouth mirror, and periodontal probe. Exams included: 1) full-mouth periodontal probing depths (PD) and bleeding on probing (BOP; yes/no), both measured at 6 sites (mesiofacial, facial, distofacial, mesiolingual, lingual, distolingual) on all teeth including 3rd molars; 2) plaque assessment using the Plaque Index (PI) (22) and; 3) detection of visible untreated decay. The exams were conducted by a highly experienced dental examiner who was trained to assess caries according to the indicator for untreated decay in the Basic Screening Survey manual (23). Training in assessing PD included calibration by the gold standard examiner, a periodontist and co-investigator. The intraclass correlation coefficient (ICC) in measuring PD for two subjects between the two examiners was r=0.60. For intraexaminer reliability for four subjects, ICC was r=0.86. Data were recorded and entered into Microsoft Access.
Analysis variables
Independent variables included: race/ethnicity (Hispanic, White, Other); dental insurance (private, public, none); education (<high school (HS), =HS, >HS); and variables that were dichotomized to evaluate group differences, including income <$20,000 vs. ≥$20,000- commonly used for individuals who refuse to respond or are uncertain of their exact income (24); last dental visit ≤6 months ago vs. >6 months ago- an indicator of recent care (25); and self-reported oral hygiene practices as “optimal” defined as both brushing twice/day and daily flossing- the American Dental Association’s recommendation for consumers (26, 27). For the mediation analyses, income was scored as a continuous variable and age was included as a covariate.
Dependent variables included: presence of untreated decay (yes/no), and % sites for: PD ≥5mm plus BOP; BOP; and PI scores ≥2. Smoking was not included because only one woman reported current or history of smoking. There were a few cases in which there was missing demographic or health behavior data and those cases were excluded from the bivariable analysis.
Statistical analysis
Objective 1: Describe the OH status and behaviors
Descriptive analyses of demographic, OH behaviors, and clinical OH were conducted by categorizing variables and calculating proportions and mean values. BOP was categorized into 4 levels: 1) ≤5% of sites; 2) >5%–10%; 3) >10% – 20%; and 4) >20%. PD ≥5 mm were categorized into 5 levels: 1) 0–3 sites; 2) 4–8 sites; 3) 9–12 sites; 4) 13–16 sites and 5) >16 sites. PD ≥5 mm plus BOP were categorized into 3 levels: 1) ≤10% of sites; 2) >10%–20%; and 3) >20%. PI scores ≥2 were categorized into 2 levels: present in ≥50% and <50% of sites.
Objective 2: Examine bivariable relationships between sociodemographic and behavioral characteristics with OH status
Stratifying by sociodemographic and behavioral variables, analyses conducted included Chi-squares derived from logistic regression analysis to determine the significance of differences for untreated decay, and one-way ANOVAs using Tukey’s Studentized Range Test of planned comparisons for predictor variables with >2 levels (race/ethnicity, education, and insurance) to determine significant differences for the mean proportion of sites with BOP, PD ≥5mm plus BOP, and PI scores ≥2. These same analyses were conducted to test for differences in independent variables or study outcomes by method of questionnaire administration (in person versus over the phone). A two-sided p-value of 0.05 was considered significant.
Objective 3: Examine whether, in multivariable analyses, sociodemographic factors relate to OH status and whether OH behaviors (brushing and flossing, recent dental visit) mediate those relationships
Cluster analysis
Within the sample, demographic variables were highly intercorrelated, making it impossible to include all of them as covariates in regression models. Therefore, we used cluster analysis to identify parsimonious demographic groupings. First, Gower’s method (28) was used to estimate squared Euclidean distances between participants based upon demographic variables: race/ethnicity, a 3-category ordinal indicator of educational attainment, continuous income (cube-root transformed), and categorical dental insurance status (private, public, none). Next, Ward’s method (29) was used to form clusters of participants. The final number of clusters was chosen by referencing plots of the semi-partial R-squared against the number of clusters, as well as substantive appeal of competing solutions.
