Abstract
Study Objectives:
A chinstrap is potentially useful to reduce unintentional air leak by preventing mouth opening during PAP treatment. This study examines whether the addition of a chinstrap to PAP therapy has any effect on adherence, nightly duration of use, air leak, and residual AHI.
Methods:
This was a retrospective study performed at an AASM-accredited VAMC sleep center. Clinical sleep data of veterans (n = 124) prescribed PAP therapy for sleep apnea was evaluated, and the effect of chinstrap use vs non-use on the above parameters was assessed.
Results:
Chinstrap users had significantly greater PAP adherence, longer nightly duration of PAP use, lower residual AHI and lower leak compared to chinstrap non-users at first follow up visit.
Conclusions:
The addition of a chin strap to PAP therapy is a simple and inexpensive method of increasing PAP adherence.
Citation:
Knowles SR; O'Brien DT; Zhang S; Devara A; Rowley JA. Effect of addition of chin strap on PAP compliance, nightly duration of use, and other factors. J Clin Sleep Med 2014;10(4):377-383.
Keywords: Chin strap, sleep apnea, positive airway pressure, adherence, compliance, air leak, AHI
Sleep apnea is associated with increased risk for cardiovascular disease, hypertension, heart attack, and stroke. Positive airway pressure (PAP) therapy has been shown to reduce this risk.1–3 Due to the significant health consequences of untreated sleep apnea, it is desirable to achieve high PAP compliance. PAP is usually initiated during a PAP “titration” (incremental adjustment of PAP pressure) during polysomnography in the sleep lab. PAP treatment is a closed system for treatment of sleep apnea that delivers pressurized air to the site of obstruction in the pharynx. The pressurized air splints the airway open and relieves the obstruction. Unintentional air leak in the system results in development of an open circuit that may reduce the pressure of air delivered to the site of obstruction, with associated recurrence of respiratory events (including apneas, hypopneas, RERAs, flow limitation and snoring). Mouth opening during PAP treatment is a source of air leak. A chin strap may be useful to reduce this leak by preventing mouth opening during PAP treatment, and may be applied during PAP titration or later in the course of PAP clinical follow-up. The chin strap supports the mandible with sufficient tension to reduce mouth opening during sleep (Figure 1). Chin strap application may also reduce complaints of dry mouth and arousals associated with air leak.30 American Academy of Sleep Medicine (AASM) Best Clinical Practices for PAP titration recommends addition of chin strap (or switch to full-face mask) to reduce leak.29 After in-lab PAP titration, the patient then uses PAP during sleep at home and is seen in follow-up in sleep clinic to assess compliance and response to therapy. Overall reported PAP compliance rates vary widely and range between 30% and 84%.4,6,10 Literature review reveals many studies examining factors potentially affecting compliance, such as heated humidity, patient education, mask type, and type of PAP machine used and its properties (CPAP vs BPAP, auto-PAP vs fixed PAP, expiratory pressure relief settings, etc.).5–13,28 Unresolved air leak has been associated with persistence of sleep apnea in PAP-treated patients, and also with reduced PAP compliance,14,15 but there are few studies evaluating whether chin strap use has any effect on leak, residual AHI, or compliance.
Figure 1. Chin strap front and side views.
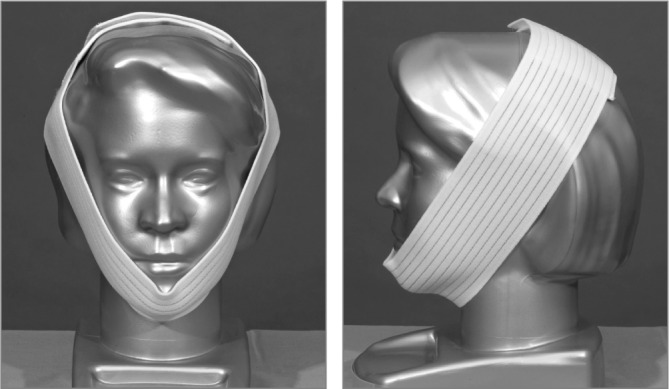
Example of wide white chin strap application
BRIEF SUMMARY
Current Knowledge/Study Rationale: Achieving good positive airway pressure (PAP) adherence in OSA patients is a challenge. The purpose of the current study was to identify whether addition of a chin strap to PAP therapy may be beneficial in increasing PAP adherence.
Study Impact: This is the first outpatient study to specifically demonstrate the positive impact of chin strap use on leak and adherence to PAP therapy. The findings suggest that a chin strap should be routinely prescribed as part of PAP therapy, to improve adherence.