Regression modeling
Clinical OH assessed at multiple intraoral locations included: 1) BOP; 2) PD ≥5mm plus BOP; and 3) PI scores of ≥2. Each was modeled via logistic regression for binomial outcomes with two components: the number of events (e.g., locations with BOP) and the number of trials (e.g., number of locations probed). Using these binomial outcomes allowed for participant-specific numbers of observed locations. Additionally, a binary outcome describing any observed untreated decay was modeled with standard logistic regression. Logistic regression models of each outcome were fit in two stages. In the first stage, each outcome was regressed onto explanatory variables describing demographic cluster membership, participant age as a covariate, binary indicators of oral hygiene practices (brushing and flossing), and having a dental visit within the prior 6 months. The second stage estimated and tested the indirect (mediated) effects of the demographic clusters on each outcome, via the oral hygiene and dental visit variables (30). In each stage, a backward elimination process removed nonsignificant effects from all models: p<0.15. Except as noted, we report odds ratios, 95% confidence intervals, and p-values estimated via a bootstrap procedure with 1000 replicate samples. Because indirect effect estimates can be skewed, we do not report their p-values.
Results
Table 1 and Figure 1 present sociodemographic characteristics and OH behaviors. Most were Hispanic (65%), 50% had annual household incomes <$20,000, 56% had public dental insurance, and 23% had <HS education. Mean age was 28.7 years (sd = 5.3, range = 18–40). 2010 California survey results of pregnant women are presented for comparison: mean age was 28.5 years; 51% reported as Hispanic, 44% reported income ≤$22,000, 52% reported having Medi-Cal coverage for prenatal care, which includes limited dental coverage during pregnancy, and 20% did not complete high school (or GED), (21, California Maternal, Child and Adolescent Health Program, emailed personal communication 2013 May 9). No significant differences in independent variables or study outcomes were found when analyzing by method of questionnaire administration (in person or over the phone), excepting a higher likelihood of phone administration among White compared to Hispanic participants, p=0.05.
Table 1.
Sociodemographic and self-reported oral health behavior characteristics
| Participant Characteristic | n | % |
|---|---|---|
| Race/Ethnicity (n=99) | ||
| Hispanic | 64 | 64.7 |
| White | 20 | 20.2 |
| Other | 15 | 15.2 |
|
| ||
| Annual Household Income (n=97) | ||
| <$20,000 | 48 | 49.5 |
| ≥ $20,000 | 49 | 50.5 |
|
| ||
| Education Level (n=99) | ||
| < High School | 23 | 23.2 |
| High School | 25 | 25.3 |
| > High School | 51 | 51.5 |
|
| ||
| Dental Insurance Status (n=95) | ||
| Public | 53 | 55.8 |
| Private | 27 | 28.4 |
| None | 15 | 15.8 |
|
| ||
| Frequency of Toothbrushing (n=99) | ||
| < twice a day | 12 | 12.1 |
| ≥ twice a day | 87 | 87.9 |
|
| ||
| Frequency of Flossing (n=99) | ||
| Rarely or never | 25 | 25.3 |
| Once or more per week but not daily | 30 | 30.3 |
| At least once a day | 42 | 42.4 |
| I don’t know what floss is | 2 | 2.2 |
|
| ||
| Oral Hygiene (n=97) | ||
| “Suboptimal”† | 57 | 58.8 |
| “Optimal”‡ | 40 | 41.2 |
|
| ||
| Last Dental Visit (n=99) | ||
| 6 months or less | 50 | 50.5 |
| More than 6 months, but not more than 1 year ago | 9 | 9.1 |
| More than 1 year, but less than 2 years ago | 16 | 16.2 |
| More than 2 years | 24 | 24.2 |
“Suboptimal” = does not brush at least 2X/day and floss at least once a day
“Optimal” = brushes at least 2X/day and flosses at least once a day
Figure 1.
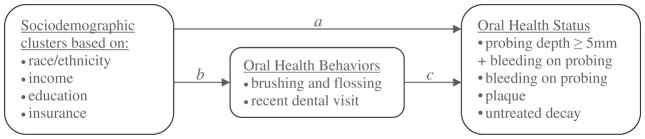
Hypothesized effects of sociodemographic factors on clinical oral health status include direct effects (a) and indirect effects via oral health behaviors (b & c).
Objective 1 Clinical OH status
Eighty-eight percent reported brushing at least twice a day, 42% flossed at least daily, and 51% had a past 6-month dental visit (Table 1). On average, participants had 9% of sites with PD ≥5mm depth, 18% of sites with BOP, and a mean PI score of 0.9. Seventy-seven percent had at least 4 sites with PD ≥5mm, two-thirds had ≥10% of sites with BOP, 18% had greater than 10% sites with PD ≥5mm plus BOP, and 45% had untreated decay (Table 2).
Table 2.
Oral health status of study sample (n=94)
| Mean | sd | |
|---|---|---|
| Mean number of teeth (including 3rd molars) | 28.1 | 2.6 |
| Mean probing depth | 2.8mm | 0.4 |
| Mean percentage of tooth sites with probing depth ≥ 5mm | 8.5% | 9.4 |
| Mean percentage of tooth sites with bleeding on probing | 18.4% | 16.9 |
| Mean percentage of tooth sites with probing depth ≥ 5mm + bleeding on probing | 5.7% | 7.8 |
| Mean Plaque Indexβ score | 0.9 | 0.4 |
|
| ||
| n | % | |
|
| ||
| % of women with ≥ 5mm probing depth | ||
| Present in 0–3 sites | 22 | 23.4 |
| Present in 4–8 sites | 28 | 29.8 |
| Present in 9–12 sites | 10 | 10.6 |
| Present in 13–16 sites | 8 | 8.5 |
| Present in > 16 sites | 26 | 27.7 |
|
| ||
| % of women with bleeding on probing | ||
| Present in ≤ 5% sites | 14 | 14.9 |
| Present in > 5–10% sites | 20 | 21.3 |
| Present in > 10–20% sites | 35 | 37.2 |
| Present in > 20% sites | 25 | 26.6 |
|
| ||
| % of women with ≥ 5mm probing depth + bleeding on probing | ||
| Present in ≤ 10% sites | 77 | 81.9 |
| Present in > 10–20% sites | 9 | 9.5 |
| Present in > 20% sites | 8 | 8.5 |
|
| ||
| % of women with Plaque Indexβ score ≥ 2 | ||
| Present in < 50% sites | 74 | 78.7 |
| Present in ≥ 50% sites | 20 | 21.3 |
|
| ||
| % of women with untreated decay | 42 | 44.7 |
Silness & Löe Plaque Index
Objective 2 Bivariable analyses
Stratifying by sociodemographic and behavior variables (Table 3), disparities were found in all four OH measures. Hispanic women, compared to Whites, fared worse on BOP, PD ≥5mm plus BOP, and PI scores (p<0.05) and on the presence of untreated decay (Chi-square 13.3, p<0.001). Lower (versus higher) income was related to a greater likelihood of untreated decay (Chi-square 7.6, p<0.01). Compared to the highest education level, those with the lowest level had higher % BOP and those with middle level had higher PI, both p<0.05, and a greater likelihood of untreated decay (Chi Square 4.0, p<0.05). Those with public (versus private) dental insurance had greater % BOP, PD ≥5mm plus BOP, both p<0.05, and a greater likelihood of untreated decay (Chi-square 16.9, p<0.001). Lacking a dental visit in the past 6 months (versus having one) was related to greater: BOP, PD ≥5mm plus BOP, and PI ≥2 (F range 6.2–8.7, p<0.01–.05); and greater untreated decay (Chi Square 12.0, p<0.001). Self-reported optimal oral hygiene practices (versus suboptimal) were related to lower % BOP and PD ≥5mm plus BOP (F range 4.5–6.7, both p<0.05).
Table 3.