The primary purpose of this study is to determine whether the addition of a chin strap alone improves PAP compliance and nightly duration of use as measured by download of PAP smart card data, reduces residual apnea-hypopnea index (AHI) and/or leak, and improves daytime function as measured by the Epworth Sleepiness Scale (ESS) score.
METHODS
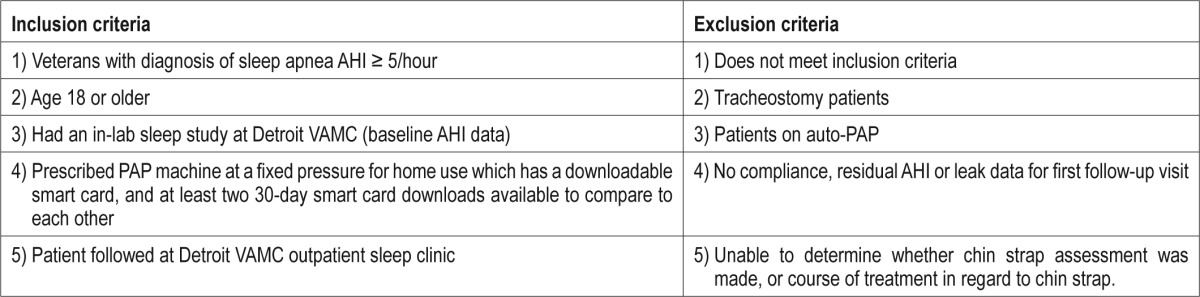
This was a retrospective analysis of existing data previously collected during routine sleep clinic follow-up visits. The study was approved by the Wayne State University and John D. Dingell VAMC Institutional Review Boards, and all records held in strictest confidentiality. The study was done at the John D. Dingell VAMC, an AASM-accredited Sleep Center. Computerized records of veterans who had had follow-up at the VAMC sleep clinic, already prescribed PAP for sleep apnea were reviewed. Sleep clinic follow-up data between August 2008 and May 2011, where 2 “smart card” 30-day downloads were available, were evaluated. Records for which it could not be determined whether a chin strap had been prescribed or used, or were missing compliance, residual AHI, or leak information for first follow-up visit, or for which the course of treatment was not adequately documented were excluded. Typically patients had been clinically evaluated 1 month after PAP was initially dispensed, then again 3 to 6 months later. The most recent 30-days compliance was evaluated for the 2 visits (in a few cases first follow-up download was done at 60 days). Most records did not meet criteria, because the smart card did not report AHI/leak data (older PAP machines), there was not a second compliance download, or the download period exceeded 60 days (during which multiple undocumented interventions may have been made to treatment, which might affect results). A total of 124 records met criteria to be included in the study. All 124 subjects were treated with a fixed positive airway pressure (PAP) for their sleep apnea, which had been identified as effective via in-lab polysomnography with PAP titration. In our lab, autoPAP is not used as a final treatment for sleep apnea. AutoPAP records were also excluded from the analysis due to reports of variance in leak rates with variable pressures,25 which may have led to confounding of variables under analysis. Inclusion and exclusion criteria are listed in Table 1.
Table 1.
Inclusion and exclusion criteria
Data were extracted from the electronic medical record and Respironics Encore-Pro and Encore-Pro 2 software, which was used for smart card downloads. Only Respironics download data was included for standardization purposes (to avoid discrepancies in units of measurement, i.e., with reported leak). Variables analyzed included patient age, sex, BMI (body mass index), baseline AHI (apnea-hypopnea index), ESS (Epworth sleepiness score), 1st and 2nd smart card download % compliance (percentage of nights used), % compliance ≥ 4 h, average duration of usage on nights used (min), residual AHI and leak (min/ night), whether chin strap was prescribed and whether chin strap was used (the latter determined by clinical interview), and ESS at the follow-ups. Baseline AHI was obtained from in-lab polysomnography and is defined as per 2007 AASM scoring criteria.16
We evaluated data from chin strap users vs. non-users, and data from non-users who became chin strap users after their first clinic visit. SAS version 9.3 (SAS Corporation, Cary, NC) was used for statistical analysis including frequency distributions, t-test and general linear regression procedures. Paired t-test was used for within-subjects analysis.
RESULTS
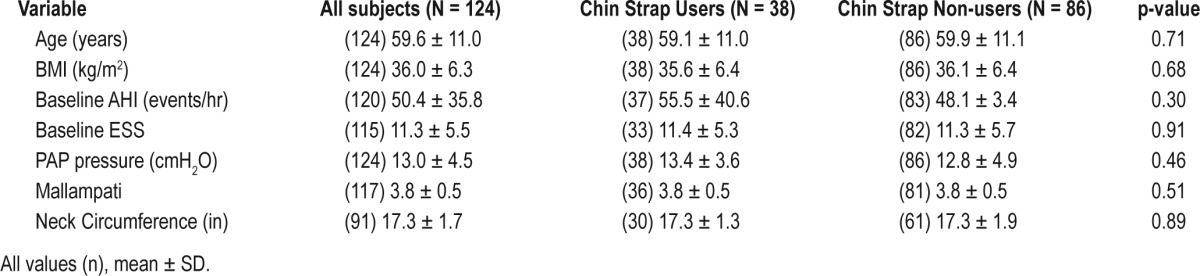
Demographic data are presented in Table 2, which shows BMI, age, sex, baseline AHI, neck circumference, Mallampati score, initial PAP pressure, and baseline ESS were not statistically different between chin strap users and non-users. There were more men than women in the sample, consistent with a VAMC general sleep clinic setting (117 males, 7 females). Sixty-one of 124 patients (49%) were prescribed a chin strap after initial in-lab PAP titration.
Table 2.
Baseline characteristics of subjects
First Follow-up Visit
At the first sleep clinic follow-up visit, most patients were not using a chin strap (38 chin strap users vs. 86 chin strap non-users [31% vs 69%, respectively]); Reasons for chin strap non-use included personal choice, patient did not understand the reason for the chin strap, patient lost the chin strap, chin strap was not initially prescribed, or patient had not received the chin strap as prescribed. Two patients for whom no chin-strap prescription could be found were using chin strap at first follow-up.
In all subjects at first follow-up, with PAP treatment AHI was reduced by 92% compared to baseline AHI (4.2 ± 3.6 vs 50.4 ± 35.7, p < 0.0001) and the ESS was reduced by a mean of 2.4 points in all subjects compared to their baseline ESS (8.9 ± 6.0 vs 11.3 ± 5.54, p = 0.0108).
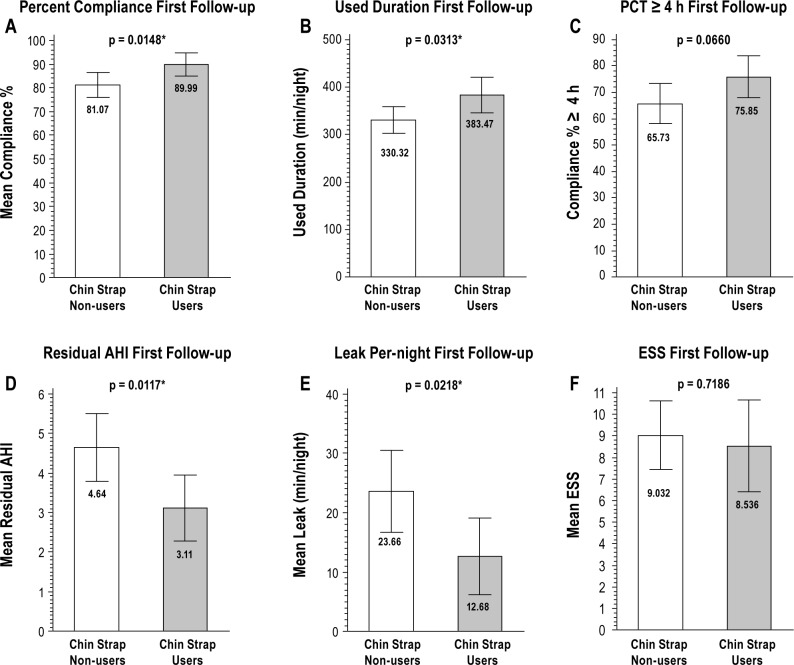
When chin strap users were compared to non-users, at the first follow-up visit there was significantly greater PAP adherence, longer nightly duration of use, greater reduction in air leak, and lower residual AHI in chin strap users compared to non-users (Figure 2). Compliance was 9% higher in chin strap users compared to non-users, and chin strap users had 53 min/night longer duration of PAP use compared to non-users (Figure 2A and 2B). Chin strap users had a significantly lower mean residual AHI than non-users (Figure 2D). Chin strap users also had lower leak/night compared to non-users (Figure 2E). Percent compliance ≥ 4 h/night was 10% greater in the chin strap user group (Figure 2C), but it was not statistically signifi-cant. Chin strap users also had lower ESS than non-users at first follow-up, but it was not statistically significant.
Figure 2. Effect of chin strap use at first follow up visit.