Oral health status stratified by sociodemographic and behavioral variables
| Oral Health Status
|
||||
|---|---|---|---|---|
| Probing depth ≥ 5mm + bleeding on probing (mean % sites§) | Bleeding on probing (mean % sites§) | Plaque Indexβ score ≥ 2 (mean % sites§) | Untreated Decay (%) | |
|
| ||||
| Total sample | 5.7 | 18.4 | 29.8 | 44.7 |
|
| ||||
| Race/Ethnicity (n=94) | ||||
| Hispanic | 6.9*a | 21.5*a | 33.3*a | 60.0*** |
| White | 1.2 | 7.9 | 18.8 | 10.5 |
| Other | 6.2 | 19.2 | 30.0 | 26.7 |
|
| ||||
| Annual Household Income (n=93) | ||||
| < $20,000 | 7.1 | 21.6 | 33.2 | 58.7** |
| ≥ $20,000 | 4.3 | 15.3 | 27.0 | 29.8 |
|
| ||||
| Education Level (n=94) | ||||
| < High School | 7.7 | 24.3*a | 35.1 | 68.2 |
| High School | 7.5 | 23.2 | 37.2*a | 69.6* |
| > High School | 3.9 | 13.5 | 24.0 | 22.5 |
|
| ||||
| Dental Insurance Status (n=90) | ||||
| Public | 7.6*a | 22.3*a | 33.1 | 68.0*** |
| Private | 1.9 | 10.6 | 24.5 | 4.0 |
| None | 4.3 | 17.0 | 24.7 | 33.3 |
|
| ||||
| Dental Visit Past Six Months (n=94) | ||||
| No | 7.8** | 23.2** | 35.3* | 62.5*** |
| Yes | 3.5 | 13.3 | 24.1 | 26.1 |
|
| ||||
| Self-reported Oral Hygiene (n=92) | ||||
| “Suboptimal”† | 7.1* | 22.1* | 31.7 | 47.3 |
| “Optimal”‡ | 3.6 | 13.0 | 27.9 | 43.2 |
Italicized text = reference group,
p=0.05,
p<0.05,
p<0.01,
p<0.001
Silness & Löe Plaque Index
mean % sites = mean % of tooth sites for each sociodemographic and behavioral subgroup
“Suboptimal” = does not brush at least 2X/day and floss at least once a day
“Optimal” = brushes at least 2X/day and flosses at least once a day
Objective 3 Mediation analyses
For multivariable regression models, the demographic variables describing race/ethnicity, education, income, and insurance were highly intercorrelated. Therefore, these variables were used to derive demographic clusters.
Cluster analysis
A four-cluster solution was chosen, accounting for 80.4% of all interperson variation in distance matrix. The largest cluster included 47 Hispanic participants: 98% with ≤HS education; the lowest median income ($14K), and 81% with public dental insurance (‘Hispanic-lower-SES’). A second Hispanic-only cluster included 17 participants: 100% had >HS education; a median income of $19K; and 92% having private or public dental insurance (‘Hispanic-middling-SES’). A third cluster included 20 White participants: 95% had >HS education; 70% with private insurance; and the highest median income ($100K; ‘White-higher-SES’). The fourth cluster included 15 participants of ‘other’ race/ethnicity: 93% had >HS education; median income was $75K; and 79% had private or public insurance (‘Other-higher-SES’).
Multivariable regression models
Stage 1 models suggested significant direct effects of cluster membership on all OH status measures. Compared to the ‘White-higher-SES’ group, the ‘Hispanic-lower-SES’ group had significantly less favorable OH status on all four clinical measures (p=0.001–0.009) (Figure 1, Table 4) while the ‘Hispanic-middling-SES’ and ‘Other-higher-SES’ groups fared worse for 2 of the 4 OH measures (PD ≥5mm plus BOP and BOP, p=0.001–0.020). Finally, self-reported brushing and flossing were significantly associated with less BOP (p=0.012) whereas having attended a recent dental visit was negatively and significantly related to the other three OH measures (p=0.018–0.051). In the second stage analyses, the OH disadvantages of the ‘Hispanic-lower-SES’ and ‘Hispanic-middling-SES’ clusters (versus the ‘White-higher-SES’ cluster) on PD ≥5mm plus BOP, PI, and untreated decay were partially and significantly mediated by having a recent dental visit: odds ratios for these indirect effect estimates ranged from ORind=1.20 (1.02, 1.49) to ORind=1.93 (1.09, 4.15).
Table 4.
Multivariable and mediation analyses of sociodemographic clusters, self-reported behavioral mediators, and clinical oral health status
| Direct effects – Odds ratios | ||||
|---|---|---|---|---|
| Sociodemographic clusters or behaviors | % ≥ 5mm probing depth plus BOP (n=94) | % BOP (n=92) | % Plaque Indexβ score ≥ 2 (n=94) | untreated decay (yes/no) (n=94) |
| Hispanic-Lower-SESc |
3.64 (1.69, 8.93) p=.002 |
2.49 (1.65, 3.86) p<.001 |
1.88 (1.18, 3.10) p=.009 |
10.58 (2.67, 40.06) p=.001 |
| Hispanic-Middling-SESc |
2.89 (1.18, 7.00) p=.020 |
2.29 (1.39, 3.72) p=.001 |
1.35 (0.75, 2.46) p=.314 |
3.03 (0.48, 17.10) p=.364 |
| Other-Higher-SESc |
3.93 (1.61, 10.08) p=.002 |
2.49 (1.21, 4.57) p=.008 |
1.70 (0.88, 3.32) p=.119 |
2.04 (.31, 10.83) p=.432 |
| “Optimal” ‡ Oral hygiened | a |
0.60 (0.39, 0.88) p=.012 |
a | a |
| Recent dental visit (6 months)e |
0.54 (0.28, 0.94) p=.051* |
a |
0.61 (0.41, 0.92) p=.018 |
0.26 (0.08, 0.75) p=.018 |
| Indirect effects mediated by dental visit in last 6 months – Odds ratios | ||||
| Hispanic-Lower-SES via visit | 1.26 (1.01, 1.80) | b | 1.20 (1.02, 1.49) | 1.63 (1.07, 3.16) |
| Hispanic-Middling-SES via visit | 1.35 (1.02, 2.09) | b | 1.28 (1.03, 1.75) | 1.93 (1.09, 4.15) |
| Other-Higher-SES via visit: | 1.13 (0.93, 1.51) | b | 1.10 (0.95, 1.36) | 1.29 (0.86, 2.33) |
BOP = Bleeding on probing
Silness & Löe Plaque Index
Bold text = significant odds ratios
p-value >.05, but bootstrap 95% CI excludes 1.0
Potential mediator is not significantly related to the dependent variable
Mediation model was not tested because potential mediator was not significantly related to the dependent variable.
Reference group = White-Higher-SES
Reference group = “Suboptimal” oral hygiene (does not brush at least 2X/day and floss at least once a day)
Reference group = No dental visit in past 6 months
“Optimal” = brushes at least 2X/day and flosses at least once a day
Discussion
This study assessed the clinical OH status of a diverse group of pregnant women and found that a significant proportion had dental disease, with the greatest burden among those in disadvantaged circumstances. Nearly 1 in 2 had untreated decay which is higher than national estimates of 23% of women aged 25–44 years (31). Three of four women had at least 4 sites with PD ≥5mm; and roughly 9 of 10 had at least 5% of sites with BOP, higher than what has been found in other studies of pregnant women using similar parameters (11, 32, 33) possibly owing to factors such as differences in socioeconomic status and later gestational period at the time of the examination for our sample. Given the similarity of the sample characteristics to those of pregnant women in the state of California, home to 1 of 8 Americans (34), these findings suggest that similar levels of oral disease may be found among a substantial proportion of U.S. pregnant women.
Our finding that minority women from disadvantaged backgrounds had the greatest burden of poor OH corroborates current literature on OH disparities in general (8–10). Disparities based on having had a dental visit in the past 6 months were more consistent for all OH measures than those by income and education, suggesting that utilization of care may have a stronger influence. The mediation analyses supported this, showing that recent dental care partially explained the OH disparity between the Hispanic and White groups, highlighting its importance. Nevertheless, significant differences remained between the groups, indicating the persistence of demographic disparities. This is consistent with other research demonstrating OH disparities during pregnancy (11). However, most studies consider self-reported (12, 13) rather than clinically assessed OH as measures of OH status.
The importance of dental care utilization found in our study confirms and supports the focus on increasing access to and utilization of dental care during pregnancy in the recent professional clinical guidelines (35–37). Yet, numerous population-based surveys of pregnant women report low utilization and disparities by sociodemographic characteristics (13, 18–20). Care-seeking and utilization are influenced by factors at the personal, provider, and environmental levels that include: financial resources and insurance; health literacy regarding knowledge of insurance eligibility; need for care, and perceptions of the importance and value of OH; the availability of care; access to care; and provider knowledge or comfort in treating pregnant women (38, 39). Thus, efforts to increase utilization of dental care during pregnancy must address change at these levels. Educational campaigns targeting pregnant women and dental and perinatal care providers that promote the importance and safety of dental care are necessary, though not sufficient. Multilevel intervention strategies that address the socioeconomic context that drives OH status and behaviors offer further potential. For example, one community-based intervention included home visits and case management to improve dental care utilization during pregnancy (40). While this and other studies and public health efforts should continue, our findings also indicate the importance of targeting research and intervention efforts on Hispanic women, a group with well-documented OH- and other health-related disparities (41).