Data from first sleep clinic follow up visit after PSG with in-lab CPAP titration. Chin strap users N = 38, non-users N = 86. Compliance %, percentage of nights PAP used; used duration, nightly duration of PAP use in minutes; PCT ≥ 4 h, percentage of nights used greater than or equal to 4 hours duration; leak is in minutes/ night; ESS, Epworth Sleepiness Score. Residual AHI, apnea-hypopnea index from PAP machine smart card. Results from t-test, * = statistically significant.
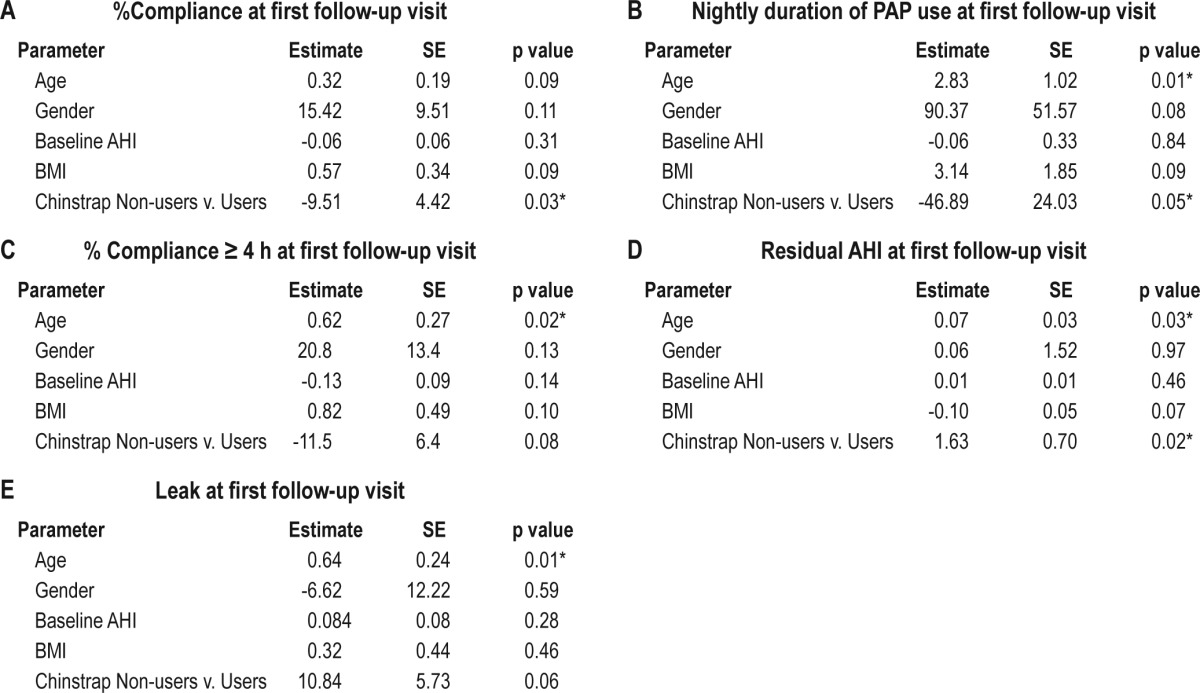
The compliance parameters were corrected for age, gender, and BMI, and the resulting regression analyses are shown in Tables 3A, 3B, 3C, 3D, and 3E. PAP percent compliance was reduced in chin strap non-users compared to users (Table 3A) and was not influenced by age, gender, or BMI. Both chin strap use and increasing age were positively associated with longer nightly duration of PAP use at first follow-up visit (Table 3B). Age was the only determinant of percent compliance ≥ 4 h/ night; chin strap showed only a trend (Table 3C). Residual AHI at first follow up was higher in chin strap non-users at first follow up (Table 3D), with a higher residual AHI also associated with increasing age. Chin strap non-users had higher air leak/night which approached significance. Age was associated with greater leak, which was significant (Table 3E).
Table 3.