This study had limitations. The relatively small sample size limited the external validity of results. However the demographics of this sample are representative of California’s MIHA sample, thus providing valuable information regarding a highly diverse population group. The CPOP study aimed to improve gingival health within a 2–3 month period, thus clinical attachment measurements or DMFT were not assessed, resulting in the varying level of detail in measures included in this analysis. The subjective self-report nature of the questionnaire could have influenced results. It is possible that other factors not included in the analyses such as hyperemesis, diet, and previous pregnancies could have affected the findings. Though our results suggest a directional effect of sociodemographic factors on OH status mediated by dental care utilization, definitive conclusions regarding directionality cannot be made due to the cross-sectional design. However, the primary independent variables- sociodemographic characteristics-tend to be stable and are unlikely to be influenced by behaviors or health status. Additionally, given the timeframes of the retrospective health behavior questions regarding past utilization and oral hygiene, versus the dental exams, the most plausible causal direction is from sociodemographics to behaviors to health status.
This study provides empirical evidence to support continued efforts in promoting OH during pregnancy. The identification of a significant level of OH problems during pregnancy, particularly for Hispanic women, reinforces the importance of providing comprehensive OH care that includes both treatment and education. Our finding of recent dental care mediating the associations between the demographic factors and OH status contributes new evidence regarding its importance. These findings may be useful for identifying priorities and tailoring OH promotion efforts for expectant mothers.
Further research and program development that take into account individual-level, provider-level, environmental, policy, and other larger social contextual factors is needed to more effectively target and reduce OH disparities during pregnancy.
Acknowledgments
Funding source:
This study is supported by NIH/NIDCR R21DE019211 and the Dental Trade Alliance Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH/NIDCR.
References
- 1.Laine MA. Effect of pregnancy on periodontal and dental health. Acta Odontol Scand. 2002;60(5):257–64. doi: 10.1080/00016350260248210. [DOI] [PubMed] [Google Scholar]
- 2.American Dental Association Council on Access Prevention and Interprofessional Relations. Oral health care series: women’s oral health issues [Internet] Chicago: American Dental Association; Nov, 2006. [cited 2012 September 19]. Available from: http://www.ada.org/sections/professionalResources/pdfs/healthcare_womens.pdf. [Google Scholar]
- 3.Armitage GC. Bi-directional relationship between pregnancy and periodontal disease. Periodontol 2000. 2013;61(1):160–76. doi: 10.1111/j.1600-0757.2011.00396.x. [DOI] [PubMed] [Google Scholar]
- 4.Zeeman GG, Veth EO, Dennison DK. Focus on primary care: periodontal disease: implications for women’s health. Obstet Gynecol Surv. 2001;56(1):43–9. doi: 10.1097/00006254-200101000-00024. [DOI] [PubMed] [Google Scholar]
- 5.Lalonde M. Canada Department of National Health and Welfare. A new perspective on the health of Canadians: a working document. Ottawa, ON: Ministry of Supply and Services; 1974. [Google Scholar]
- 6.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 7.U.S. Department of Health and Human Services. Oral health in America: a report of the Surgeon General [Internet] Rockville, MD: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. [cited 2013 Jun 28]. Available from: http://www.nidcr.nih.gov/DataStatistics/SurgeonGeneral/sgr/figures/Fig10-03.htm. [Google Scholar]