Patients Who Switched from Chinstrap Non-use To Use
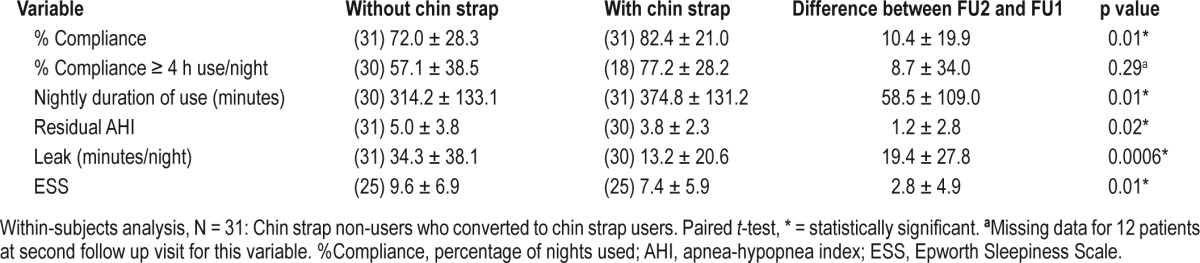
Data were separately analyzed for patients who initially did not use a chin strap but were then prescribed one at first follow-up and began using it. Reasons for chin strap prescription included complaints of dry mouth, continued unrefreshing sleep despite adequate PAP pressure, elevated leak on smart card download, or reported arousals due to mouth leak. For patients who had a second download containing the required data, there were 31 chin strap non-users who became chin strap users (“converters”): The data for these patients are presented in Table 4. Patients who converted from chin strap non-use to chin strap use at second follow-up visit had 10.4% higher compliance and slept with PAP for 59 min longer/night compared to the period without a chin strap. Leak was 19 min/ night less with chin strap use compared to non-use. ESS scores were reduced an additional 2.8 points with chin strap use, and residual AHI at second follow-up was reduced an additional 1.2 events/h compared to without chin strap. Percentage use > 4 h/ night was not significantly different.
Table 4.
Converters: comparison of means between first and second follow-up visits, with addition of chin strap, expressed as (N) mean ± SD
DISCUSSION
This study shows that addition of chin strap to PAP was associated with improved PAP adherence, nightly duration of PAP use, residual AHI, and leak compared to without chin strap. In patients whose PAP use is suboptimal, addition of a chin strap may increase adherence.
In 1999, Teschler et al.17 found that air leak reduced nasal bilevel PAP effectiveness and that taping the mouth closed during BPAP treatment significantly reduced leak, arousal index, and improved BPAP effectiveness as measured by reduction in PaCO2 in hypercapnic patients. Taping the mouth closed was also associated with a significant increase in percentage of REM sleep in that study. Similarly, Gonzalez et al. reported reduction in both air leak and hypercapnia with addition of chin strap in five noninvasively ventilated patients, as compared to without chin strap.32 Two studies by Bachour et al. in 2004 indicated that mouth breathing reduces nasal PAP compliance and that addition of a chin strap reduces air leak.18,19 The latter study (N = 15) was performed with in-lab polysomnography where chin strap was added to PAP therapy, and the arousal index positively correlated with mouth leak. A more recent outpatient PAP mask analysis by Bachour et al. reported subjective patient comfort and leak differences between different brands/types of masks, but the PAP smart card download data were not reported and there was no mention of chin strap usage.20 Sopkova et al. found that mask leak was the single biggest predictor of PAP adherence,21 and Valentin et al.22 demonstrated that air leak and elevated residual AHI is associated with poor compliance to autoPAP therapy; in both of these studies, chin strap use was not specifically examined.
Two recent PAP mask-analysis studies were performed: A study by Bakker et al.23 concluded that full face masks resulted in increased leak and residual AHI and that nasal masks were associated with lower leak; use of chin strap was not reported. Teo et al.24 also reported higher leak with full face masks. In that study, a chin strap was used with nasal masks, but sub-analysis on chin strap and leak was not reported.
Reduction of OSA with use of chin strap alone, confirmed with polysomnography and nasopharyngolaryngoscopy, has also been reported.31 In our study, the addition of a chin strap to PAP therapy was associated with an increased percentage of nights used, with almost one hour longer PAP use at night and greater reduction of AHI. In addition to chin strap use, age was also associated with increased duration of nightly PAP usage, but also with higher residual AHI on PAP therapy. The latter may be due to higher leak in older patients.
When evaluating the effect of chin strap on leak, in our study chin strap users had lower leak than non-users; this lost a degree of significance on regression, and the effect of age on leak was found to be a stronger modifier. Age has been associated with air leak in other studies.37,38 This may represent changes in facial morphology with aging due to loss of teeth, removal of dentures for sleep, changes in skin elasticity or subcutaneous fat, or other etiologies. Older patients may have reduced dexterity due to arthritis or other factors, which may impair ability to adjust the mask and reduce leak.
Results of this study are consistent with others suggesting air leak is a significant factor in PAP compliance. However, this is the first outpatient study to specifically demonstrate the beneficial impact of chin strap use on leak and compliance with therapy.
One difference between this and preceding related studies is that autoPAP was not used. Fixed PAP was used in all patients. Since fixed PAP was used, there is no confounding by variations in leak with varying pressures or variable machine efficacy over certain leakage rates, which has been ascribed to some autoPAP devices.25 The combination of chin strap with autoPAP has not been specifically studied. In contrast to Bachour's in-lab study on addition of chin strap, this was an outpatient study which relied on machine-reported variables.