- 8.Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, et al. Trends in oral health status: United States, 1988–1994 and 1999–2004. National Center for Health Statistics Vital Health Stat. 2007;11(248):1–92. [PubMed] [Google Scholar]
- 9.Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012;91(10):914–20. doi: 10.1177/0022034512457373. [DOI] [PubMed] [Google Scholar]
- 10.Grembowski D, Spiekerman C, Milgrom P. Social gradients in dental health among low-income mothers and their young children. J Health Care Poor Underserved. 2012;23(2):570–88. doi: 10.1353/hpu.2012.0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lieff S, Boggess KA, Murtha AP, Jared H, Madianos PN, Moss K, et al. The oral conditions and pregnancy study: periodontal status of a cohort of pregnant women. J Periodontol. 2004;75(1):116–26. doi: 10.1902/jop.2004.75.1.116. [DOI] [PubMed] [Google Scholar]
- 12.Lydon-Rochelle MT, Krakowiak P, Hujoel PP, Peters RM. Dental care use and self-reported dental problems in relation to pregnancy. Am J Public Health. 2004;94(5):765–71. doi: 10.2105/ajph.94.5.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hwang SS, Smith VC, McCormick MC, Barfield WD. Racial/ethnic disparities in maternal oral health experiences in 10 states, pregnancy risk assessment monitoring system, 2004–2006. Matern Child Health J. 2011;15(6):722–9. doi: 10.1007/s10995-010-0643-2. [DOI] [PubMed] [Google Scholar]
- 14.Christensen LB, Jeppe-Jensen D, Petersen PE. Self-reported gingival conditions and self-care in the oral health of Danish women during pregnancy. J Clin Periodontol. 2003;30(11):949–53. doi: 10.1034/j.1600-051x.2003.00404.x. [DOI] [PubMed] [Google Scholar]
- 15.Offenbacher S, Lin D, Strauss R, McKaig R, Irving J, Barros SP, et al. Effects of periodontal therapy during pregnancy on periodontal status, biologic parameters, and pregnancy outcomes: a pilot study. J Periodontol. 2006;77(12):2011–24. doi: 10.1902/jop.2006.060047. [DOI] [PubMed] [Google Scholar]
- 16.Michalowicz BS, Hodges JS, DiAngelis AJ, Lupo VR, Novak MJ, Ferguson JE, et al. Treatment of periodontal disease and the risk of preterm birth. N Engl J Med. 2006;355(18):1885–94. doi: 10.1056/NEJMoa062249. [DOI] [PubMed] [Google Scholar]
- 17.Green LW, Ottoson JM. Community and population health. 8. Boston: McGraw-Hill; 1999. [Google Scholar]
- 18.Marchi KS, Fisher-Owens SA, Weintraub JA, Yu Z, Braveman PA. Most pregnant women in California do not receive dental care: findings from a population-based study. Public Health Rep. 2010;125(6):831–42. doi: 10.1177/003335491012500610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gaffield ML, Gilbert BJ, Malvitz DM, Romaguera R. Oral health during pregnancy: an analysis of information collected by the pregnancy risk assessment monitoring system. J Am Dent Assoc. 2001;132(7):1009–16. doi: 10.14219/jada.archive.2001.0306. [DOI] [PubMed] [Google Scholar]
- 20.Boggess KA, Urlaub DM, Massey KE, Moos MK, Matheson MB, Lorenz C. Oral hygiene practices and dental service utilization among pregnant women. J Am Dent Assoc. 2010;141(5):553–61. doi: 10.14219/jada.archive.2010.0228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maternal Infant Health Assessment Statewide Snapshots. Sacramento, CA: California Department of Public Health; 2010. [Internet] 2010 [cited 2013 May 10]. Available from: http://www.cdph.ca.gov/data/surveys/Pages/MIHASnapshots.aspx. [Google Scholar]
- 22.Silness J, Löe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 23.Association of State and Territorial Dental Directors. Basic screening surveys: an approach to monitoring community oral health. Columbus, OH: Association of State and Territorial Dental Directors; 1999. revised September 2003. [Google Scholar]
- 24.NHIS Survey Description [Internet] Hyattsville, MD: National Center for Health Statistics, Centers for Disease Control and Prevention; 2012. [cited 2013 May 13]. Available from: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2011/srvydesc.pdf. [Google Scholar]
- 25.2013–2014 National Health and Nutrition Examination Survey (NHANES) Sample Person Questionnaire [Internet] Hyattsville, MD: National Center for Health Statistics, Centers for Disease Control and Prevention; 2013. [cited 2013 Jul 5]. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_13_14/OHQ_H.pdf. [Google Scholar]
- 26.American Dental Association’s Mouth Healthy [Internet] Chicago: American Dental Association; 2012. [cited 2013 June 28]. Available from: http://www.mouthhealthy.org/en/az-topics/b/brushing-your-teeth.aspx. [Google Scholar]
- 27.American Dental Association’s Mouth Healthy [Internet] Chicago: American Dental Association; 2012. [cited 2013 June 28]. Available from: http://www.mouthhealthy.org/en/az-topics/f/flossing.aspx. [Google Scholar]
- 28.Gower JC, Legendre P. Metric and euclidean properties of dissimilarity coefficients. J Classif. 1986;3(1):5–48. [Google Scholar]
- 29.Ward JH. Hierarchical grouping to optimize an objective function. J Am Stat Assoc. 1963;58(301):236–244. [Google Scholar]
- 30.Li Y, Schneider JA, Bennett DA. Estimation of the mediation effect with a binary mediator. Stat Med. 2007;26(18):3398–414. doi: 10.1002/sim.2730. [DOI] [PubMed] [Google Scholar]
- 31.U.S. Department of Health and Human Services. Health Resources Services Administration. Women’s health USA 2009. Rockville, MD: U.S. Department of Health and Human Services; 2009. [Internet] [cited 2012 Sep 11]. Available from: http://mchb.hrsa.gov/publications/pdfs/womenhealth2009.pdf. [Google Scholar]
- 32.Vogt M, Sallum AW, Cecatti JG, Morais SS. Factors associated with the prevalence of periodontal disease in low-risk pregnant women. Reprod Health. 2012;9:3. doi: 10.1186/1742-4755-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xie Y, Xiong X, Elkind-Hirsch KE, Pridjian G, Maney P, Delarosa RL, et al. Change of periodontal disease status during and after pregnancy. J Periodontol. 2012 doi: 10.1902/jop.2012.120235. Epub 2012/08/10. [DOI] [PubMed] [Google Scholar]
- 34.U.S. Department of Commerce. US Census Bureau. State and county quickfacts [Internet] Washington, DC: U.S. Census Bureau; 2012. [updated 2013 Jun 27; cited 2013 Jun 28]. Available from: http://quickfacts.census.gov/qfd/states/06000.html. [Google Scholar]
- 35.California Dental Association Foundation, American College of Obstetricians and Gynecologists District IX. Oral health during pregnancy and early childhood: evidence-based guidelines for health professionals. J Calif Dent Assoc. 2010;38(6):391–403. 5–40. [PubMed] [Google Scholar]
- 36.New York State Department of Health. Oral health care during pregnancy and early childhood: practice guidelines. Albany, NY: New York State Department of Health; Aug, 2006. [Google Scholar]
- 37.Oral Health Care During Pregnancy Expert Workgroup. Oral health care during pregnancy: a national consensus statement [Internet] Washington, DC: National Maternal and Child Oral Health Resource Center; 2012. [cited 2012 December 10]. Available from: http://www.mchoralhealth.org/pdfs/OralHealthPregnancyConsensus.pdf. [Google Scholar]
- 38.Le M, Riedy C, Weinstein P, Milgrom P. Barriers to utilization of dental services during pregnancy: a qualitative analysis. J Dent Child (Chic) 2009;76(1):46–52. [PMC free article] [PubMed] [Google Scholar]
- 39.Kloetzel MK, Huebner CE, Milgrom P, Littell CT, Eggertsson H. Oral health in pregnancy: educational needs of dental professionals and office staff. J Public Health Dent. 2012;72(4):279–86. doi: 10.1111/j.1752-7325.2012.00333.x. [DOI] [PubMed] [Google Scholar]
- 40.Milgrom P, Ludwig S, Shirtcliff RM, Smolen D, Sutherland M, Gates PA, et al. Providing a dental home for pregnant women: a community program to address dental care access--a brief communication. J Public Health Dent. 2008;68(3):170–3. doi: 10.1111/j.1752-7325.2007.00049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Centers for Disease Control and Prevention. CDC health disparities and inequalities report - United States, 2011. MMWR Surveill Summ. 2011;60(Suppl):1–2. [PubMed] [Google Scholar]