Antic et al. demonstrated that longer nightly duration of PAP use was associated with normalization of ESS, especially in patients using PAP for at least 7 h/night.26 In a meta-analysis, Weaver and Sawyer noted improvements in mean sleep latency (on multiple sleep latency testing) and Functional Outcomes of Sleep Questionnaire with 6 hours/night and 7.5 hours/night of PAP use, respectively.4 Thus addition of chin strap may reduce daytime sleepiness and improve daytime function by increasing nightly hours of PAP use. In this study, there was a significant reduction in ESS in patients who adopted use of chin strap between first and second follow-up visits (within-subjects analysis). However, for all patients at first follow-up visit, while EDS was reduced compared to baseline, there was no significant difference between chin strap users and non-users in between-subjects analysis. The mean nightly usage in both groups was at least 5.5 hours/night. The initial magnitude of the reduction in AHI in both groups with associated sleep improvement may have masked quantitative differences in ESS. ESS is not always a sensitive indicator of residual sleepiness. Patient estimate of arousals/night or nocturia (see Pressman et al.27) might be a better choice to determine subjective response to differences in treatment.
This study was designed to explore the influence of chin strap use and was not designed to explore the effects of other demographic and social factors on compliance. There are numerous other variables that may influence PAP adherence which were not addressed in this study, including but not limited to marital status, living/sleeping arrangements, employment, race, and socioeconomic status.33–36 However, in performing the regression analyses, we did find that age was a significant independent factor in predicting compliance, with increasing age associated with small increases in the percentage of nights used > 4 hours and nightly hours of use. In most studies on CPAP adherence, age has not been shown to be a predictor of compliance39–42; however, in one study analyzing use in a large cohort, increasing age was associated with increased number of days of use and hours used per night.37
Another weakness of this study is small sample size due to missing data on review of the databases, which may have impacted results where a nonsignificant result was found despite obvious differences in the means. Use of a structured PAP follow-up template including the variables to be analyzed might resolve this issue. Because the study was retrospective and only data on patients who presented for follow-up were analyzed, there may be some bias toward patients who are motivated to improve their health and would have higher compliance in general.
Summary
This study shows that the addition of a chin strap was associated with improved patient PAP compliance, nightly duration of use, residual AHI, and leak in patients with sleep apnea. The improved compliance and duration of use is most likely due to reduction of leak and associated micro-arousals. The addition of a chin strap during home PAP use is a simple and inexpensive method for improving PAP adherence, and because of this has potential to affect the morbidity and mortality from sleep apnea and potentially reduce associated health care costs from this disease. Further studies with larger numbers of patients need to be done in this area.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Special thanks to Ms. Aneesa Shaik, who assisted with formatting of tables and figures. Also thanks to Dr. John Flack, MD (Chair, WSU Department of Internal Medicine) for advice and Dr. John K. Fink, MD (Professor of Neurology, University of Michigan) for advice.
REFERENCES
- 1.Martinez-Garcia MA, Campos-Rodriguez F, Catalán-Serra P, et al. Cardiovascular mortality in obstructive sleep apnea in the elderly. Role of long-term CPAP treatment: a prospective observational trial. Am J Respir Crit Care Med. 2012;186:909–16. doi: 10.1164/rccm.201203-0448OC. [DOI] [PubMed] [Google Scholar]
- 2.Martínez-García MA, Soler-Cataluña JJ, Ejarque-Martínez L, et al. Continuous positive airway pressure treatment reduces mortality in patients with ischemic stroke and obstructive sleep apnea: a 5-year follow-up study. Am J Respir Crit Care Med. 2009;180:36–41. doi: 10.1164/rccm.200808-1341OC. [DOI] [PubMed] [Google Scholar]
- 3.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 4.Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnea: implications for future interventions. Indian J Med Res. 2010;131:245–58. [PMC free article] [PubMed] [Google Scholar]
- 5.Beecroft J, Zanon S, Lukic D, Hanly P. Oral continuous positive airway pressure for sleep apnea: effectiveness, patient preference, and adherence. Chest. 2003;124:2200–8. doi: 10.1378/chest.124.6.2200. [DOI] [PubMed] [Google Scholar]
- 6.Smith I, Nadig V, Lasserson TJ. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines for adults with obstructive sleep apnoea. Cochrane Database Syst Rev. 2009:CD007736. doi: 10.1002/14651858.CD007736. [DOI] [PubMed] [Google Scholar]
- 7.Chai CL, Pathinathan A, Smith B. Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006:CD005308. doi: 10.1002/14651858.CD005308.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nilius G, Happel A, Domanski U, Ruhle KH. Pressure-relief continuous positive airway pressure vs constant continuous positive airway pressure: a comparison of efficacy and compliance. Chest. 2006;130:1018–24. doi: 10.1378/chest.130.4.1018. [DOI] [PubMed] [Google Scholar]
- 9.Ballard RD, Gay PC, Strollo PJ. Interventions to improve compliance in sleep apnea patients previously non-compliant with continuous positive airway pressure. J Clin Sleep Med. 2007;3:706–12. [PMC free article] [PubMed] [Google Scholar]
- 10.Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121:430–5. doi: 10.1378/chest.121.2.430. [DOI] [PubMed] [Google Scholar]
- 11.Mortimore IL, Whittle AT, Douglas NJ. Comparison of nose and face mask CPAP therapy for sleep apnoea. Thorax. 1998;53:290–2. doi: 10.1136/thx.53.4.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haniffa M, Lasserson TJ, Smith I. Interventions to improve compliance with continuous positive airway pressure for obstructive sleep apnea. Cochrane Database Syst Rev. 2004:CD003531. doi: 10.1002/14651858.CD003531.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Kushida CA, Berry RB, Blau A, et al. Positive airway pressure initiation: a randomized controlled trial to assess the impact of therapy mode and titration process on efficacy, adherence, and outcomes. Sleep. 2011;34:1083–92. doi: 10.5665/SLEEP.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baltzan MA, Elkholi O, Wolkove N. Evidence of interrelated side effects with reduced compliance in patients treated with nasal continuous positive airway pressure. Sleep Med. 2009;10:198–205. doi: 10.1016/j.sleep.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 15.Baltzan MA, Kassissia I, Elkholi O, Palayew M, Dabrusin R, Wolkove N. Prevalence of persistent sleep apnea in patients treated with continuous positive airway pressure. Sleep. 2006;29:557–63. [PubMed] [Google Scholar]
- 16.American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Westchester, IL: American Academy of Sleep Medicine; 2007. [PMC free article] [PubMed] [Google Scholar]
- 17.Teschler H, Stampa J, Ragette R, Konietzko N, Berthon-Jones M. Effect of mouth leak on effectiveness of nasal bilevel ventilator assistance and sleep architecture. Eur Respir J. 1999;14:1251–57. doi: 10.1183/09031936.99.14612519. [DOI] [PubMed] [Google Scholar]
- 18.Bachour A, Maasilta P. Mouth breathing compromises adherence to nasal continuous positive airway pressure therapy. Chest. 2004;126:1248–54. doi: 10.1378/chest.126.4.1248. [DOI] [PubMed] [Google Scholar]
- 19.Bachour A, Hurmerinta K, Maasilta P. Mouth closing device (chinstrap) reduces mouth leak during nasal CPAP. Sleep Med. 2004;5:261–7. doi: 10.1016/j.sleep.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 20.Bachour A, Vitikainen P, Virkkula P, Maasilta P. CPAP interface: satisfaction and side effects. Sleep Breath. 2013;17:667–72. doi: 10.1007/s11325-012-0740-0. [DOI] [PubMed] [Google Scholar]
- 21.Sopkova Z, Dorkova Z, Tkacova R. Predictors of compliance with continuous positive airway pressure treatment in patients with obstructive sleep apnea and metabolic syndrome. Wien Klin Wochenschr. 2009;121:398–404. doi: 10.1007/s00508-009-1181-z. [DOI] [PubMed] [Google Scholar]
- 22.Valentin A, Subramanian S, Quan S, Berry R, Parthasarathy S. Air leak is associated with poor adherence to autoPAP therapy. Sleep. 2011;34:801–6. doi: 10.5665/SLEEP.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bakker JP, Neill AM, Campbell AJ. Nasal versus oronasal continuous positive airway pressure masks for obstructive sleep apnea: a pilot investigation of pressure requirement, residual disease, and leak. Sleep Breath. 2012;16:709–16. doi: 10.1007/s11325-011-0564-3. [DOI] [PubMed] [Google Scholar]
- 24.Teo M, Amis T, Lee S, Falland K, Lambert S, Wheatley J. Equivalence of nasal and oronasal masks during initial CPAP titration for obstructive sleep apnea syndrome. Sleep. 2011;34:951–5. doi: 10.5665/SLEEP.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coller D, Stanley D, Parthasarathy S. Effect of air leak on the performance of auto-PAP devices: a bench study. Sleep Breath. 2005;9:167–75. doi: 10.1007/s11325-005-0032-z. [DOI] [PubMed] [Google Scholar]
- 26.Antic NA, Catcheside P, Buchan C, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34:111–9. doi: 10.1093/sleep/34.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pressman MR, Figueroa WG, Kendrick-Mohamed J, Greenspon LW, Peterson DD. Nocturia. A rarely recognized symptom of sleep apnea and other occult sleep disorders. Arch Intern Med. 1996;156:545–50. doi: 10.1001/archinte.156.5.545. [DOI] [PubMed] [Google Scholar]
- 28.Gentina T, Fortin F, Douay B, et al. Auto-bilevel with pressure relief during exhalation as a rescue therapy for optimally treated obstructive sleep apnoea patients with poor compliance to continuous positive airways pressure therapy-a pilot study. Sleep Breath. 2011;15:21–7. doi: 10.1007/s11325-009-0322-y. [DOI] [PubMed] [Google Scholar]
- 29.Berry RB, Chediak A, Brown LK, et al. NPPV Titration Task Force of the American Academy of Sleep Medicine. Best clinical practices for the sleep center adjustment of noninvasive positive pressure ventilation (NPPV) in stable chronic alveolar hypoventilation syndromes. J Clin Sleep Med. 2010;6:491–509. [PMC free article] [PubMed] [Google Scholar]
- 30.Meyer TJ, Pressman MR, Benditt J, McCool FD, Millman RP, Natarajan R, Hill NS. Air leaking through the mouth during nocturnal nasal ventilation: effect on sleep quality. Sleep. 1997;20:561–9. doi: 10.1093/sleep/20.7.561. [DOI] [PubMed] [Google Scholar]
- 31.Vorona RD, Ware JC, Sinacori JT, Ford ML, 3rd, Cross JP. Treatment of severe obstructive sleep apnea syndrome with a chinstrap. J Clin Sleep Med. 2007;3:729–30. [PMC free article] [PubMed] [Google Scholar]
- 32.Gonzalez J, Sharshar T, Hart N, Chadda K, Raphael JC, Lofaso F. Air leaks during mechanical ventilation as a cause of persistent hypercapnia in neuromuscular disorders. Intensive Care Med. 2003;29:596–602. doi: 10.1007/s00134-003-1659-5. [DOI] [PubMed] [Google Scholar]
- 33.Gagnadoux F, Le Vaillant M, Goupil F, et al. IRSR sleep cohort group. Influence of marital status and employment status on long-term adherence with continuous positive airway pressure in sleep apnea patients. PLoS One. 2011;6:e22503. doi: 10.1371/journal.pone.0022503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cartwright R. Sleeping together: a pilot study of the effects of shared sleeping on adherence to CPAP treatment in obstructive sleep apnea. J Clin Sleep Med. 2008;4:123–7. [PMC free article] [PubMed] [Google Scholar]
- 35.Simon-Tuval T, Reuveni H, Greenberg-Dotan S, Oksenberg A, Tal A, Tarasiuk A. Low socioeconomic status is a risk factor for CPAP acceptance among adult OSAS patients requiring treatment. Sleep. 2009;32:545–52. doi: 10.1093/sleep/32.4.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Billings ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34:1653–8. doi: 10.5665/sleep.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Woehrle H, Graml A, Weinreich G. Age- and gender-dependent adherence with continuous positive airway pressure therapy. Sleep Med. 2011;12:1034–36. doi: 10.1016/j.sleep.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 38.Amfilochiou A, Tsara V, Kolilekas L, et al. Determinants of continuous positive airway pressure compliance in a group of Greek patients with obstructive sleep apnea. Eur J Intern Med. 2009;20:645–50. doi: 10.1016/j.ejim.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 39.Kohler M, Smith D, Tippett V, Stradling JR. Predictors of long-term compliance with continuous positive airway pressure. Thorax. 2010;65:829–32. doi: 10.1136/thx.2010.135848. [DOI] [PubMed] [Google Scholar]
- 40.Yetkin O, Kunter E, Gunen H. CPAP compliance in patients with obstructive sleep apnea syndrome. Sleep Breath. 2008;12:365–67. doi: 10.1007/s11325-008-0188-4. [DOI] [PubMed] [Google Scholar]
- 41.Popescu G, Latham M, Allgar V, Elliott MW. Continuous positive airway pressure for sleep apnoea/hypopnoea syndrome: usefulness of a 2 week trial to identify factors associated with long term use. Thorax. 2001;56:727–33. doi: 10.1136/thorax.56.9.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pelletier-Fleury N, Rakotonanahary D, Fleury B. The age and other factors in the evaluation of compliance with nasal continuous positive airway pressure for obstructive sleep apnea syndrome. A Cox's proportional hazard analysis. Sleep Med. 2001;2:225–32. doi: 10.1016/s1389-9457(00)00063-0. [DOI] [PubMed] [Google Scholar]